Translate this page into:
Total sacrectomy rehabilitation: Implementation of the international classification of functioning, disability, and health model – A case report
*Corresponding author: Alfredo A Lopes, Center for Rehabilitation Research, School of Health of Polytechnic of Porto, Porto Center University Hospital, Matosinhos, Portugal. adl@ess.ipp.pt
-
Received: ,
Accepted: ,
How to cite this article: Lopes AA, Mesquita I, Torres R. Total sacrectomy rehabilitation: Implementation of the international classification of functioning, disability, and health model – A case report. J Musculoskelet Surg Res. 2025;9:140-4. doi: 10.25259/JMSR_289_2024
Abstract
This study aims to outline an evaluative diagnostic process and intervention for a patient who underwent total sacrectomy based on the International Classification of Functioning, Disability, and Health (ICF) model. A 70-year-old male with a history of an aggressive sacral chordoma experiencing intense pain, constipation, and polyuria without the sensation of bladder filling, underwent a total sacrectomy. Two evaluations at two-time points were conducted 12 weeks apart. The patient then underwent an individualized rehabilitation program tailored to address impairments, activity limitations, and participation restrictions. The care plan was adjusted based on the patient’s health status and relevant personal and environmental factors. The Barthel Scale scores improved from 60 to 80. Motor scores on the American Spinal Injury Association scale increased from 62 to 66, while sensory scores for light touch improved from 86 to 96. However, pain scores remained stable at 86. Functional reach tests showed notable enhancements, with anterior reach increasing from 16.4 cm to 23.7 cm and lateral reach from 9.6 cm to 15.2 cm. The patient also showed progress in mobility, increasing the number of steps taken from 0 to 10. This case report highlights the positive therapeutic outcomes achieved, illustrating improvements in functional activities and patient independence, thereby underscoring the effectiveness of the ICF model in managing patients undergoing total sacrectomy.
Keywords
Health
Incapacity
Independency
Physiotherapy
Sacral chordoma
INTRODUCTION
Chordoma is a rare malignant bone tumor originating from ectopic remnants of notochordal tissue, predominantly found in the axial skeleton. It is more prevalent in males, particularly in the sacrococcygeal region, characterized by slow growth yet locally aggressive behavior.[1] The primary treatment for aggressive sacral chordomas involves total sacrectomy, which entails the complete removal of the sacrum at the L5/S1 level. Disruption of spinal-pelvic continuity post-surgery results in absolute spinal instability, necessitating reconstruction of the pelvic ring to establish a bilateral union between the lumbar spine and the iliac using techniques such as bone grafts, autologous grafts, autoclaved sacral pieces, or metallic prostheses.[2]
Although surgical mortality rates are low, post-operative morbidity is notable, often manifesting as decreased muscle strength and sensory function, along with urinary, sexual, and intestinal dysfunctions. Complications are more common with total sacrectomy, significantly impacting the patient’s quality of life.[2] Despite this, comprehensive studies on physiotherapy interventions following total sacrectomy are lacking.[3]
Given the limited research in this area, a detailed investigation utilizing the International Classification of Functioning, Disability, and Health (ICF) framework is warranted.[4] Recent discourse within the physiotherapy community has explored the potential of using the ICF to structure patient treatment plans, offering a valuable tool for clinical decision-making.[5]
This case report aimed to present an evaluative diagnostic process and intervention based on the ICF model for a patient who underwent total sacrectomy.
CASE REPORT
This is a case of a 70-year-old male, married and retired, standing at 165 cm and weighing 59 kg, with a body mass index of 22 kg/m2. He presented with chronic low back pain radiating to both legs. There was no significant medical history or prior surgical interventions.
