Translate this page into:
Evaluation of surgical site infections and their incidence in patients after total knee arthroplasty at a tertiary care hospital in Riyadh, Saudi Arabia
2 College of Medicine, King Saud Bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
3 Department of Surgery, Division of Orthopedic Surgery, National Guard Health Affairs, King Abdulaziz Medical City, Riyadh, Saudi Arabia
4 College of Medicine, King Saud Bin Abdulaziz University for Health Sciences; Population Health Research Section, King Abdullah International Medical Research Center, Riyadh, Saudi Arabia
Corresponding Author:
Karam M Basham
King Saud Bin Abdulaziz University for Health Sciences, Al Hars Al Watani, Ar Rimayah, Riyadh 14611
Saudi Arabia
Kbasaham@gmail.com
| How to cite this article: Alsheikh KA, Basham KM, Alazaz RN, Alsulaiman FM, Alrasheed AT, Benmeakel MA, Almubarak AK, Alhandi AA. Evaluation of surgical site infections and their incidence in patients after total knee arthroplasty at a tertiary care hospital in Riyadh, Saudi Arabia. J Musculoskelet Surg Res 2020;4:152-155 |
Abstract
Objectives: Superficial surgical site infections (SSI) are a well-documented complication after total knee arthroplasty (TKA). The main objective of this research was to investigate the incidence of SSIs in patients who underwent a TKA and whether it is correlated with comorbidities, length of stay, and postoperative care. This will provide valuable insight into local infection rates as there is a lack of literature in this area. Methods: This is a retrospective chart review at a tertiary care hospital in Riyadh, Saudi Arabia. All patients from January 2016 to December 2018 undergoing TKA were included. We excluded patients with a history of infection, Tumor, or cases where surgical intervention was needed due to deeper infection. Data were collected for patients' demographic variables, length of hospital stay, comorbidities, site of infection, and then assessed whether it affects the rate of SSI in TKA. Results: A total of 735 had TKA. Of these, 558 patients (75.9%) were females . The most prevalent comorbidity was obesity (80.3%), followed by hypertension (63.3%). A rate of 1.5% (11 cases) of SSIs was found with no correlation to the length of hospital stay, comorbidities, and site of infection. Methicillin-sensitive Staphylococcus aureus and methicillin-resistant S. aureus were the most common organisms found in cultures. Conclusion: This study shows comparable incidence rates of SSIs following TKA to the published literature. It provides important regional data about the rate of SSIs, common organisms, and patient variables to aid future research.
Introduction
Total knee arthroplasty (TKA) is still considered after many years a significant advancement in orthopedic surgery, achieving high rates of patient satisfaction.[1] The goal of the surgery is to reconstruct damaged knees by repairing mobility and decreasing pain caused by different types of arthritis such as rheumatoid arthritis, degenerative osteoarthritis, and posttraumatic osteoarthritis.[2] The number of knee arthroplasty surgeries is increasing with the aging population worldwide.[3] It also showed a significant increase in prevalence over time and a shift to younger ages.[4] An estimated number of 3.0 million women and 1.7 million men had undergone TKA in the US in 2010, indicating a higher prevalence in females.[5] Another US study expected that by 2050, 6 million people would have TKA.[6]
Similar to other major surgeries, TKA comes with risks and complications, surgical site infection (SSI) is one of the main complications.[7] A study by Babkin et al. in 2007 included 180 patients who underwent TKA showed that 5.6% developed superficial or deep SSIs.[8] Another study by Carroll and Camins had an annual rate of SSI after TKA that ranged from 0.3% to 1.6% over 10 years from 2001 to 2011.[9] The most common organisms found in SSIs after TKA surgery have been studied as well. Berríos-Torres et al. conducted a study between 2006 and 2009 that showed methicillin-sensitive Staphylococcus aureus (MSSA) representing 23% of 6,263 cases, followed by methicillin-resistant S. aureus (MRSA), which accounted for 18%, and coagulase-negative Staphylococci accounted for 17%.[10] This study reviewed the rates of SSIs in TKA surgery and whether comorbidities, length of stay, body mass index (BMI), and other variables affect the rate of SSI. This study is considered the first in the region, and such data would provide valuable insight into the local rate of SSI post-TKA.
