Translate this page into:
Seizure-related bilateral asynchronous displaced late presenting Delbet type I fractures: A case report and literature review
*Corresponding author: Khaled L. El-Adwar, Department of Orthopaedics Surgery and Traumatology, Hadra Orthopaedic University Hospital, Lambrouso, Alexandria, Egypt. khaled_eladwar@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: El-Adwar KL. Seizure-related bilateral asynchronous displaced late presenting Delbet type I fractures: A case report and literature review. J Musculoskelet Surg Res. 2025;9:134-9. doi: 10.25259/JMSR_402_2024
Abstract
Delbet type I transphyseal hip fractures without dislocation are extremely rare injuries. This is the first report of a bilateral case caused by seizures. A 4-year-old girl with global developmental delay, who walks supported, fell off her bed during an epileptic fit. The parents presented two weeks later, and radiographs revealed a displaced right Delbet type I transphyseal upper femoral separation. Under general anesthesia, surprisingly, the physis was reduced anatomically using the Leadbetter maneuver. Fixation was carried out with three smooth Kirschner wires (KWs), after which uneventful healing occurred. Sixteen months following the first injury, the girl had another seizure, which resulted in a buckle fracture of her left distal femur. Unfortunately, an identical left hip physeal injury was missed. On presentation three months later, stress radiographs showed non-union of the physis. Fortunately, again, the Leadbetter maneuver succeeded in reducing the physis, which was fixed using two smooth KWs. She was seen one year following the left hip surgery (2.5 years after the right hip surgery), and the left physis had united with no ischemic necrosis on both sides. The patient then resumed her ability to walk supported and sit cross-legged. A telephone call to the father six years post-surgery to the right hip and four years and six months post-surgery to the left hip confirmed that she was asymptomatic and maintained her previous abilities. Because of the COVID-19 pandemic, she could not attend for clinical and radiographic examinations.
Keywords
Hip fracture
Ischemic necrosis
Late presenting
Pediatric
Seizure
Traumatic separation of capital femoral epiphysis
Trauma
INTRODUCTION
Transphyseal separation of the upper femoral epiphysis (epiphysiolysis) is a rare entity of pediatric femoral neck fractures. Delbet first described this around the turn of the twentieth century.[1] He classified these fractures into four types: Where type I is a transphyseal fracture with or without femoral head dislocation, and type IV is a trochanteric fracture. Colonna later reported this in the English literature in 1929, who described 12 cases of pediatric femoral neck fractures.[2] In his article, he stated what seemed to be his and other authors’ opinion at the time: “We feel that separation of the epiphysis alone in very young children is an anatomical impossibility due to the thick plate of the cartilage covering the whole upper end of the femur.”[2] However, this statement proved false in the following years, where Delbet type I injuries were repeatedly reported due to high-velocity injuries such as falling from a height and road traffic accidents. However, several reports have shown that these injuries were rare among all Delbet types.[3-6]
The English literature has described seizure-related transphyseal hip fractures in only four articles.[7-10] Furthermore, the incidence of bilaterality is extremely rare and was first reported in 1975 (without seizure) by Milgram and Lyne.[11] The aim of presenting this case was to highlight the possibility of developing Delbet type I fractures following seizures after low-velocity injuries and to draw the attention of attending orthopedic surgeons to such rare injuries and that bilaterality is not impossible.
