Translate this page into:
Open versus Minimally invasive transforaminal lumbar interbody fusion: Intermediate outcomes in overweight and obese patients
2 College of Medicine, King Saud Bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia
Corresponding Author:
Muath M Alswat
College of Medicine, King Saud Bin Abdulaziz University for Health Sciences, P.O. Box 9515, Mail Code: 6556, Jeddah 21423
Saudi Arabia
alswat016@ksau-hs.edu.sa
| How to cite this article: Khashab MA, Alswat MM, Alsofiani BS, Algamedi OA, Shulan MF. Open versus Minimally invasive transforaminal lumbar interbody fusion: Intermediate outcomes in overweight and obese patients. J Musculoskelet Surg Res 2020;4:82-86 |
Abstract
Objectives: To compare the intermediate results between minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) and open approach in obese and overweight patients. Methods: A retrospective cohort study was conducted in which all cases of obese (body mass index [BMI] ≥30) and overweight (BMI ≥25) patients who had TLIF done in KAMC-NGHA, Jeddah, from January 2009 to December 2018 were reviewed. Patients were divided into two groups, namely MIS-TLIF and OPEN-TLIF and were compared in operative time, blood loss, length of hospitalization (LOH), decrease in hemoglobin, time before ambulation (TBA), and postoperative medium-term function using the Oswestry Disability Index (ODI). Results: Sixty-three MIS-TLIF and 41 Open-TLIF patients were included in the study. BMI for the open group was 31.5 kg/m2 and 33.2 kg/m2 for the MIS group. Blood loss was 175 ml for MIS-TLIF and 414.89 ml for OPEN-TLIF (P = 0.004). LOH was 4.60 days for MIS-TLIF and 8.29 days for OPEN-TLIF (P = 0.018). TBA was 1.86 days for MIS-TLIF and 3.60 days for OPEN-TLIF (P = 0.022). Operative time was 3.96 h for MIS-TLIF and 4.47 h for OPEN-TLIF (P = 0.56). The decrease in hemoglobin was 1.13 g/dl for MIS-TLIF and 1.61 g/dl for OPEN-TLIF (P = 0.435). ODI score was 25.57 points for MIS-TLIF and 19.67 points for OPEN-TLIF (P = 0.767). Conclusion: The results in MIS-TLIF are comparable with OPEN-TLIF in terms of functional outcomes. The advantages of MIS-TLIF are lesser blood loss, shorter hospital stay, and early mobilization; therefore, it is an attractive alternative for OPEN-TLIF in obese and overweight patients. However, large randomized studies are still needed.Introduction
According to the World Health Organization, obesity has nearly tripled since 1975. In 2016, more than 1.9 billion adults were overweight, third of whom were obese.[1] In Saudi Arabia, obesity prevalence was recently estimated to be 28.7%, with women having higher prevalence.[2] Among obese and overweight people, degenerative spine diseases were more common, and studies have shown obesity to be a risk factor in developing them,[3],[4],[5],[6],[7] with a higher risk of developing degenerative spine disease, the number of obese patients who need spine surgery is on the rise.
Degenerative diseases of the lumbar spine are increasing in prevalence. In a study done in Saudi Arabia that included patients attending the department of physical therapy at King Fahd Hospital in Dammam, they found the prevalence of spinal disorders to be 28.1% of all referred patients and 53.1% of the disorders were affecting the lumbar spine.[8] Degenerative spine diseases lower the quality of life by causing disturbing back pain and radicular symptoms. Their spectrum includes degenerative disc diseases, facet joint arthritis, spinal stenosis, degenerative spinal scoliosis, and spondylolisthesis.[9]
As the number of affected obese patients increases, surgeons face challenges in managing such patients with their other obesity-related problems, for example, diabetes, hypertension, and dyslipidemia. Spine fusion is a surgical option in managing degenerative spinal diseases. However, three systematic reviews have shown obesity to be associated with more blood loss, longer hospital stay, and higher complication rate in lumbar spine fusion surgeries.[10],[11],[12]
One of the surgical fusion options is transforaminal lumbar interbody fusion (TLIF). Since 1998, when Harms and Jeszenszky popularized TLIF, it has stood the test of time in accomplishing its goals.[13] In comparison to its predecessors such as posterior lumbar interbody fusion (PLIF), TLIF has many advantages such as allowing easy access to the lamina, ligamentum flavum, facet joints, less soft tissue and paraspinal muscle dissection, less removal of bony surfaces, and decrease the exposure of midline neural structures (e.g., dura).[9] TLIF can be performed using an open approach or via a newer minimally invasive method. The newer minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) approach has received increased interest and acceptance with the same fusion technique used in OPEN-TLIF.[14],[15] Although minimal invasive spine surgeries have shown to be safe and not contraindicated in obese patients, the superiority of MIS-TLIF over OPEN-TLIF is yet to be established, and few studies have compared the two in obese or overweight patients.[7],[16],[17]
Our aim in this study was to determine the difference between OPEN-TLIF and MIS-TLIF in intermediate operative results and clinical outcomes. Up to our knowledge, this is the first study to compare the results of the two techniques in the Saudi population and one of the few studies that has focused on overweight and obese patients worldwide.
