Translate this page into:
Challenges of biplane double-supported screw fixation technique for osteosynthesis of femoral neck fractures in the South Indian population
*Corresponding author: Prajwal P. Mane, Department of Orthopaedics, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Manipal -576104, Karnataka, India. pjlmane@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Middha I, Hegde A, Joseph N, Mane PP, Shetty C, Rao SB, et al. Challenges of biplane double-supported screw fixation technique for osteosynthesis of femoral neck fractures in the south Indian population. J Musculoskelet Surg Res. 2025;9:236-43. doi: 10.25259/JMSR_361_2024
Abstract
Objectives:
Controversy exists in the management of neck of femur fractures. Insufficient reduction, unstable fixation, and poor–quality osteoporotic bone result in complications. This study was conducted to evaluate the functional and radiological outcomes of femoral neck fractures managed by the biplane double-supported screw fixation (BDSF) technique in the South Indian population, which is predominantly short profile.
Methods:
A prospective study was conducted among subjects aged (18–60 years) with femoral neck fractures over 2 years. All participants underwent fixation with the BDSF technique. Patients were followed up regularly for 12 months postoperatively. Harris hip score and radiological assessment were assessed. Complications such as screw backout, implant failure, and avascular necrosis (AVN) were assessed during the follow-up.
Results:
Of the 60 patients, 43 (71.7%) were males and 17 (28.3%) females. The mean age was 44 ± 11.2 years. Pair-wise post hoc test was statistically significant (P < 0.001). Harris hip scores decreased with the patient’s age increasing. The radiological union was noted in 49 cases. Eleven (18%) cases had non-union. Seven (11%) had AVN of the femoral head, four (6%) had screw backout with varus collapse, and 3 had (5%) varus mal-reduction.
Conclusion:
The functional outcomes of femoral neck fractures managed by the biplane BDSF technique were excellent. This technique was a safe, viable, and cost-effective option for neck of femur fractures in old and young populations. Further comparative studies and randomized control trials would be beneficial in providing evidence.
Keywords
Biplane double-supported screw fixation
Femoral neck
Fracture
Functional outcome
Osteoporosis
Radiological outcome
INTRODUCTION
About 50% of all fractures around the hip are fractures of the neck of the femur. The incidence of hip fractures is between 40–50% for females and 12–22% for males worldwide.[1] Increased incidence of osteoporosis, age-related eyesight loss with poor neuromuscular coordination, lifestyle changes, sedentary behavior, and greater life expectancy have caused an upsurge in the frequency of these fractures.[1-3] Most fractures in the neck of the femur are due to low-energy mechanisms in elderly or osteoporotic individuals. In contrast, these fractures are often associated with high-energy mechanisms in the younger population.
The primary aim of treating such fractures is to restore function with minimal morbidity. There are various methods to treat femoral neck fractures, such as triangle screw fixation, inverted triangle screw fixation, dynamic screw fixation, hemiarthroplasty, as well as a total hip replacement depending upon the age, condition of the bone, the displacement of fracture in the subject, time since fracture and surgeon’s choice.
While late avascular necrosis (AVN), which can range from 9% to 32%, depends on a variety of biological and surgical variables, fixation failure, which can range from 9% to 30%, is mostly caused by inadequate hold of screws in osteoporotic bone.[3-7] Fixation failure might be reduced by enhancing the internal fixation construct’s main stability. Osteosynthesis treatment problems are caused by inadequate reduction, unstable fixation, and osteoporotic bone.