CASE REPORT
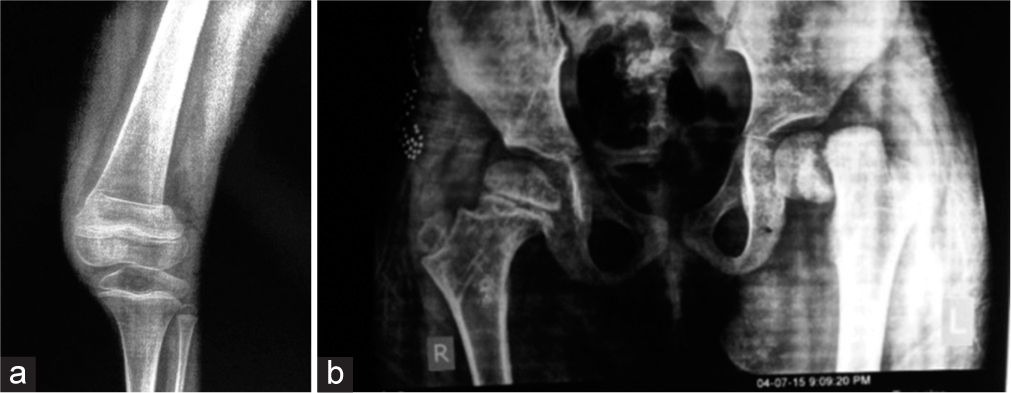
A 4-year-old girl with global developmental delay, who walks supported, fell off her bed during an epileptic fit. The parents presented the patient two weeks later, and radiographs and computed tomography (CT) scans revealed a markedly displaced right Delbet type I transphyseal upper femoral separation, without femoral head dislocation, with loose bony fragments within the joint mimicking heterotopic ossification [Figures 1 and 2]. The three-dimensional CT coronal image showed what seemed like rounding of the metaphysis [Figure 3]. The options of treatment were discussed with the parents, which were essentially to reduce the fracture, whether closed or open, and internally fix it, with the possibility of development of nonunion and avascular necrosis (AVN). Closed reduction, however, seemed to be a remote possibility. Surprisingly, the physis was reduced anatomically under general anesthesia using the Leadbetter maneuver [Figure 4], after which the limb was held on a fracture table. After that, fixation was carried out with three smooth KWs [Figure 5], and the hip was immobilized in a spica cast for 1.5 months. She was followed up for seven months when the KWs were removed. At the time, the patient had resumed her pre-injury ambulatory status, and uneventful healing had occurred with no sign of AVN [Figure 6].

- Anteroposterior radiograph of both hips showing right Delbet type I fracture.
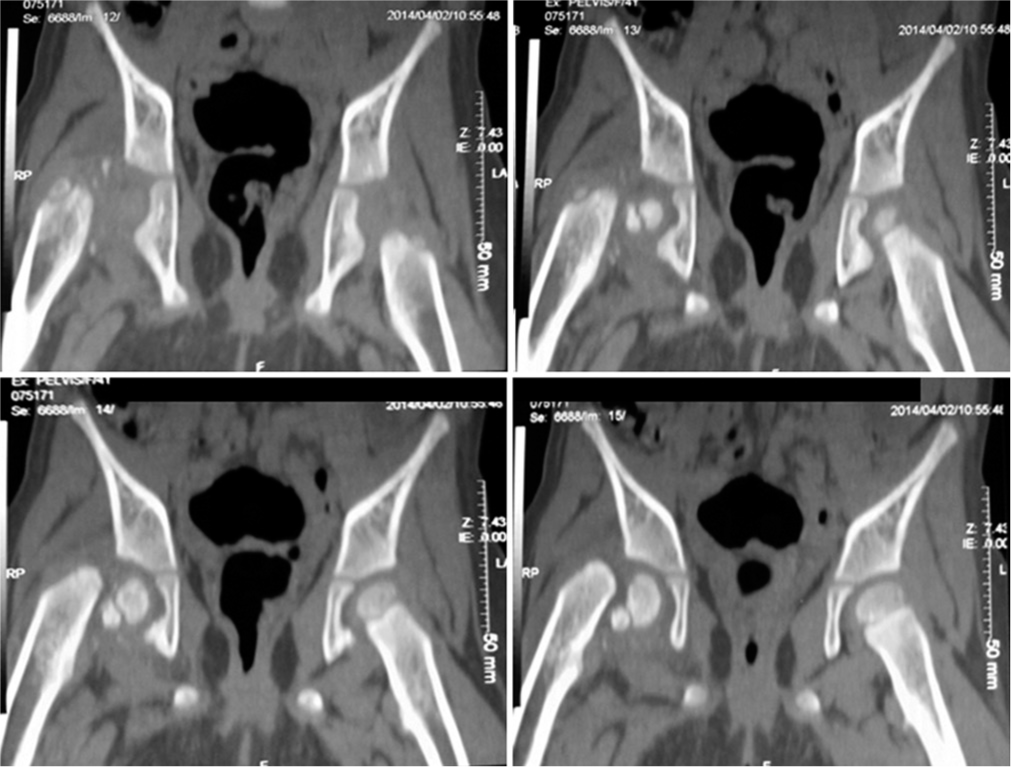
- Coronal computed tomography images show superior displacement of the metaphysis with flecks of calcification and a possibly intact medial retinacular hinge.