Materials and Methods
Study design
All cases of OPEN-TLIF and MIS-TLIF that were done in the National Guard Hospital, Jeddah, Saudi Arabia, in the period between January 2009 to December 2018 were reviewed. A retrospective cohort study then was done to compare the two interventions. The comparison parameters were intraoperative parameters (operative time and estimated blood loss), immediate postoperative parameters (length of hospital stay, drainage, pretransfusion decrease in hemoglobin, and time before ambulation [TBA]), and postoperative med-term function, which was assessed by telephone interviews with the patients using a validated Arabic version of the Oswestry Disability Index (ODI). The response rate to the phone calls was 89% (n = 93).[18] All data were obtained from the hospital's electronic record and patients' files using data collection sheets, which included patients' demographics (age and gender), indications for surgery (degenerative disc disease, prolapsed intervertebral discs, spinal stenosis, and spondylolisthesis), levels of surgery, and the mentioned comparison parameters.
Study population
Patients who underwent OPEN-TLIF OR MIS-TLIF for degenerative conditions (degenerative spondylolisthesis and disc herniation) were reviwed. Only patients who were obese with a body mass index (BMI) ≥30 or overweight with a BMI ≥25 were included, whereas patients with spondylodiscitis or previous lumbar spine surgery were excluded. A consecutive sampling technique was used since we included all the patients who fulfilled the criteria.
Surgical techniques
Minimally invasive-transforaminal lumbar interbody fusion
The patient was intubated under general anesthesia and then was placed in a prone position on the Jackson table with proper padding of all the pressure points. Skin marking was done under the guidance of anterior–posterior fluoroscopy. In sterile fashion, the patient was then prepped and draped. Above the symptomatic side, an approximately 3 cm paramidline incision was made for placement of the quadrant retractor system until the desired working diameter was achieved. After exposure of the posterolateral element of the spine has been made, laminectomy and facetectomy were performed. Identification of the disc followed by subtotal discectomy and preparation of the endplate for fusion were achieved. Bone graft was packed anterior to the cage and within the cage, including the autogenous bone grafting harvested from the decompression. Screws and rods were then placed percutaneously on both sides, and compression applied across the cage. Throughout the procedure, the use of neuronavigation with O-arm (multidirectional imaging) has been utilized for accuracy of pedicle screws insertion, decompression as well as cage placement. Thorough washing and hemostasis followed by the closure of the skin in layers were done, and pressure dressing was applied.
OPEN-transforaminal lumbar interbody fusion
The open approach was executed as described by Harms and Jeszensky using a longitudinal midline incision.[13]
Statistical analyses
Statistical analysis was performed using the IBM Statistical Package for the Social Sciences Software for Windows, version 25 (IBM Corp., Armonk, NY, USA). The following parameters (operative time, estimated blood loss, length of hospital stay, drainage, pretransfusion decrease in hemoglobin, and TBA) were presented as mean ± standard deviation. No missing data were found in the previous parameters except in ODI 11 patients (7 in MIS-TLIF and 4 in OPEN-TLIF groups) who did not respond to the phone interviews, and they were handled using mean substitution. Student's t-test was used for the comparison of continuous variables. P <0.05 was accepted for significance.
