Translate this page into:
Barriers to compliance with the Ponseti method for childhood clubfoot management in developing nations: A systematic review
*Corresponding author: Jia Xuan Ong, IMU University, Clinical Campus, Seremban, Malaysia - 70300, Kuala Lumpur, Malaysia. 00000034257@student.imu.edu.my
-
Received: ,
Accepted: ,
How to cite this article: Xuan Ong J, Yi Lim J, Thisinayagam S, Mohd Iznee M, Ikram MA. Barriers to compliance with the Ponseti method for childhood clubfoot management in developing nations: A systematic review. J Musculoskelet Surg Res. doi: 10.25259/JMSR_461_2024
Abstract
Congenital clubfoot, a condition that affects 1–2 in 1000 live births globally, is a significant musculoskeletal congenital disability. The Ponseti method has proven to be the gold standard in non-surgical treatment for congenital clubfoot and has expanded worldwide in the 21st century. Despite the procedure’s low cost and high success rate, there are still incidences of patients defaulting on treatment. This study aimed to determine the barriers to clubfoot treatment in selected developing nations worldwide. A systematic literature search from 2000 to 2024 was performed using PubMed, Scopus, ScienceDirect, and Google Scholar databases. A total of 2135 articles on barriers to clubfoot treatment were initially recognized, with 15 studies that met the inclusion criteria and were included in the final analysis after screening. This study yielded 2525 participants: 150 physicians and 2375 caregivers of children with clubfoot. Among the 2525 participants, 675 dropped out of the studies. Family factors were the most frequently mentioned reason for dropping out (n = 757). This was followed by the doctor or healthcare factors (n = 687) and the economic factors (n = 685). Four hundred sixty-one participants were not compliant with geographical factors; 197 were not compliant with the Ponseti method due to logistic factors. This was then followed by patient factors (n = 132), socio-cultural factors (n = 83), and finally, the other factors (n = 2). Our systematic review explored the barriers to treating clubfoot among children in developing nations. It proposed solutions to overcome the obstacles, as understanding them is vital for successfully implementing the treatment program.
Keywords
Barriers
Bracing
Children
Clubfoot
Compliance
Developing nations
Ponseti
INTRODUCTION
Clubfoot, also referred to as congenital talipes equinovarus, is characterized by feet that are inwardly and downwardly rotated, impacting approximately 1–2/1000 live births worldwide, with 80% born in developing countries.[1-4] When left untreated, it can lead to lifelong deformity, disability, and social stigma, delaying access to education and employment.[2,5]
The early initiation of treatment, mainly using the Ponseti method, has shown promising outcomes in correcting deformity, boasting a success rate of over 90% when applied correctly. Thus, it is also considered the gold standard for treating clubfoot worldwide.[1-3,6,7] It has been indicated to be economical and easy to implement. Despite the effectiveness of this method, adherence to treatment protocols, including the crucial use of abduction braces, remains a significant challenge, particularly in resource-limited settings.[3,7]
In many developing regions, clubfoot treatment is hindered by a complex interplay of factors. These barriers often include a lack of knowledge and understanding, financial constraints, limited healthcare infrastructure, transportation problems, inadequate medical personnel training, and cultural misconceptions. Moreover, the scarcity of resources and limited public health initiatives exacerbate these challenges, leading to delayed or suboptimal treatment outcomes. Several studies on barriers to clubfoot treatment were performed in other countries, such as India, Uganda, Bangladesh, Peru, Brazil, China, Chile, and Guatemala.[2,3,8-20] One of the studies was conducted in Uganda, discussing the challenges caused by poor infrastructure, including the lack of clinical resources and facilities, forcing the families to travel long distances to seek treatment.[5,8]
Our systematic review focuses on exploring the barriers to treating clubfoot among children in developing nations, as understanding these obstacles is vital for successfully implementing treatment programs. In doing so, the need for comprehensive approaches will be highlighted to overcome the barriers and improve the children’s quality of life.
