Translate this page into:
Evaluation of total hip arthroplasty for management of acetabular fracture complications: A prospective cohort study
*Corresponding author: Mohamed Abdelmoneim, Department of Orthopedic Surgery, Kasralainy School of Medicine, Cairo University, Cairo, Egypt. m.abdulmoneim@kasralainy.edu.eg
-
Received: ,
Accepted: ,
How to cite this article: Abd-Elmoneim MA, Farid H, El-Nahal AA, Mohamad MM. Evaluation of total hip arthroplasty for management of acetabular fracture complications: A prospective cohort study. J Musculoskelet Surg Res. 2024;8:210-20. doi: 10.25259/JMSR_90_2024
Abstract
Objectives:
Total hip arthroplasty (THA) has been recommended as an effective tool for restoring joint function. This study aimed to evaluate the functional and clinical outcomes of THA management of acetabular fracture late complications such as arthritis by both Harris-Hip Score (HHS) and Western Ontario McMaster Osteoarthritis Index (WOMAC) score, anticipate, and prevent the most common complications such as infection and dislocation.
Methods:
This prospective case series included 30 patients with THA to manage acetabular fracture complications such as arthritis. The study started in November 2021 and ended in September 2023. Inclusion criteria were patients with acetabular fractures with secondary arthritis (pre-existing osteoarthritis were excluded) aged 25– 70 and who had at least 1 year from fracture to arthroplasty. Exclusion criteria were patients with a history of previous infection.
Results:
Heterotopic ossification (HO) improved statistically significantly after using ketorolac at an 18-month follow-up compared to preoperatively. Using both the HHS and WOMAC scores, a statistically significant difference was found between pre-operative and post-operative functional outcomes for estimating HO development using radiographs.
Conclusion:
THA was safe and effective in managing late acetabular fracture complications. Ketorolac use showed promising results in prophylaxis against HO.
Keywords
Heterotopic ossification
Human
Ketorolac
Osteoarthritis
Total hip arthroplasty
INTRODUCTION
Acetabular fractures are linked to a high risk of late post-traumatic degenerative disorders, as high as 57%.[1] Imperfect reductions, femoral head lesions, chondral injuries to the acetabulum, and pre-existing arthritis can all lead to hip joint degeneration.[2-6] The common causes of surgically treated acetabular fracture failure can be mechanical or biological. The mechanical failure can be caused by (1) inadequate internal fixation technique, (2) acetabular fractures not reduced anatomically, (3) femoral head cartilage lesions, (4) marginal impaction fractures, (5) poor bone quality, and (6) screw protrusion within the joint, whereas the biological failure causes can be (1) chondrolysis, (2) avascular necrosis (AVN), (3) infection, and (4) non-union.
Since it helps to restore the hip center of rotation, initial open reduction and internal fixation (ORIF) of acetabular fractures may make the subsequent total hip arthroplasty (THA) easier. The arthroplasty surgeon must manage possible difficulties such as significant soft-tissue scarring, heterotopic ossification (HO), retained internal devices, and residual bone defects after ORIF. However, THA after non-operative treatment of acetabular fractures presents challenges since patients frequently show up with malunion or non-union, resulting in acetabular bone defects and an acetabular discontinuity.[7]
In general, both cemented and cementless THA can be used to manage hip osteoarthritis (OA) post-acetabular fractures and femoral head AVN.[8,9] Winemaker et al. reported high complication rates following the conversion of failed acetabular fracture treatment to THA.[10,11]
Loosening prevention could be achieved by reducing the wear of polyethylene. Design elements, including modularity, geometry, and implant attachment, have been demonstrated to be among the most crucial factors influencing the production of wear particles to prevent wear. The femoral head’s dimensions should be chosen to ensure that the polyethylene layer is at least 6 mm thick, ideally 8 mm thick. Ceramic on ceramic or ceramic on polyethylene has a lower wear rate than metal on polyethylene, affecting the osteolysis rate.[12]
The aim of the present study was to evaluate functional results using the Harris-Hip Score (HHS) and Western Ontario McMaster Osteoarthritis Index (WOMAC) of THA following late acetabular fracture complications to anticipate and prevent the common complications encountered after procedures such as dislocation, infection, HO, and aseptic loosening, and properly manage them if they happen.
MATERIALS AND METHODS
This prospective case series included 30 patients with THA for the management of late acetabular fracture complications such as arthritis due to malunion and/or AVN. The study was conducted in November 2021 and September 2023, with a mean follow-up time postoperatively of 14.3 months (Range 12–18 months). Inclusion criteria were patients who developed hip OA secondary to acetabular fractures arthritis (pre-existing OA was excluded either radiologically if available or according to patients’ history if no previous radiographs were available), aged 25–70 years, and time from fracture to arthroplasty of at least 1 year to give time for the fracture to have a solid union. Exclusion criteria were patients with a history of infection preoperatively before undergoing THA.
The mean age at arthroplasty was 47.8 (±11.3) years (Range 26–69 years), with a male predominance of 24 males [Table 1].
| No. (cases) | Age in years | % | ||||
|---|---|---|---|---|---|---|
| Sex | ||||||
| Male | 24 | 80 | ||||
| Female | 6 | |||||
| Age, years (at arthroplasty) | ||||||
| Mean of age (year)±SD | 47.8±11.3 | 20 | ||||
| Median (IQR) | 50 (15) | |||||
| Range (in years) | 26–69 | |||||
| Type I | Type IIA | Type IIb | Type IIC | Type IIIA | Type IIIB | |
| Classification according to Paprosky classification | 30% | 20% | 13.3% | 13.3% | 20% | 3.3% |
| Type I | Type II | Type III | Type IV | |||
| Classification according to AAOS classification | 36.7% | 30.3% | 36.7% | 3.3% | ||
IQR: Inter-quartile range, SD: Standard deviation, AAOS: American Academy of Orthopedic Surgeons
Pre-operative assessments were clinical, functional, radiological, and laboratory assessments. Radiological assessment was done by plain radiographs of the affected joint (anteroposterior, iliac and obturator oblique views) and computed tomography of the affected joint to assess the acetabular defect to plan the suitable option for acetabular reconstruction. The defect was classified by Paprosky and the American Academy of Orthopedic Surgeons (AAOS) classifications [Table 1].[13,14] Pre-operative erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were done to exclude infection in addition to proper clinical examination of symptoms and signs of infection. If there is a suspicion of infection, a pre-operative hip aspiration was performed, and the results were sent for a cell count with differential and a 14-day culture.
Patients were counseled about the management plan, and informed consent was obtained regarding participation and use of medical data for publication.
Post-operative HO was prevented using Ketorolac 60 mg intraoperatively and five doses postoperatively with doses of 30 mg\8 h by IM injection.[15]
A protocol for the prevention of postoperative dislocation was performed. Intraoperatively, the acetabular defect was managed by bone grafts, either autograft, allograft, metal augments, or cages, to reach the normal hip center of rotation and good tension of the abductor’s muscles, trying to have a stable prosthesis. Furthermore, the version of the stem and the cup were to be in the normally accepted range.
