Translate this page into:
Indications of blood transfusion following total knee replacement at a tertiary care center in central Saudi Arabia
2 Department of Family Medicine, King Fahad Medical City, Riyadh, Saudi Arabia
3 Department of Otorhinolaryngology Head and Neck surgery, King Fahad Armed Forces Hospital, Jeddah, Saudi Arabia
4 College of Medicine, Princess Nora University, Riyadh, Saudi Arabia
5 Department of Population Health, King Abdullah International Medical Research Center, Riyadh, Saudi Arabia
Corresponding Author:
Ali A Alhandi
Department of Surgery, Division of Orthopedic Surgery, King Abdulaziz Medical City Riyadh, National Guard Health Affairs, Post Box 22490, Riyadh 11426
Saudi Arabia
ali.alhandi@gmail.com
| How to cite this article: Alturki AA, Algufaili RS, Alnefaie MN, Almojel SA, Alghnam S, Alhandi AA. Indications of blood transfusion following total knee replacement at a tertiary care center in central Saudi Arabia. J Musculoskelet Surg Res 2020;4:132-135 |
Abstract
Objectives: Total knee replacement (TKR) is an increasingly common procedure worldwide with a continued projected increase in the future. Blood loss following TKR can be relatively high. Globally, the incidence rate of blood transfusion (BT) following TKR has been reported to range between 8% and 18%, whereas a higher estimate reported locally (35%). This study aims to review the indications leading to BT following TKR in a single center. Methods: This is a retrospective study of patients who had BT following primary TKR (171 patients) at a single tertiary center between 2012 and 2016. Patients were categorized into “transfusion indicated” and “transfusion not indicated” groups. Cases were considered indicated if their hemoglobin (Hb) level was ≤8 g/dL, or if there was a drop accompanied by the clinical findings. Patient's demographics, comorbidities, surgery-related data, laboratory findings, blood loss, number of blood units transfused, and their complications were compared between the two groups. Results: Of the study sample, 50 (29.24%) patients were classified as cases without a clear indication for BT. Postoperative Hb was significantly higher in the nonindicated transfusion group (Hb nonindicated 8.54 g/dL, Hb indicated 7.74 g/dL, P < 0.001). Similarly, the body mass index (BMI) was significantly higher in the nonindicated group (BMI nonindicated 35.54, BMI indicated 32.49, P = 0.0123). Conclusion: The number of cases with no clear indication for BT following TKR remains relatively high, enforcing hospital-based policies that require the documentation of rationale for BT might help reduce transfusions with no clear reasoning behind them.
Introduction
Total knee replacement (TKR) is a common surgical procedure, mostly indicated for treating end-stage arthritis of the knee joint.[1] TKR is increasingly common in the United States as in 2010, more than half a million underwent TKR surgery. Moreover, the prevalence has increased from 31 to 62 per 10,000 Medicare enrollees annually, and this is expected to increase in the future.[2],[3]
Certain complications are associated with TKR, such as bleeding, wound complication, thromboembolic disease, and deep joint infection.[4] Postoperative blood loss following TKR can be relatively high; in some cases, the loss may reach quantities ≥1.5 L (about 30% of the circulating blood volume), which could lead to acute anemia postoperatively.[1],[5]
Globally, the incidence rate of blood transfusion (BT) following TKR has been reported to range between 8% and 18%, with a higher estimate found in Saudi Arabia, 35%.[6],[7],[8],[9],[10],[11] Nevertheless, BT is not a riskless therapeutic procedure, as it is associated with possible serious complications such as the transmission of infectious diseases such as HIV and hepatitis, transfusion-related acute lung injury, hemolytic reactions, fluid overload, and an increased rate of postoperative infection.[12]
In a study by Hart et al. that reported complications of BT following TKR, they found that the odds of mortality were higher among patients who received a transfusion during TKR.[6] In another study by Jonas et al., the only surgical factor that influenced the length of stay was postoperative BT following TKR surgery (P< 0.0001).[13] In addition, BT is an expensive procedure, as revealed by a multicenter study in the United States that calculated the average cost per patient to be $219.[13]
There is a myriad of preventative measures that could reduce the need for BT, either pharmacological or simple practice modification methods, that would avoid unnecessary BT. Although BT following TKR is needed for some patients, inappropriate use may subject patients to unnecessary harm.[14] A recent local study noted a higher percentage of BTs post-TKR compared to the international average; this prompted the authors to further investigate if all BT s given were indicated.[11] This study aims to offer insight into the current local practices in relation to BT and TKR.
