Translate this page into:
Managing severe flexion deformity of the lower femur in a young child
2 Medical Interns, Faculty of Medicine, AlMaarefa University, Riyadh, Saudi Arabia
Corresponding Author:
Mayas W Sabhan
Dallah Hospital, Riyadh
Saudi Arabia
mayyas.08@gmail.com
| How to cite this article: Kremli MK, Elrafi AK, Zainab MM, Sabhan MW. Managing severe flexion deformity of the lower femur in a young child. J Musculoskelet Surg Res 2020;4:109-112 |
Abstract
A severe flexion deformity of the knee that prevented a 2-year-old-child from walking caused by a 90° flexion of the lower right femur is presented. It was managed surgically by a large closed-trapezoid wedge extension-shortening osteotomy resulting in gaining the ability to walk. This case report represents a dilemma of diagnosis and management and discusses a well-planned trapezoid excision shortening osteotomy to save the neurovascular structures.Introduction
Fixed flexion deformities of the femur in young children could be due to multiple causes. Osteomyelitis of the lower femur may cause a deformity by either affecting the growth plate or causing a pathological fracture that may cause deformity of the lower femur. Fractures and epiphyseal plate injuries are also possible causes of deformity of the lower femur,[1] usually with a clear history of trauma, or as part of a nonaccidental injury. Congenital pseudoarthrosis of the femur may present with sclerosis and deformity as well. However, it usually affects the proximal femur and has been only reported once in the femoral shaft,[2] but never in the distal femur. Progressive knee flexion deformity may be caused by spasticity as in cerebral palsy, but the deformity is caused by soft-tissue shortening, with hardly any bony morphological changes. The history of perinatal hypoxia with other features of spasticity was clinically evident. Osteogenesis imperfecta may cause distal femoral flexion deformity,[3] but usually presents with multiple fractures and widespread osteopenia. Arthrogryposis may present with knee fixed flexion deformity, but it usually affects multiple joints. Congenital conditions would clearly present immediately after birth and would be again clinically evident. This case report represents a dilemma of diagnosis and management and discusses a well-planned trapezoid excision-shortening osteotomy to save the neurovascular structures, without the need to advance the patellar tendon.
Case Report
A 14-month-old male, who is a product of normal full-term pregnancy, and cesarean section delivery, presented to the clinic with an inability to straighten the right knee. There was no history of trauma, pain, fever, swelling, or redness.
The problem started as acute flaccid pseudoparalysis of the right lower limb at 10 days of age without fever. He was admitted to the neonatal intensive care unit and received empirical antibiotics. Blood investigations including a complete blood count (CBC), and erythrocyte sedimentation rate (ESR) was normal, and a radiograph of the right lower limb was inconclusive at the time. A needle bone marrow aspiration from the lower femur was normal. Two weeks later, he had an open biopsy and curettage at the lower femur, but a definitive diagnosis could not be reached. He started slowly to regain movement but could not straighten his knee.
The child had normal developmental milestones but could not walk because of the severe flexion deformity at his right knee. The child was not known to have any other medical condition and he is not on medications, and the family history was unremarkable.
When seen at the age of 14 months, the child was healthy and afebrile. He could stand with support on the left foot and had a 90° fixed flexion deformity of the right knee. There was no swelling, redness, or tenderness. The knee flexion ranged from 90° to full flexion, and the hamstrings were tight [Figure - 1]. Trunk, upper limbs and left lower limb were all normal.
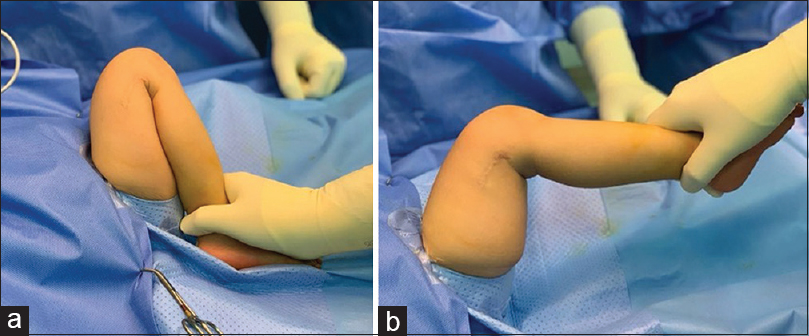 |
| Figure 1: (a and b) On presentation, a 90° fixed flexion deformity of the knee |
Basic blood investigations, including CBC, ESR, C-reactive protein, urea, and electrolytes, were all normal. The radiograph of the right lower limb showed a 90° flexion deformity of the distal femur just above the epiphyseal plate with areas of medullary sclerosis and sclerotic new bone formation at the posterior aspect of the lower femur [Figure - 2]. A skeletal survey was not performed as clinically the right lower limb was the only region showing pathology.
