Translate this page into:
Correlation between kinesiophobia and pain in people with knee osteoarthritis: A cross-sectional pilot study
*Corresponding author: Akshatha K. Shetty, Department of Musculoskeletal Sciences (Orthopedic Physiotherapy), JSS College of Physiotherapy, Mysuru, Karnataka, India. akshathashetty1998@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shetty AK, Uma HM. Correlation between kinesiophobia and pain in people with knee osteoarthritis: A cross-sectional pilot study. J Musculoskelet Surg Res. 2025;9:90-4. doi: 10.25259/JMSR_116_2024
Abstract
Objectives:
Osteoarthritis (OA) is a degenerative joint disease that impacts articular cartilage. As people age, OA becomes a more common major public health issue. The study’s goal was to determine how kinesiophobia, pain severity, and pain interference are related.
Methods:
The study included 24 individuals with OA who visited the institute’s outpatient department by convenience sampling. Data collection included applying the Kellgren–Lawrence classification for OA and three outcome scales. The participants included in this study were adults with knee pain diagnosed with OA, according to OA Research Society International guidelines and radiologically confirmed, who can understand the instructions on the scale. The participants excluded from this study were those who had a recent fracture, recent corticosteroid injection in the knee, history of systemic inflammatory arthritis, connective tissue disorder, genetic and congenital disorders, bleeding disorder, uncontrolled diabetes mellitus, knee replacement surgery, recent surgical excision of menisci, ligament, and osteomyelitis.
Results:
Spearman’s correlation coefficients (r) revealed a significant positive relationship between kinesiophobia and knee pain intensity (r = 0.7, P < 0.001). The study also revealed a considerable positive association between pain interference and knee pain intensity (r = 0.59, P = 0.002). Furthermore, favorable association was observed between kinesiophobia and pain interference (r = 0.63, P < 0.001).
Conclusion:
People with OA knee experience increased levels of kinesiophobia in response to worsening knee pain and hindrance from the pain.
Keywords
Activity avoidance
Kinesiophobia
knee
Osteoarthritis
Pain interference
INTRODUCTION
Osteoarthritis (OA) is a degenerative joint disease that damages the articular cartilage.[1,2] Kellgren–Lawrence (KL) classified OA into five stages based on pathological alterations in joint structures to determine the severity of the disease. According to Vaishya R, this categorization was proposed in 1957, and the World Health Organization approved it in 1961.[3] The most significant element is pain, one of OA’s primary symptoms. This trait is diverse and can cause either a dull or excruciating type of pain.[4] Pain interference is one potential functional effect of pain severity.[5,6]
The majority of people experience musculoskeletal pain at least once in their lifetime. Many known factors (physical, biological, cognitive, behavioral, social, and occupational) are connected to poor prognosis after the onset of musculoskeletal pain, which helps to explain why many people do not recover after an episode of acute musculoskeletal pain, frequently leading to a downward spiral of detrimental physical, social, and psychological effects. Patients struggle with a vicious cycle that perpetuates their chronic pain, functional limitations, growing disability, and pain thresholds. Fear of movement (kinesiophobia) may impact the progressive degradation and loss of muscle strength, endurance, and proprioceptive deficits in older people with knee OA.[7] On synthesizing the literature, it can be concluded that there is a documented association between kinesiophobia and pain intensity in other musculoskeletal illnesses. However, there has been no research on kinesiophobia, pain severity, and pain interference in knee OA. This study aimed to ascertain the relationship between kinesiophobia, pain intensity, and pain interference.
MATERIALS AND METHODS
Study design
Cross-sectional pilot study; Sampling technique: Convenience sampling; Sample size: 24 (calculated using G Power Software).
Participant characteristics
Inclusion criteria
Adults with knee pain diagnosed with OA according to OA Research Society International guidelines, radiologically confirmed KL stage, who could understand the instructions in the scale, were included in the study.
Exclusion criteria
Recent fracture (<1 year), recent corticosteroid injection in the knee (past six months), history of systemic inflammatory arthritis, connective tissue disorder, genetic and congenital disorders, bleeding disorder, uncontrolled diabetes mellitus, knee replacement surgeries, recent surgical excision of menisci, ligament, and osteomyelitis were excluded from the study.
Procedure
Ethical permission was obtained from the Institutional Ethical Committee before the study. The study process was explained to the participants who met the eligibility requirements based on inclusion and exclusion criteria. Participants who provided informed consent were included in the study. Participants’ demographic information was gathered and analyzed, and results were formulated.