Methods
This is a retrospective chart review study in a single tertiary center that included all patients who underwent TKA from January 2016 to December 2018. We included all patients who underwent primary TKA due to osteoarthritis and developed superficial SSI. The exclusion criteria included any patient with documented previous infection (superficial or deep) in the upper or lower limbs, patients with positive urine, blood or respiratory cultures, any tumor case, no follow up for at least 2 years, any patient using immunosuppressive medications or labeled as immunocompromised, and patients who developed deep or chronic infection that led to surgical intervention.
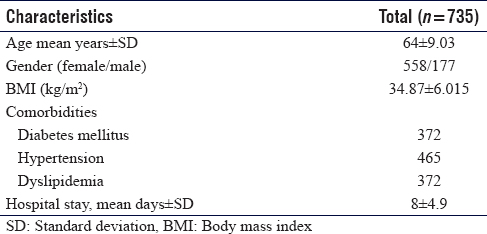
The data was collected by the co-investigators after obtaining approval from the institutional review board (IRB). The data were accessed and collected from the electronic medical records (Bestcare 2.0, ezCaretech, Seoul, Korea) of the patients. The data collection sheet included [Table - 1] the following variables (age, gender, BMI, comorbidities, site of knee arthroplasty, presence of an infection, site of infection, the organism causing SSI, drain volume and duration, time of primary dressing removal, duration of stay, and year of operation). The diagnosis of the infection was made by the findings of clinical examinations acutely (<3 weeks postoperatively) that included small superficial abscess, redness, swelling, or discharge, which was confirmed afterward by cultures obtained from a wound swab.
Data were entered using Excel and analyzed using STATA 14 (StataCorp. 2015. Stata Statistical Software: Release 14. StataCorp LP, College Station, TX, USA). Statistical summaries were viewed as frequencies and percentages to describe categorical variables and mean ± standard deviation (SD) was used for numerical variables (age, gender, BMI, comorbidities, site of knee arthroplasty, the presence of an infection, site of infection, the organism of SSI, drain volume and duration, time of primary dressing removal, duration of stay). Chi-square with Fisher's exact tests were used for categorical variables to assess associations between infections and the demographics and comorbidities between the two groups. The Student's t-test was utilized to test differences between the means of the two groups for numerical variables. The level of significance at alpha ≤0.05.
Results
A total of 735 surgeries were performed, 46% of those cases were left TKA, 40% were right TKA, while the remaining 14% were bilateral. Females represented 75.9% (558) of patients, and the mean age was 64 ± 9.3 SD. Obesity was the most prevalent comorbidity. According to the Centers for Disease Control and Prevention's classification,[11] 80.3% of the patients were obese. The other common comorbidities were hypertension (63.3%), dyslipidemia (50.6%), diabetes mellitus (50.6%). Detailed patients' characteristics are listed in [Table - 1].
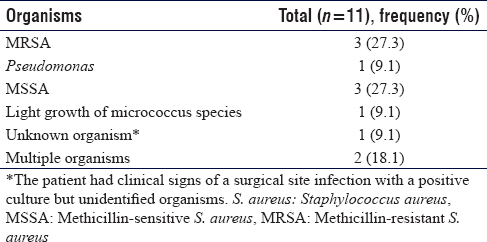
SSIs were found in 11 patients, and two of them had multiple organisms. Five organisms were identified; the most common were MRSA and MSSA, each affecting three patients [Table - 2]. These patients received an appropriate course of antibiotics based on the organisms found in their respective cultures [Table - 3]. None of the cases needed irrigation and debridement since deep infections were excluded from data collection.