 |
| Figure 2: A lateral radiograph of the right femur showing sclerosis and severe flexion of the lower femur with posterior sclerotic bone formation |
A computerized tomography scan of the right lower limb confirmed the same findings of sclerosis, almost obliterating the medullary cavity of the lower femur with a posterior new sclerotic bone formation that seemed to be coming from the lower femur. The epiphyseal plate did not seem to be affected [Figure - 3].
 |
| Figure 3: (a and b) The computerized tomography scan shows the deformity of the lower femur and bone sclerosis extending into the distal diaphysis |
As the deformity was severe and resulted in an inability to walk, and with no clinical, laboratory, or radiographic signs of active infection, or tumor growth over a follow-up period of 8 months, it was decided to correct the deformity surgically.
Surgical technique
After thorough planning, the decision was to perform a large trapezoid-shaped excision of the entire pathological sclerotic segment with cuts perpendicular to the long axes of the upper and distal femur – at a right angle to each other – to straighten the bone fully [Figure - 4]. Although this would cause shortening of the femur, it will result in immediate full correction and spare the neurovascular bundle from overstretching. Surgery was performed at the age of 2 years. Through a lateral incision, the trapezoid segment of the deformed lower femur was excised carefully after it was released from adhesions to the quadriceps anteriorly and hamstrings posteriorly. Cutting was very difficult because of severely sclerotic bone [Figure - 5]. The completely obliterated sclerotic medullary cavity of the distal end of the proximal femoral segment was drilled to enhance blood supply and healing. A correction was fully achieved without overstretching the neurovascular bundle and soft-tissue release of hamstrings proved unnecessary intraoperatively. Fixation was achieved with three Kirschner wires, and a hip spica cast was applied. The patient had an uneventful postoperative recovery, and the culture and sensitivity from the excised segment were negative. The histopathology report showed nonspecific bone sclerosis. The postoperative radiographs showed a good correction. On follow-up, 3 months postoperatively, the child was walking very well with a shortening of 3.5 cm, and the knee range of motion was 10°–110° [Figure - 6]. The radiographs showed good healing [Figure - 7]. A 2-cm shoe raise was prescribed.
 |
| Figure 4: The preoperative planning of the trapezoid excision extension shortening osteotomy. The solid lines represent the bone cuts, which are drawn perpendicular to the corresponding long axes (dotted lines) to result in full correction of the angulation |
 |
| Figure 5: (a) The excised bone segment, the Kirschner wire represents the lower femur, and the ruler represents the upper femur. (b) Sclerosis of the proximal cut end totally obliterating the medullary cavity |
 |
| Figure 6: The knee almost fully extended at 3 months postoperatively |
 |
| Figure 7: (a and b) Follow-up anteroposterior and lateral radiographs at 3 months postoperatively |
Long term follow-up is definitely required to assess growth and length of the femur and possibly an operative intervention by lengthening or epiphysiodesis of the contralateral side may be needed in the future.
Discussion
What clinically appeared a severe knee fixed flexion deformity in this young child that prevented walking was not a joint deformity but a 90° bony flexion deformity of the lower femur. This is one of the most severe-angled bone deformities in the lower femur in children of this age. Osteomyelitis was probably the cause presenting at the neonatal period with pseudoparalysis with no clear constitutional manifestations of infection. This has probably caused a pathological fracture of the lower femur that has deformed into sever flexion deformity.
The challenge, in this case, was to correct this rare and severe 90° deformity without overstretching and compromising the posterior structures, particularly the neurovascular bundle.[4],[5] Femoral shortening by excising a large trapezoid-shaped piece of the sclerotic segment achieved full correction and spared the neurovascular bundle from overstretching, as has been stressed in the literature.[6],[7] In our case, the risk was very high as the deformity was severe, especially with the presence of bone sclerosis posterior to the lower femur and fibrosis of soft tissues posteriorly. Furthermore, femoral shortening relaxed the hamstrings and other soft tissues, so that the need for soft-tissue release was minimal. Closed wedge extension and shortening osteotomies have been reported in older children with cerebral palsy or arthrogryposis to overcome a fixed knee flexion gait. However, these were small wedges or small trapezoid excisions correcting deformities of up to 40°, much less than the one we report here.[8],[9],[10],[11] Classically, these operations are followed immediately by patellar tendon advancement to address the “Quadriceps s laxity” created by extension osteotomy (with or without) shortening. In our case, although the angle corrected was 90°, we opted not to perform patellar tendon advancement as the child was too young (2 years old) at the time of surgery. This proved to be correct as the child regained walking with a good quadriceps function 3 months postoperatively. Ilizarov instrumentation has been used to gradually correct the knee deformities of ≥40° in older children[12] but our case was probably too young for this, and the correction needed was much more.