Clinical findings and timeline
The patient experienced chronic low back pain with mechanical characteristics. A year ago, he began to feel intense pain radiating to his right lower limb, which responded well to conservative treatment. Approximately two months later, similar pain manifested in his left lower limb. Six months later, he noticed constipation and increased urination without the sensation of bladder filling. Subsequently, the patient underwent hospitalization, total sacrectomy, and colostomy, with sacrificed nerve roots during the surgery. The patient underwent evaluation at two distinct time points: Moment one (M1) occurred six weeks post-surgery and moment two (M2) occurred 12 weeks after the intervention in M1. During the initial objective assessment (M1), the International Standards for Neurological Classification of Spinal Cord Injury utilized the American Spinal Injury Association (ASIA) Impairment Scale (AIS) for classification.[6] The activities domain assessment involved tasks such as “sit-to-stand” and “stand-to-sit,” the anterior functional reach test (AFRT), the lateral functional reach test (LFRT),[7] and counting the number of steps taken. The Barthel Index was employed to evaluate activities of daily living (ADL) and functional independence.[8] The patient, who presented in a wheelchair, required assistance with transfers but demonstrated good orientation and collaboration. The patient was classified as having a complete lesion AIS A (no preservation of sensory or motor function in the sacral segments S4-5). Following the physiotherapy objective examination, similarities with cauda equina syndrome were noted, including sensory changes and flaccid paralysis of muscles of the bladder and intestine. During anteroposterior and mediolateral load transfers, the patient struggled with trunk balance, weight transmission to the feet, and difficulty assuming a standing position. The most critical assessments revolved around the “sit-to-stand” and “stand-to-sit” sequences, which the patient could not perform independently, requiring significant support from the physiotherapist. On the Barthel Index, the patient displayed limitations in ADL, including transfers, bathing, dressing, and mobility. Emotionally, prolonged hospital stays left the patient feeling discouraged, influencing his social interactions and raising concerns about the future.
Application of the ICF model
The ICF framework was employed to organize examination information, make judgments on findings, and guide decision-making for the patient’s management [Figure 1].[6,7]
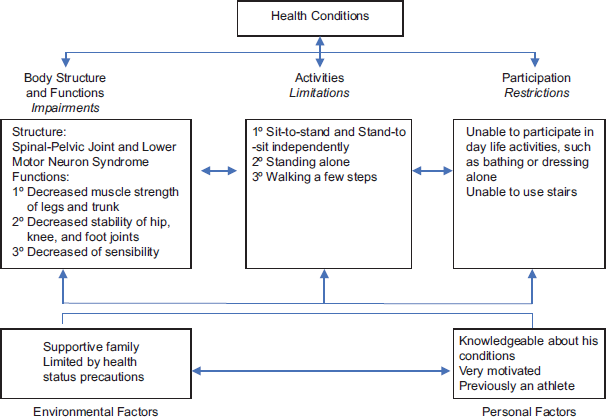
- Clinical judgments of the relationships and identification of the primary impairment of the patient into the International Classification of Functioning, Disability, and Health (ICF) model. Reprinted with permission from: ICF. Geneva, Switzerland: World Health Organization (Nº 318912).
The patient’s primary limitation was identified as the inability to independently perform “sit-to-stand” and “stand-to-sit” maneuvers, termed as his primary activity constraint. In addition, he encountered significant challenges in standing alone and walking a few steps, categorized as secondary and tertiary activity limitations. The reduced function of leg and trunk muscles directly impacted the patient’s ability to stand independently and stroll a short distance. This clinical correlation led to a reorganization of the model based on these interrelationships and the primary impairment identified. For the patient, achieving home independence and engaging in ADL were crucial components of his physical and psychological well-being. Prognostically, his target was to regain the ability to walk and perform routine tasks within a year.[3]
Diagnostic assessment
A lumbar magnetic resonance imaging scan revealed a lesion in the lumbosacral region involving the sacrum and soft tissues. A percutaneous echo-guided biopsy during hospitalization confirmed the diagnosis of chordoma. Bone scintigraphy displayed diffuse radiopharmaceutical hypofixation at the sacral level, consistent with a chordoma diagnosis, which indicated an unfavorable prognosis.