Postoperative management was carried out by a multidisciplinary team. Weightbearing precautions varied and were determined by the surgeon individually. Patients who underwent extra plate osteosynthesis or received a bone graft were advised to toe-touch weight-bearing for six weeks. Then, this was increased gradually to partial weightbearing (50%) for another six weeks. At 12 weeks after having a check radiograph to ensure the graft was taken in patients who needed acetabular reconstruction and sound union achieved in patients with osteosynthesis, the weightbearing was increased to full weightbearing.[16,17]
After the arthroplasty, combined mechanical and pharmacological prophylaxis against deep venous thrombosis was started.[18,19] Each patient was given printed instructions regarding home exercises.
Protocol for infection prevention was performed. A first-generation cephalosporin antibiotic was given before induction of anesthesia, and two doses were given postoperatively. ESR and CRP were negative three weeks after the operation, so the possibility of infection was excluded from the study. All patients were followed postoperatively and later to exclude infection using clinical evaluation first, including symptoms of infection such as rest pain, wound discharge, and signs of infection such as redness, tenderness, and draining sinus. If infection was suspected, ESR and CRP were performed. If no draining sinus was present in the suspected cases, image-guided hip aspiration under complete aseptic precautions in the operating room was performed. Following the final reduction, the trial heads should be used to conduct the equator test, the dislocation test, and a component telescoping check. A dual mobility cup was considered for weak gluteus medius or neuromuscular disorders.
In the present study, HO was prevented by radiological assessment of the pre-operative HO in radiographs. If present, the surgeon had to be sure if it was mature or not to decrease its incidence of recurrence, and postoperative prophylaxis was performed using ketorolac with the aforementioned protocol.[15]
Statistical analysis
Data was loaded into the computer, and IBM Statistical Package for the Social Sciences software package version 20.0 was used for analysis (IBM Corp., Armonk, NY). Numbers and percentages were used to describe the qualitative data. The Shapiro–Wilk test was performed to confirm the distribution’s normality. The terms range (minimum and maximum), mean, standard deviation, median, and interquartile range were used to characterize quantitative data. P < 0.05 was considered when determining statistical significance.
The Chi-square test is used to compare categorical variables in different groups. Fisher’s Exact or Monte Carlo correction for correction for Chi-square when more than 20% of the cells have an expected count of <5. Student t-test for normally distributed quantitative variables to compare between two studied groups. Paired t-test for normally distributed quantitative variables to compare between two periods. Mann–Whitney test for abnormally distributed quantitative variables was used to compare the two studied groups. Wilcoxon signed-ranks test for abnormally distributed quantitative variables to compare between two periods. Pearson coefficient was to correlate between two normally distributed quantitative variables.
RESULTS
All study patients received THA per the proposed protocol [Figure 1]. The mean follow-up period was 14.3 months (Range 12–18 months). The estimated blood loss was 670 mL, and the average hospital stay was 4.9 days (Range 3–7 days).
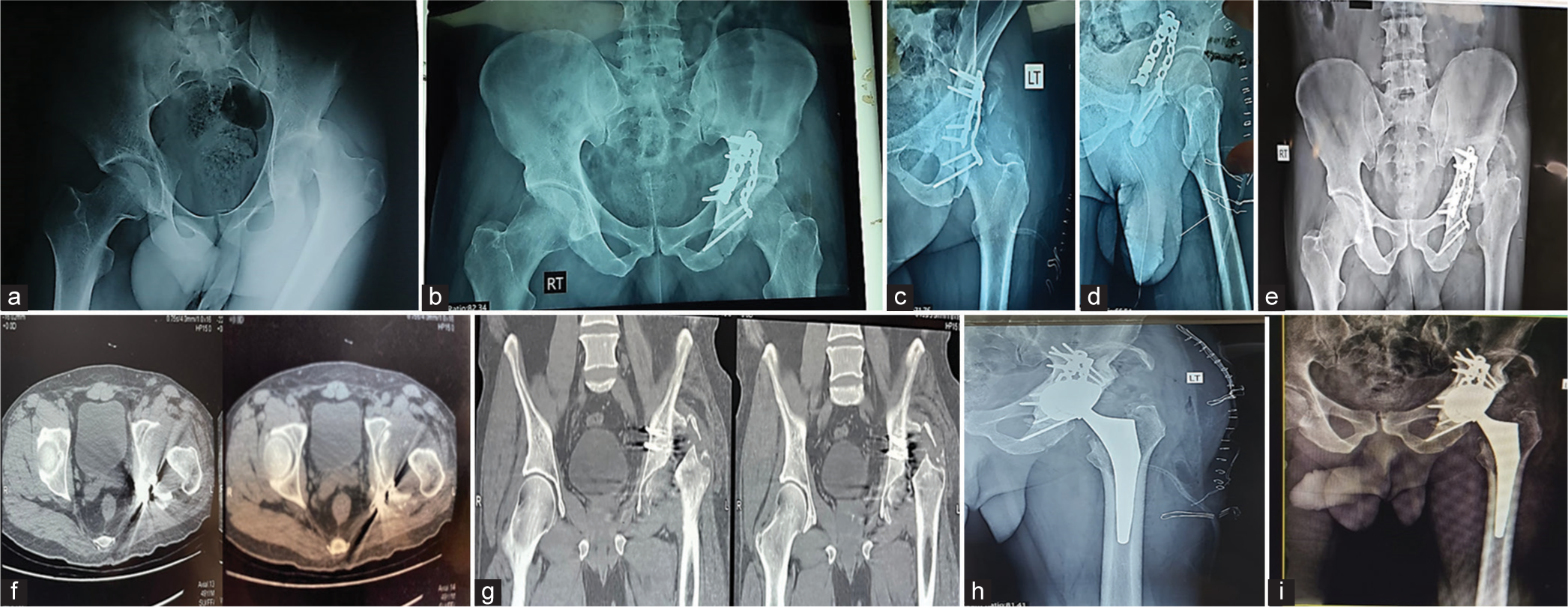
- (a) Anteroposterior (AP) radiograph of both hips of a 65-year-old male patient, showing fracture posterior wall and posterior dislocation of the left (Lt) hip due to road traffic accident. (b) AP radiograph, (c) obturator oblique view, and (d) iliac oblique view of showing the posterior wall did not reduce well after open reduction and internal fixation of the posterior wall by plate and screws and fragments of the posterior wall still displaced and not fixed. (e) AP, radiograph after 1 year from acetabular fixation showing dislocated Lt hip with resorbed femoral head and heterotopic ossification (HO) grade III (f) axial and (g) coronal computed tomography cuts of Lt hip showing the acetabular defect and resorbed femoral head. (h) Immediately post-operative radiograph showing dual mobility total hip arthroplasty with strut graft fixed by two screws. The remaining HO was grade I. (i) AP radiograph of the Lt hip after 18 months shows stable prosthesis and no newly formed HO.
