Translate this page into:
Atypical presentation of hereditary multiple osteochondromas: Thirteen years of follow-up and analysis
Corresponding Author:
Jagadish Prabhu
Department of Orthopedics, Bahrain Defence Force and Royal Medical Services, Riffa
Kingdom of Bahrain
drjagsortho@gmail.com
| How to cite this article: Mukhtar IA, Alqasim E, Abdulkareem I, Prabhu J. Atypical presentation of hereditary multiple osteochondromas: Thirteen years of follow-up and analysis. J Musculoskelet Surg Res 2018;2:73-76 |
Abstract
Thirteen years long follow-up was carried out in our pediatric orthopedic clinic on an 18-year-old left-hand-dominant male who suffered from hereditary multiple osteochondromas affecting only his hands since he was 5 years of age. Progressive angular and rotational deformities were observed during his childhood resulting in disabilities affecting his schooling. Although successive conservative and surgical management were undertaken, the exostoses reappeared constantly and randomly. A great functional improvement was noticed following each surgical intervention resulting in the patient being left with absolutely no functional impairment and little cosmetic deformity in his adulthood.Introduction
Hereditary multiple osteochondromas (HMO) also known as hereditary multiple exostoses is an autosomal dominant disease related to the mutation of three genes; the exostosis genes EXT1, EXT2, and rarely EXT3. It is a chondrogenic disorder arising from abnormal cartilage leading to the formation of multiple benign bony tumors with cartilaginous caps (osteochondromas).[1]
The most common form of exostosis occurs in a solitary form (85%), while HMO accounts only for 15%. The disease affects the long and flat bones most commonly with rare involvement of the hands. In hand, the metacarpals, proximal, and middle phalanges are the most common sites of affection.[2]
Clinical features may include asymptomatic swellings or nodules, but rotational or angular deformities of the digits and block to flexion of the proximal interphalangeal joint may occur.[2] Pain and sensory deficits may result from either fracture or soft-tissue pressure, for example, tendons, capsule, nerves, or vessels. Rarely, a malignant transformation may occur in 1% of solitary osteochondromas and 3%–5% of HMO.[3] Predictors of malignant transformation may include a large thickness of the cartilaginous cap, that is, more than 3 cm before skeletal maturity and more than 1.5 cm in adults, exostosis growth after maturity, increasing pain, and irregular mineralization.[4]
The mainstay of diagnosis is plain radiograph. Sessile (large base) or pedunculated (narrow stalk) lesions may be seen. Other diagnostic modalities include computerized tomography, magnetic resonance imaging, ultrasound, radionuclide bone scintigraphy, and positron-emission tomography.[5] Histological studies can also be used to confirm the diagnosis.
Case Report
We present a case of an 18-year-old male who suffered since his childhood from multiple small swellings affecting the fingers of his both hands. We followed up this patient since his childhood at our pediatric orthopedic clinic until his adulthood.
He was first presented to our clinic at the age of 5 years by his father when he noticed that his son developed multiple progressive hard swellings affecting his left hand. The patient was completely healthy, and there was no history of congenital anomaly or trauma. Physical examination revealed multiple, hard, immobile bony swellings over the dorsum of the left hand involving the 3rd and 5th metacarpal bones. The father was reassured considering the benign nature of the bony lesions, and the patient was followed up at regular intervals.
At the age of 9 years, however, he presented again complaining of difficulty in holding his school bag and playing cricket, which needed good grip strength and complete flexion of metacarpophalangeal joints of both the hands. Radiographic examination [Figure - 1] revealed bony eminences over the dorsoulnar aspect of the distal metaphysis of the 3rd and 5th metacarpal bones, the same findings as seen in his first radiograph, but quite larger at this stage. Skeletal survey was conducted to look for other similar silent bony lesions anywhere else in the body. There were no such lesions except left-hand involvement. Since the child was symptomatic at this stage, we planned excisional biopsy of both bony masses and came to the definitive diagnosis. Considering clinical radiographic findings and histopathological examination of biopsy, the diagnosis of HMO of the left hand was established. Later on, the child was asymptomatic for many years and was able to do his daily activities and involved in sports without discomfort.