The participants were seated on a chair or bed. The participants were at ease and comfortable. The room was quiet (no sound) and ventilated with good light. The participants received explanations in the language that they could understand regarding the study’s methods and goal. A consent form was given to the participant in their preferred language. The participants were allowed to review the consent form and clarify doubts. Written consent was obtained from the participant after the procedure was explained. If the participant could not read and write, the procedure was explained to them verbally in front of two witnesses. Then, if the participant agreed, a thumb impression was taken (Indian Council of Medical Research guidelines).
The procedure was standardized before the scale was administered to knee OA individuals. Five persons who knew both English and their native language were asked to fill out the questionnaire in both languages.
The participants were given a list of questions from three separate questionnaires to respond to. Participants in the first outcome measure, the Numerical Pain Rating Scale (NPRS), were asked to score on a scale of 0–10, with 10 denoting the highest level of pain and 0 denoting not feeling pain at all. Participants in the second outcome measure, the Tampa Scale of Kinesiophobia 11 (TSK-11), were asked to rate their answers to 11 items on a scale of 1 (strongly disagree) to 4 (strongly agree). In the third outcome measure, the Patient-Reported Outcomes Measurement Information System Pain Interference 6b (PROMIS PI-6b), participants were asked to score from 1 (no pain interference) to 5 (very much) for six questions. The questions from TSK-11 and PROMIS PI-6b were randomly asked in a meaningful order. The TSK-11 has good to outstanding internal consistency, with Cronbach’s alpha values ranging from 0.85 to 0.92.[8] PROMIS PI-6b has excellent test-retest reliability (Intraclass Correlation Coefficient = 0.83).[9] It was a one-time assessment.
Data analysis
Data were spread in an Excel sheet and categorized according to age, sex, body mass index (BMI), NPRS, TSK–11, and PROMIS–PI-6b. Data were analyzed using descriptive statistics. The association of values was calculated using Spearman’s correlation. Jamovi software was used for data analysis.[10] The P-value of less than or equivalent to 0.05 was deemed significant.
RESULTS
Six individuals were eliminated throughout the screening procedure out of the initial 30 who were recruited. Three individuals had a history of fractures 5–6 months prior, and three more had congenital deformities. Consequently, this study involved 24 participants.
Participant demographic data
A total of 24 individuals with knee OA participated in the study, seven of whom were males (29.2%) and 17 females (70.8%). The mean height was 158 cm, the mean weight was 68.9 kg, the mean age was 59 years, and the mean BMI was 27.6kg/m2 [Tables 1 and 2].
| Characteristics | Mean±Standard deviation |
|---|---|
| Age | 59±9.03 |
| Height (cm) | 158±6.15 |
| Weight (kg) | 68.9±8.07 |
| Body mass index (kg/m2) | 27.6±4.13 |
| Sex | Count | Percentage | BMI±Standard deviation |
|---|---|---|---|
| Male | 7 | 29.2 | 25.6±0.98 |
| Female | 17 | 70.8 | 28.3±4.52 |
BMI: Body mass index
Since all three outcome measures are ordinal scales, the median was considered. The median values of NPRS, TSK-11, and PROMIS PI-6b, respectively, are 6, 30, and 24. The interquartile range of NPRS, TSK-11, and PROMIS PI-6b, respectively, is 3, 4.50, and 8.50 [Table 3].
| Scales/Variables | Median | IQR |
|---|---|---|
| NPRS | 6 | 3 |
| TSK-11 | 30 | 4.50 |
| PROMIS PI-6b | 24 | 8.50 |
IQR: Interquartile range, NPRS: Numerical pain rating scale, TSK-11: Tampa scale of kinesiophobia-11, PROMIS PI-6b: Patient-reported outcomes measurement information system pain interference-6b
A considerably strong positive association (r = 0.7, P < 0.001) was found between the intensity of knee discomfort and kinesiophobia, according to the results of Spearman’s correlation coefficients (r). Furthermore, it revealed a somewhat favorable and statistically significant connection (r = 0.59, P = 0.002) between pain interference and knee pain intensity. In addition, a noteworthy moderate positive connection (r = 0.63, P < 0.001) was observed between kinesiophobia and pain interference. No relationship was found between age, sex, and all three scales [Table 4 and Figure 1].