Approaches used
The posterior approach to the hip was used in 25 (83.33%) patients, while the direct lateral approach was used in five (16.66%) patients (mostly not in need of acetabular reconstruction). The mean operative time was 2.6 (±0.4) h, ranging from 2.1 to 4 h.
The overall intraoperative complications rate was 16.6%, which was related to intraoperative prosthetic fractures, while the postoperative complications rate was 23.3% [Table 2].
| No.(cases) | % | |
|---|---|---|
| Intraoperative complications | ||
| Greater trochanter fracture | 3 | 10 |
| Calcar fracture | 2 | 6.7 |
| Postoperative complications | ||
| Dislocation | 2 | 6.7 |
| Stem loosening | 1 | 3.3 |
| Cup loosening | 2 | 6.7 |
| Newly formed heterotopic ossification | 2 | 6.7 |
| Reoperation (Revision) | 2 | 6.7 |
| Surgical Site Infection | 0 | 0 |
Postoperatively, there were no symptoms or signs of acute infection. ESR and CRP, three weeks postoperatively, were negative, so the possibility of acute infection was excluded from the study.
Regarding loosening postoperatively, at the 10-month follow-up, one case (3.3%) had stem loosening (cementless stem), which was managed by revising the stem with a long cementless stem. The patient was followed for three months and then died due to causes not related to her arthroplasty operation. After 15 months of the arthroplasty, two cases had cup loosening. The first patient was managed by revision using the Delta TT Revision System (Cementless cup with cementless metal augment), and the other patient was planned for later revision.
Two (6.7%) cases of prosthetic dislocations were reported. The first patient was dislocated after six months of follow-up and managed conservatively by closed reduction and abduction brace for three months and no further consequences were encountered; the second patient was mentioned before to have loosening of the stem, which caused dislocation (10 months postoperatively) [Figure 2].
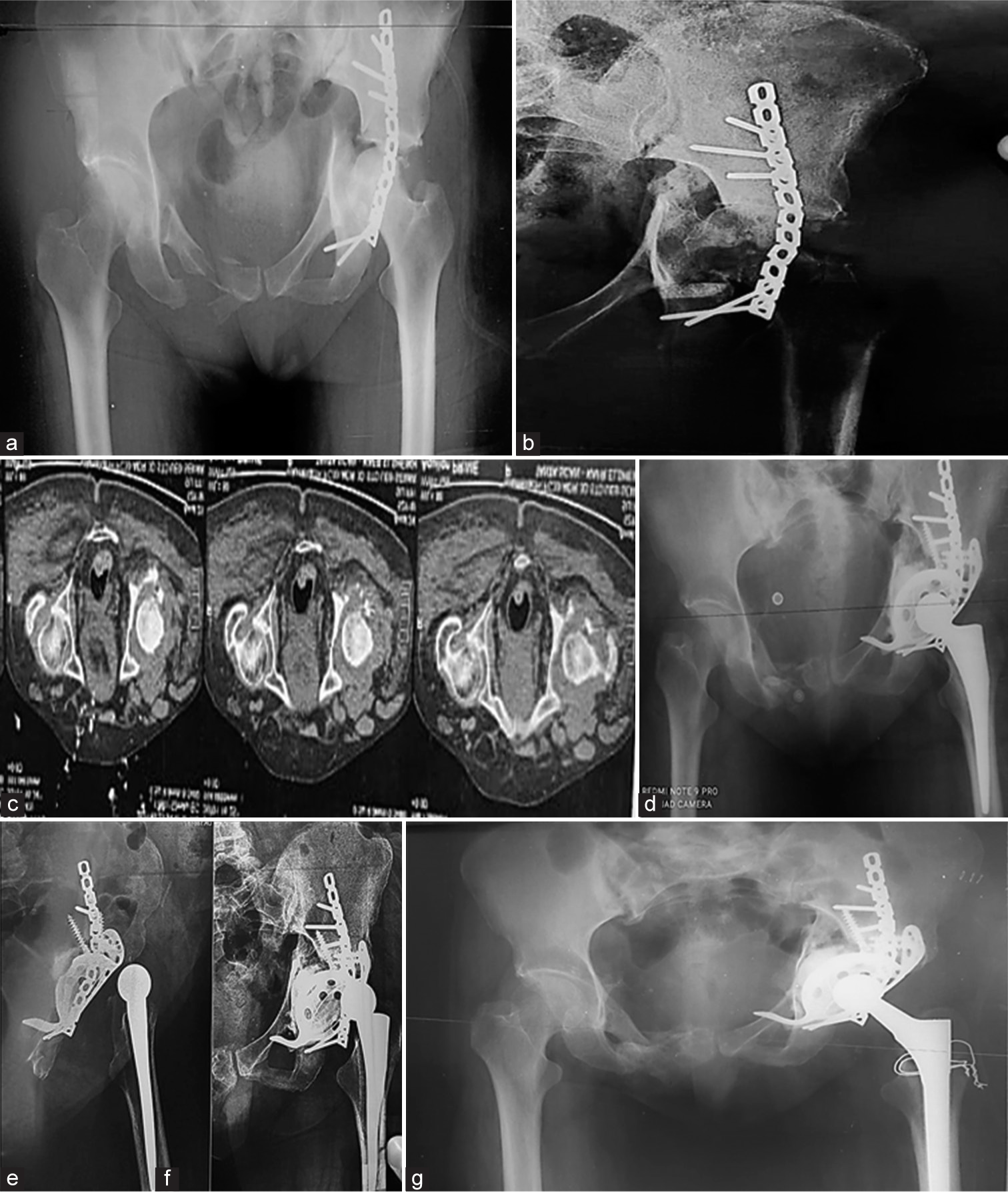
- (a) Anteroposterior (AP) radiograph of the pelvis showing transverse left (Lt) acetabular fracture fixed by plate and screws of a 59-year-old female, (b) acetabular defect classified as American Academy of Orthopedic Surgeons type IIIb, (c) axial cuts of the Lt hip showing the acetabular defect, (d) total hip arthroplasty (THA) (cemented cup and cementless stem) with autograft and Burch-Schneider ring to reconstruct the acetabular defect. (e) AP radiograph, (f) lateral radiograph of the hip, 10 months after THA, showing prosthetic dislocation with stem loosening, and (g) revision of the stem by a long cementless stem and cerclage due to greater trochanter fissure fracture.
Regarding HO at 18-month follow-up, newly formed HO occurred in two (6.7%) patients. One patient (3.3%) was grade I (no HO pre-arthroplasty) [Figure 3]. Another one (3.3%) was grade II (he had HO preoperatively graded as grade IV and was partially excised during THA and after arthroplasty. The remaining HO was grade I and then progressed to grade II after 18 months), which did not affect the range of motion, so no further management was required. HO assessment in the current study was done using radiographs as extra-skeletal bone formation in the surrounding muscles and tissues.