MATERIALS AND METHODS
Study design
A systematic literature review was carried out and documented based on the preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines.[21] The study protocol was registered in PROSPERO with ID CRD42024498072.
Study method
A search strategy is presented in Table 1. Five authors individually searched PubMed, Scopus, ScienceDirect, and Google Scholar databases to identify articles for subsequent evaluation by assessing the titles and abstracts. Every article on the barriers to clubfoot treatment using the Ponseti method among children in developing nations was reviewed, and critical data were extracted. The articles were selected for further reading to identify the barriers to clubfoot treatment.
| No | Keywords | Number of articles | Search fields |
|---|---|---|---|
| PubMed | |||
| 1 | Clubfoot AND barriers AND children | 28 | ((“clubfoot”[MeSH Terms] OR “clubfoot”[All Fields] OR “clubfeet”[All Fields]) AND (“barrier”[All Fields] OR “barrier s”[All Fields] OR “barriers”[All Fields]) AND (“child”[MeSH Terms] OR “child”[All Fields] OR “children”[All Fields] OR “child s”[All Fields] OR “children s”[All Fields] OR “childrens”[All Fields] OR “childs”[All Fields])) AND (2000:2024[pdat]) |
| 2 | (barriers OR challenges OR factors) AND clubfoot AND treatment AND Ponseti | 260 | (“barrier”[All Fields] OR “barrier s”[All Fields] OR “barriers”[All Fields] OR (“challenge”[All Fields] OR “challenged”[All Fields] OR “challenges”[All Fields] OR “challenging”[All Fields]) OR (“factor”[All Fields] OR “factor s”[All Fields] OR “factors”[All Fields])) AND (“clubfoot”[MeSH Terms] OR “clubfoot”[All Fields] OR “clubfeet”[All Fields]) AND (“therapeutics”[MeSH Terms] OR “therapeutics”[All Fields] OR “treatments”[All Fields] OR “therapy”[MeSH Subheading] OR “therapy”[All Fields] OR “treatment”[All Fields] OR “treatment s”[All Fields]) AND (“Ponseti”[All Fields] OR “Ponseti s”[All Fields]) |
| 3 | (barriers OR challenges OR factors) AND clubfoot AND developing | 177 | ((“barrier”[All Fields] OR “barrier s”[All Fields] OR “barriers”[All Fields] OR (“challenge”[All Fields] OR “challenged”[All Fields] OR “challenges”[All Fields] OR “challenging”[All Fields]) OR (“factor”[All Fields] OR “factor s”[All Fields] OR “factors”[All Fields])) AND (“clubfoot”[MeSH Terms] OR “clubfoot”[All Fields] OR “clubfeet”[All Fields]) AND (“develop”[All Fields] OR “develope”[All Fields] OR “developed”[All Fields] OR “developer”[All Fields] OR “developer s”[All Fields] OR “developers”[All Fields] OR “developing”[All Fields] OR “developments”[All Fields] OR “develops”[All Fields] OR “growth and development”[MeSH Subheading] OR (“growth”[All Fields] AND “development”[All Fields]) OR “growth and development”[All Fields] OR “development”[All Fields])) AND (2000:2024[pdat]) |
| Scopus | |||
| 1 | Clubfoot AND barriers AND children | 29 | Clubfoot AND barriers AND children |
| 2 | Clubfoot AND barriers AND Ponseti AND children | 23 | Clubfoot AND barriers AND Ponseti AND children |
| ScienceDirect | |||
| 1 | Clubfoot AND barriers AND children | 192 | Clubfoot AND barriers AND children |
| 2 | Clubfoot AND barriers AND Ponseti AND children | 22 | Clubfoot AND barriers AND Ponseti AND children |
| Google Scholar | |||
| 1 | Clubfoot AND barriers AND Ponseti AND children AND parents AND relapse | 364 | Clubfoot AND barriers AND Ponseti AND children AND parents AND relapse |
| 2 | Clubfoot AND deformity AND barriers AND children AND (plaster OR brace) | 1040 | Clubfoot AND deformity AND barriers AND children AND (plaster OR brace) |
| Total | 2135 | ||
The definition of barriers is the factors responsible for delaying or causing non-compliance with the treatment. According to the World Economic Situation and Prospects report for 2024, global countries are classified into three broad categories: Developed economies, economies in transition, and developing economies.[22] Our systematic review is based on this report and focuses on the countries under the category of developing economies.