- Smooth surface of the distal fragment’s metaphysis, indicating early sclerosis of the distal fragment.
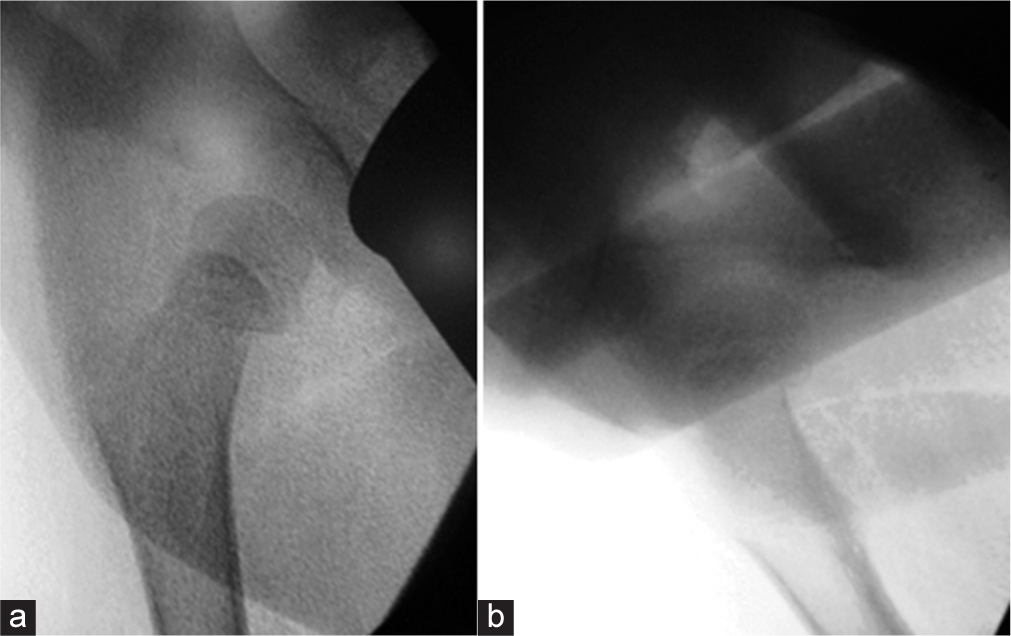
- Anatomical reduction in (a) anteroposterior and (b) lateral fluoroscopy images.
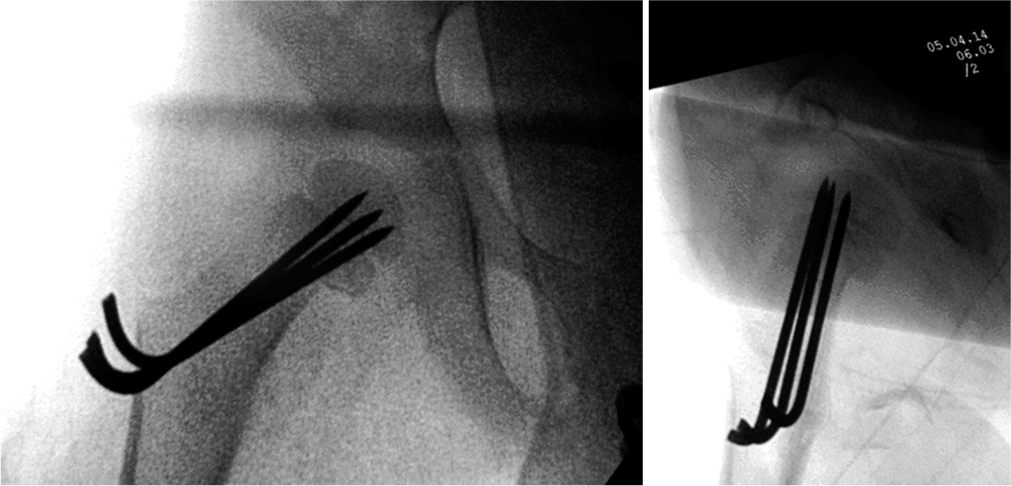
- Fixation using three smooth Kirschner wires.