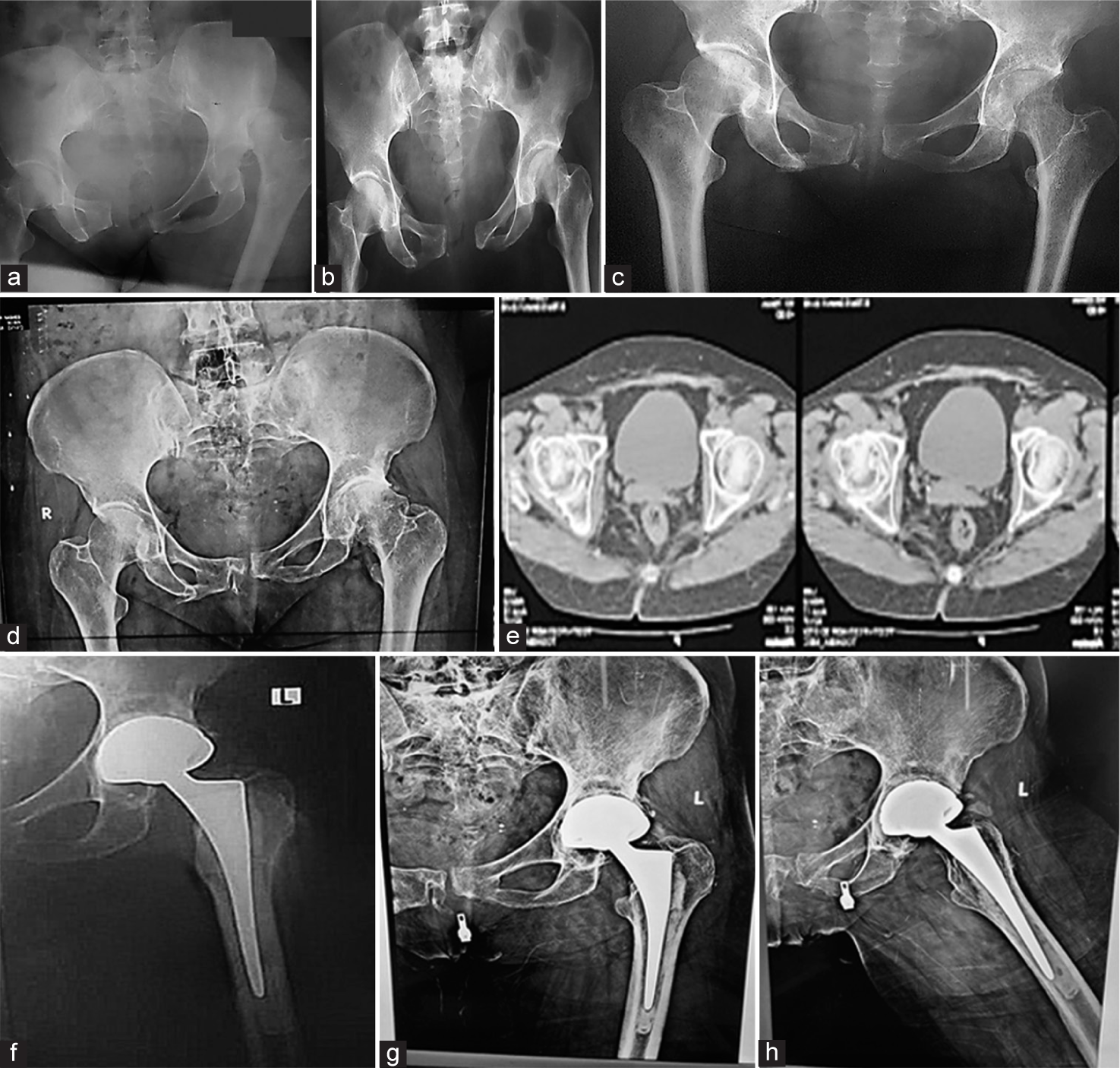
- (a) Anteroposterior (AP) radiograph of both hips showing left (Lt) acetabular posterior wall fracture-dislocation of a 69-year-old female patient at the time of accident 28-years-ago, (b) reduction of dislocated Lt hip after closed reduction and skeletal traction, (c) after 1 year from the fracture showing united acetabular fracture and osteoarthritis (OA) of the hip, (d) OA Lt hip after 28 years from the trauma, (e) computed tomography axial cuts before arthroplasty showed minimal rim defect of the posterior wall, (f) immediately postoperatively of Lt hip shows cemented dual mobility, (g) AP, and (h) lateral radiograph of the Lt hip, after 18 months of the arthroplasty, shows a radiolucent line around the superior aspect of the cup, stable prosthesis, and heterotopic ossification grade I.
Regarding functional improvement, the mean HHS improved from a pre-operative value of 39.6 (±6.8) to 80.1 (±7.9) postoperatively. The mean WOMAC score improved from 79.83 (±6.5) preoperatively to 34.9 (±9.35) postoperatively [Figure 4].
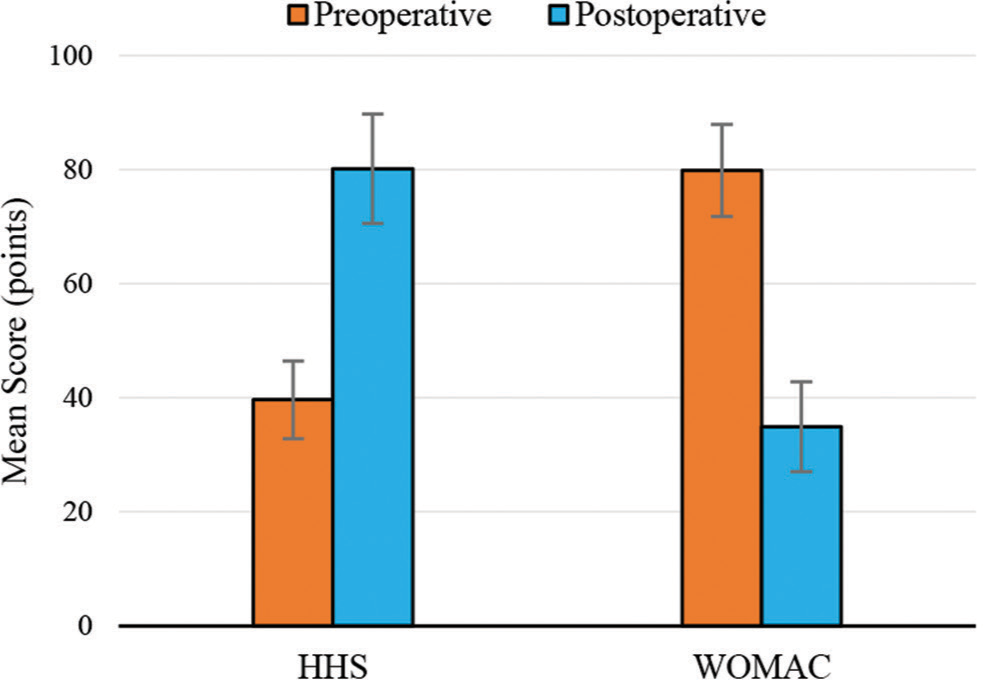
- Pre-operative and post-operative HHS and WOMAC. HHS: Harris Hip Score, WOMAC: Western Ontario McMaster Osteoarthritis Index.