In conclusion, this severe flexion deformity of the lower femur that prevented walking was most probably a sequelae of neonatal osteomyelitis. A carefully planned femoral shortening by excising a large trapezoid-shaped sclerotic segment achieved full correction and spared the neurovascular bundle from overstretching. The resultant shortening should be followed up and dealt with later on.
Ethical consideration
Consent was obtained from the parents to use the radiographs and clinical photographs of the patient's limbs. The parents understand that his name and initials will not be published, and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Acknowledgment
We acknowledge the help and support provided by Dr. Fikri Abdulfattah in gathering information from the case notes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
MK conceived and designed the study and managed the case. All authors participated equally in writing the initial and final draft of the article and providing logistic support and literature reviews. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Fragomen AT, Fragomen FR. Distal femoral flexion deformity from growth disturbance treated with a two-level osteotomy and internal lengthening nail. Strategies Trauma Limb Reconstr 2017;12:159-67. [Google Scholar] |
| 2. | Al-Hathal MM, Al-Tawil KI, Ghaffar TA, Almohrij S, Ahmed GS, Al Summan AA. Primary congenital pseudoarthrosis of the femur. Ann Saudi Med 2000;20:291-3. [Google Scholar] |
| 3. | EL-Sobky TA, Shawky RM, Sakr H, Elsayed SM, Elsayed NS, Ragheb SG, et al. A systematized approach to radiographic assessment of commonly seen genetic bone diseases in children: A pictorial review. J Musculoskelet Surg Res 2017;2:25-32. [Google Scholar] |
| 4. | İnan M, Sarikaya İA, Yildirim E, Güven MF. Neurological complications after supracondylar femoral osteotomy in cerebral palsy. J Pediatr Orthop 2015;35:290-5. [Google Scholar] |
| 5. | Pontén E. Management of the knees in arthrogryposis. J Child Orthop 2015;9:465-72. [Google Scholar] |
| 6. | Ibrahim B, Mamuda A, Taura M, Adamu L. Management of severe knee flexion contractures in a child with arthrogryposis multiplex congenita. Int J Surg Med 2015;1:76-9. [Google Scholar] |
| 7. | Mulevanova SA, Agranovich OE. Treatment of flexion contracture of the knee joint in children with arthrogryposis: A literature review. Pediatric Traumatol Orthop Reconstr Surg 2016;4:54-60. [Google Scholar] |
| 8. | DelBello DA, Watts HG. Distal femoral extension osteotomy for knee flexion contracture in patients with arthrogryposis. J Pediatr Orthop 1996;16:122-6. [Google Scholar] |
| 9. | Park H, Park BK, Park KB, Abdel-Baki SW, Rhee I, Kim CW, et al. Distal femoral shortening osteotomy for severe knee flexion contracture and crouch gait in cerebral palsy. J Clin Med 2019;8. pii: E1354. [Google Scholar] |
| 10. | Klotz MC, Hirsch K, Heitzmann D, Maier MW, Hagmann S, Dreher T. Distal femoral extension and shortening osteotomy as a part of multilevel surgery in children with cerebral palsy. World J Pediatr 2017;13:353-9. [Google Scholar] |
| 11. | Novacheck TF, Stout JL, Gage JR, Schwartz MH. Distal femoral extension osteotomy and patellar tendon advancement to treat persistent crouch gait in cerebral palsy. Surgical technique. J Bone Joint Surg Am 2009;91 Suppl 2:271-86. [Google Scholar] |
| 12. | van Bosse HJ, Feldman DS, Anavian J, Sala DA. Treatment of knee flexion contractures in patients with arthrogryposis. J Pediatr Orthop 2007;27:930-7. [Google Scholar] |
Fulltext Views
3,711
PDF downloads
1,738