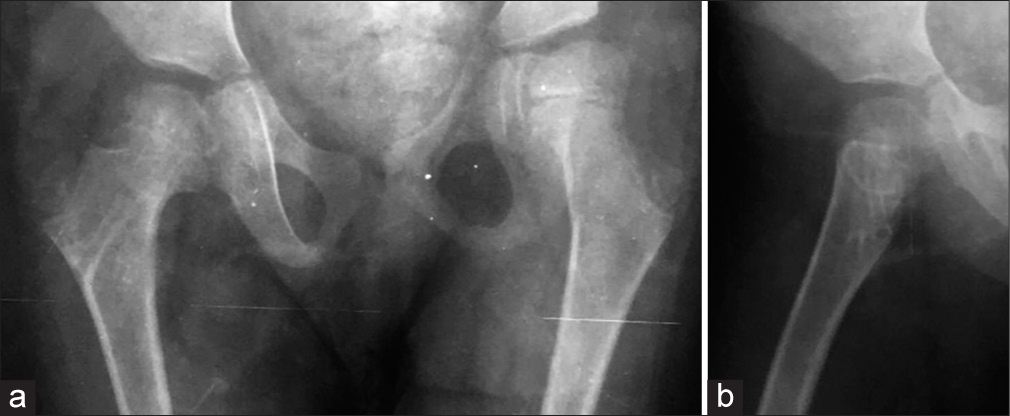
- (a) Anteroposterior and (b) lateral follow-up radiographs 7 months post-op, right after Kirschner wires removal, with no signs of avascular necrosis.
Sixteen months following the first injury, the girl had another seizure, which resulted in a buckle fracture of her left distal femur. Unfortunately, this drew the attention of the treating physician, and an identical left hip physeal injury was overlooked, though hip radiographs were taken at the time [Figure 7a and b]. On presentation three months later, stress radiographs showed no evidence of union of the physis. Axial CT images showed what seemed like sclerosis of the left metaphyseal fragment and the union of the old right transphyseal fracture [Figure 8].
- (a) Anteroposterior radiograph showing an old left supracondylar femoral buckle fracture and (b) ipsilateral Delbet type I fracture 3-month post-injury.
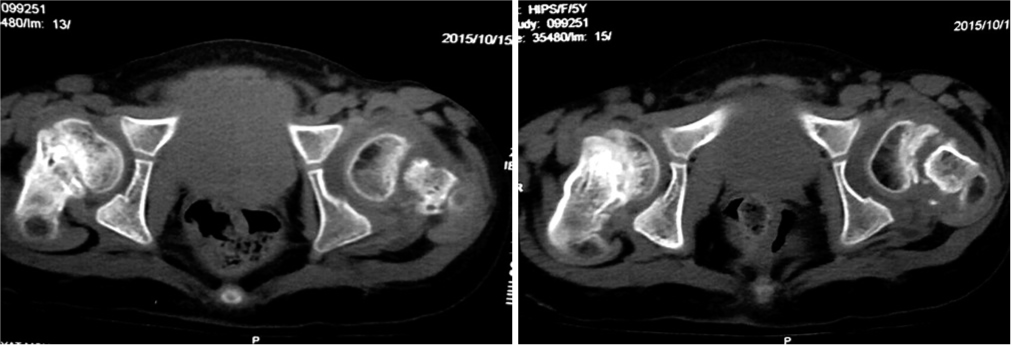
- Computed tomography axial images show a left transphyseal injury with what seems like sclerosis of the proximal femoral metaphysis. These images also confirmed the union of the right side in an acceptable position.