No statistical significance was found between the improvement of the HHS and fracture-dislocation of the hip pre-acetabular fixation (P = 0.143). The type of prosthesis also had no statistical significance [Table 3] with the improvement of the HHS (P = 0.387).
| Type of prosthesis | Number of cases |
|---|---|
| Cemented conventional THA | 1 case |
| Cementless conventional THA | 20 cases |
| Hybrid conventional THA | 1 case |
| Reverse hybrid conventional THA | 5 cases |
| Cemented dual mobility THA | 1 case |
| Cementless dual mobility THA | 1 case |
| Reverse hybrid dual mobility THA | 1 case |
THA: Total hip arthroplasty
DISCUSSION
THA surgery was saved for the aftereffects of acetabular fractures.[20] Following the failure of acetabular fracture treatment, THA is frequently utilized to restore joint function and has been recommended as an efficient means of restoring normal hip function.[21]
Regarding the mean age at the time of arthroplasty and sex, in comparison with the aforementioned results, Dawson et al.[21] showed that the mean age at the time of first surgery was 53 years and most patients were male (68%). Do et al.[22] assessed the results of a THA for acetabular fracture complications among 25 patients. The study showed that the mean age at fracture was 58 (36–85) years, and most patients were male (76%).
In agreement with the current study, Do et al.[22] showed that no infection had occurred post-THA. However, Yuan et al.[23] had implant infection among (3.44%) out of 1284 patients who underwent THA due to acetabular fracture-related post-traumatic OA. Dawson et al.[21] had one postoperative superficial infection, which was managed successfully by antibiotics. Differences between the present study and other studies compared to Yuan et al. may be because the latter study had a much larger sample size of patients.[23]
In the present study, statistical significance was found associating cases that had cup loosening and had bone graft reconstruction by allograft (two cases had loosening with bone allograft out of six cases that were reconstructed by allograft) (P = 0.004) [Table 4].
| Acetabular graft | Loosening | χ2 | MC P | |||
|---|---|---|---|---|---|---|
| No (n=27 cases) | Yes (n=3 cases) | |||||
| No. | % | No. | % | |||
| None | 13 cases | 48.1 | 0 cases | 0.0 | 9.918 | 0.004* |
| Morselized autograft | 11 cases | 40.7 | 1 cases | 33.3 | ||
| Morselized allograft | 0 cases | 0.0 | 2 cases | 66.7 | ||
| Structural | 3 cases | 11.1 | 0 | 0.0 | ||
χ2: Chi square test, MC: Monte Carlo test, P: P value for comparing between No and Yes, *: Statistically significant at P≤0.05
However, there is no statistical significance associating cup loosening with the entity of acetabular defect classification (neither Paprosky classification, P = 0.055, nor AAOS classification, P = 0.065, respectively).
Dawson et al.[21] showed that at a 12-month follow-up of 25 patients, there were no signs of implant loosening, subsidence, or radiographic loosening. However, Lucchini et al.[20] showed that at 142 months of follow-up of 68 patients, loosening occurred in 4 patients (5.8%).
In the present study, no statistically significant difference was found between the age of the patients at the arthroplasty and post-operative prosthetic dislocation (P = 0.176). Furthermore, there was no statistically significant difference (P = 1.000) between the approach used and postoperative prosthetic dislocation. On the other hand, statistical significance regarding these two points may not be accurate enough due to the relatively small number of patients in the current cohort and the fact that only two cases of dislocation were encountered.
Compared with the results of the present study, Pritchett et al. studied Ketorolac’s efficacy in the prophylaxis of HO.[15] They showed statistical significance in preventing HO and good patient compliance because all doses were given when the patient was in the hospital. Its side effects, especially gastrointestinal manifestations, were less than that of other non-steroidal anti-inflammatory drugs such as indomethacin.[15] A statistically significant improvement was found in terms of newly formed HO at an 18-month follow-up compared to pre-arthroplasty HO (Chi-square test, P = 0.001), as shown in Table 5.
| HO pre- arthroplasty | Newly formed HO post arthroplasty | P-value | ||||
|---|---|---|---|---|---|---|
| No. | % | No. | % | |||
| Brooker Grading | ||||||
| Grade 0 | 26 | 90 | 28 | 93.3 | 0.001* | |
| Grade I | 0 | 0 | 1 | 3.3 | ||
| Grade II | 0 | 0 | 1 | 3.3 | ||
| Grade III | 3 | 10 | 0 | 0 | ||
| Grade IV | 1 | 3.3 | 0 | 0 | ||
P: P-value for comparing between No and Yes, *: Statistically significant at P≤0.05. HO: Heterotopic ossification
In the present study, a relationship was found between the newly formed HO post-arthroplasty and the age of the patients at the time of arthroplasty (P = 0.031). A statistically significant difference, at P ≤ 0.05, occurred in older patients (above 60 years old at the time of arthroplasty).
The study showed a statistically significant difference between the fracture-dislocation and HO pre-arthroplasty (P = 0.008) and no statistical significance between the fracture-dislocation and newly formed HO post-arthroplasty (P = 1.000), which means that there is a relation between the fracture-dislocations of the hip preoperatively and the occurrence of HO following the dislocation in the early period and also means the effectiveness of ketorolac in preventing postoperative HO [Table 6].
| HO | Fracture dislocation (pre-arthroplasty) | χ2 | FEP | |||||
|---|---|---|---|---|---|---|---|---|
| No (n=20 cases) | Yes (n=10 cases) | |||||||
| No. (cases) | % | No. (cases) | % | |||||
| Post-fixation | ||||||||
| No | 20 | 100.0 | 6 | 60.0 | 9.231 | 0.008* | ||
| Yes | 0 | 0.0 | 4 | 40.0 | ||||
| Post-arthroplasty | ||||||||
| No | 19 | 95.0 | 9 | 90.0 | 0.268 | 1.000 | ||
| Yes | 1 | 5.0 | 1 | 10.0 | ||||
χ2: Chi-square test, FE: Fisher exact, HO: Heterotopic ossification, P-value for comparing between No and Yes,*: Statistically significant at P≤0.05
Furthermore, this study found no relation between the patient’s sex and the occurrence of the newly formed HO post-arthroplasty (P = 0.031). Hence, sex did not affect HO postoperatively in the present study. This study’s newly formed HO post-arthroplasty in this study had no statistical significance with the improvement of HHS. Like HHS, the same statistical significance was found with the WOMAC score.
Luthra and Habsi[24] reported four cases (11.11%) out of 36 cases with HO, with no prophylaxis preoperatively. However, Gavaskar et al.[7] reported HO in 17 (38%) patients out of 44. Despite that, Salama et al.[25] reported HO in 2 (10%) patients out of 21. In the previous studies, HO prophylaxis was not used.
