Translate this page into:
Tibialis anterior muscle herniation repaired with trevira tube: A surgical technique and review of literature
2 Department of Surgery, Division of Orthopedic Surgery, King Abdulaziz Medical City, Ministry of National Guard Health Affairs, Riyadh, Saudi Arabia
3 Department of Surgery, Division of Orthopedic Surgery, King Abdulaziz Medical City, Ministry of National Guard Health Affairs; King Abdullah International Medical Research Center's, King Saud Bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
Corresponding Author:
Wazzan S Al Juhani
Department of Surgery, Division of Orthopedic Surgery, King Abdulaziz Medical City, King Saud Bin Abdalaziz University for Health Sciences, National Guard Health Affairs, 2682 Ar Rimayah, Riyadh 14611
Saudi Arabia
aljohaniwa@ngha.med.sa
| How to cite this article: Al Rehaili HA, Al Ghamdi AM, Al Juhani WS. Tibialis anterior muscle herniation repaired with trevira tube: A surgical technique and review of literature. J Musculoskelet Surg Res 2019;3:357-362 |
Abstract
Muscle herniation is an outpouching of the muscle tissue through the fascia covering it. Although it is considered a rare condition, some reports had been published with the concern of misdiagnosis. Lower limbs are considered the most common area of muscle herniation and tibialis anterior muscle is the commonest. Patients usually seek medical advice for pain, cosmetic purposes, or even a worrisome swelling. It can be constitutional in origin or acquired secondary to trauma. Clinical diagnosis is the mainstay for muscle herniation confirmed by imaging (magnetic resonance imaging and ultrasound). The majority are asymptomatic and surgical treatment is reserved for the symptomatic patients using a variety of methods. In our report, we present a case of traumatic tibialis anterior muscle herniation, repaired with trevira tube (polyethylene mesh graft). The patient was satisfied during 9 months of follow-up without immediate nor late complications.Introduction
Muscle herniation is defined as an outpouching of the muscle tissue through the fascia covering it.[1],[2] Although it can present anywhere in the body, the leg, and particularly tibialis anterior muscle, remains the most common.[3] Traumatic causes account for the majority of cases, whereas case with unclear origin is described as constitutional. It is usually asymptomatic and presents with painless swelling.[4] Diagnosis is challenging, yet it is mainly clinical.[2] Misdiagnosis mostly leads to improper referral, unnecessary investigations, and incorrect management.[5] Military soldiers, athlete, mountain climbers, and skiers are at a higher risk than other population groups. A little attention was given to this problem, although there are considerable reported cases. Conservative treatment stays the first line of management, including nonsteroidal anti-inflammatory drugs (NSAIDs), rest, compressive stockings, and activity modifications.[4],[6] Surgical option is kept for severely symptomatic cases. Numerous surgical choices have been described, consisting of direct primary repair, decompressive fasciotomy, allografts and synthetic graft, and partial muscular excision.[4] In this case report, we present a tibialis anterior muscle herniation repaired using trevira tube (polyethylene mesh graft). We propose this method as a novel repair technique for muscle herniation.
Case Presentation
A 32-year-old Saudi military man, not known to have medical illnesses, presented to the clinic with right mid-leg swelling and pain for 2 years. It appeared insidiously 6 months after a history of a motor vehicle accident. Although it was not increasing in size, it was associated with dull aching and intermittent pain. It was aggravated by prolonged standing and activity and decreased with rest. There was no history of constitutional symptoms such as fever, night sweat, loss of weight or change of appetite, and systemic review was unremarkable. General examination showed stable vital signs, average body build, normal body mass index, and normal gait. On local examination, there was a 5 cm × 6 cm subcutaneous hemispherical mass over the anterolateral aspect of right mid-leg while standing with ankle dorsiflexion. The skin over it looked normal, no dilated veins, no hotness, and no visible nor palpable pulsations [Figure - 1]. The mass disappeared during supine position. Mild tenderness was noted during palpation with nonmobile mass. It had a smooth surface with indistinct borders, soft doughy sensation, deep to subcutaneous tissue, and no palpable lymphadenopathy. The patient had a full range of motion (ROM) of knee and ankle with intact distal neurovascular function.