Results
During the period from January 2009 to December 2018, there were 115 obese and overweight patients who have had TLIF, of which 104 patients were included. There were 41 patients in the OPEN-TLIF group and 63 patients on the MIS-TLIF group. None of the MIS group needed to be converted to open. Indications of the surgery and baseline characteristics were similar between the two groups, as shown in [Table - 1]. The mean age for the OPEN-TLIF group was 55.26 ± 14 years, and for the MIS-TLIF group, it was 56.92 ± 13 years, P = 0.25. The mean BMI for the OPEN-TLIF group was 31.5 kg/m2 and 33.2 kg/m2 for the MIS-TLIF group, P = 0.53.
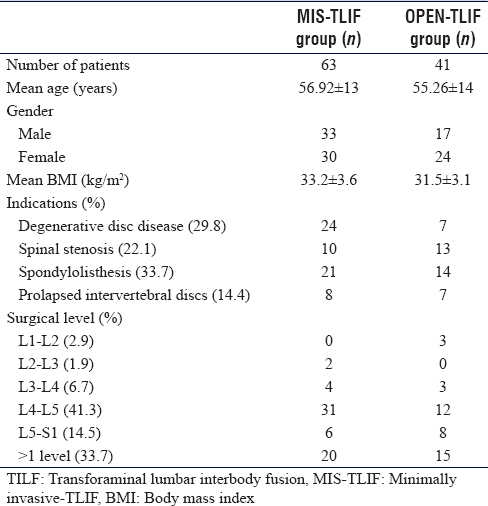
Spondylolisthesis was the most common indication for the surgery, with about one-third of the patients (n = 35), and L4–L5 was the most common level involved in 41.3% of the patients (n = 43); details of indications and levels involved are shown on [Table - 1].
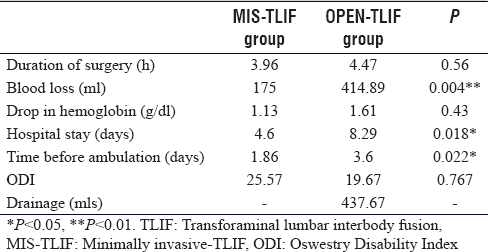
No significant difference was found between the two groups on the duration of surgery (MIS-TLIF: 3.96 ± 1 h, OPEN-TLIF 4.47 ± 1.1 h, P = 0.56). The duration of surgery was calculated from the time of skin incision to closure time. Patients on the MIS-TLIF group lost significantly less blood during the surgery than the OPEN-TLIF group (MIS-TLIF: 175 ± 130 ml, OPEN-TLIF 414.89 ± 244 ml, P = 0.004). The blood loss was measured from the suction collection pump and gauze weight. The mean postoperative pretransfusion drop in hemoglobin was not significantly different between the two groups (MIS-TLIF: 1.13 ± 0.75 g/dl, OPEN-TLIF 1.61 ± 0.83 g/dl, P = 0.435). MIS-TLIF group needed significantly shorter hospital stay than OPEN-TLIF group (MIS-TLIF: 4.60 ± 2.1 days, OPEN-TLIF 8.29 ± 4.7 days, P = 0.018). MIS-TLIF patients were able to mobilize out of bed faster than OPEN-TLIF patients with significant difference (MIS-TLIF: 1.86 ± 1.4 days, OPEN-TLIF 3.60 ± 2.3 days, P = 0.022). However, it was not statistically significant. The OPEN-TLIF group scored better than the MIS-TLIF group on ODI, which was taken postoperatively by phone interviews with patients. The mean follow-up was 45.6 months (MIS-TLIF: 25.57 ± 21.9 points, OPEN-TLIF 19.67 ± 24.1 points, P = 0.767). The OPEN-TLIF group had postoperatively with a mean drainage of 437.67 ml, whereas MIS-TLIF did not need a drain to be placed. A summary of the comparisons is shown in [Table - 2].