In the present study, no relation was found between age and improvement of HHS (P = 0.820) and WOMAC score (P = 0.906). Milenkovic et al.[26] showed that the mean HHS improved for all patients after THA following acetabular fracture surgery, going from 44.0 (±11.9) points (range 27– 58 points) preoperatively to 88.6 (±5.1) points (range 74–94 points) postoperatively (P < 0.001). Do et al.[22] (25 patients) showed that pre-operative HHS 41 (18–47) improved to 88 (77–100) postoperatively). As well, Wang et al.[27] revealed that all patients’ mean HHS improved from 44.0 ± 11.9 points (range, 27–58 points) preoperatively to 88.6 ± 5.1. Furthermore, Lucchini et al.[20] showed that HHS improved significantly after THA from 37.6 (±14.1) preoperatively to 88.4 (±11.6) (P = 0.001) postoperatively.
In the present study, a useful strategy to reduce the risk of dislocation when employing a posterior approach was the general repair of the posterior structures, capsule, and external rotators (piriformis tendon) using non-absorbable sutures. Compared with the present study’s results regarding dislocation, Zhang et al.[28] stated that 53 patients who received THA after acetabular fracture therapy failed were followed up for five years; of these, one patient (1.8%) experienced a dislocation.
Gavaskar et al.[7] also reported dislocations in 2 patients (4%) out of 44. Furthermore, Wang et al.[27] showed dislocation in 1 (3%) patient out of 33. However, Dawson et al.[21] showed no dislocation in 25 cases. Furthermore, Do et al.[22] reported that three patients had dislocations (12%) out of 25 cases.
Delgadillo and Pesantez discussed the outcomes of the fix and replace procedure for acute ORIF of acetabular fractures with THA performed in the same session, in contrast to the methodology of the present study.[29] They reported that the infection rate was approximately 11%. They reported a 19– 43% incidence of HO. According to a comprehensive study by Giannoudis et al.,[30] the HO incidence was about 25.6% in 2394 patients. However, only 5.7% of these instances had Class III or IV HO, as classified by Brooker classification. He also found no advantage in prophylactic use of indomethacin and/or radiation.[30]
In contrast, the present study’s findings showed the effective use of ketorolac in preventing HO in high-risk patients. The present study’s results differ from those of Giannoudis et al.’s.[30] However, this difference can be explained by the latter’s significantly larger sample size.
In addition, THA for acetabular fractures had a dislocation rate of 6.1% (4.0–8.5%), according to Delgadillo and Pesantez,[29] which was greater than THA for primary OA (2– 4%).[31] Closed reduction was the most common treatment, and 13.6% of cases required reoperation due to recurring dislocations.[32,33]
Delgadillo and Pesantez reported that although the fix-and-replace technique has produced good functional outcomes, its results are inferior to those of primary OA THA.[29] Among the 57 patients in Mears and Velyvis study,[34] 79% had satisfactory or outstanding results, with an average HHS of 89 points at eight years of follow-up. According to Smakaj et al.,[35] the “fix and replace” technique produced HHS outcomes that were 73 ± 2 at 3 months. The average time from fracture to THA in the current series was 2.7 years (Range 1–28 years).
The results above results showed that the fix-and-replace technique for acute THA following acetabular fractures can cause more complications than delayed THA following acetabular fractures. However, a larger sample size is needed for the present study to confirm these results. The published results of acetabular THA following acetabular fracture complications as OA/AVN compared to our study are summarized in Table 7.
| Patients number | Mean age | Methods | Follow up in months | Functional results | Complications | |
|---|---|---|---|---|---|---|
| Yuan et al. | 30 | 45 | 30 ORIF | 60 | - HHS 39 (3–71) to post HHS 82 (21–100) | - Infection: 3 - Dislocation: 2 patients - Revision: 3 patients |
| Gavaskar et al. | 47 | 24 | 27 ORIF 20 conservative |
88 | - Higher score in patients in the conservative group. | - HO: 17 patients - Dislocations: 2 patients - Revision: 2 patients |
| Wang et al. | 33 | 44 | 21 ORIF, 12 conservative | 138 | - HHS preoperative 44.0±11.9–88.6±5.1 points postoperatively | - Dislocation: 1 patient - HO: 10 patients - Revision: 3 patients |
| Salama et al. | 21 | 56 | 17 ORIF 4 conservative |
26 | - HHS was higher in the ORIF group - WOMAC From 63 preoperatively to 4 postoperatively |
- HO: 2 patients |
| Dawson et al. | 25 | 51.1 | RIF | 22 | -------------------------------------------- | - Superficial infection: 1 patient |
| Do et al. | 25 | 58 | 25 ORIF | 50 | - HHS 41 (18–47) to post HHS 88 (77–100) | - Dislocation: 3 patients - Infection: 0 |
| Lucchini et al. | 68 | 47 | 50 ORIF, 18 conservative | 142 | - HHS 37.6±14.1 to post 88.4±11.6 | - Infection: 0 - Dislocation: 2 patients - Loosening: 4 patients - Revision: 8 patients |
| Current study | 30 | 47 | 28 ORIF, 2 conservative | 20 | - HHS preoperative 37.1±6.8–78.5±9.6 postoperatively. - WOMAC improved from 80.9±1.5 preoperatively to 37.2±7.9 postoperatively |
- Infection: 0 - Dislocation: 2 patients - HO: 2 patients - Loosening: 3 patients - Revision: 2 patients |
THA: Total hip arthroplasty, ORIF: Open reduction and internal fixation, HHS: Harris hip score, HO: Heterotopic ossification, WOMAC: Western Ontario McMaster Osteoarthritis Index
The algorithm for managing post-traumatic acetabular OA proposed by the present study’s authors is summarized in Figure 5. The algorithm for managing complications of THA after acetabular fractures is summarized in Figure 6.