 |
| Figure 1: (a) Right leg in supine position showing no obvious mass. (b-d) Showing 3 cm × 5 cm subcutaneous soft-tissue mass over the anterolateral aspect of the middle right leg |
Basic laboratory results were within normal limits, and tibia-fibula radiograph was unremarkable. Magnetic resonance imaging (MRI) showed the right leg mid-tibia shaft fascia defect near the cortical edge with tibialis anterior muscle hernia [Figure - 2]. The working diagnosis was right tibialis anterior muscle hernia. The patient was started initially on nonsurgical management with NSAIDs, rest and compression stockings for 12 months, but it failed in terms of persistent discomfort during physical activity and work duties. The patient was offered the surgical option and agreed with its possible risks and complications. The patient consented for direct fascia defect repair with possible mesh repair, which was successfully attempted.
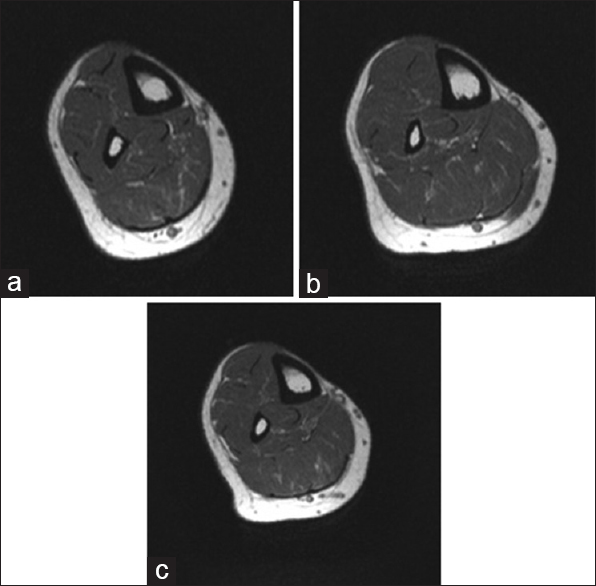 |
| Figure 2: (a-c) Magnetic resonance imaging T1 cross-section showed the right leg mid-tibia shaft fascia defect near the cortical edge with tibialis anterior muscle hernia |
Operative procedure
Preoperative skin marking was done during the maximum swelling bulge. The patient was positioned supine on the operating table, and then general anesthesia was induced combined with a popliteal regional block. Cefazoline 2 g intravenously was given. A thigh tourniquet was applied, followed by prepping and draping in a sterile technique. Tourniquet inflated to 300 mmHg. A longitudinal 9 cm incision bisecting the swelling was done, followed by careful subcutaneous dissection. A deep fascial defect measuring 10 cm longitudinally was seen and proximal and distal edges were identified with tibialis anterior muscle herniation. Stay sutures were used on defect edges to help in view and repair. Direct primary repair of fascia was not amenable because of the excessive tension. We elected to use polyethylene terephthalate mesh (trevira tube) to cover the defect. We fixed it to the fascia edges using interrupted Polydioxanone Suture (PDS) size 1, then reinforced it with a running vicryl suture size 0 [Figure - 3]. Tourniquet was deflated and hemostasis was assured. Subcutaneous tissue was approximated with vicryl sutures then skin closed with prolene size 2-0 in vertical mattress fashion and covered with a sterile dressing. A below-knee backslap with a full ankle cast in neutral position was applied to prevent ankle dorsiflexion.