Materials and Methods
After proper institutional board review approval, a retrospective study was conducted through data gathered from the medical files of all the patients who had BT following primary TKR surgery done by any of the four arthroplasty surgeons (171 patients) at a single tertiary care center. Data collection included adults (age ≥18 years) who met the above criteria between the period 2012 and 2016. Those with a history of any type of anemia, coagulation disease, or liver disease were excluded from the study.
BT was considered “indicated” if the hemoglobin (Hb) level was ≤ 8 g/L, or if there was a serious sign or symptom of blood loss such as pallor, tachycardia, hypotension, decreased mental status, drowsiness, and poor urine output.[15]
Patient's demographic information (i.e., age in years at the time of surgery, gender, and body mass index [BMI]), comorbidities (i.e., heart diseases, hypertension, diabetes mellitus, and dyslipidemia), documentation from physicians and laboratory data findings (i.e., pre and postoperative Hb levels), amount of blood loss (i.e., intraoperative and postoperative), number of units transfused during the hospital stay, and whether the TKR was bilateral or unilateral, were reviewed for each medical record.
Data abstracted from the medical records were collected and then analyzed using SAS software (SAS Institute Inc., version 9.2 (2008), Cary, NC, USA). Single surgeon analysis was done before the final analysis to exclude any data bias toward one surgeon over the other. After ensuring normal sample variation between surgeons, total sample variables were summarized and reported across the study using descriptive statistics. Continuous variables such as Hb level and amount of blood loss were summarized in terms of the mean and standard deviation, whereas the categorical variables, such as comorbidities, gender, and whether the surgery was unilateral or bilateral, were summarized and reported in terms of the frequency distribution. Group comparison was conducted using Chi-square test for binary variables and Student's t-test for continuous variables. The difference was considered statistically significant when P < 0.05.
Results
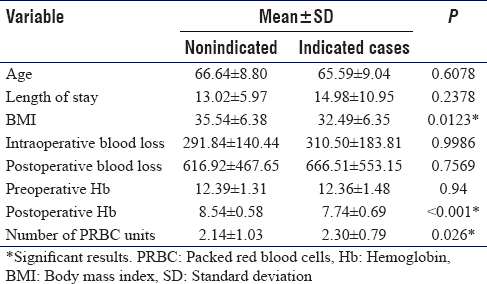
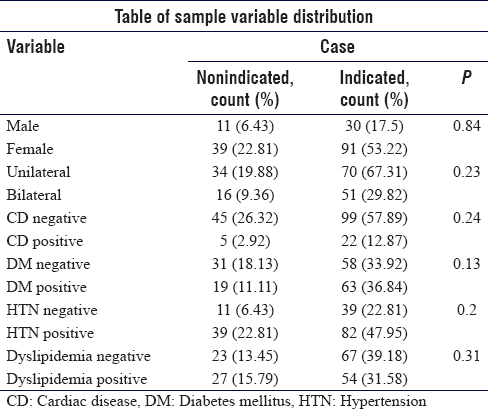
The sample included 171 patients, 41 (24%) males, and 130 (76.0%) females. Patients with no clear indication for BT were 50 (29.2%), whereas the indicated cases were 121 (70.8%), as shown in [Figure - 1]. The age average for the indicated group was 65.5 ± 9.04, and the nonindicated group had an average age of 66.64 ± 8.80, with no statistically significant difference (P = 0.61). The BMI was significantly lower in the BT indicated group when compared to the nonindicated group (32.49 ± 6.35 versus 35.54 ± 6.38, respectively), P = 0.01.
 |
| Figure 1: Number of cases transfused per year (2012–2016) |
The mean preoperative Hb showed no statistically significant difference between the two groups, whereas postoperative Hb was significantly higher in the nonindicated group (P = 0.94 and P < 0.001, respectively). The mean intra- and postoperative blood loss showed no significant difference between the two groups (P = 0.99 and P = 0.76, respectively). The mean number of blood units transfused, however, was significantly higher in the indicated group, P = 0.026. Continuous variables' summary is shown in [Table - 1]. Other comorbidities and dichotomous variables showed no significant differences between the two groups [Table - 2].