| Variables | Spearman’s rho (r) | P-value |
|---|---|---|
| NPRS and TSK-11 | 0.71 | P<0.001 |
| NPRS and PROMIS PI-6b | 0.59 | P=0.002 |
| TSK-11 and PROMIS PI-6b | 0.635 | P<0.001 |
| Age and NPRS | −0.2 | P=0.3 |
| Age and TSK-11 | −0.09 | P=0.64 |
| Age and PROMIS PI-6b | −0.18 | P=0.39 |
| Sex and NPRS | 0.3 | P=0.1 |
| Sex and TSK-11 | 0.1 | P=0.59 |
| Sex and PROMIS PI – 6b | 0.22 | P=0.28 |
NPRS: Numerical pain rating scale; TSK-11: Tampa scale of kinesiophobia 11; PROMIS PI-6b: Patient-reported outcomes measurement information system pain interference 6b
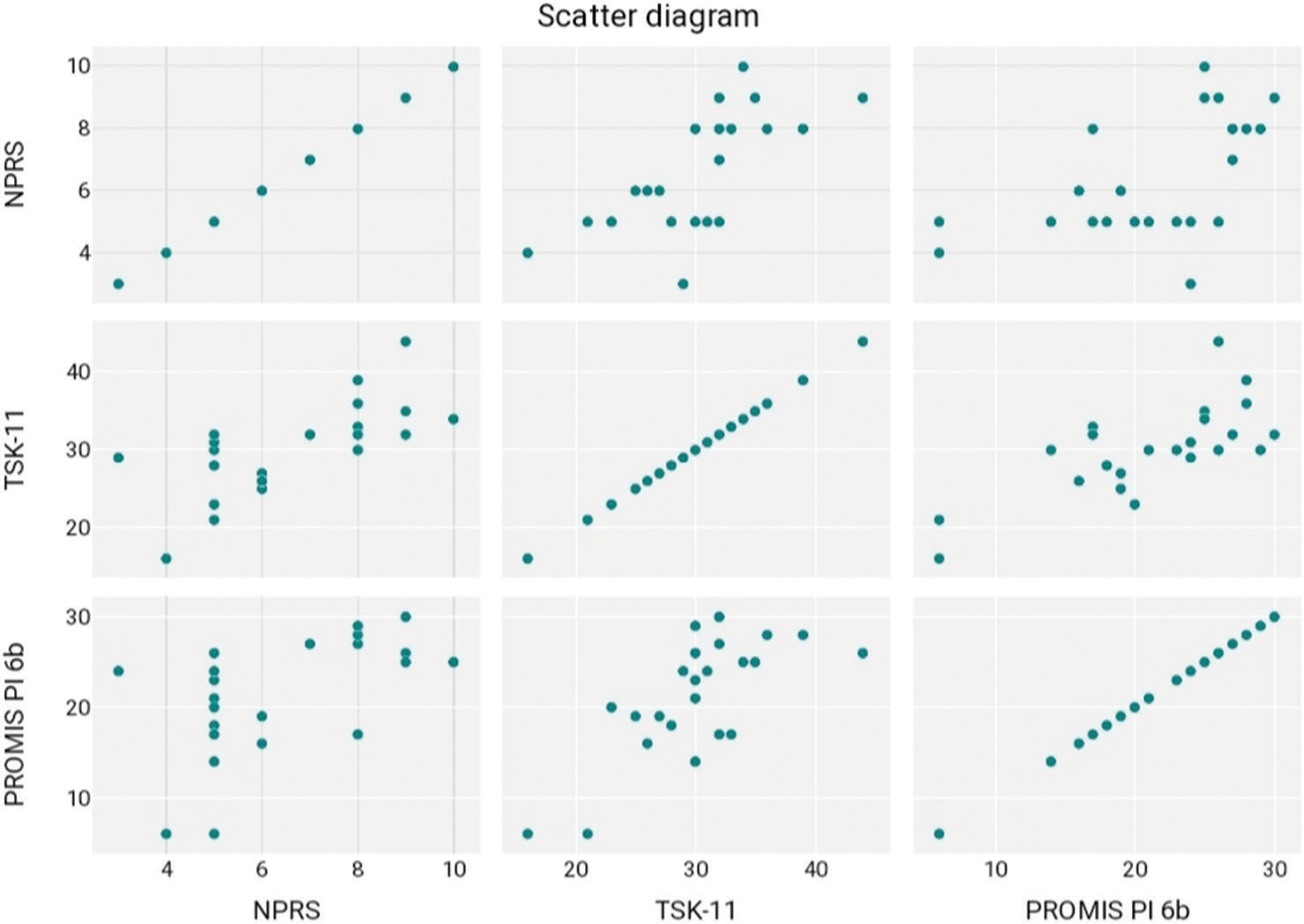
- Scatter plot matrix of correlation between pain severity, kinesiophobia, and pain interference. NPRS: Numerical pain rating scale, TSK-11: Tampa scale of kinesiophobia 11, PROMIS PI-6b: Patient-reported outcomes measurement information system pain interference-6b.