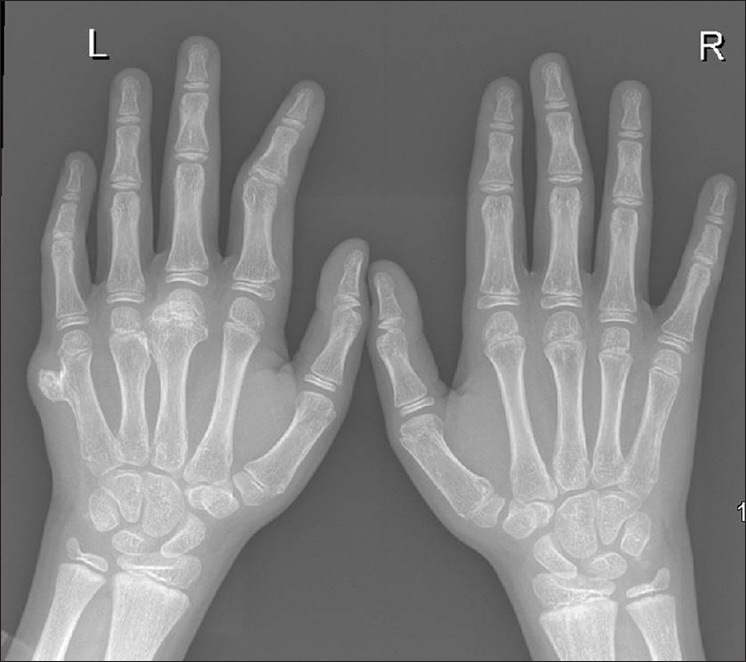 |
| Figure 1: Radiographic picture showing exostoses/osteochondroma lesion involving bones in the left hand at 8 years of age |
At 11 years of age, he presented to our clinic with a painful deformity in the left index finger restricting him from holding a pen, key, and similar small objects. On clinical examination, he had a small bony hard mass over the dorsal aspect of the proximal interphalangeal joint with secondary boutonniere deformity of the left index finger. Radiograph [Figure - 2] showed exostoses involving the base of the middle phalanx, which resulted in attenuation of central slip and volar migration of lateral bands of extensor apparatus of the left index finger resulting in the boutonniere deformity. He underwent excision of the bony mass and reconstruction of extensor mechanism to correct the boutonniere deformity, which corrected his pinch grip and writing ability.
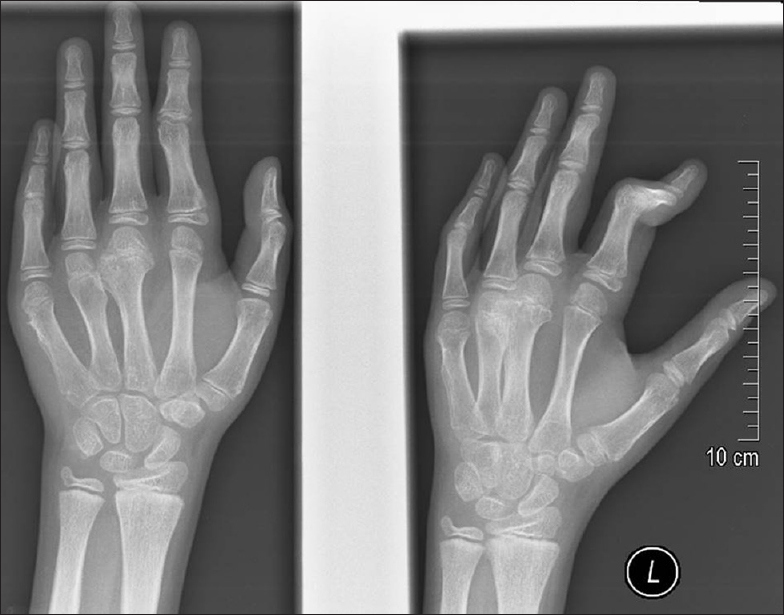 |
| Figure 2: Radiographic picture showing new exostoses/osteochondroma lesion involving bones in the left hand at 11 years of age |
Certainly, at the age of 15 years, he presented again with similar complaints, but this time affecting the fingers of both the hands. Radiograph demonstrated [Figure - 3] exostoses involving distal phalanx of the right ring finger, right 3rd metacarpal, and left 2nd and 4th metacarpal bones. A second radiological skeletal survey still did not show any affection of other bones except those of the digits of both hands. This time even though multiple bones were involved, we considered excision of only symptomatic bony masses.