Discussion
The choice between open or minimal invasive TLIF for obese and overweight patients remains an area of debate. On the one hand, OPEN-TLIF has been associated with extensive dissection of paravertebral musculature leading to greater morbidity, slower recovery, and a higher risk of violating neurovascular structures during dissection to expose the spine.[19] A multicenter randomized study conducted by Alamin et al. has shown OPEN-TLIF to be associated with a greater muscle injury and edema on MRI when compared to MIS-TLIF.[20] On the other hand, MIS-TLIF is done using a small para-midline skin incision. This way of accessing the spine preserves the soft tissue that otherwise will be damaged by the open technique.[21] As a result of less tissue injury, the potential advantages of MIS-TLIF are less blood loss, less hospital stay, less postoperative pain, and quicker recovery.[7],[22] Moreover, because of less hospitalization and shorter recovery period are needed in MIS-TLIF; the total cost of the surgery is reduced, and the risk of infection is lower.[23],[24] Some observed downsides of MIS-TLIF are more radiation exposure and intraoperative technical difficulties in the early part of the learning curve due to the smaller corridor. Therefore, surgeons' experience in MIS surgery is very helpful in both reducing radiation exposure and achieving technical proficiency. Whether or not the potential advantages offered by MIS-TLIF will affect the clinical outcome in overweight or obese patients needs further investigation. A study conducted by Rosen et al. showed obese patients to have more estimated blood loss but similar surgical duration, hospital stay, and complication rate when compared to nonobese patients after minimally invasive spine surgeries.[25]
Our study retrospectively evaluated 104 obese and overweight patients who had degenerative diseases of the lumbar spine and had undergone open or minimal invasive TLIF surgeries. We found obese and overweight patients who undergone MIS-TLIF to have significantly less blood loss (175 ml) than those who had OPEN-TLIF (415 ml). This can be attributed to the fact that MIS-TLIF is a considerably less traumatic approach and the use of retractors to pull the muscle instead of dissecting them. Furthermore, the use of the microscope during MIS-TLIF helps to decrease blood loss by ensuring that the veins around the nerve roots were well protected or coagulated. Moreover, other significant differences between the two groups were in the length of hospital stay and time before mobilization. Whereas the MIS-TLIF group stayed 4.6 days and were able to mobilize after 1.9 days, the OPEN-TLIF group spent 8.3 days on hospital and took 3.6 days to mobilize partly because of less postoperative pain in the early stage after surgery. Although the difference was not statistically significant, the shorter duration of surgery needed for the MIS-TLIF group (4 h) was considered a great advantage for obese and overweight patients. The thick layer of the subcutaneous tissue and increased need for more dissection and retraction resulted in a longer duration in the OPEN-TLIF group (4.5 h). Interestingly, the drop on hemoglobin between the MIS-TLIF group (1.1 g/dl) and the OPEN-TLIF group (1.6 g/dl) was not statistically significant despite the significant difference in blood loss, which can be explained by the observation that the amount of the blood loss in the two groups was not high enough to be reflected in the postoperative hemoglobin. Postoperative ODI with a mean follow-up of 45.6 months showed that OPEN-TLIF group scored better (19.7) than MIS-TLIF (25.6), but they were statistically comparable. OPEN-TLIF group had mean postoperative drainage of 438 ml. In MIS-TLIF patients, no drain tube has been used because studies have shown no benefits using it, and it might lead to pain, anxiety, and discomfort during the postoperative period.[26],[27]
Few comparative studies have been done to compare the results and outcome of OPEN- and MIS-TLIF with a focus on obese and overweight patients. Similar results to ours were observed by Wang et al. in their study of 81 obese and overweight patients. They found the MIS-TLIF group to have significantly less operating time, less blood loss, and less postoperative back pain.[7] Another study by Lau et al. investigated 127 obese patients and showed MIS-TLIF to be associated with significantly less estimated blood loss and a shorter hospital stay than OPEN-TLIF when all patients were evaluated as a single cohort and within individual obesity classes. Moreover, MIS-TLIF patients had lower complications rate than OPEN-TLIF, and the difference was most profound and statistically significant in patients with BMI ≥40 kg/m2.[23] A similar study was done including 71 patients who had MIS-TLIF and had OPEN-TLIF and found that MIS-TLIF was superior to OPEN-TLIF in terms of duration of hospital stay and blood loss, whereas patients who underwent OPEN-TLIF had a lesser operative time and lesser fluoroscopy exposure comparing to MIS-TLIF patients. There was no statistically significant difference in the improvement of long-term function using ODI between the two groups.[28] A fourth study that compared 49 patients who underwent OPEN-TLIF and 49 patients who underwent MIS-TLIF concluded similar results to the previous studies supporting the excellence of MIS-TLIF in blood loss, hospital stay, TBA, and morphine intake. Moreover, fusion rates were similar in both MIS-TLIF and OPEN-TLIF patients.[25] The clinical data on long-term functional outcomes are still deficient. In a study that followed up open and minimally invasive TLIF patients for 5 years, the two groups had comparable results in visual analog scale, Japanese orthopedic association score, and ODI at 2 and 5 years postoperatively. Moreover, they did not find significant differences between the two groups in terms of fusion rate and prevalence of adjacent segment disease.[15]
In comparison to our study, all studies found similarly lesser blood loss, shorter hospital stay, and TBA in the MIS-TLIF group. MIS-TLIF was found to be longer in operative duration in some studies and shorter in others, which might be due to the differences in surgeons' experience in MIS surgeries.