Discussion
The need for BT following major surgeries, including TKR, is a concern for the surgeons, anesthetists, and patients. Although BT is a life-saving intervention for many patients undergoing major surgeries, postoperative low Hb level was noted to be associated with high morbidity and mortality rates.[16],[17]
Patients who receive BT postoperatively had significantly increased hazard of 30-day death (hazard ratio 11.72), especially patients without postoperative anemia, according to Bursi et al.'s study.[18] Furthermore, BT is an expensive procedure. Klika et al.'s study showed an 18% increase in cost per admission for a patient who received BT following TKR.[7]
A local study estimated that 13% of adults have knee osteoarthritis, and many of them may need to have TKR performed.[19] In addition, a previous study carried out in the same center[11] showed a 50% higher incidence of BT rate following TKR in comparison to published literature.[7],[8],[9],[10] The findings of the present study suggested that BT may be overused, as 29.2% of patients who underwent TKR and received BT had no clear indication for BT. Moreover, blood availability for BT is scarce and costly. In this study, 107 units were transfused despite not having a clear indication for BT. Furthermore, there was a statistically measurable difference in the postoperative Hb mean between the two groups with no clear difference in the preoperative Hb mean. This may translate into approximately $51,815 of avoidable costs in the sample over the study period, which might be reduced with clearly defined indications for BT. Moreover, the availability of blood for patients remains a challenge with little published locally about the matter. A recent study by Badawi reviewed some of the known issues that face the system with procuring ample amounts of blood units for transfusion with the main highlighted problem being the institution-based model used in blood collection.[20]
BMI was significantly lower in patients with a clear indication for BT as defined by this study, although both groups were found to have an average BMI of more than 30 and such, no conclusions could be drawn in relation to BMI.
Most of the available literature studied the predictors for BT following TKR by including patients who underwent BT and patients who did not. Carling et al. showed that low preoperative Hb, low BMI, and long operation time were significant predictors of BT following TKR.[10] Hart et al. identified female gender, age, BMI of <30 kg/m2, and preoperative low Hb level as high indicators for BT following TKR.[6] Al-Turki et al. found in a study done in the same institution that low preoperative Hb levels, high amount of blood loss (peri/postoperatively), bilateral surgery, high American Society of Anesthesiologists score, and general anesthesia were significant predictors of BT following TKR.[11]
The lack of proper documentation to explain why the patient received BT in detail is a weakness that can be attributed to the retrospective nature of the study design. However, the study offers a unique perspective on patients who underwent a BT following TKR by assessing clearly defined indications. The study noted that approximately 30% of the sample had no clear reason for receiving a BT. This is further solidified by higher postoperative mean Hb in the nonindicated group and the lack of other statistically significant differences.
Conclusion
The number of cases with no clear indication for BT following TKR was found to be relatively high at approximately 30%. The authors recommend starting clear hospital-based policies for BT, especially in nonemergency situations, that require documentation of rationale for transfusion; this may help in mitigating transfusions where the clinical reasoning is not clear.
Ethical consideration
An Institutional Review Board approval was obtained by the King Abdullah International Medical Research Center, Ministry of National Guard Health Affairs, Riyadh, Saudi Arabia.