The three cancellous screws commonly used today to fix the femoral neck in a parallel fashion act along the femoral neck axis, which leads to unsatisfactory outcomes in 20– 42% of cases.[1,2,5,8] Conventional screw fastening methods have a significant failure rate due to several biomechanical problems.[8-10] The structure is not stable under varus stress, there is no sliding action, and three parallel screws cannot be positioned when the screws’ entrance site is shifted into the robust diaphyseal cortex. The three cancellous screws used in conventional femoral neck fixation enter at or very close to the greater trochanter’s fragile, thin cortex. These screws are placed parallel to the axis of the neck of the femur and to each other. Even without cortical reinforcement, the screws are frequently inserted into the brittle cancellous bone at the axis of the femoral neck. The implant behaves like a static beam on an elastic basis, as with conventional techniques, since there are not two strong supporting points. The soft cancellous bone implements the elastic base. The evolving concepts and techniques have led to a continuous debate on how to handle these fractures.[11-15] The major causes of treatment issues include inadequate reduction, unstable fixation, and osteoporotic bone stock.[14-16]
BDSF is a recently developed innovative technique that offers better cortical screw support and greater fixation strength.[8-10] Three cannulated screws may be positioned with entry sites significantly farther out inside the thicker cortex of the proximal diaphysis according to the idea of biplane placement, which enhances their beam function and cortical support. As per Sengodan et al., the anatomical variables of the hip joint, such as neck shaft angle, neck width, head diameter, acetabular angle, horizontal offset, and vertical offset, in the Indian population differ from those of the Western population.[17] In their study, they also mentioned differences amongst the Indian population based on the different regions to which the study population belonged. This diversity makes it challenging to reproduce similar results of fractures in the neck of femur fixation across various populations.
The study aimed to assess the functional and radiological results of fixing a neck femur fracture using the BDSF technique. Due to the lack of knowledge about the aforementioned approach in the South Indian population and the paucity of literature on it, this study was taken up.
MATERIALS AND METHODS
This prospective study was done in a tertiary care center between 2020 and 2022. Institutional ethical approval was obtained. The following patients were included.
Inclusion criteria and exclusion criteria
Garden type 1 and fractures of the femur neck in those above 18 years of age and Garden type 3 and 4 with age between 18 and 60 years of age were included whereas fractures presenting late (>1 week), associated fractures of lower limbs, neck of femur fracture with established osteoarthritis hip, and neck of femur fracture with failure of osteosynthesis were excluded.
Patient’s general details were collected from the hospital records using a proforma. Patients with neck or femur fractures fulfilling the inclusion criteria underwent BDSF by a single surgeon. Post-operative follow-up was done at 1, 3, 6, 9, and 12 months. The functional outcome of each participant was evaluated using the Harris hip score (HHS) and three crucial indicators for independent living: pain relief (good, poor), mobility (good, poor), and the ability to put on socks and shoes (easy, difficult), which were assessed both physically and verbally. Post-operative radiographs were used to assess the quality of reduction, union, screw position, screw complications like backout, breakage, osteolysis, and signs of non-union or AVN.
Operative technique
All participants underwent fixation with the BDSF technique for femoral neck fractures using three 6.5 mm cannulated cancellous screws. The anatomical reduction was achieved by traction, internal rotation, and slight abduction. It was confirmed with Gardens’ alignment index and Lowell’s S lines in AP and lateral views under fluoroscopic assistance. Joystick manipulation was done to aid reduction whenever needed.
A straight lateral incision of 6–10 cm beginning below the level of the greater trochanter was made. The 6.5 mm cannulated cancellous screws are positioned in the frontal plane at a significantly increased angle using the BDSF technique. The distal and middle screws are in tangential contact with the femoral neck cortex distally. All three screws are positioned in two vertical oblique planes (in lateral view). The two planes are oblique with respect to the frontal plane and diverge in the direction of the femoral head. The dorsal oblique plane is where the distal screw is placed. The ventral oblique plane is where the middle and proximal screws are put.
Off the three screws, the guide wire for the distal screw is first placed with an entry point which is about 5–7 cm distal to the base of the greater trochanter and slightly anterior on the femoral cortex. The guide wire is placed such that it makes an angle of about 150–160° with the femoral shaft. The direction of the wire is anteriorly at the distal end and goes posteriorly at the proximal end (sharp end of the guide wire). The wire will be in the posterior aspect of the femoral head in the lateral view.
The second guide wire is the middle one. This guide wire entry point is about 2–4 cm proximal to the distal wire and posteriorly placed on the femoral shaft. This wire makes an angle of about 130–140° and is directed posteriorly at the distal end and goes anteriorly at the proximal end (sharp end of the guide wire). The wire will be in the anterior one-third of the femoral head in the lateral view.
The proximal-most guide wire is placed last. This guide wire entry point is about 1–2 cm proximal to the middle guide wire and is in the posterior aspect of the femoral shaft. This guide wire should be parallel to the middle guide wire in both antero-posterior and lateral views. The guide wire will be placed anteriorly in the femoral head in the lateral view. After satisfactory placement of the guide wires, the proximal and middle screws are first placed, followed by the distal and inferior most screws [Figure 1a-c].