There were some limitations in our study, including being retrospective, lack of randomization in the study design, the relatively small number of patients, the study being conducted in a single center, and the lack of preoperative baseline of ODI to evaluate the improvement. Furthermore, we did not collect data describing the complication rate, postoperative infections, and cage placement accuracy, which could have been of great value to the comparison.
Conclusion
MIS-TLIF seems to be superior to OPEN-TLIF in obese and overweight patients in terms of blood loss, length of hospital stay, and TBA, as shown by the results of our study and the reviewed literature. However, the superiority in long-term functional outcomes is yet to be established with good designed large prospective randomized control studies.
Ethical considerations
The study was approved by the Institutional Ethics Review Board of King Abdullah International Medical Research Center. Only the research participants were able to access the data. Information that identify the patient, such as the name and medical record number, were not collected. A code (letters and numbers) was given instead for each patient to replace their identifying information.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
MAK has contributed with concepts, design, definition of intellectual content, clinical study, manuscript preparation, editing, and review. MMA has contributed with design, definition of intellectual content, literature search, data acquisition and analysis, manuscript preparation, editing, and review. BSA, OAA, and MFS have contributed to literature search, data acquisition, and analysis manuscript preparation, editing, and review. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Obesity and Overweight Who.int; 2018. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. [Last accessed on 2019 Aug 15]. [Google Scholar] |
| 2. | Memish ZA, El Bcheraoui C, Tuffaha M, Robinson M, Daoud F, Jaber S, et al. Obesity and associated factors – Kingdom of Saudi Arabia, 2013. Prev Chronic Dis 2014;11:E174. [Google Scholar] |
| 3. | Heuch I, Hagen K, Heuch I, Nygaard Ø, Zwart JA. The impact of body mass index on the prevalence of low back pain: The HUNT study. Spine (Phila Pa 1976) 2010;35:764-8. [Google Scholar] |
| 4. | Heuch I, Heuch I, Hagen K, Zwart JA. Body mass index as a risk factor for developing chronic low back pain: A follow-up in the nord-trøndelag health study. Spine (Phila Pa 1976) 2013;38:133-9. [Google Scholar] |
| 5. | Dario AB, Ferreira ML, Refshauge KM, Lima TS, Ordoñana JR, Ferreira PH. The relationship between obesity, low back pain, and lumbar disc degeneration when genetics and the environment are considered: A systematic review of twin studies. Spine J 2015;15:1106-17. [Google Scholar] |
| 6. | Sheng B, Feng C, Zhang D, Spitler H, Shi L. Associations between Obesity and Spinal Diseases: A Medical Expenditure Panel Study Analysis. Int J Environ Res Public Health 2017;14. pii: E183. [Google Scholar] |
| 7. | Wang J, Zhou Y, Feng Zhang Z, Qing Li C, Jie Zheng W, Liu J. Comparison of the clinical outcome in overweight or obese patients after minimally invasive versus open transforaminal lumbar interbody fusion. J Spinal Disord Tech 2014;27:202-6. [Google Scholar] |
| 8. | Alshami AM. Prevalence of spinal disorders and their relationships with age and gender. Saudi Med J 2015;36:725-30. [Google Scholar] |
| 9. | Hey HW, Hee HT. Lumbar degenerative spinal deformity: Surgical options of PLIF, TLIF and MI-TLIF. Indian J Orthop 2010;44:159-62. [Google Scholar] |
| 10. | Jiang J, Teng Y, Fan Z, Khan S, Xia Y. Does obesity affect the surgical outcome and complication rates of spinal surgery? A meta-analysis. Clin Orthop Relat Res 2014;472:968-75. [Google Scholar] |
| 11. | Lingutla KK, Pollock R, Benomran E, Purushothaman B, Kasis A, Bhatia CK, et al. Outcome of lumbar spinal fusion surgery in obese patients: A systematic review and meta-analysis. Bone Joint J 2015;97-B: 1395-404. [Google Scholar] |