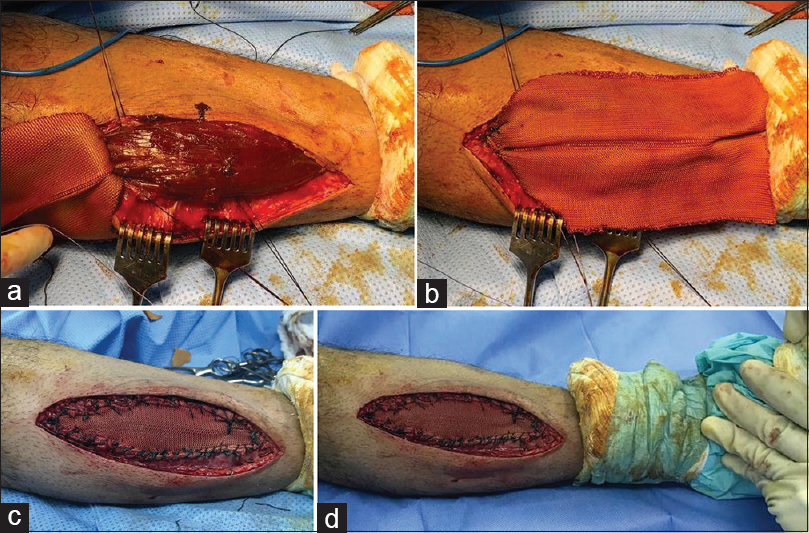 |
| Figure 3: (a) Right tibialis anterior muscle hernia with fascial defect. (b) Trevira tube over the muscle hernia. (c) After suturing, the muscle hernia with trevira tube in resting position. (d) No muscle hernia with ankle dorsiflexion indicating intact fascial repair |
The patient was kept in the hospital for 1-day postoperatively to observe for compartment syndrome. He received three doses of prophylactic antibiotics before discharge. He was supplied with NSAIDs as needed for pain, low-molecular-weight heparin and oral antibiotic (augmentin) for 2 weeks. Postoperative instructions were nonweight bearing for 3 weeks and follow-up after 1 week for wound check. There were no postoperative complications such as wound dehiscence, infection, and compartment syndrome. After 3 weeks from the operation, stitches and cast were removed, and he was allowed for full weight-bearing as tolerated with physiotherapy referral for ankle ROM exercises. The patient returned to his normal activities after 3 months without symptoms [Figure - 4] and was followed for 9 months satisfied with the outcome.
 |
| Figure 4: (a and b) Three months postright tibialis anterior muscle hernia repair with no sign of recurrence |
Discussion
Historically, the first recorded case of muscle herniation in literature was in 1839 by Dupuytren, a French surgeon, in which he distinguished it from the varicose veins.[7] Later, it was described by 1853 by Richet, then properly defined in 1861 by Mourlon as “the movement of a muscle out of its torn aponeurosis.”[4] Its prevalence is not well studied and all published studies are case reports.
Tibialis anterior is thought to have a higher risk for its tight, weak, and superficial fascia compared to other compartments, and the leg is a more susceptible area for trauma.[4],[6],[8] This could be the circumstance in the patient we presented. Although tibialis anterior muscle is the most common site of hernia, there were other reported cases involving other muscles as peroneus longus, peroneus brevis, extensor digitorum longus, gastrocnemius, and flexor digitorum longus.[9]
Fascia defect was first classified by Ihde into congenital (constitutional) or acquired (traumatic).[10] A constitutional defect occurs with no clear cause, either congenital or repetitive minor stresses over the fascia. A mesodermal insufficiency results in fascia weakness and predisposition to tear.[6],[11] Vascular fenestrations in the fascia possess a weak area for herniation, especially if strained by vascular engorgement and muscular hypertrophy.[2],[12] Repetitive minor stresses and increased intracompartmental pressure would increase the risk of herniation through such weak areas.[2],[6],[8] Traumatic type is more common, and it usually occurs after a direct blunt or penetrating trauma to the compartment, causing a tear in the fascia, or even by an iatrogenic origin.[4],[6],[8] It can also happen indirectly by an injury to the contracting muscle causing disruption of the overlying fascia.[6],[11] Interestingly, even a bilateral leg muscle herniation have been reported by Ceyhan et al.[8] Most of the cases reported were males in young adult age.[1],[4] Population at higher risk are those involved in activities or occupations that require prolonged standing with vigorous activity as military soldiers, athletes, mountain climbers, and skiers.[2],[9] Our patient has some of these risk factors being male, military, and after blunt trauma.