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
AAT conceived and designed the study, conducted research, and provided research materials. RSA, MNA, and SAA collected and organized data, wrote the initial draft of the article, and provided logistic support. SA was involved in the study design data analysis. AAA was involved in data interpretation, wrote the final draft of the article, and provided logistic support. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Tavares Cardozo R, Fidelis de Souza Junior E, Campoli Alves W, Barbi Filho F. Total knee arthroplasty: Indication of blood transfusion according to hematimetric variation and clinical symptoms of hypoperfusion. Rev Bras Ortop 2014;49:507-12. [Google Scholar] |
| 2. | HCPUnet, Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality; 2012. [Google Scholar] |
| 3. | Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-5. [Google Scholar] |
| 4. | Healy WL, Della Valle CJ, Iorio R, Berend KR, Cushner FD, Dalury DF, et al. Complications of total knee arthroplasty: Standardized list and definitions of the Knee Society. Clin Orthop Relat Res 2013;471:215-20. [Google Scholar] |
| 5. | Clarke AM, Dorman T, Bell MJ. Blood loss and transfusion requirements in total joint arthroplasty. Ann R Coll Surg Engl 1992;74:360-3. [Google Scholar] |
| 6. | Hart A, Khalil JA, Carli A, Huk O, Zukor D, Antoniou J. Blood transfusion in primary total hip and knee arthroplasty. Incidence, risk factors, and thirty-day complication rates. J Bone Joint Surg Am 2014;96:1945-51. [Google Scholar] |
| 7. | Klika AK, Small TJ, Saleh A, Szubski CR, Chandran Pillai AL, Barsoum WK. Primary total knee arthroplasty allogenic transfusion trends, length of stay, and complications: Nationwide inpatient sample 2000-2009. J Arthroplasty 2014;29:2070-7. [Google Scholar] |
| 8. | Yamaguchi S, Ohno G, Kitamura J. Evaluation of perioperative blood loss and transfusion in total knee arthroplasty. Masui 2014;63:1029-33. [Google Scholar] |
| 9. | Park JH, Rasouli MR, Mortazavi SM, Tokarski AT, Maltenfort MG, Parvizi J. Predictors of perioperative blood loss in total joint arthroplasty. J Bone Joint Surg Am 2013;95:1777-83. [Google Scholar] |
| 10. | Carling MS, Jeppsson A, Eriksson BI, Brisby H. Transfusions and blood loss in total hip and knee arthroplasty: A prospective observational study. J Orthop Surg Res 2015;10:48. [Google Scholar] |
| 11. | Al-Turki AA, Al-Araifi AK, Badakhan BA, Al-Nazzawi MT, Alghnam S, Al-Turki AS. Predictors of blood transfusion following total knee replacement at a tertiary care center in Central Saudi Arabia. Saudi Med J 2017;38:598-603. [Google Scholar] |
| 12. | Haien Z, Yong J, Baoan M, Mingjun G, Qingyu F. Post-operative auto-transfusion in total hip or knee arthroplasty: A meta-analysis of randomized controlled trials. PLoS One 2013;8:E55073. [Google Scholar] |
| 13. | Jonas SC, Smith HK, Blair PS, Dacombe P, Weale AE. Factors influencing length of stay following primary total knee replacement in a UK specialist orthopaedic centre. Knee 2013;20:310-5. [Google Scholar] |
| 14. | Forbes JM, Anderson MD, Anderson GF, Bleecker GC, Rossi EC, Moss GS. Blood transfusion costs: A multicenter study. Transfusion 1991;31:318-23. [Google Scholar] |
| 15. | Liumbruno GM, Bennardello F, Lattanzio A, Piccoli P, Rossetti G; Italian Society of Transfusion Medicine and Immunohaematology Working Party. Recommendations for the transfusion management of patients in the peri-operative period. III. The post-operative period. Blood Transfus 2011;9:320-35. [Google Scholar] |
| 16. | Hadjianastassiou VG, Virich G, Lennox IA. Transfusion practice in primary unilateral total knee replacement arthroplasty; the need for guidelines. Ann Chir Gynaecol 2001;90:23-7. [Google Scholar] |
| 17. | Carson JL, Noveck H, Berlin JA, Gould SA. Mortality and morbidity in patients with very low postoperative Hb levels who decline blood transfusion. Transfusion 2002;42:812-8. [Google Scholar] |
| 18. | Bursi F, Barbieri A, Politi L, Di Girolamo A, Malagoli A, Grimaldi T, et al. Perioperative red blood cell transfusion and outcome in stable patients after elective major vascular surgery. Eur J Vasc Endovasc Surg 2009;37:311-8. [Google Scholar] |
| 19. | Al-Arfaj AS, Alballa SR, Al-Saleh SS, Al-Dalaan AM, Bahabry SA, Mousa MA, et al. Knee osteoarthritis in Al-Qaseem, Saudi Arabia. Saudi Med J 2003;24:291-3. [Google Scholar] |
| 20. | Badawi MA. Building a blood system: The view from Saudi Arabia. ISBT Sci Series 2019;14:119-22. [Google Scholar] |
Fulltext Views
3,334
PDF downloads
1,343