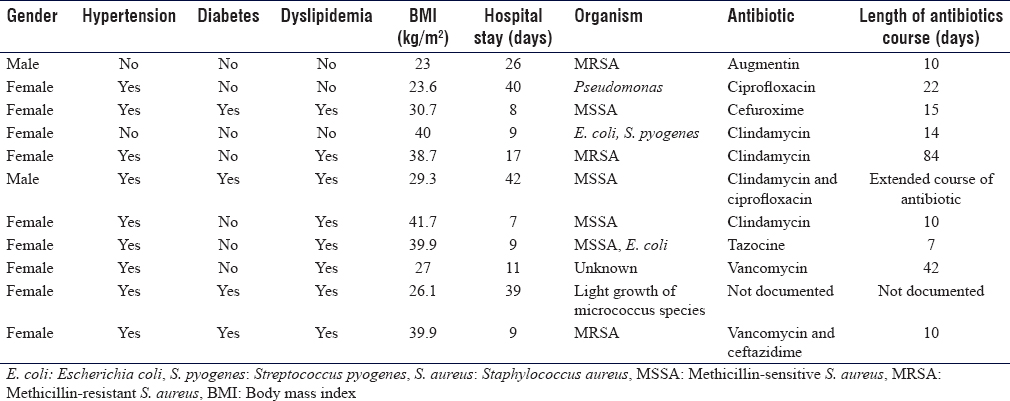
All patients had received preoperative cefazolin for prophylaxis, and postoperative prophylaxis was given for 1 or 3 days depending on each consultant's protocol, no differences in infection rates between protocols were noted. Clips for skin closure were used, and hemovac drain was on average put for 3 ± 1.6 days.
The mean total drain volume was 365 ml. The primary dressing was removed after 4 days on average, which is mostly a day after the drain's removal. The mean length of hospital stay after the surgery was 8 ± 4.9 days. All tested variables and comorbidities returned statistically insignificant correlations in Pearson's Chi-square test and Fisher's exact test. Appropriate mean testing was not possible due to the wide distribution discrepancy between the two groups (positive and negative infection).
Discussion
This study showed a comparable incidence of SSI when compared to international data (ranging from 0.1% to 5.5%).[12] In the United States, a nationwide study was conducted, including all patients who had undergone TKA between the years 1990 and 2004. The data were collected from the Nationwide Inpatient Sample (NIS) database and found an incidence of 0.9% SSI after TKA among 4,619,633 patients. There are many patient factors that could influence outcomes in arthroplasty that cannot be determined from the NIS data due to the fact that it is not intended to be a clinical data set.[13]
The different backgrounds of each culture and country may have an effect on medical practice, and the incidence infection, including SSI.[14] Ashraf et al.[15] studied the SSI rate among TKA patients in Pakistan and found 1.2% to be the incidence in one tertiary hospital. This may represent resemblance to this study and population; however, their sample size was relatively small in comparison (164 patients).
In a specialized hospital in Hannover, Baier et al. conducted a retrospective cohort study that included 2439 patients who underwent TKA between the years 2007 and 2010.[16] He found that the cumulative incidence of SSI was 3.4%, which is relatively high compared to the published literature. However, it decreased continuously over time, from 4.4% in 2007 to 2.5% in 2010. The analyzed independent risk factors showed results, in line with the published reports.
Looking at local data, a national surveillance has not yet been established. Moreover, local studies were focused more on involving all kinds of orthopedic surgeries. Al-Mulhim et al. found an SSI rate of 2.6% among 3096 patients over 5 years of analysis.[17] However, their results were calculated from emergency and elective orthopedic surgeries. Another study by Al-Kenani et al. showed a rate of 3.42% SSI following foot and ankle surgeries in 295 patients who underwent 353 surgeries.[18] However, comparisons to local data cannot be drawn to this study sample.