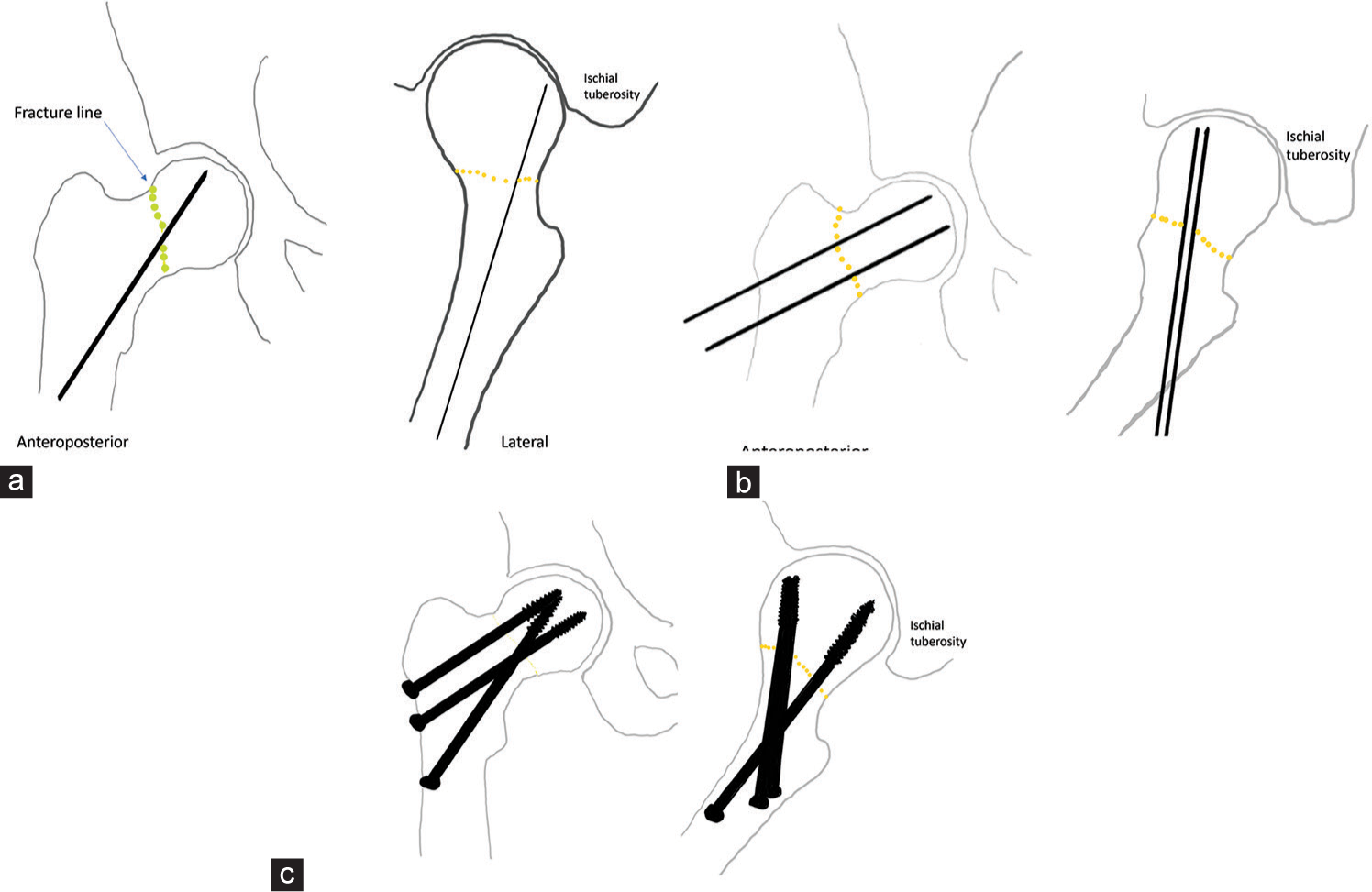
- (a) Line diagram showing the fractured neck of the femur and the passage of 1st guide wire (inferior and posterior) in both anteroposterior and lateral views. (b) Line diagram showing the fractured neck of the femur and the passage of 2nd and 3rd guide wire in both anteroposterior and lateral views. (c) Line diagram showing the fractured neck of the femur fixed with 3 6.5 mm cannulated cancellous screws.