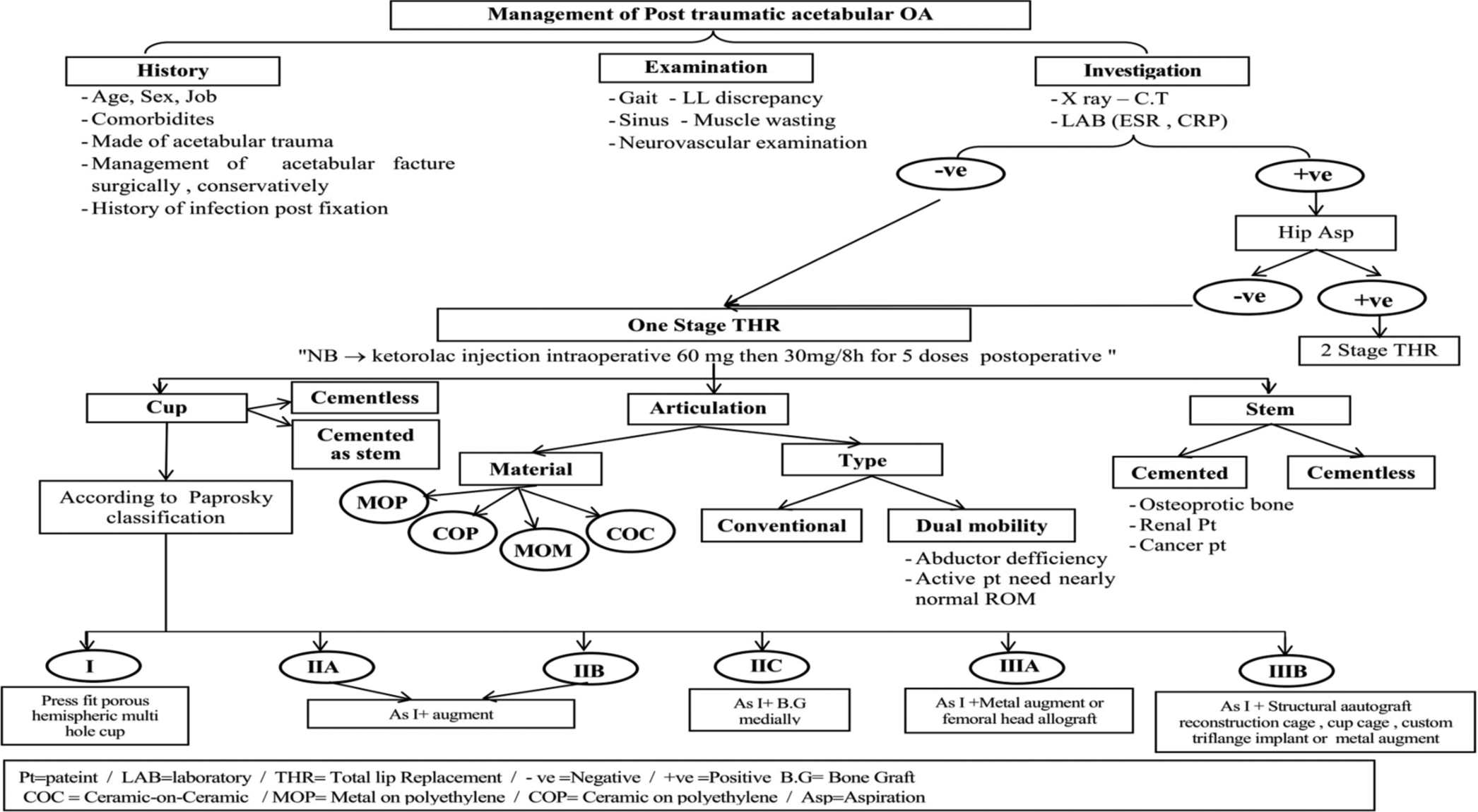
- Management of post-traumatic acetabular osteoarthritis. OA: Osteoarthritis, LL: Lower limb, NB: Nota bene, MOM: Metal-on-metal, ROM: Range of motion.
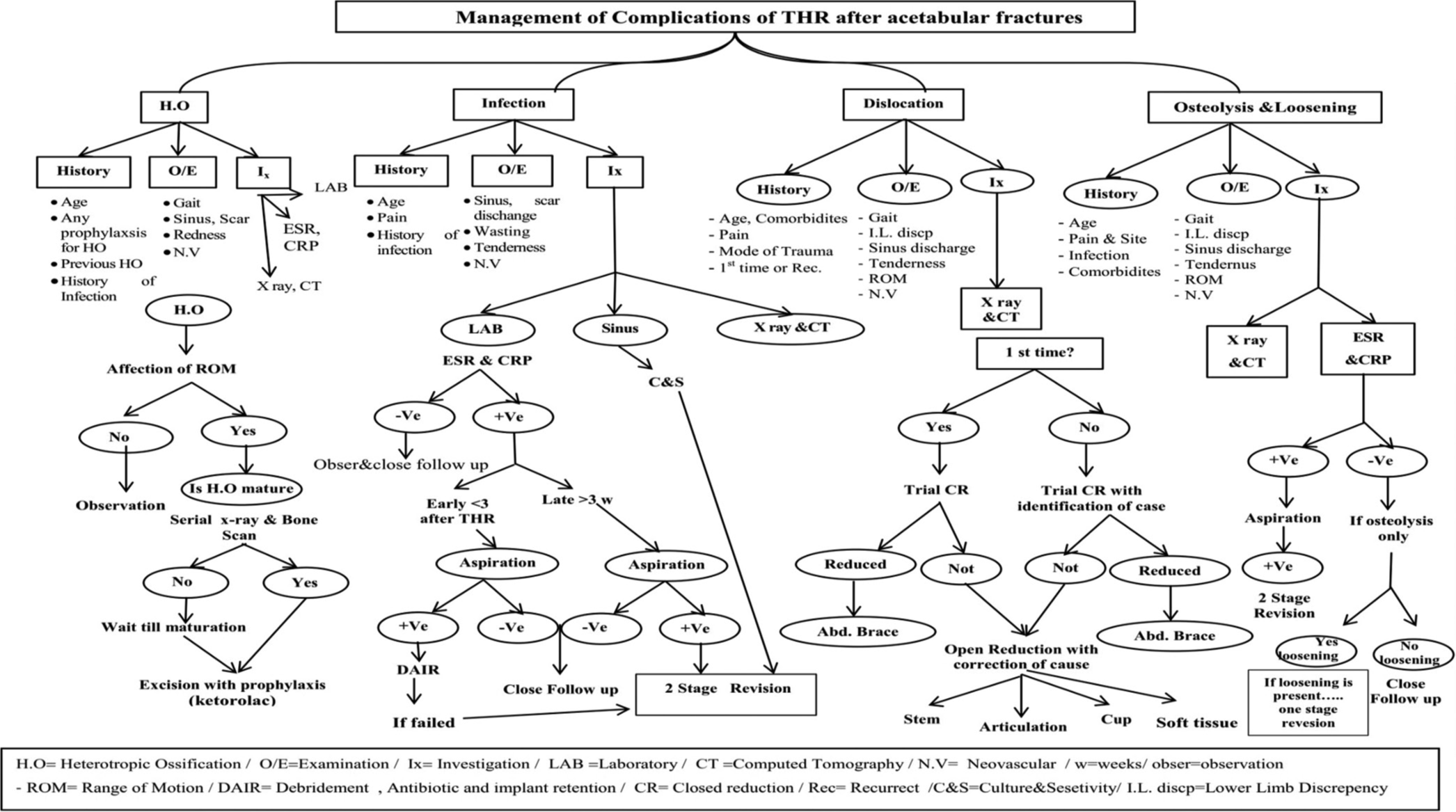
- Management of complications of total hip arthroplasty after acetabular fractures. THR: Total hip replacement.
The present study was limited by a small sample size, the lack of a control group, and a relatively short follow-up period.
CONCLUSION
The present study showed that THA was safe and effective in the late management of complicated acetabular fractures, significantly improving functional results. It was associated with minor complications compared with other series following proper anticipation and prevention of such complications using cementless fixation, which was preferred for fixation of the cup in cases with the previous acetabular fractures due to its better stability and longevity. Allograft use was associated with an increased incidence of postoperative loosening. Ketorolac use showed promising results in prophylaxis against HO and needs to be compared with other methods of HO prevention in literature.