SSI rate is believed to have multiple factors, which can be categorized into the patient, surgical technique, and environmental factors.[19] Obesity was found to be high among this study sample; 96% of our patients had a BMI of >25, and 45% had BMI of >35. This was reflected in the results; a high percentage of patients who developed SSI were found to be obese (54% - as defined by BMI >30), although no clear statistical significance was noted. Obesity is still one of the most prevalent risk factors that have a primary influence on the rate of SSI among recipients of TKA. Questioning whether obesity is an independent factor to develop SSI in TKA can be affected by the fact that patients with high BMI are at greater risk of developing knee osteoarthritis, which is apparent among this study population (>96%). Recent data in 2018 by Wilson et al.[20] failed to show obesity (BMI >30) as an independent risk factor to develop SSI.
Most of the study subjects who developed SSI had 2 or more medical comorbidities (72%); including diabetes mellitus, hypertension, dyslipidemia, and cardiovascular disease. Kong et al.[21] conducted a meta-analysis studying the risk factors of SSI among TKA recipients; they included 15 studies from 1990 to 2015 and found that diabetes, obesity, and age have a measurable influence on the rate of infection. However, other comorbidities failed to be correlated.
SSI in the orthopedic reconstructive surgery literature has many conflicting data to consider whether bilateral TKA is an independent risk factor or not. Kong et al.,[21] in their meta-analysis, had two studies that failed to show higher statistically significant risk with bilateral surgery, with P value of 0.59. Among this study sample, only 18% of those who developed SSI, underwent bilateral surgery without any statistical significance. The authors attribute this to low number of positive cases of superficial SSI among in the sample, and as such, conclusions cannot be drawn from this study regarding comorbidities and their effect on SSI. Moreover, the organisms responsible for the infections may not be accurately represented since swabs from the wounds can give false-positive results of S. aureus from the skin flora. More limitations are noted, including the limited regional literature on SSIs post-TKA. In Addition, retrospective review of such patients was influenced by the different surgeons' style and preference.
Conclusion
This study showed a comparable incidence of SSIs to the published literature. The incidence of SSIs after TKA in this study was 1.5%, while international data showed incidence that ranged from 0.1% to 5.5%.[12] The authors believe that this study while failing to draw conclusions that identify the risk factors of developing SSI post-TKA, due to the small proportion of positive outcomes (SSIs); it reports an important incidence figure of SSI post-TKA in the region.
Recommendations
Regional efforts to accurately represent measurable surgical outcomes are currently lacking in the literature. This study affirms the need for future multi-central studies for a complete picture. Moreover, additional research should focus on approaches to prevent SSI after TKA surgeries.
Ethical approval
An IRB approval was obtained by King Abdullah International Medical Research Center, Ministry of National Guard Health Affairs, Riyadh, Saudi Arabia.
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
KAA study concept, study design, manuscript review. KMB study concepts, data collection, data interpretation, manuscript drafting. RNA study design, data collection, data interpretation, manuscript drafting. FMA study design, data collection, data interpretation, manuscript drafting. ATA study design, data collection, data interpretation, manuscript drafting. MABM literature search, data interpretation, manuscript drafting. AKA data preparation, statistical analysis, manuscript drafting. AAA study design, data review, data analysis, manuscript editing, manuscript review. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Aumiller WD, Dollahite HA. Advances in total knee arthroplasty. JAAPA 2016;29:27-31. [Google Scholar] |