Data analysis: The data from MS Excel were entered into Jamovi for analysis. The Harris hip scores of the patients assessed at various intervals of the post-operative period were not found to follow normal probability distribution (as observed by the Kolmogorov–Smirnov test). However, the age distribution of the patients followed normal probability distribution. Hence, descriptive statistics were presented as mean, standard deviation, median, and interquartile range. The Friedman test was used to assess whether repeated measures of the HHS differed significantly among the patients during various assessment intervals in the post-operative period. Post hoc analysis of pair-wise analysis was done using the Durbin–Conover test. The Mann–Whitney U-test was used to test whether the HHS differed significantly among males and females at a particular time interval in the postoperative period. Karl Pearson’s coefficient of correlation was used to find the correlation between the ages of the patients and their HHS at various periods of assessment during the post-operative period. A P < 0.05 was taken as a statistically significant association.
RESULTS
Of the 60 patients in this study, 43 (71.7%) were males and 17 (28.3%) were females. The mean age of the patients was 44 ± 11.2 years, ranging from 24 to 64 years.
Functional outcome
In the present study, the mean functional outcomes at 1 month and 3 months were 43.5 and 58.9, respectively, which improved as the follow-up duration increased. At 6 months, the mean functional outcome was 75.48; at 9 months, 84.52 and at 12 months, the functional outcome was noted to be 91.15, which falls into the excellent category.
The HHSs were found to significantly increase among the patients at every time interval of assessment during the post-operative period (P < 0.001). Pair-wise post hoc test was statistically significant with P < 0.001 [Table 1].
| Time interval of assessment during the post-operative period | No. of participants | HHSs | Friedman test value | P-value | |
|---|---|---|---|---|---|
| Median | IQR (Q1, Q3) | ||||
| 1st month | 60 | 42.4 | (34.4, 51.9) | ||
| 3rd month | 60 | 58.7 | (48.3, 68.3) | ||
| 6th month | 60 | 77.9 | (68.9, 82.9) | ||
| 9th month | 60 | 84.0 | (79.1, 89.0) | ||
| 12th month | 60 | 92.5 | (87.3, 95.1) | 233.5 | <0.001 |
HHS: Harris hip score, IQR: Inter quartile range
The distribution of the median HHS among the patients with intra-capsular fracture neck of the femur during various intervals of the post-operative period (n = 60) was analyzed. The median HHS was found to increase among the patients at every time interval of assessment during the post-operative period [Figure 2], which indicated that the patient’s functional outcomes were improving at every interval of post-operative follow-up.
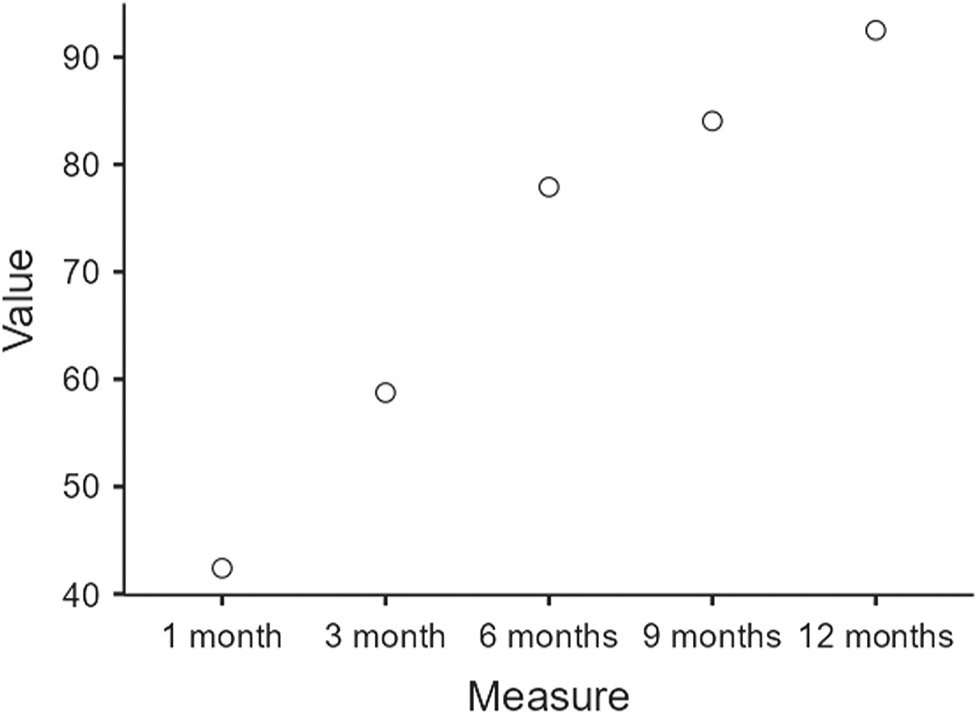
- Distribution of the median Harris hip score among the patients with intra-capsular fracture neck of the femur during various intervals of the post-operative period (n=60).