DISCUSSION
In this study, where 24 participants were included, 17 were female and seven were male. Our study observed that 29.2% of men and 70.8% of women were affected. Long et al. concluded that knee OA is more prevalent in females than males due to their different kinematics.[11] The average BMI of females and males was 28.3 and 25.6, respectively, which lies in the overweight category. Participants age ranged from 50 to 68 years. Vina and Kwoh conducted a study that corroborates our findings, indicating that obesity and advanced age may be precursors for knee OA.[12]
The median values of NPRS, TSK-11, and PROMIS PI-6b, respectively, are 6, 30, and 24. Each scale’s scores were connected, meaning that when one rose, so did the other scales, and vice versa. Negative or maladaptive psychological elements, such as fear/dread, are among the most significant of the many biopsychosocial components that influence how pain is experienced and manifested. To comprehend how some people’s acute pain develops into chronic pain and why pain and its results (such as incapacity) continue even after the tissue damage has healed, fear is thought to be a key element.[13]
As per Alshahrani et al., we also hypothesized that knee OA individuals demonstrated fear of movement based on TSK.[7] To explain the increasing amount of knee discomfort and pain, the fear of motion appears to be a coping mechanism. The study’s findings demonstrate a positive link between kinesiophobia, pain interference, and knee pain intensity, suggesting that as kinesiophobia rises, so does knee discomfort.
Limitations of the study
The results of this study can be extrapolated to females more than males, as we had an insufficient number of males.
CONCLUSION
In this pilot study, kinesiophobia increased with increasing extent of pain and pain interference in individuals with knee OA between the ages of 37 and 80.
RECOMMENDATIONS
Future studies can be done on a larger sample size in the male population and secondary knee OA individuals.
AUTHORS’ CONTRIBUTIONS
AKS conceived and designed the study, conducted research, provided research materials, and collected and organized data. UHM analyzed the data. AKS wrote the initial and final draft of the article and provided logistic support. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The research/study approved by the Institutional Review Board at JSS Medical College, number EC-CT-2018-0018, dated December 01, 2022.
DECLARATION OF PARTICIPANT CONSENT
The authors certify that they have obtained all appropriate participant consent forms. In the form, the participants have given their consent for their images and other clinical information to be reported in the journal. The participants understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Extracellular vesicles and their potential significance in the pathogenesis and treatment of osteoarthritis. Pharmaceuticals. 2021;14:315.
- [CrossRef] [PubMed] [Google Scholar]
- Physical activity and osteoarthritis: A consensus study to Harmonise self-reporting methods of physical activity across international cohorts. Rheumatol Int. 2017;37:469-78.
- [CrossRef] [PubMed] [Google Scholar]
- Knee osteoarthritis: Clinical update. KWX Communications Pvt Ltd. Available from: https://books.google.com/books/about/knee_osteoarthritis.html?id=nhyzdwaaqbaj [Last accessed on 2024 May 30]
- [Google Scholar]
- The relationships between pain beliefs and kinesiophobia and clinical parameters in Turkish patients with chronic knee osteoarthritis: A cross-sectional study. J Pak Med Assoc. 2019;69:823-7.
- [Google Scholar]
- Pain assessment using the NIH Toolbox. Neurology. 2013;80(11 Supplement 3):S49-53.
- [CrossRef] [Google Scholar]
- Pain interference and physical function demonstrate poor longitudinal association in people living with pain: A PROMIS investigation. Pain. 2017;158:1063.
- [CrossRef] [PubMed] [Google Scholar]
- Association between kinesiophobia and knee pain intensity, joint position sense, and functional performance in individuals with bilateral knee osteoarthritis. Healthcare. 2022;10:120.
- [CrossRef] [PubMed] [Google Scholar]
- Reliability and validity of Kannada version of Tampa scale of kinesiophobia (TSKKA-11)-a validation study. Indian J Physiother Occup Ther. 2022;16:15-9.
- [CrossRef] [Google Scholar]
- Translation and cross-cultural adaptation of Nepali versions of the patient-reported outcomes measurement information system (PROMIS®) pain intensity, pain interference, pain behavior, depression, and sleep disturbance short forms in chronic musculoskeletal pain. Qual Life Res. 2021;30:1215-24.
- [CrossRef] [PubMed] [Google Scholar]
- Jamovi (Version 2.3) [Computer Software] 2022. Available from: https://www.jamovi.org [Last accessed on 2024 Apr 05]
- [Google Scholar]
- Prevalence trends of site-specific osteoarthritis from 1990 to 2019: Findings from the global burden of disease study 2019. Arthritis Rheumatol. 2022;74:1172-83.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of osteoarthritis: Literature update. Curr Opin Rheumatol. 2018;30:160-7.
- [CrossRef] [PubMed] [Google Scholar]
- Role of kinesiophobia on pain, disability and quality of life in people suffering from chronic musculoskeletal pain: A systematic review. Br J Sports Med. 2019;53:554-9.
- [CrossRef] [PubMed] [Google Scholar]






