Translate this page into:
Progression and clinical implications of boutonniere deformity
*Corresponding author: Roberto Tedeschi, Department of Biomedical and Neuromotor Sciences, Alma Mater Studiorum, University of Bologna, Bologna, Italy. roberto.tedeschi2@unibo.i
-
Received: ,
Accepted: ,
How to cite this article: Boccolari P, Tedeschi R, Donati D. Progression and clinical implications of boutonniere deformity. J Musculoskelet Surg Res. 2024;8:317-8. doi: 10.25259/JMSR_120_2024
Dear Editor,
The boutonniere deformity is a complex condition characterized by flexion of the proximal interphalangeal joint (PIP) and hyperextension of the distal interphalangeal joint (DIP), primarily caused by damage to the central slip of the extensor tendon and subsequent involvement of other structures like the triangular ligament.[1] This letter aims to shed light on the intricate mechanisms and management strategies for boutonniere deformity, underscoring its complexity and the necessity for precise, individualized treatment plans to achieve optimal patient outcomes. The progression of the deformity is initiated by the central slip lesion, which disrupts the force moment necessary for PIP extension. However, the isolated central slip lesion alone is insufficient for boutonniere deformity development in the acute phase, as other structures such as the triangular ligament and interossei fibers initially prevent dorsal migration of the lateral bands [Figure 1]. Clinical presentation in the acute phase may include slight swelling and modest loss of extension in the PIP followed by the manifestation of the true deformity in subsequent weeks. The rupture of the central slip leads to increased tension on dorsal structures, predisposing to further failure of interossei fibers and the triangular ligament, resulting in volar subluxation of the lateral bands and the flexion paradox. Diagnosing a central slip lesion poses challenges, with various tests proposed over the years. Among these, Elson’s test[2] stands out for its focus on flexing the PIP to isolate the central slip function. The test helps reveal the anomaly between PIP and DIP mechanics, which is crucial for accurate diagnosis. Conservative treatment[3-5] Options include immobilization with static or dynamic orthoses, early mobilization, or a combination of both. While various orthotic approaches exist, none have shown superiority over others. However, consensus suggests a period of complete immobilization followed by gradual mobilization, aiming to restore the range of motion and maintain the length of the oblique retinacular ligament. This comprehensive understanding underscores the complexity of boutonniere deformity management, emphasizing the importance of tailored treatment strategies for optimal outcomes. Relating treatment options to the pathology is essential; for instance, immobilization helps prevent further damage to the central slip and triangular ligament in the early stages, while early mobilization can aid in maintaining joint flexibility and preventing stiffness in later stages.
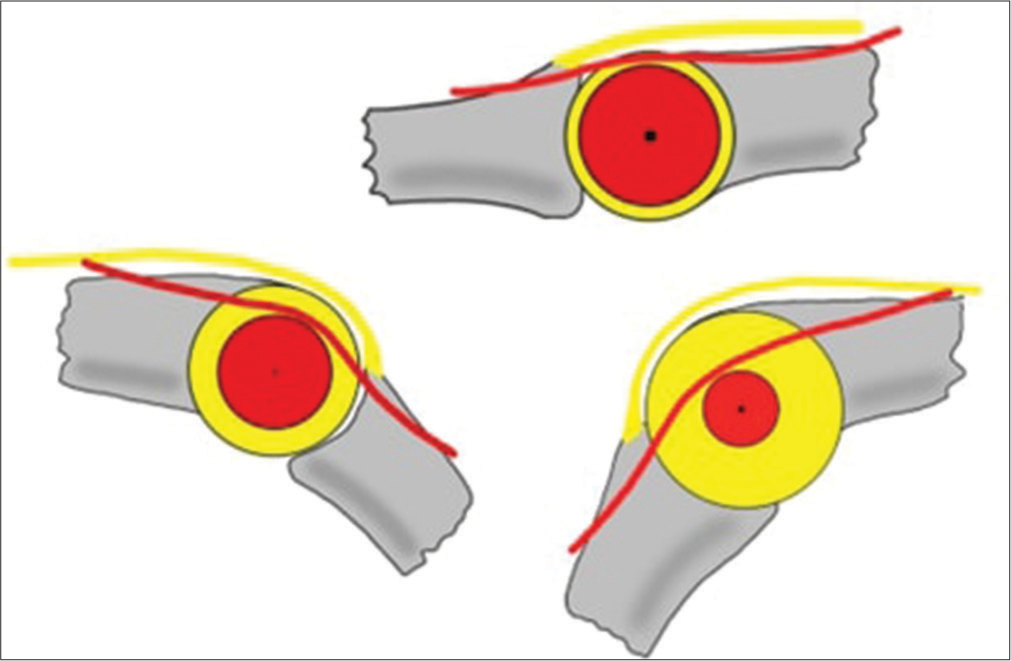
- Top view of the forces exerted by the lateral and central bands on a simulated proximal interphalangeal joint, illustrating the distribution and orientation of force moments under normal conditions and during flexion.
The treatment choice should be individualized based on several factors, including the severity of the deformity, patient age, activity level, and overall health.[6-8] For acute cases, immediate immobilization with a splint is often recommended to prevent further damage and allow healing. In contrast, chronic cases might require a combination of splinting and therapeutic exercises aimed at regaining motion and strength.
Patients with high activity levels or those involved in sports might benefit from dynamic splinting, which allows some degree of movement while still protecting the affected structures. Elderly patients or those with comorbid conditions may require a more conservative approach, with static splinting and gradual physical therapy to avoid additional stress on the joints.
AUTHORS’ CONTRIBUTIONS
RT and PB designed this letter for the editor, provided the data material, interpreted the data, wrote the initial and final manuscript, and reviewed the literature. PB and DD have critically reviewed and approved the final draft. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The Institutional Review Board approval is not required.
DECLARATION OF PATIENT CONSENT
Patient’s consent was not required as there are no patients in this study.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that no artificial intelligence (AI)-assisted technology was used to assist in the writing or editing of the manuscript, and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit.
References
- Treating the proximal interphalangeal joint in swan neck and boutonniere deformities. Hand Clin. 2018;34:167-76.
- [CrossRef] [PubMed] [Google Scholar]
- Central slip and bilateral lateral band laceration with negative Elson's and modified Elson's tests. Trauma Case Rep. 2022;40:100671.
- [CrossRef] [PubMed] [Google Scholar]
- Non-surgical treatment of oblique diaphyseal fractures of the fourth and fifth metacarpals in a professional athlete: A case report. Int J Surg Case Rep. 2024;115:109256.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of short-stretch bandage and long-stretch bandage for post-traumatic hand edema. Int J Surg Case Rep. 2023;111:108854.
- [CrossRef] [PubMed] [Google Scholar]
- A case report: Pain in the hand and tingling of the upper limb may be a symptom of a schwannoma in the supraclavicular region. Int J Surg Case Rep. 2023;110:108664.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and patient acceptability of 3 orthosis models for radial nerve palsy. Hand Surg Rehabil. 2024;43:101677.
- [CrossRef] [PubMed] [Google Scholar]
- Integrating the Drucebo effect into PM&R: Enhancing outcomes through expectation management. Am J Phys Med Rehabil 2024
- [CrossRef] [PubMed] [Google Scholar]
- An overview of rehabilitation approaches for focal hand dystonia in musicians: A scoping review. Clin Rehabil. 2024;38:589-99.
- [CrossRef] [PubMed] [Google Scholar]