The HHSs did not significantly vary with the patient’s sex during the various assessment intervals in the post-operative period [Table 2].
| Time interval of assessment during the post-operative period | Sex | No. of participants | HHSs | Z-value | P-value | |
|---|---|---|---|---|---|---|
| Median | IQR (Q1, Q3) | |||||
| 1st month | Males | 43 | 40.5 | (33, 50) | ||
| Females | 17 | 50.7 | (40.1, 57.3) | 1.838 | 0.066 | |
| 3rd month | Males | 43 | 58.5 | (47.2, 69) | ||
| Females | 17 | 59.8 | (54.3, 66.2) | 0.599 | 0.549 | |
| 6th month | Males | 43 | 77.5 | (66, 83) | ||
| Females | 17 | 78.0 | (69.5, 82.8) | 0.459 | 0.646 | |
| 9th month | Males | 43 | 82.5 | (78.9, 88.5) | ||
| Females | 17 | 86.6 | (82, 91.6) | 1.444 | 0.149 | |
| 12th month | Males | 43 | 92.5 | (86.7, 94.5) | ||
| Females | 17 | 92.8 | (88.7, 96.5) | 1.067 | 0.286 | |
HHS: Harris hip score, IQR: Inter quartile range
The HHS was found to decrease with the increasing age of the patients. This negative correlation between ages and the HHS of the patients was significant at the assessment done at the end of the 3rd month (r = −0.216, P = 0.022) and at the end of the 12th month of the post-operative period (r = −0.259, P = 0.046) among the patients [Table 3].
| Time interval of assessment during the post-operative period | Pearson correlation (r) between age and HHS among the patients | P-value |
|---|---|---|
| 1st month | −0.216 | 0.097 |
| 3rd month | −0.295 | 0.022 |
| 6th month | −0.186 | 0.156 |
| 9th month | −0.219 | 0.092 |
| 12th month | −0.259 | 0.046 |
HHS: Harris hip score
No significant difference was found between results and males and females or between people of different age brackets. In the study, 93% had good pain relief and 7% had poor pain relief. In the study, 90% had good mobility and 10% had poor mobility.
Radiological outcome
The radiological union was noted in 49 (81%) cases. Eleven (18%) cases did not go on to unite, which further needed to be converted to hemiarthroplasty/total hip arthroplasty. Seven patients (11%) had AVN of the femoral head, four patients (6%) had screw backout with varus collapse, which did not unite, and three patients (5%) had varus mal-reduction but went on to unite [Figures 3 and 4].