Because of the significant delay in presentation on the left, it was thought that this side would need an open reduction and probably carry a grave prognosis. Fortunately, again, the Leadbetter maneuver succeeded in reducing the physis, which was fixed using two smooth KWs followed by cast immobilization for a period similar to that on the right side.
She was seen one year following surgery to the left hip (2.5 years post-surgery to the right hip). This delay was due to the parents’ non-compliance with the follow-up regimen. The wires were removed then, where the left physis had united with no ischemic necrosis on both sides [Figure 9a and b]. The patient then resumed her ability to walk supported and was able to sit cross-legged. A telephone call to the father six years post-surgery to the right hip and four years and six months post-surgery to the left hip confirmed that she was asymptomatic and maintained her previous abilities.
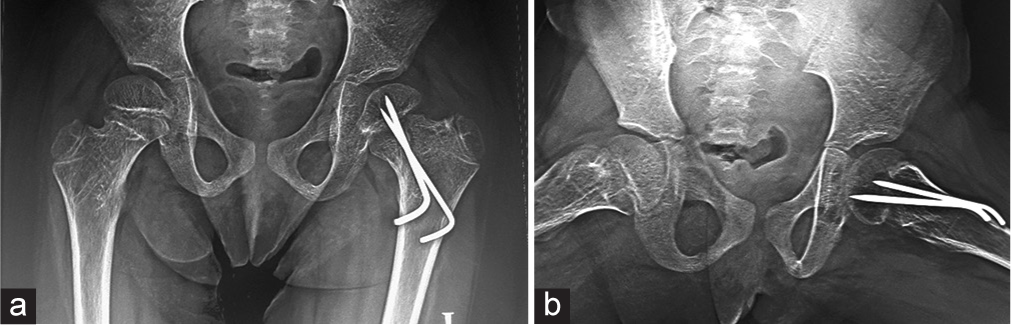
- (a) Anteroposterior and (b) frog lateral radiographs of both hips 1 year following surgery on the left and 2.5-year post-surgery on the right, showing the union of the left hip fracture in an anatomical position, with no signs of avascular necrosis bilaterally. Kirschner wires were removed at the time.
DISCUSSION
Delbet type I pediatric transphyseal femoral neck fractures are rare injuries, which have been reported in 0.03–37.5% among all four Delbet types.[3-6,12] These injuries are prone to AVN, premature epiphyseal closure, and coxa vara.[13] The causation of AVN is multifactorial and has been studied extensively, and risk factors have been looked at. Non-modifiable risk factors include fracture type, displacement, and patient’s age at injury, whereas modifiable risk factors include time to reduction, quality, and method of reduction, stability of fixation, and capsular decompression.[14]
Factors related to the development of AVN
Delbet fracture type
Some studies have found that more proximal fractures were more susceptible to AVN. Moon and Mehlman looked at their 25 femoral neck fractures in 23 years and identified 360 patients in a PubMed search covering a 38-year duration. Their meta-analysis found that fracture type was a significant predictor of AVN. Delbet types I, II, and III were 15, 6, and 4 times, respectively, more likely to develop AVN than type IV fractures. Their rates of AVN were 38% in type I, 28% in type II, 18% in type III, and 5% in type IV fractures.[14]
Moreover, a systematic review and meta-analysis of six studies by Alkhatib et al., including 231 fractures, found that Delbet types I and II were 2.4 times more associated with AVN than types III and IV.[15] Furthermore, in Riley’s series, AVN was reported in 50% (2 of 4) of their type I injuries.[16]
Delbet type I fracture itself is divided into those with or without hip dislocation, both being significantly different, with the former being more prone to AVN. Some studies did not mention the number of type I fractures associated with hip dislocation.[2,5,6,16] Canale and Bourland reported on 61 cases with an average 17-year follow-up, 5 of whom (8.2%) had type I fractures with hip dislocations, all of whom developed AVN.[17]
Heiser and Oppenheim in their series of 40 fractures, 7 of which were type I (17.5%), all 7 ending up in complications, AVN in 2 (28.6%), coxa vara in 2 (28.6%), and premature epiphyseal closure in 3 (42.8%).[5] A 7.5-year-old boy with a type I injury with hip dislocation was described by Tsirikos et al. He was operated upon 4-h post-injury through anterior and posterior approaches. The epiphysis was found without soft-tissue attachments. This is probably why the patient developed AVN radiologically two months post-injury.[18]