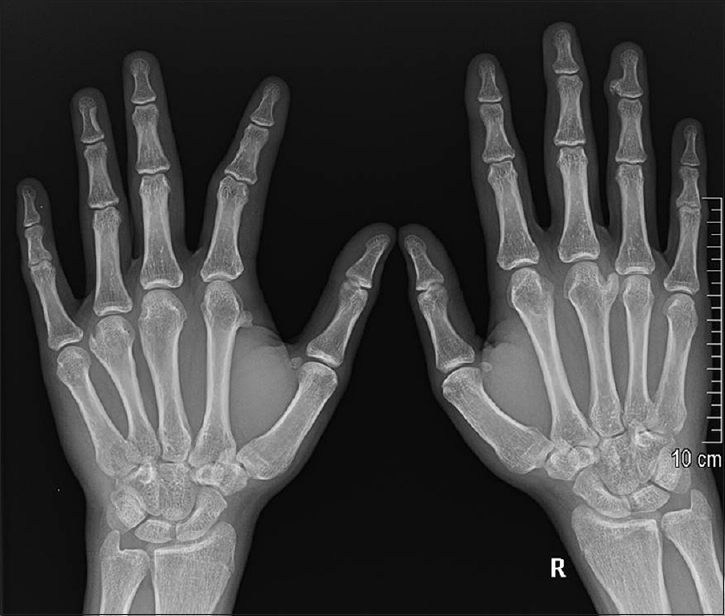 |
| Figure 3: Radiographic picture showing exostoses/osteochondroma lesion involving bones in both the hands at 15 years of age |
During his last follow-up visit at 18 years of age, the patient reported no pain, no motor weakness, no sensory loss, and no limitation of function. However, we noticed small insignificant nonsymptomatic nodules [Figure - 4], minor deformity of the fingers without functional limitation [Figure - 5], or secondary malignant transformation of the lesions. Radiographic examination of other joints including the knees, shoulders, and cervical spine were also performed revealing no affection of other joints. The patient was finally discharged from the pediatric orthopedic clinic.
 |
| Figure 4: Radiographic picture of both the hands of the same patient at 13-year follow-up |
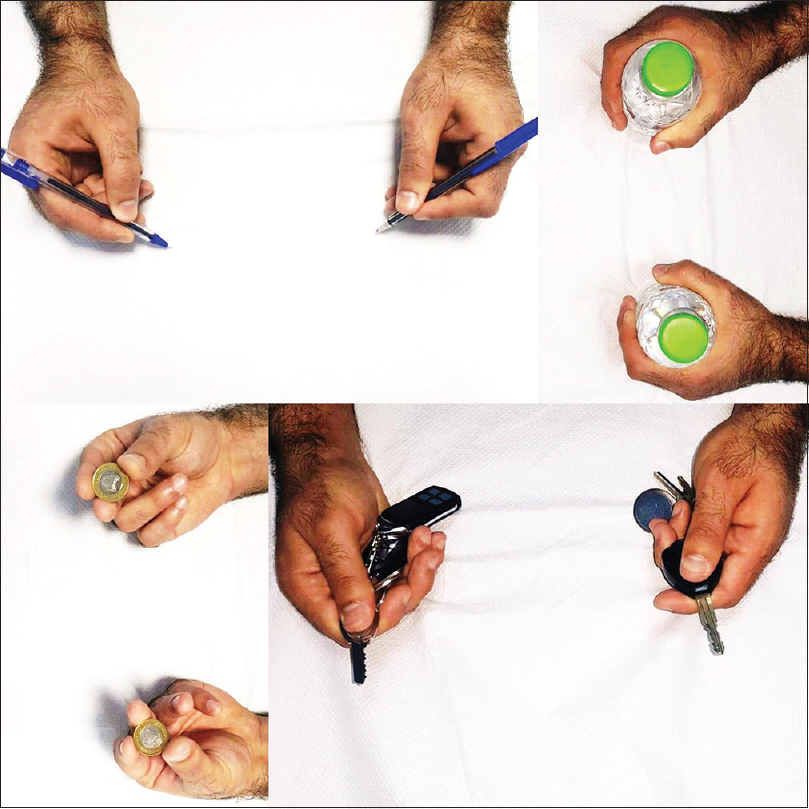 |
| Figure 5: Final clinic picture of the patient demonstrating functional outcome without deficit |
Discussion
The diagnosis of HMO is rarely made at birth.[6] The distribution is usually bilateral,[7] but a strong unilateral predominance has been described by other authors.[6] Symptoms may be due to fracture, osseous deformity limiting the range of motion, impingement of osteochondromas on vessels, nerves and tendons, bursa formation, and malignant transformation.[8],[9] In affected children and adults, annual surveillance of the osteochondromas is recommended. Monitoring the size of adult osteochondromas is important, due to the risk of malignant transformation into chondrosarcomas.[10] Surgical excision of an osteochondroma should be performed after the fusion of the epiphyses to avoid as early intervention risks disruption of the growth plate. Asymptomatic and uncomplicated osteochondroma are best managed conservatively with regular surveillance; however, sometimes surgical interventions become mandatory to deal with complications.[11]
In our opinion, if the condition results in a functional impairment, it is essential to surgically excise the osteochondromas. This is especially true in a growing child where the growth plates are still open in which such deformities would ultimately result in long-term functional and cosmetic disruption and consequently, leading to disability.