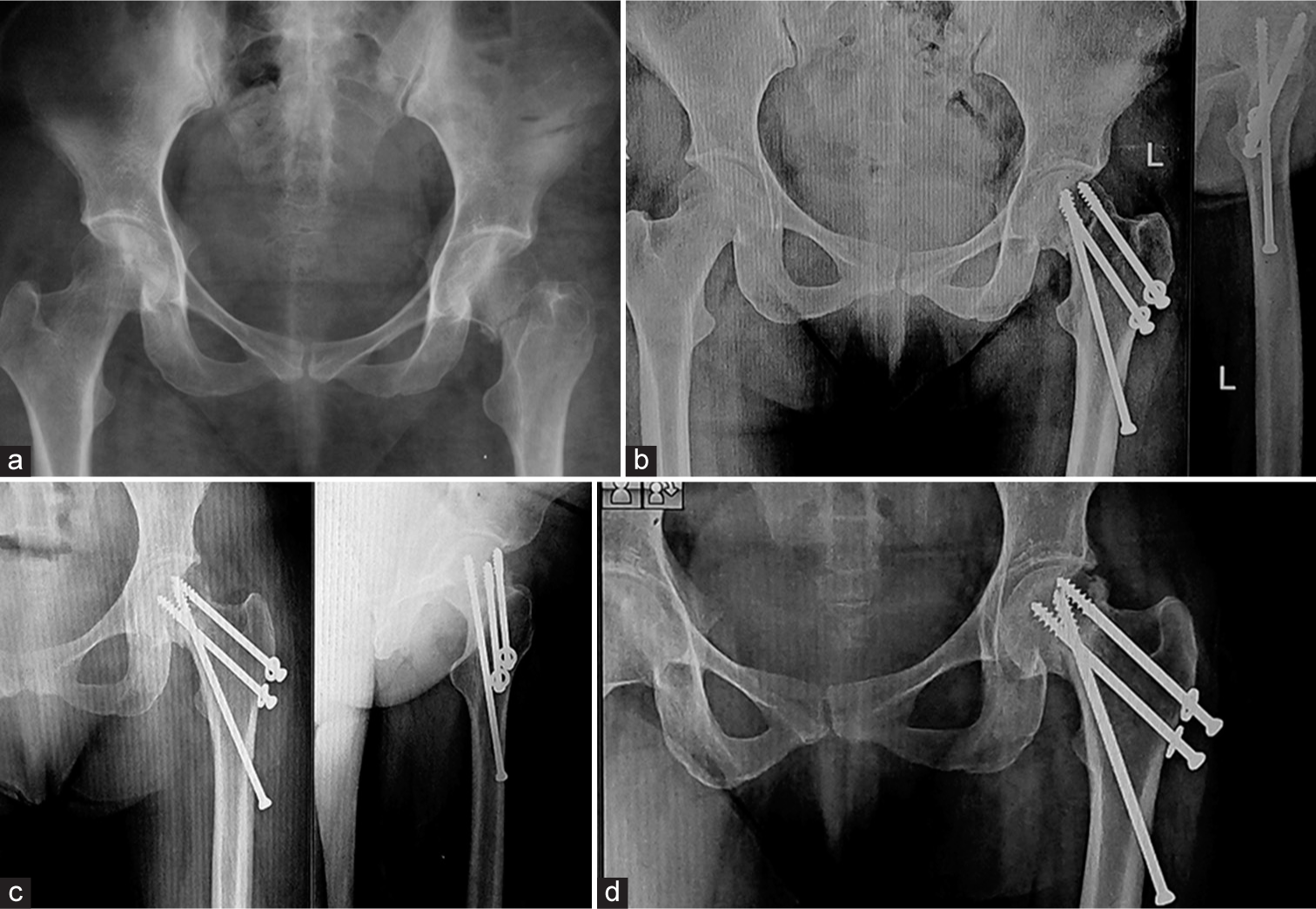
- (a) Radiograph showing left side neck of femur fracture. (b) Immediate postoperative AP and lateral radiographs. (c) Six months follow-up radiograph, AP and lateral, showing fracture union. (d) One year follow-up radiograph showing good union.

- (a) Radiograph showing right side neck of femur fracture. (b) Immediate postoperative AP and lateral radiographs. (c, d) Six months follow-up radiographs, AP and lateral, showing varus collapse of the head and screw back out.
DISCUSSION
With the increase in the aging population, the incidence of femoral fractures is rising worldwide. It is a common practice to fix the femoral neck with three cancellous screws placed parallel to the femoral neck axis and parallel to one another. However, studies have shown that in 20–42% of cases, these procedures fail to provide good results and are biomechanically weak when loading happens across the joint.[18,19] The BDSF technique makes use of the idea of a biplane arrangement of three screws at an acute angle to overcome problems with the conventional method. The patient’s bone quality is of least concern since the two firm implant supporting sites and their oblique location enable the body weight to be safely transferred from the head fragment onto the diaphysis. Due to their location, the screws may glide under tension with less risk of being displaced. In terms of fracture consolidation, the results obtained with the BDSF approach are significantly better than those obtained with traditional fixation techniques.