This contrasts with a 4-year-old patient reported by Mass et al. with dislocation, in whom no AVN was seen after a follow-up of two years. They thought that an intact lateral retinacular hinge between the femoral head and neck was behind the success of open reduction and internal fixation. This was seen on initial anteroposterior radiographs, with a relatively narrower lateral physeal gap. Favorable anatomy, with a vascular soft-tissue bridge joining the head and neck, seemed to result in a favorable clinical result.[19] This is consistent with the current report, in which there was definitely an intact soft-tissue bridge in both hips, maintaining vascularity to the femoral heads resulting in no AVN after follow-up, despite the delay in treatment.
Age at injury
Moon and Mehlman found that age was a significant predictor of AVN, where older children were 1.14 times more likely to develop AVN for each year of increasing age.[14] Heiser and Oppenheim also found the average age for AVN to be 13.5 years, compared to 6.5 years for those without this complication.[5] Likewise, Riley et al., in a retrospective review of 44 fractures (4 type I, i.e., 9%), reported that age ≥11 years was their only statistically significant predictor of AVN. Age was considered among other factors, including fracture type and displacement, time to reduction, reduction type and quality, and whether a decompression was performed or not.[16] The findings in the latter two studies are in agreement with the preserved femoral head blood supply in our 4-year-old patient.
Time to reduction
On the one hand, Shrader et al., in a retrospective study of 20 consecutive patients of Delbet types I to III fractures (2 type I, i.e., 10%), were the first to document a significant association between delayed treatment (i.e., more than 48 h after injury) and the occurrence of AVN (P = 0.05), after a mean folow-up of seven years.[4] Furthermore, Bukva et al., in a retrospective review of 28 patients of Delbet types I to IV fractures (1 type I, i.e., 3.6%), who were followed up for an average of nine years, found an optimal time for a lower incidence of AVN to be 12 h (P = 0.014).[12]
Pavone et al. followed up eight patients for an average of 39.2 months (types I–IV), of whom three were type I (37.5%). Although they treated all their patients within 12 h following admission, they had a 25% rate of AVN, indicating that time to reduction was not the sole factor involved.[6] Likewise, Astur et al., in 29 of all Delbet types, reported 73.3% good results if patients were operated upon within the first 24 h, while only 42.8% of the results were good among patients who were treated later.[10]
On the other hand, Riley et al. proved that early reduction did not reduce rates of AVN.[16] Moreover, Alkhatib et al. found that there was no statistically significant difference between early (<24 h) and late (>24 h) interventions in relation to the development of osteonecrosis.[15] This is consistent with a case report by Atmaca et al. in an 11-month-old infant with Delbet type I fracture without dislocation, where there was a delay of 1.5 months before open reduction and KW fixation. After a follow-up of 1.5 years, there was no evidence of AVN.[9] This is in agreement with findings in the currently reported patient, who had a delay of 18 days on the right and three months on the left side before treatment, with no signs of AVN bilaterally, after radiological follow-up of one year on the left and 2.5 years on the right side.