The vast majority of cases are asymptomatic but cosmetically bothering.[4],[8] We believe appropriate history taking and physical examination would lead to the diagnosis. Diagnosis is mainly clinical, and few history and clinical points should raise the suspension for muscle herniation among the deferential diagnosis.[2] Characteristic finding in lower limb muscle herniation during examination is positional change of swelling size, which increases during weight-bearing and muscle contraction as dorsiflexion of the ankle “fencer's lunge position,” and reduces during relaxation and supine position.[13] These signs were clearly seen in our patient with a significant change of size with position change, especially while standing and squatting. An observed sign that may be favoring muscle herniation as a diagnosis is “skin slide” sign in which skin clearly slides over the bulge.[8] Peripheral nerve palsy may be present as reported by Nguyen et al. in a case of peroneus brevis hernia concurrently with superficial peroneal nerve compression that improved after fasciotomy.[4] Some studies considered muscle herniation a rare condition, while others believed that it is underdiagnosed and not well studied.[2],[6],[14] The patient in this report was referred from a primary care clinic with unclear diagnosis and maybe a soft-tissue tumor. The rarity of similar cases maybe a contribution to ignorance or misdiagnosis.[2] Misdiagnosis can lead to wrong referrals, unnecessary investigations, the persistence of symptoms, and patient suffering.[5] There are multiple possible differential diagnoses of muscle hernia such as muscle tear, hematoma, vascular diseases (varicose vein, angioma, arteriovenous malformation, and thrombophlebitis), and soft-tissue neoplasm (lipoma, epidermoid cyst, fibroma, and schwannoma).[4],[5],[9],[15],[16],[17]
Dynamic ultrasonography and MRI are complementary and confirmatory investigating tools.[4] Imaging is helpful to eliminate other differential diagnoses, while small hernias may be unnoticed by imaging.[6] MRI would show loss of fascial integrity, muscle tissue hernia through fascia, or avulsion of fascia tibial attachment.[12] Likewise, in our case, MRI showed a fascia defect near the anterior tibial cortical edge.
There are various treatment options with great debate and no clear agreement for superiority.[2] In general, asymptomatic patients are reassured and effectively treated conservatively, and the surgical option is not recommended for this group.[14] Rest, analgesia, activity modifications, compression stockings, and avoidance of vigorous activities are efficient.[4],[5],[6],[15],[18] In our case, we followed the recommendation of initial conservative treatment even in symptomatic patients. Surgical options are reserved for severe cases or symptomatic patients whom conservative treatment have failed.[1],[4]
Different surgical options had been described in the literature [Table - 1], including decompressive fasciotomy, direct primary repair, autologous fascia graft, synthetic patch and mesh, periosteal flap, partial muscular excision, and acellular porcine dermal matrix.[4],[6],[14],[19] There is no gold standard surgical method nor clear indications to use a specific surgical option. Intracompartmental injections were also used including sodium morrhuate (sclerosing agents), triamcinolone (glucocorticoid), and botulinum toxins.[1],[4],[14]