The BDSF approach provides accurate fixation, prompt recovery, and outstanding long-term results. Being biomechanically more stable, they allow early weight bearing when compared to conventional screw fixation techniques.[20,21] The factors which make BDSF more biomechanically stable are as follows:
The angle of the screws and the purchase of the screws in stronger distal cortical bone.
The screws are spaced out widely over the lateral cortex of the proximal femur reducing the screw density and distributing the stress and load over a larger area. In conventional screw technique, three-four screws are placed in a smaller area owing to increased stress/load at a specific area, which may result in iatrogenic fracture. Furthermore, in the conventional screw technique, the screws are placed more in the metaphyseal cancellous region, which is inferior to the distal cortical bone with respect to handling stress and load.
The position of the BDSF screws permits them to slide under loading/stress at minimal risk of displacement.[20,21]
Our results were consistent with the results published by other authors [Table 4]. Even though, as per Dhivya and Nandhini, the average neck length of the Indian population is lesser when compared to the Western population, in a few of our cases, the distal screw length measured was more than 120 mm, which was not readily available in our operation theatre.[22] Due to this issue, a few of our cases had to be converted to the conventional technique.
| Author | Total Patients | Union | Non- union |
Average | Poor HHS | Fair HHS | Good HHS | Excellent HHS | Complications |
|---|---|---|---|---|---|---|---|---|---|
| Hawam et al[11] | 20 | 18 | 2 | 88.6 | 2 | 3 | 6 | 9 | Fixation failure: 2 |
| Filipov,[16] | 88 | 27 | 61 | 87.6 | 10 | 20 | 21 | 37 | Screw back out: 1 |
| Sami et al.[23] | 27 | 25 | 2 | 94.8 | 1 | 1 | 2 | 23 | AVN: 3 Screw back out: 3 |
| Kalia et al.[24] | 25 | 25 | 0 | 81.2 | 3 | 4 | 9 | 9 | Femoral head chondrolysis: 1 |
| Filipov O et al.[21] | 207 | 200 | 7 | 86.2 | 24 | 21 | 37 | 125 | Pseudoarthrosis: 1 Fixation failure: 5 AVN: 1 |
| Our study | 60 | 43 | 17 | 92.5 | 4 | 7 | 20 | 29 | AVN: 7 Screw back out: 4 Varus collapse: 3 |
BDSF: Biplane double-supported screw fixation, HHS: Harris hip score, AVN: Avascular necrosis
Another challenge we faced was drilling the distal-most guide wire tangentially to the distal femoral neck cortex. The strong cortical bone tends to deflect the flimsy guide wire, preventing its proper placement. Getting the guide wire in the correct trajectory is the most crucial step in the BDSF technique. We advise the usage of thicker and stronger guide wires to get the right trajectory. We overcame this issue using a 2.5 mm thick long K-wire instead of a guide wire to get the right trajectory.
Although the BDSF technique provides multiple benefits, such as better biomechanical stability and better cortical, it also comes with drawbacks, such as difficulty in getting the precise arrangement of the guide wires, which at first glance may appear challenging but can be learned over time with proper attention to the steps of the procedure and planning for the surgery. As discussed before, the South Indian population’s neck length is smaller compared to the other ethnicities, so BDSF can be a good alternative procedure for neck of femur fracture fixation. However, in a few patients, the availability of screws longer than 120 mm becomes challenging, which may result in switching over to the conventional fixation technique.
CONCLUSION
The functional outcomes of femoral neck fractures managed by the BDSF technique were excellent. The improvement was not influenced by age and sex. Most subjects had good union, functional scores, and pain-free mobility. BDSF technique gives overall satisfactory functional and radiological outcomes.
Authors’ contributions
IM, AH, PPM, and SR conceived and designed the study, conducted research, provided research materials, and collected and organized data. NJ, AH, and PPM analyzed and interpreted data. CS, IM, and PPM wrote the initial and final draft of the article and provided logistic support. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
Ethical approval
The research/study was approved by the Institutional Review Board at KASTURBA MEDICAL COLLEGE, MANGALORE, number IEC KMC MLR 12-2020/421, dated December 24, 2020.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Conflicts of interest
There are no conflicting relationships or activities.
Financial support and sponsorship: This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Rockwood and green’s fractures in adults United States: Lippincott Williams and Wilkins; 1991.
- [Google Scholar]
- Anthropometric analysis of femur in South Indian population. Biomed Pharmacol J. 2020;13:167-73.