Recommendations
The THA is a successful tool for treating acetabular fracture complications. The most successful treatment method is anticipating and preventing complications following THA in such cases. Ketorolac can provide effective preventive treatment for HO in this high-risk group of patients, so it should be used whenever needed. Restoration of native hip anatomy and center of rotation is the cornerstone in preventing implant-related complications such as dislocation and loosening. Hence, surgeons should always aim for the restoration of native hip anatomy.
AUTHORS’ CONTRIBUTIONS
MA: Suggestion of idea, operating cases, article writing, corresponding author. MM: Suggestion of idea, help in article writing, followup of cases. AE: Operating cases, collecting information. HF: Collecting information, followup of cases. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The study was conducted after obtaining the hospital Research Ethics Committee approval code (MD-408-2021). Date: 16 March 2022.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
The study did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
References
- Outcomes of delayed total hip arthroplasty in patients with a previous ipsilateral acetabular fracture. Expert Rev Med Devices. 2015;12:297-306.
- [CrossRef] [PubMed] [Google Scholar]
- Primary total hip arthroplasty after acetabular fracture. Instr Course Lect. 2001;50:335-54.
- [Google Scholar]
- Total hip arthroplasty in acetabular fractures. J Clin Orthop Trauma. 2020;11:1090-8. Erratum in: J Clin Orthop Trauma 2021; 21:101558
- [CrossRef] [PubMed] [Google Scholar]
- Fractures of the pelvis and acetabulum Vol 40. Baltimore: Williams and Wilkins; 2003. p. :741-50.
- [Google Scholar]
- Total hip arthroplasty for post-traumatic arthritis after previous acetabular fractures. Semin Arthroplasty. 2008;19:303-6.
- [CrossRef] [Google Scholar]
- Delayed total hip arthroplasty for failed acetabular fractures: The influence of initial fracture management on outcome after arthroplasty. J Arthroplasty. 2017;32:872-6.
- [CrossRef] [PubMed] [Google Scholar]
- Management of complex acetabular fractures by using 3D printed models. Medicina (Kaunas). 2022;58:1854.
- [CrossRef] [PubMed] [Google Scholar]
- Fractures of the pelvis and acetabulum Baltimore: Lippincott Williams and Williams; 1995.
- [Google Scholar]
- Short-term outcomes of total hip arthroplasty after complications of open reduction internal fixation for hip fracture. J Arthroplasty. 2006;21:682-8.
- [CrossRef] [PubMed] [Google Scholar]
- Total hip arthroplasty in acute acetabulum fractures: A systematic review. Arch Orthop Trauma Surg. 2023;143:6665-73.
- [CrossRef] [PubMed] [Google Scholar]
- Goodman and Jiri Gallo periprosthetic osteolysis: Mechanisms, prevention and treatment. J Clin Med. 2019;8:2091.
- [CrossRef] [PubMed] [Google Scholar]
- Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994;9:33-44.
- [CrossRef] [PubMed] [Google Scholar]
- Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop Relat Res. 1989;243:126-37.
- [CrossRef] [Google Scholar]
- Ketorolac prophylaxis against heterotopic ossification after hip replacement. Clin Orthop Relat Res. 1995;314:162-5.
- [CrossRef] [Google Scholar]
- Total hip replacement postop clinical practice guideline. 2022. Ohio: OSU; Available from: https://hrsosu.edu/media/files/wexnermedical/patient-care/healthcare-services/sports-medicine/education/medical-professionals/hip/totalhipreplacement.pdf?la=en&hash=622323146bb495b688822d5126988fd59d669ba0 [Last accessed on 2024 Mar 12]
- [Google Scholar]
- Post-operative total hip replacement protocol Colorado: Western Orthopaedics; 2010.
- [Google Scholar]
- The incidence and trauma mechanisms of acetabular fractures: A nationwide study in Finland between 1997 and 2014. Injury. 2017;48:2157-61.
- [CrossRef] [PubMed] [Google Scholar]
- Cementless ceramic-on-ceramic total hip arthroplasty in post-traumatic osteoarthritis after acetabular fracture: Long-term results. Arch Orthop Trauma Surg. 2021;141:683-91.
- [CrossRef] [PubMed] [Google Scholar]
- Total hip arthroplasty for the treatment of osteoarthritis secondary to acetabular fractures treated by open reduction and internal fixation. Eur J Orthop Surg Traumatol. 2019;29:1049-54.
- [CrossRef] [PubMed] [Google Scholar]
- Cementless total hip arthroplasty after failed internal fixation of acetabular fractures: A single center experience of 25 consecutive patients. J Orthop Surg (Hong Kong). 2020;28:2309499020910666.
- [CrossRef] [PubMed] [Google Scholar]
- Total hip arthroplasty for posttraumatic osteoarthritis secondary to acetabular fracture: An evidence based on 1,284 patients from 1970 to 2018. Front Surg. 2022;9:953976.
- [CrossRef] [PubMed] [Google Scholar]
- Delayed total hip arthroplasty in patients developing osteoarthritis following acetabular fractures. J Musculoskelet Surg Res. 2021;5:257-61.
- [CrossRef] [Google Scholar]
- Cementless total hip arthroplasty in the treatment after acetabular fractures. Eur J Orthop Surg Traumatol. 2018;28:59-64.
- [CrossRef] [PubMed] [Google Scholar]
- Total hip arthroplasty after acetabular fracture surgery. Int Orthop. 2021;45:871-6.
- [CrossRef] [PubMed] [Google Scholar]
- Delayed total hip arthroplasty after failed treatment of acetabular fractures: An 8-to 17-year follow-up study. J Orthop Surg Res. 2018;13:208.
- [CrossRef] [PubMed] [Google Scholar]
- Total hip arthroplasty for failed treatment of acetabular fractures: A 5-year follow-up study. J Arthroplasty. 2011;8:1189-93.
- [CrossRef] [PubMed] [Google Scholar]
- Fix and replace technique in elderly acetabular fractures. J Musculoskelet Surg Res. 2023;7:252-8.
- [CrossRef] [Google Scholar]
- Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg Br. 2005;87:2-9.
- [CrossRef] [PubMed] [Google Scholar]
- Acute total hip arthroplasty for older patients with acetabular fractures: A meta-analysis. J Clin Orthop Trauma. 2022;11:976-82.
- [CrossRef] [PubMed] [Google Scholar]
- Acute total hip arthroplasty for the treatment of acetabular fractures: A retrospective study with a six-year follow-up. Cureus. 2020;12:e10139.
- [CrossRef] [PubMed] [Google Scholar]
- Acetabular fractures in patients aged >55 years: A systematic review of the literature. Bone Joint J. 2014;96-B:157-63.
- [CrossRef] [PubMed] [Google Scholar]
- Acute total hip arthroplasty for selected displaced acetabular fractures: Two to twelve-year results. J Bone Joint Surg Am. 2002;84:1-9.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes of acetabular fractures treated with acute fix and replace versus open reduction and internal fixation in elderly population: A multicentric retrospective study. Int Orthop. 2022;46:2659-66.
- [CrossRef] [PubMed] [Google Scholar]