| 12. | Abdallah DY, Jadaan MM, McCabe JP. Body mass index and risk of surgical site infection following spine surgery: A meta-analysis. Eur Spine J 2013;22:2800-9. [Google Scholar] |
| 13. | Harms J, Jeszensky D. The unilateral transforaminal approach for posterior lumbar interbody fusion. Orthop Traumatol 1998;6:88-99. [Google Scholar] |
| 14. | Adogwa O, Parker SL, Bydon A, Cheng J, McGirt MJ. Comparative effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion: 2-year assessment of narcotic use, return to work, disability, and quality of life. J Spinal Disord Tech 2011;24:479-84. [Google Scholar] |
| 15. | Yang Y, Liu ZY, Zhang LM, Pang M, Chhantyal K, Wu WB, et al. Microendoscopy-assisted minimally invasive versus open transforaminal lumbar interbody fusion for lumbar degenerative diseases: 5-year outcomes. World Neurosurg 2018;116:e602-e610. [Google Scholar] |
| 16. | Wang T, Han C, Jiang H, Tian P. The effect of obesity on clinical outcomes after minimally invasive surgery of the spine: A systematic review and meta-analysis. World Neurosurg 2018;110:e438-e449. [Google Scholar] |
| 17. | Xie L, Wu WJ, Liang Y. Comparison between minimally invasive transforaminal lumbar interbody fusion and conventional open transforaminal lumbar interbody fusion: An updated meta-analysis. Chin Med J (Engl) 2016;129:1969-86. [Google Scholar] |
| 18. | Algarni AS, Ghorbel S, Jones JG, Guermazi M. Validation of an arabic version of the oswestry index in Saudi Arabia. Ann Phys Rehabil Med 2014;57:653-63. [Google Scholar] |
| 19. | Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: Techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 2015;1:2-18. [Google Scholar] |
| 20. | Alamin T, Mitchell H, Kim C, Kim K, Fox B, Taylor W, et al. Preliminary results of a multicenter randomized study to evaluate the effect of minimally invasive vs. open lumbar fusion on paraspinal musculature using MR imaging. Spine J 2008;8:85-95. [Google Scholar] |
| 21. | Virdee JS, Nadig A, Anagnostopoulos G, George KJ. Comparison of peri-operative and 12-month lifestyle outcomes in minimally invasive transforaminal lumbar interbody fusion versus conventional lumbar fusion. Br J Neurosurg 2017;31:167-71. [Google Scholar] |
| 22. | Serban D, Calina N, Tender G. Standard versus minimally invasive transforaminal lumbar interbody fusion: A prospective randomized study. Biomed Res Int 2017;2017:7236970. [Google Scholar] |
| 23. | Zhang W, Li X, Shang X, Xu X, Hu Y, He R, et al. Modified minimally invasive transforaminal lumbar interbody fusion using a trans-multifidus approach: A safe and effective alternative to open-TLIF. J Orthop Surg Res 2015;10:93. [Google Scholar] |
| 24. | Sulaiman WA, Singh M. Minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis grades 1-2: Patient-reported clinical outcomes and cost-utility analysis. Ochsner J 2014;14:32-7. [Google Scholar] |
| 25. | Rosen DS, Ferguson SD, Ogden AT, Huo D, Fessler RG. Obesity and self-reported outcome after minimally invasive lumbar spinal fusion surgery. Neurosurgery 2008;63:956-60. [Google Scholar] |
| 26. | Hung PI, Chang MC, Chou PH, Lin HH, Wang ST, Liu CL. Is a drain tube necessary for minimally invasive lumbar spine fusion surgery? Eur Spine J 2017;26:733-7. [Google Scholar] |
| 27. | Wong AP, Smith ZA, Stadler JA 3rd, Hu XY, Yan JZ, Li XF, et al. Minimally invasive transforaminal lumbar interbody fusion (MI-TLIF): Surgical technique, long-term 4-year prospective outcomes, and complications compared with an open TLIF cohort. Neurosurg Clin N Am 2014;25:279-304. [Google Scholar] |
| 28. | Kulkarni AG, Bohra H, Dhruv A, Sarraf A, Bassi A, Patil VM. Minimal invasive transforaminal lumbar interbody fusion versus open transforaminal lumbar interbody fusion. Indian J Orthop 2016;50:464-72. [Google Scholar] |
Fulltext Views
2,314
PDF downloads
581