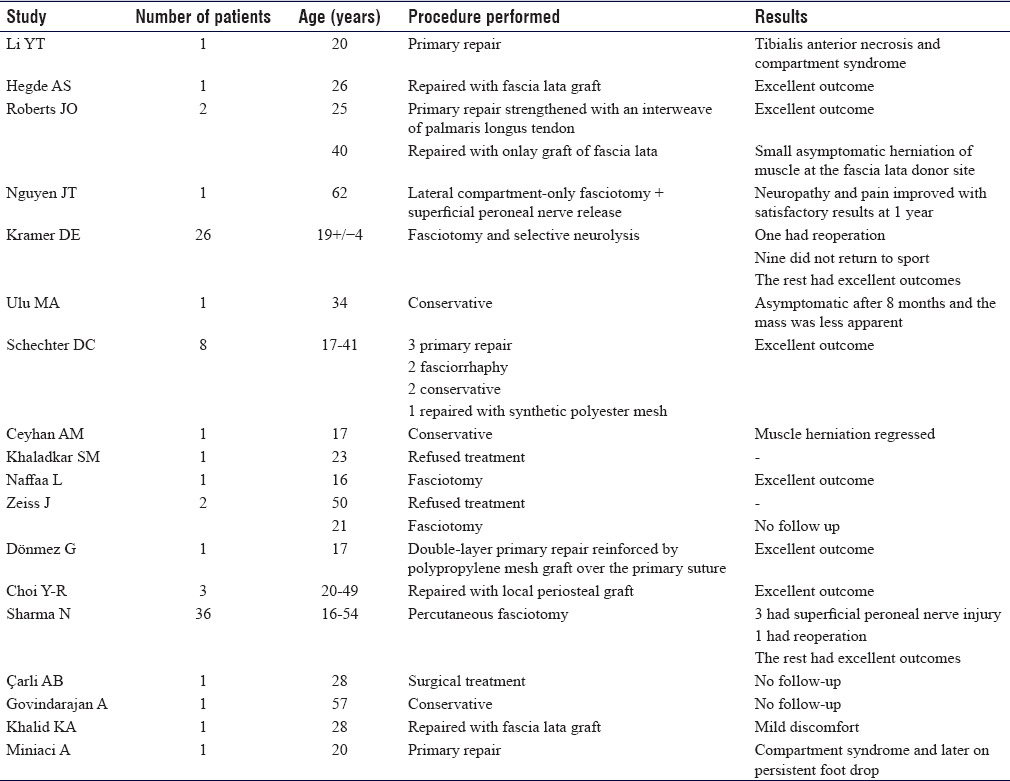
Complications of neglecting symptomatic muscle hernia would include chronic pain, chronic compartment syndrome, and nerve palsy of nearby nerves. Surgical complications include compartment syndrome, infection, recurrence of hernia, and a large scar in pure fasciotomy.[2],[4],[6],[14] Fasciotomy is considered the safest surgical option but cosmetically inferior and may potentiate for venous system disease by decreasing intracompartmental pressure and calf muscles pump.[4] Large symptomatic muscle hernias would benefit more from fasciotomy, while small hernias can be primarily repaired.[2],[6] Autologous fascia graft predisposes donor site to hernia.[2] Three cases of leg hernia reported were repaired with tibia periosteum flap followed for 1 year with no complications nor recurrence of symptoms.[14]
Synthetic mesh carry out the risk of soft-tissue sensitivity, adhesions, and infection.[2],[4] When primarily repaired, large hernias are at risk of compartment syndrome or hernia recurrence.[2] Li et al. reported a case that developed compartment syndrome 1 day following primary repair of leg fascia, which mandated fasciotomy and frequent irrigation and debridement and resulted in common peroneal nerve denervation.[1] Compartment necrosis can happen in as early as 3 h after an insult or ischemia to the compartment.[20] For primary facia repair, a two-stage repair was recommended to prevent compartment syndrome and soft-tissue necrosis.[1] For these reasons, we preferred to prevent serious complications and avoid direct primary facia repair.
During the literature review, we did not come across a study dealing with muscle herniation repaired with trevira soft-tissue attachment tube. We used “MUTARS® ImplantCast made of polyethylene terephthalate 55/300 mm.” This material we often used it in cases of soft-tissue defect reconstruction after musculoskeletal tumor resections. Therefore, we thought of it as a new method of repair that was not used previously. Risk of infection is considered higher when using trevira tube, for that reason, we elected to continue postoperative prophylactic antibiotic for 2 weeks.
Postoperative activities varied between researchers, but most of them had restricted ROM and nonweight-bearing for the first 1–2 weeks, followed by gradually joint ROM and weight-bearing.[2],[14] To decrease stress on the graft and surgical wound, we chose to immobilize the muscle contraction and restrict weight-bearing for 3 weeks. We used a below-knee backslap with a full ankle cast in a neutral position and nonweight-bearing for 3 weeks. That was followed by gradual full weight-bearing as tolerated with physiotherapy referral for ankle ROM exercises. After 9 months of follow-up in the clinic, we did not encounter postoperative complications and the patient was satisfied functionally and cosmetically. He was able to return to his normal daily activity without symptoms after 5 months from the facia repair.
Our study limitation is that we followed the patient for 9 months and we did not use clinical score measurement. We lost contact with the patient after 9 months.