Fracture displacement and quality of reduction and fixation
Norouzi and Naderi, who reported 20 fractures with 1 Delbet type I (5%), stated that AVN was related to fracture displacement and quality of reduction and fixation.[3] Alkhatib et al. found a positive relation between fracture displacement and AVN. They found that displaced fractures were 3.8 times more associated with AVN than nondisplaced ones.[15] In the current case, neither developed AVN despite the significant displacement of both fractures. Shrader et al. also reported a significant relationship between the occurrence of AVN and poor/fair reduction (P < 0.01).[4]
Method of reduction
In their meta-analysis, Alkhatib et al. found no statistically significant difference in the risk of AVN between open and closed reduction of femoral neck fractures in children.[15] Furthermore, in Riley et al.’s series, although open reduction cases trended toward a higher incidence of AVN compared with closed reduction, this did not reach a significant level (P = 0.068).[16]
Hip decompression
Unequivocally, Bukva et al. showed positive effects of hip decompression on the incidence of AVN, with similar efficiency of open and needle techniques. They found a lower incidence of AVN in patients in whom decompression was performed (P = 0.044).[12] However, Riley et al. found no bearing of decompression on their incidence of AVN.[16]
Bilaterality
Bilateral epiphysiolysis (Delbet type I fractures) was first reported by Milgram and Lyne in 1975 in two patients, one with myelomeningocele and the other with battered baby syndrome, both younger than 1.5 years of age.[11] The time lag before presentation was not reported in both patients. The former developed bilateral mild varus deformity and bilateral heterotopic ossification, and the latter developed unilateral nonunion.
Bilateral Delbet fractures are extremely rare. Upadhyay et al. reported on two cases with bilateral Delbet type II fractures in 11 and 8-year-old children after falling from a height, the latter associated with a pelvic injury. Despite the fact that the injury was diagnosed six weeks later in the former, both cases were treated by closed reduction and screw fixation with uneventful healing and no AVN.[20]
The current case report represents the first description of bilateral asynchronous late presenting Delbet Type I fractures (without dislocation), with a delay before presentation in both.
Seizure-related injuries
Four previous reports of such injuries have been published, with two cases in one publication (i.e., five hips in total), with a delay in treatment in two hips ranging from 3 days to 1.5 months [Table 1]. The current case is the fifth report and the first bilateral case. It shares the absence of complications with that published by Atmaca et al., despite a delay in treatment of 1.5 months.[9]
| Case Report | Age | Timing of reduction | Type of reduction+fixation | Duration of follow-up | Complications |
|---|---|---|---|---|---|
| Ballal et al. 2008 (2 cases) | 22 months 9 years | Both cases<24 h | CR+2 KWs+hip spica CR+single screw+hip spica |
Both cases 18 months | None |
| Aoudi et al. 2009 | 5 months | 3 days | CR+hip spica | 19 months | None |
| Astur et al. 2010 | 6 months | No comment | Hip spica | 2 years | AVN+Coxa vara |
| Atmaca et al. 2012 | 11 months | 1.5 months | OR+2 KWs+hip spica | 18 months | None |
| Current study 2023 (Bilateral) | 4 years | Right 18 days, left 3 months | CR+KWs (3 Right/2 Left)+hip spica | 6 years 4 years+6 months |
None |
CR: Closed reduction, OR: Open reduction, KWs: Kirschner wires, AVN: Avascular necrosis
In the current report, the presence of synovial fluid within the hip around these fractures prevented them from uniting after that length of time, allowing free manipulation, contrary to all extra-articular epiphyseal injuries, which readily unite even if displaced. Despite bilateral significant initial displacement in both fractures and delay in treatment, the age of the patient and a possibly intact medial retinacular hinge in both hips (seen on radiographs in retrospect) might be the recognizable factors that made the patient escape AVN. Furthermore, the quality of fracture reduction helped optimize the outcome.
Future research has to look into diagnosing prior to treatment the unforeseeable intact vascular soft-tissue bridge, which is a principal factor in preserving blood supply to the site of injury and the femoral head and determining the likelihood of the prognosis.