Our patient presented to us almost once in 2 years with new deformity causing functional disability, and they were isolated only to the hands. Some of the lesions were in the same small bone but at different site. Although successive conservative and surgical management were undertaken, the osteochondromas reappeared constantly and randomly. It is sometimes suggested that surgical excision of the osteochondromas results in complete resolution. In our patient, however, we noticed that the multiple nodules kept reappearing at different sites in the hands. Indeed, the condition, as expected, did stop at adolescence and the patient reported no new nodules. This is why we recommend “timely intervention” for these patients as such patients need either a surgical procedure or physical therapy, before they develop permanent deformity and disability. He is currently participating in sports that require fine skills of the hands. Apart from the minor residual cosmetic angular deformity, he reports absolutely no impairment or limitations to the daily use of his hands. This, we believe, was due to the multiple prompts and effective surgical approaches we undertook toward his complaints during his childhood.
Conclusion
The main purpose of presenting this case report is to discuss the atypical presentation of isolated hand HMO, importance of timely limited surgical intervention for the symptomatic bony lesions and need of frequent follow-up with the assessment of the case to make sure that patients will not end up with the permanent functional disability or related complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Acknowledgment
We would like to thank Maj. Gen. Prof. Khalid Bin Ali Al-Khalifa for his continuous support and encouragement toward research and publications at the Royal Medical Services, Bahrain Defence Force hospital.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors contributions
All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Ohkuma R, McCarthy EF, Deune EG. Hereditary multiple exostoses in the hands and fingers: Early presentation and early surgical treatment in family members. Case reports. Hand (N Y) 2011;6:209-16. [Google Scholar] |
| 2. | Yoshioka S, Hamada Y, Takata S, Takai H, Yasui N. An osteochondroma limiting flexion of the proximal interphalangeal joint in hereditary multiple exostosis: A Case report. Hand (N Y) 2010;5:299-302. [Google Scholar] |
| 3. | Tzaveas A, Paraskevas G, Gekas C, Vrettakos A, Antoniou K, Spyridakis I, et al. Anatomical variation of co-existence of 4th and 5th short metacarpal bones, sesamoid ossicles and exostoses of ulna and radius in the same hand: A case report. Cases J 2008;1:281. [Google Scholar] |
| 4. | Kalyani R, Prabhakar K, Gopinath B, Sheik Nasser B, Krishnamurthy D. Multiple hereditary exostoses in a family for three generation of Indian origin with review of literature. J Clin Diagn Res 2014;8:LD01-3. [Google Scholar] |
| 5. | Kok HK, Fitzgerald L, Campbell N, Lyburn ID, Munk PL, Buckley O, et al. Multimodality imaging features of hereditary multiple exostoses. Br J Radiol 2013;86:20130398. [Google Scholar] |
| 6. | Legeai-Mallet L, Munnich A, Maroteaux P, Le Merrer M. Incomplete penetrance and expressivity skewing in hereditary multiple exostoses. Clin Genet 1997;52:12-6. [Google Scholar] |
| 7. | Greenfield GB. Hereditary multiple exostoses (diaphysael aclasis). In: Radiology of Bone Diseases. Philadelphia: Lippincott; 1990. p. 672-8. [Google Scholar] |
| 8. | Murphey MD, Choi JJ, Kransdorf MJ, Flemming DJ, Gannon FH. Imaging of osteochondroma: Variants and complications with radiologic-pathologic correlation. Radiographics 2000;20:1407-34. [Google Scholar] |
| 9. | Mehta M, White LM, Knapp T, Kandel RA, Wunder JS, Bell RS, et al. MR imaging of symptomatic osteochondromas with pathological correlation. Skeletal Radiol 1998;27:427-33. [Google Scholar] |
| 10. | Pannier S, Legeai-Mallet L. Hereditary multiple exostoses and enchondromatosis. Best Pract Res Clin Rheumatol 2008;22:45-54. [Google Scholar] |
| 11. | Carpintero P, León F, Zafra M, Montero M, Berral FJ. Fractures of osteochondroma during physical exercise. Am J Sports Med 2003;31:1003-6. [Google Scholar] |
Fulltext Views
3,675
PDF downloads
1,138