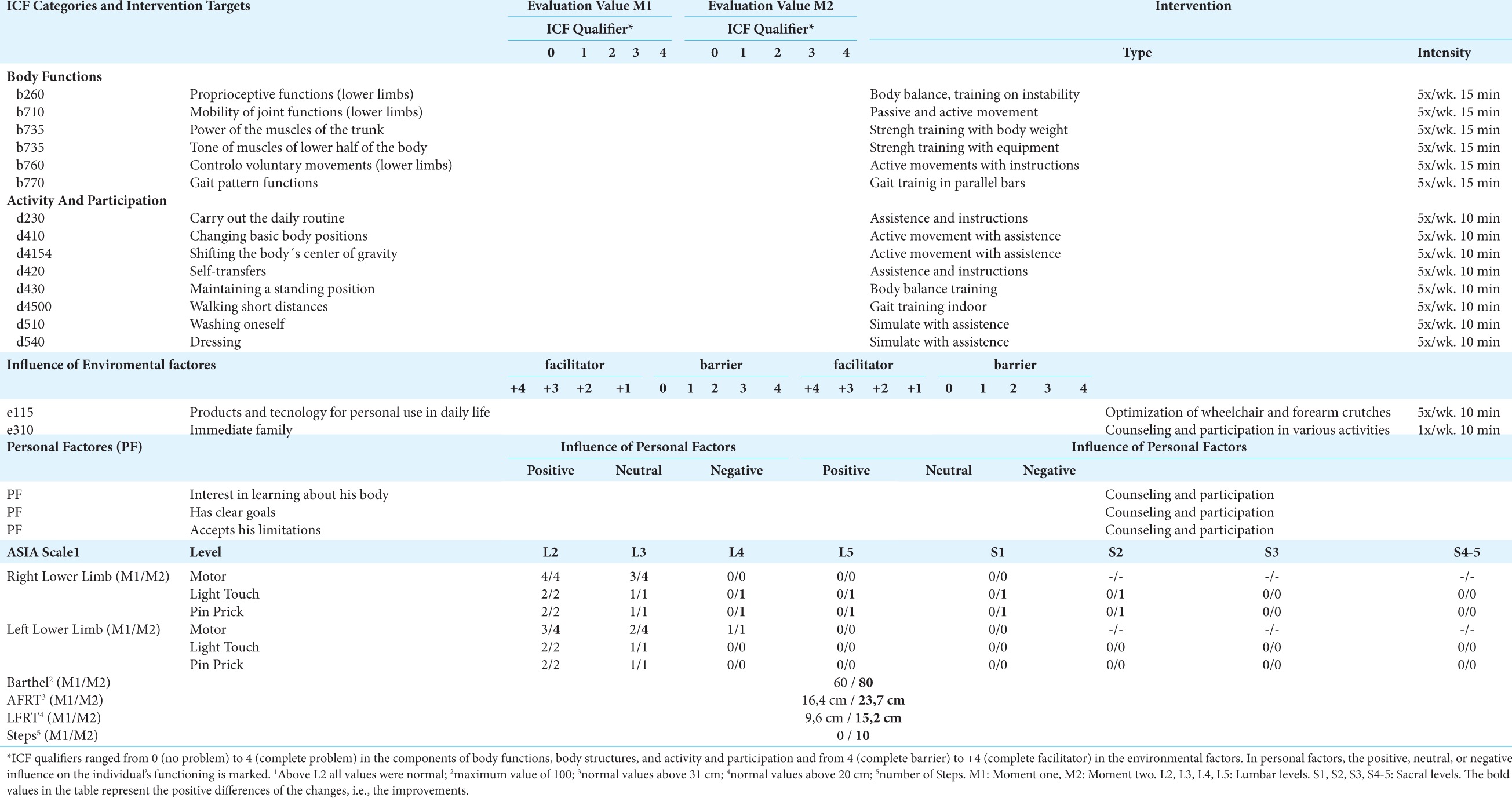
Therapeutic intervention
A comprehensive therapeutic plan was devised based on rehabilitation guidelines post-total sacrectomy.[3] Therapy sessions were scheduled five days a week for 12 weeks, each lasting approximately 180 min [Table 1].
Follow-up and outcomes
Positive outcomes were observed through postural and movement sequence analysis alongside assessments with specific instruments [Table 1].
Increased activation of stabilizing muscles in the abdominal core allowed for improved anteroposterior and mediolateral load transfers, as evidenced by improvements in the AFRT and the LFRT. Increased activation of lower trunk and leg muscles facilitated an improved extension pattern in the lower limbs. While the patient still required some support during “sit-to-stand” and “stand-to-sit” maneuvers, the need for assistance significantly decreased. The Barthel Scale reassessment indicated ongoing limitations in ADL, such as transfers, bathing, dressing, and mobility, although with reduced impact, leading to increased scores.
By the end of the 12-week treatment, the patient exhibited advancements in activities such as sit-to-stand and stand-tosit maneuvers, sitting posture, standing balance, and walking ten steps using a forearm walking stick.