CONCLUSION
Transphyseal hip fractures (Delbet type I), without dislocation, are extremely rare injuries. This is the first report of a bilateral case caused by seizures occurring asynchronously. Even if presenting late, closed reduction should be attempted and, if successful, might result in a favorable outcome.
ETHICAL APPROVAL
The research/study was approved by the Institutional Review Board at the University of Alexandria, Egypt, number 0306422 (IRB no 00012098/FWA no 00018699), dated 1st March 2024.
DECLARATION OF PATIENT CONSENT
The author certifies that he has obtained all appropriate patient consent forms. In the form, the parents have given their consent for her images and other clinical information to be reported in the journal. The parents understand that her name and initials will not be published, and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Femoral neck fractures in children: A follow-up study of 19 cases. Eur J Trauma Emer Surg. 2009;35:124-6.
- [CrossRef] [PubMed] [Google Scholar]
- Femoral Neck Fractures in pediatric patients. 30 years experience at a level 1 trauma center. Clin Orthop Relat Res. 2007;454:169-73.
- [CrossRef] [PubMed] [Google Scholar]
- Fractures of the hip in children: A review of forty cases. Clin Orthop Relat Res. 1980;149:177-84.
- [CrossRef] [Google Scholar]
- Surgical treatment with cannulated screws for pediatric femoral neck fractures: A case series. Injury. 2019;50(Suppl 2):S40-4.
- [CrossRef] [PubMed] [Google Scholar]
- Traumatic transepiphyseal separation of the upper femoral epiphysis following seizures in two children with cerebral palsy. J Bone Joint Surg. 2008;90B:382-4.
- [CrossRef] [PubMed] [Google Scholar]
- Traumatic transepiphyseal separation of the upper femoral epiphysis following seizures in a 5-month-old child: A case report. Childs Nerv Syst. 2009;25:1039-41.
- [CrossRef] [PubMed] [Google Scholar]
- Neglected femoral neck fracture in patient with seizure: A case of a delayed fixation of type 1A fracture in 11-month-old infant. Eur J Orthop Surg Traumatol. 2012;22(Suppl):S173-6.
- [CrossRef] [PubMed] [Google Scholar]
- Correlation between avascular necrosis and early stabilization of proximal femoral fractures in childhood. Rev Bras Ortop. 2010;45:426-32.
- [CrossRef] [PubMed] [Google Scholar]
- Epiphysiolysis of the proximal femur in very young children. Clin Orthop Relat Res. 1975;110:146-53.
- [CrossRef] [PubMed] [Google Scholar]
- Femoral neck fractures in children and the role of early hip decompression in final outcome. Injury. 2015;46(Suppl 6):S44-7.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for avascular necrosis after femoral neck fractures in children: 25 Cincinnati cases and meta-analysis of 360 cases. J Orthop Trauma. 2006;20:323-9.
- [CrossRef] [PubMed] [Google Scholar]
- Early versus late treatment of paediatric femoral neck fractures: A systematic review and meta-analysis. Int Orthop. 2019;43:677-85.
- [CrossRef] [PubMed] [Google Scholar]
- Earlier time to reduction did not reduce rates of femoral head osteonecrosis in pediatric hip fractures. J Orthop Trauma. 2015;29:231-8.
- [CrossRef] [PubMed] [Google Scholar]
- Fracture of the neck and intertrochanteric region of the femur in children. J Bone Joint Surg Am1977;. ;59:431-43.
- [CrossRef] [Google Scholar]
- Transpyseal fracture-dislocation of the femoral neck: A case report and review of the literature. J Orthop Trauma. 2003;17:648-53.
- [CrossRef] [PubMed] [Google Scholar]
- Dislocation of the hip with traumatic separation of the capital femoral epiphysis: Report of a case with successful outcome. Clin Orthop Relat Res. 1980;146:184-7.
- [CrossRef] [Google Scholar]
- Simultaneous bilateral fractures of femoral neck in children-mechanism of injury. Injury. 2004;35:1073-5.
- [CrossRef] [PubMed] [Google Scholar]