Eligibility criteria
Articles were deemed suitable if they fulfilled the following criteria: Research papers from January 2000 to January 2024 related to barriers to the Ponseti method for children clubfoot management in developing nations, studies written in English, participants below the age of 18 with clubfoot, studies conducted in developing nations as defined by World Economic Situation and Prospects in 2024,[22] study design of cross-sectional and cohort studies.
Data extraction
Five authors then separately collected data from all suitable reports using a standardized form. A summary of all the studies involved is shown in Table 2. The data were categorized into patient, family, socio-cultural, economic, doctor or healthcare, geographical, logistic, and other factors [Tables 3 and 4].
| No | Author | Country | Year | Study design | Number of participants | Number of drop out/Non-compliance patients |
|---|---|---|---|---|---|---|
| 1 | Pinto et al.[2] | India | 2021 | Retrospective | 965 | 155 |
| 2 | Dreise et al.[8] | Uganda | 2023 | Retrospective | 163 | 66 |
| 3 | Evans et al.[9] | Bangladesh | 2021 | Cross-sectional | 311 | 309 |
| 4 | Kazibwe and Struthers[10] | Uganda | 2009 | Cross-sectional | 167 | 17 |
| 5 | Poudel et al.[11] | India | 2019 | Cross-sectional | 238 | 100 |
| 6 | Evans et al.[17] | Bangladesh | 2020 | Cross-sectional | 72 | 0 |
| 7 | Palma et al.[12] | Peru | 2013 | Cross-sectional | 37 | 5 |
| 8 | Alam et al.[13] | Bangladesh | 2015 | Cross-sectional | 102 | 0 |
| 9 | Nogueira et al.[3] | Brazil | 2013 | Cross-sectional | 45 Physicians | 0 |
| 10 | Lu et al.[14] | China | 2010 | Cross-sectional | 39 Physicians | 0 |
| 11 | Boardman et al.[15] | Chile, Peru, Guatemala | 2011 | Cross-sectional | 28 Physicians | 0 |
| 12 | Gadhok et al.[16] | India | 2012 | Cross-sectional | 38 Physicians | 0 |
| 13 | Iqbal et al.[18] | India | 2021 | Cross-sectional | 108 | 0 |
| 14 | Patel et al.[19] | India | 2022 | Retrospective | 110 | 23 |
| 15 | Alam et al.[20] | Bangladesh | 2014 | Cross-sectional | 102 | 0 |
| Pinto et al.[2] | Dreise et al.[8] | Evans et al.[9] | Kazibwe and Struthers[10] | Poudel et al.[11] | Evans et al.[17] | Palma et al.[12] | Alam et al.[13] | |
|---|---|---|---|---|---|---|---|---|
| Patient factors | ||||||||
| Child discomfort with cast/brace | 4 | 0 | 24 | 0 | 0 | 30 | 0 | 0 |
| Family factors | ||||||||
| Other commitments and responsibilities | 10 | 4 | 86 | 49 | 33 | 22 | 0 | 13 |
| Lack of knowledge and understanding | 9 | 0 | 23 | 111 | 23 | 0 | 27 | 0 |
| Lack of family support | 28 | 0 | 0 | 0 | 17 | 0 | 0 | 5 |
| Socio-cultural factors | ||||||||
| Cultural beliefs | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Economic factors | ||||||||
| Financial problem | 28 | 62 | 22 | 137 | 17 | 5 | 39 | 61 |