| 2. | Medical Advisory Secretariat. Total knee replacement: An evidence-based analysis. Ont Health Technol Assess Ser 2005;5:1-51. [Google Scholar] |
| 3. | Çaǧla Karakoç Z, Haklar U. Zero surgical site infection in primary knee arthroplasty with multidisciplinary intervention: Is it possible? Infez Med 2018;26:15-21. [Google Scholar] |
| 4. | Losina E, Katz JN. Total knee arthroplasty on the rise in younger patients: Are we sure that past performance will guarantee future success? Arthritis Rheum 2012;64:339-41. [Google Scholar] |
| 5. | Maradit Kremers H, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am 2015;97:1386-97. [Google Scholar] |
| 6. | Inacio MC, Paxton EW, Graves SE, Namba RS, Nemes S. Projected increase in total knee arthroplasty in the United States – An alternative projection model. Osteoarthritis Cartilage 2017;25:1797-803. [Google Scholar] |
| 7. | Agodi A, Auxilia F, Barchitta M, Cristina ML, D'Alessandro D, Mura I, et al. Risk of surgical site infections following hip and knee arthroplasty: Results of the ISChIA-GISIO study. Ann Ig 2017;29:422-30. [Google Scholar] |
| 8. | Babkin Y, Raveh D, Lifschitz M, Itzchaki M, Wiener-Well Y, Kopuit P, et al. Incidence and risk factors for surgical infection after total knee replacement. Scand J Infect Dis 2007;39:890-5. [Google Scholar] |
| 9. | Carroll C, Camins B. Knee arthroplasty surgical site infection rates over a ten-year period at a community hospital. Am J Infect Control 2013;41:S112-3. [Google Scholar] |
| 10. | Berríos-Torres SI, Yi SH, Bratzler DW, Ma A, Mu Y, Zhu L, et al. Activity of commonly used antimicrobial prophylaxis regimens against pathogens causing coronary artery bypass graft and arthroplasty surgical site infections in the United States, 2006-2009. Infect Control Hosp Epidemiol 2014;35:231-9. [Google Scholar] |
| 11. | Defining Adult Overweight and Obesity. Centers for Disease Control and Prevention; 2017. Available from: https://www.cdc.gov/obesity/adult/defining.html. [Last accessed on 2020 Feb 25]. [Google Scholar] |
| 12. | European Centre for Disease Prevention and Control. Healthcare-associated infections: Surgical site infections. In: ECDC. Annual Epidemiological Report for 2017. Stockholm: ECDC; 2019. [Google Scholar] |
| 13. | Kurtz SM, Lau E, Schmier J, Ong KL, Zhao K, Parvizi J. Infection burden for hip and knee arthroplasty in the United States. J Arthroplasty 2008;23:984-91. [Google Scholar] |
| 14. | Fan Y, Wei Z, Wang W, Tan L, Jiang H, Tian L, et al. The incidence and distribution of surgical site infection in mainland China: A meta-analysis of 84 prospective observational studies. Sci Rep 2014;4:6783. [Google Scholar] |
| 15. | Ashraf I, Mohib Y, Hasan O, Malik A, Ahmad K, Noordin S. Surgical site infection surveillance following total knee arthroplasty: Tertiary care hospital experience. Ann Med Surg (Lond) 2018;31:14-6. [Google Scholar] |
| 16. | Baier C, Adelmund S, Schwab F, Lassahn C, Chaberny IF, Gossé F, et al. Incidence and risk factors of surgical site infection after total knee arthroplasty: Results of a retrospective cohort study. Am J Infect 2019;47:1270-2. [Google Scholar] |
| 17. | Al-Mulhim FA, Baragbah MA, Sadat-Ali M, Alomran AS, Azam MQ. Prevalence of surgical site infection in orthopedic surgery: A 5-year analysis. Int Surg 2014;99:264-8. [Google Scholar] |
| 18. | Al-Kenani NS, Alsultan AS, Alosfoor MA, Bahkali MI, Al-Mohrej OA. Incidence and predictors of surgical site infections following foot and ankle surgery. J Musculoskelet Surg Res 2017;1:6-9. [Google Scholar] |
| 19. | Carvalho RL, Campos CC, Franco LM, Rocha AM, Ercole FF. Incidence and risk factors for surgical site infection in general surgeries. Rev Lat Am Enfermagem 2017;25:e2848. [Google Scholar] |
| 20. | Wilson CJ, Georgiou KR, Oburu E, Theodoulou A, Deakin AH, Krishnan J. Surgical site infection in overweight and obese Total Knee Arthroplasty patients. J Orthop 2018;15:328-32. [Google Scholar] |
| 21. | Kong L, Cao J, Meng F, Shen Y. Incidence and risk factors for surgical site infection following total knee arthroplasty: A systematic review and meta-analysis. Int J Clin Exp Med 2016;9:20642-50. [Google Scholar] |
Fulltext Views
3,429
PDF downloads
769