- [CrossRef] [Google Scholar]
- Anthropometric study of proximal femur geometry and its clinical application. Ann Natl Acad Med Sci. 2018;54:203-15.
- [CrossRef] [Google Scholar]
- Avascular necrosis after internal fixation of intracapsular hip fractures; a study of the outcome for 1023 patients. Injury. 2009;40:1143-6.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. J Bone Joint Surg. 1994;76:15-25.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term outcome of patients with avascular necrosis, after internal fixation of femoral neck fractures. Injury. 2003;34:525-8.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence of fracture-healing complications after femoral neck fractures. Clin Orthop Relat Res. 2007;458:175-9.
- [CrossRef] [PubMed] [Google Scholar]
- The method of biplane double-supported screw fixation (BDSF) at femoral neck fractures-principle and clinical outcomes. J IMAB Annu Proc Sci Pap. 2013;19:423-8.
- [CrossRef] [Google Scholar]
- Cortical screw support in femoral neck fractures. A radiographic analysis of 87 fractures with a new mensuration technique. Acta Orthop Scand. 1993;64:289-93.
- [CrossRef] [PubMed] [Google Scholar]
- Optimum configuration of cannulated hip screws for the fixation of intracapsular hip fractures: A biomechanical study. Injury. 2004;35:136-41.
- [CrossRef] [PubMed] [Google Scholar]
- Role of Biplane double support screw fixation for fracture neck of femur in elderly population. Al-Azhar Int Med J. 2020;1:81-4.
- [CrossRef] [Google Scholar]
- Fractures and dislocations of the hip In: Canale ST, ed. Campbell's operative orthopedics. Philadelphia, PA: Mosby-Elsevier; 2008. p. :3237-308.
- [CrossRef] [Google Scholar]
- Risk factors for nonunion in patients with intracapsular femoral neck fractures treated with three cannulated screws placed in either a triangle or an inverted triangle configuration. J Bone Joint Surg Am. 2013;95:61-9.
- [CrossRef] [PubMed] [Google Scholar]
- Finite element analysis of different internal fixation methods for the treatment of Pauwels type III femoral neck fracture. Biomed Pharmacother. 2019;112:108658.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical evaluation of the reconstruction of the calcar femorale in femoral neck fractures: A comparative finite element analysis. J Int Med Res. 2022;50:1-11.
- [CrossRef] [PubMed] [Google Scholar]
- Biplane double-supported screw fixation (F-technique): A method of screw fixation at osteoporotic fractures of the femoral neck. Eur J Orthop Surg Traumatol. 2011;21:539-43.
- [CrossRef] [PubMed] [Google Scholar]
- Anthropometric analysis of the hip joint in South Indian population using computed tomography. Indian J Orthop. 2017;51:155-61.
- [CrossRef] [PubMed] [Google Scholar]
- Intracapsular fractures of the femoral neck. Results of cannulated screw fixation. J Bone Joint Surg Am. 1994;76:1793-803.
- [CrossRef] [PubMed] [Google Scholar]
- Internal fixation versus hemiarthroplasty for displaced fractures of the femoral neck in elderly patients with severe cognitive impairment. J Bone Joint Surg Br. 2005;87:523-9.
- [CrossRef] [PubMed] [Google Scholar]
- Non-parallel screw fixation for femoral neck fractures in young adults. J Clin Orthop Trauma. 2017;8:220-4.
- [CrossRef] [PubMed] [Google Scholar]
- Femoral neck fracture osteosynthesis by the biplane double-supported screw fixation method (BDSF) reduces the risk of fixation failure: Clinical outcomes in 207 patients. Arch Orthop Trauma Surg. 2017;137:779-88.
- [CrossRef] [PubMed] [Google Scholar]
- A study of certain femoral metrics in south Indian population and its clinical importance. Int J Sci Stud. 2015;3:132-5.
- [Google Scholar]
- Biplane double supported screw fixation for femoral neck fracture in young adults: A prospective cohort study. J Orthop. 2022;33:117-23.
- [CrossRef] [PubMed] [Google Scholar]
- Role of biplane double supported screw fixation for fracture neck femur in elderly population: A prospective study. Open Orthop J. 2018;12:12.
- [CrossRef] [Google Scholar]