| Doctor/healthcare factors | ||||||||
| Lack of trained professionals | 0 | 0 | 0 | 0 | 0 | 0 | 31 | 0 |
| Difficult to use or put on bracing/Frequent changing of casts and cast care | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Lack of explanation from the healthcare staff | 0 | 0 | 0 | 113 | 0 | 11 | 0 | 11 |
| Long term treatment | 9 | 0 | 28 | 0 | 0 | 0 | 24 | 71 |
| Overcrowded clinic or hospital | 7 | 0 | 0 | 0 | 43 | 4 | 0 | 101 |
| Negative experience with healthcare staff | 3 | 0 | 3 | 0 | 0 | 8 | 0 | 0 |
| Nation’s healthcare system | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Geographical factors | ||||||||
| Distance to treatment is far | 22 | 25 | 54 | 0 | 0 | 62 | 30 | 34 |
| Logistics factors | ||||||||
| Transportation problem | 20 | 55 | 0 | 0 | 32 | 2 | 0 | 18 |
| Other factors | ||||||||
| Aesthetic reasons | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Nogueira et al.[3] | Lu et al.[14] | Boardman et al.[15] | Gadhok et al.[16] | Iqbal et al.[18] |
Patel et al.[19] |
Alam et al.[20] |
|
|---|---|---|---|---|---|---|---|
| Patient factors | |||||||
| Child discomfort with cast/brace | 10 | 0 | 0 | 0 | 64 | 0 | 0 |
| Family factors | |||||||
| Other commitments and responsibilities | 0 | 0 | 0 | 0 | 63 | 0 | 0 |
| Lack of knowledge and understanding | 12 | 6 | 0 | 26 | 0 | 35 | 11 |
| Lack of family support | 34 | 6 | 12 | 30 | 57 | 0 | 5 |
| Socio-cultural factors | |||||||
| Cultural beliefs | 5 | 2 | 10 | 0 | 57 | 7 | 0 |
| Economic factors | |||||||
| Financial problem | 3 | 14 | 23 | 24 | 117 | 72 | 61 |
| Doctor/healthcare factors | |||||||
| Lack of trained professionals | 0 | 8 | 25 | 0 | 0 | 0 | 0 |
| Difficult to use or put on bracing/Frequent changing of casts and cast care | 8 | 0 | 0 | 0 | 39 | 0 | 0 |
| Lack of explanation from the healthcare staff | 0 | 0 | 0 | 0 | 36 | 0 | 0 |
| Long term treatment | 0 | 0 | 0 | 0 | 0 | 0 | 71 |
| Overcrowded clinic or hospital | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Negative experience with healthcare staff | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Nation’s healthcare system | 0 | 0 | 23 | 10 | 0 | 0 | 0 |
| Geographical factors | |||||||
| Distance to treatment is far | 0 | 0 | 21 | 31 | 47 | 55 | 80 |
| Logistics factors | |||||||
| Transportation problem | 0 | 0 | 21 | 31 | 0 | 0 | 18 |
| Other factors | |||||||
| Aesthetic reasons | 2 | 0 | 0 | 0 | 0 | 0 | 0 |
RESULTS
The preliminary literature review determined 2135 related articles on barriers in clubfoot treatment. After screening the titles and abstracts, 23 articles were selected for full-text assessment, and 15 studies satisfied the inclusion criteria and were involved in the systematic review.[2-3,8-20] The PRISMA flowchart [Figure 1] presents the study selection.