The ICF Evaluation Display was utilized to visualize and evaluate the re-examination results, offering a comprehensive snapshot of the patient’s functional state to guide further treatment planning. ICF qualifiers were employed as a composite rating scale to assess the extent of issues related to specific ICF categories based on data gathered during assessments and patient interviews [Table 1].[9]
DISCUSSION
In this case report, significant changes were observed in voluntary muscle contraction strength and sensibility despite the challenges posed by removing the sacrum and sacrificing nerve roots (S1–S5).[1] The sacrum plays a critical role in supporting body weight and providing fixation for key muscles involved in locomotion and core stability. Surgical accesses compromising muscles such as the abdominals, glutes, piriform, abductors, iliopsoas, and pelvic floor muscles can impact overall function.[2] The primary goal of any intervention is to facilitate social and professional reintegration with maximum functionality and quality of life within the injury context. The ICF model was instrumental in guiding treatment decisions by assessing functional limitations, impairments, and environmental factors to optimize rehabilitation strategies.[6,7] The selection of primary impairments focused on strengthening lower limb and core muscles to improve stability, muscle function, and postural control.[10] As part of the therapeutic intervention, a combination of strength training, balance retraining, and postural re-education was implemented to enhance muscle activity, stability, and mobility.[10] The training focused on improving weight transference, trunk stabilization, and facilitating essential functional movements such as “sit-to-stand” and “stand-to-sit.”[10] Integrating educational components promoting independence in daily activities alongside functional training underscored a comprehensive approach to rehabilitation.[7]
While no changes were noted in the ASIA classification reflecting a complete spinal cord injury, notable improvements in motor strength and sensory perception were observed. Postural re-education and strength training enhanced muscle activation and stability, contributing to better postural control and mobility. The interactive elements of the ICF model allowed for a holistic assessment of the patient’s functional status, aiding in goal setting and treatment planning.
Despite the limitations of a single-case design and the scarcity of similar studies, the application of the ICF framework shows its utility in guiding comprehensive rehabilitation practices for patients undergoing total sacrectomy, highlighting the significance of patient involvement in decision-making processes for improved health outcomes and quality of life.
CONCLUSION
This case report demonstrates the efficacy of incorporating the ICF framework in the rehabilitation of patients’ post-total sacrectomy.
Patient perspectives
The patient was aware of the seriousness of his situation and accepted his limitations. He recognized that his lower-limb muscle strength and level of independence had improved, but he would always have many limitations in his quality of life and health status.
AUTHORS’ CONTRIBUTIONS
AAL created the intervention and treated the patient. IM and RT were heavily involved in the research and writing of the paper. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The research/study was approved by the Institutional Review Board at the Ethics Committee of the Santo António Hospital and University Center, Santo António Local Health Unit, Porto, Portugal (2022.19195) dated 19/12/2022.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published, and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Rehabilitation and functional result after total scapulectomy without protetization. Int J Med Rev Case Rep. 2023;7(Suppl 1):9-15.
- [CrossRef] [Google Scholar]
- Total sacrectomy and reconstruction with structural allografts for neurofibrosarcoma of the sacrum. A case report. J Bone Joint Surg Am. 2005;87:864-9.
- [CrossRef] [PubMed] [Google Scholar]
- Sacrectomy rehabilitation guidelines of royal national orthopaedic hospital. 2014. Available from: https://www.rnoh.nhs.uk/services/rehabilitation-guidelines [Last accessed on 2024 Mar 12]
- [Google Scholar]
- International classification of functioning disability and health ICF Geneva: World Health Organization. 2001. Available from: https://www.who.int/standards/classifications/international-classification-of-functioning-disability-and-health [Last accessed on 2024 Mar 12]
- [Google Scholar]
- Creating an interface between the International classification of functioning, disability and health and physical therapist practice. Phys Ther. 2010;90:1053-63.
- [CrossRef] [PubMed] [Google Scholar]
- Classifications in brief: American Spinal Injury Association (ASIA) impairment scale. Clin Orthop Relat Res. 2017;475(Suppl 5):1499-504.
- [CrossRef] [PubMed] [Google Scholar]
- Validation of a test battery to assess functional autonomy of adults with spinal cord injury. Rev Bras Educ Fís Esporte. 2014;28(Suppl 1):41-55.
- [CrossRef] [Google Scholar]
- Barthel index of activities of daily living. Nurs Res. 2015;64(Suppl 2):88-99.
- [CrossRef] [PubMed] [Google Scholar]
- Using a case report of a patient with spinal cord injury to illustrate the application of the International Classification of functioning, disability and health during multidisciplinary patient management. Phys Ther. 2010;90(Suppl 7):1039-52.
- [CrossRef] [PubMed] [Google Scholar]
- Bobath concepts: Theory and clinical practice in neurological rehabilitation United States: John Wiley and Sons; 2013.
- [Google Scholar]