Conclusion
Muscle herniation is rarely encountered in the Orthopedic Clinic that may represent true rarity or neglect and misdiagnosis. Its true prevalence is unknown. In our study, we diagnosed a tibialis anterior muscle herniation clinically and confirmed it by MRI. Conservative treatment for 12 months has failed. Thus, the surgical option was planned. Innovative repair of leg fascia with trevira tube was performed. After 9 months of follow-up, outcomes were pleasing clinically and to the patient. In this regard, we suggest using trevira tube as one of the treatment options of repairing fascia tissue in cases of muscle herniation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
HAA, AMA, and WSA conceived and designed the study, conducted research, provided research materials, and collected and organized data. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Li YT, Hung CC, Pan RY, Hua SY. Compartment syndrome following directly Repair of hernia of anterior tibialis. J Med Sci 2015;35:261-3. [Google Scholar] |
| 2. | Hegde AS. An interesting case of post traumatic tibialis anterior muscle herniation. Kathmandu Univ Med J (KUMJ) 2013;11:332-4. [Google Scholar] |
| 3. | Roberts JO, Regan PJ, Dickinson JC, Bailey BN. Forearm muscle herniae and their treatment. J Hand Surg Br 1989;14:319-21. [Google Scholar] |
| 4. | Nguyen JT, Nguyen JL, Wheatley MJ, Nguyen TA. Muscle hernias of the leg: A case report and comprehensive review of the literature. Can J Plast Surg 2013;21:243-7. [Google Scholar] |
| 5. | Kramer DE, Pace JL, Jarrett DY, Zurakowski D, Kocher MS, Micheli LJ. Diagnosis and management of symptomatic muscle herniation of the extremities: A retrospective review. Am J Sports Med 2013;41:2174-80. [Google Scholar] |
| 6. | Report C, Sunumu O, Ulu MA, Çakmak M, Nas K. A case of tibialis anterior muscle herniation diagnosed by ultrasonography. Pol J Radiol 2013;59:73-5. [Google Scholar] |
| 7. | Schechter DC, Palmieri AJ, Vaden OL. Myocele of the lower limb. Arch Surg 1961;83:825-34. [Google Scholar] |
| 8. | Ceyhan AM, Chen W, Yener M, Yildirim M, Yesildag A, Akkaya VB. Bilateral tibialis anterior muscle herniation simulating a soft tissue tumour in a young amateur football player. Australas J Dermatol 2010;51:142-4. [Google Scholar] |
| 9. | Khaladkar SM, Kondapavuluri SK, Kamal A, Kalra R, Kamal V. Detection of myofascial herniation on dynamic sonography and magnetic resonance imaging. Case Rep Radiol 2016;2016:4245189. [Google Scholar] |
| 10. | Idhe H. On muscular hernia of the leg. Acta Chir Scand 1929;65:97-120. [Google Scholar] |
| 11. | Naffaa L, Moukaddam H, Samim M, Lemieux A, Smitaman E. Semimembranosus muscle herniation: A rare case with emphasis on muscle biomechanics. Skeletal Radiol 2017;46:373-8. [Google Scholar] |
| 12. | Zeiss J, Ebraheim NA, Woldenberg LS. Magnetic resonance imaging in the diagnosis of anterior tibialis muscle herniation. Clin Orthop Relat Res 1989;244:249-53. [Google Scholar] |
| 13. | Dönmez G, Evrenos MK, Cereb M, Karanfil Y, Doral MN. Double layer repair of tibialis anterior muscle hernia in a soccer player: A case report and review of the literature. Muscles Ligaments Tendons J 2015;5:331-4. [Google Scholar] |
| 14. | Harwin SF, Choi YR, Hong CG. Repair of tibialis anterior muscle herniation using periosteum. Orthopedics 2014;37:748-50. [Google Scholar] |
| 15. | Sharma N, Kumar N, Verma R, Jhobta A. Tibialis anterior muscle hernia: A case of chronic, dull pain and swelling in leg diagnosed by dynamic ultrasonography. Pol J Radiol 2017;82:293-5. [Google Scholar] |
| 16. | Çarli AB, Turgut H, Bozkurt Y. Choosing the right imaging method in muscle hernias: Musculoskeletal ultrasonography. J Sports Sci 2015;33:1919-21. [Google Scholar] |
| 17. | Govindarajan A, Inigo A. Tibialis anterior muscle hernia: A rare differential of a soft tissue tumour. BMJ Case Rep 2015;2015. pii: bcr2015212462. [Google Scholar] |
| 18. | Khalid K, Mah E. Treatment of a symptomatic forearm muscle herniation with a wrap-around fascia lata graft. J Hand Microsurg 2016;1:54-9. [Google Scholar] |
| 19. | Miniaci A, Rorabeck CH. Compartment syndrome as a complication of repair of a hernia of the tibialis anterior. A case report. J Bone Joint Surg Am 1986;68:1444-5. [Google Scholar] |
| 20. | Vaillancourt C, Shrier I, Vandal A, Falk M, Rossignol M, Vernec A, et al. Acute compartment syndrome: How long before muscle necrosis occurs? CJEM 2004;6:147-54. [Google Scholar] |
Fulltext Views
12,924
PDF downloads
1,581