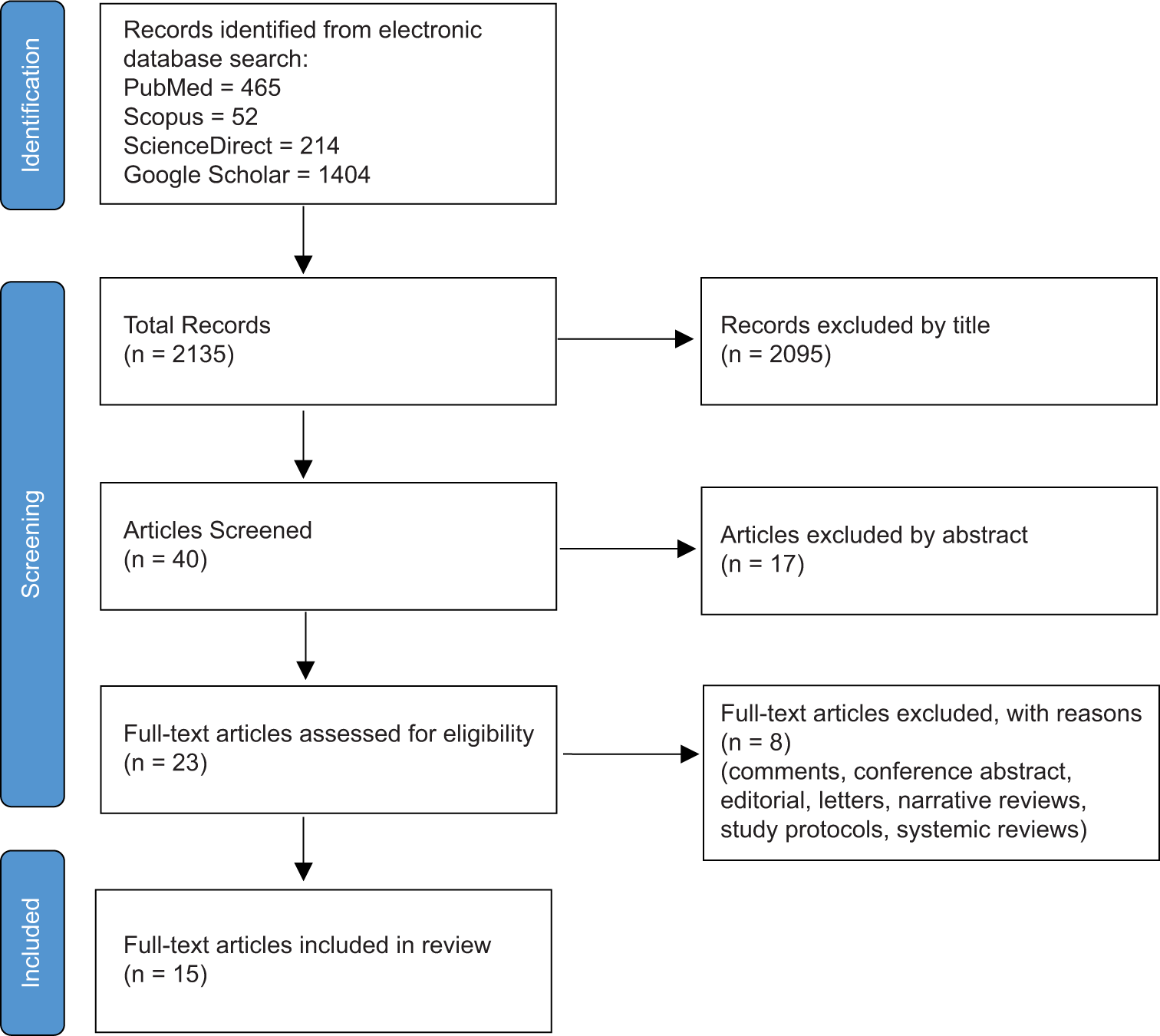
- Preferred reporting items for systematic reviews and meta-analyses study flow diagram.
Synthesis of results
Our study yielded 2525 participants; 150 of them were physicians, while 2375 were caregivers of children with clubfoot. Of the 2525 participants, 675 dropped out of the studies. Figure 2 shows eight factors affecting the treatment of clubfoot among children in developing nations: Patient factors, family factors, socio-cultural factors, economic factors, doctor or healthcare factors, geographical factors, logistic factors, and other factors. Family factors were the most frequently mentioned reason for dropping out (n = 757). This was followed by doctor or healthcare factors (n = 687) and economic factors (n = 685). Four hundred sixty-one participants were not compliant with geographical factors; 197 were not compliant with the Ponseti method due to logistical factors. This was followed by patient factors (n = 132), socio-cultural factors (n = 83), and finally, the other factors (n = 2). Figures 3 and 4 showed the family and doctor or healthcare factors subgroups.
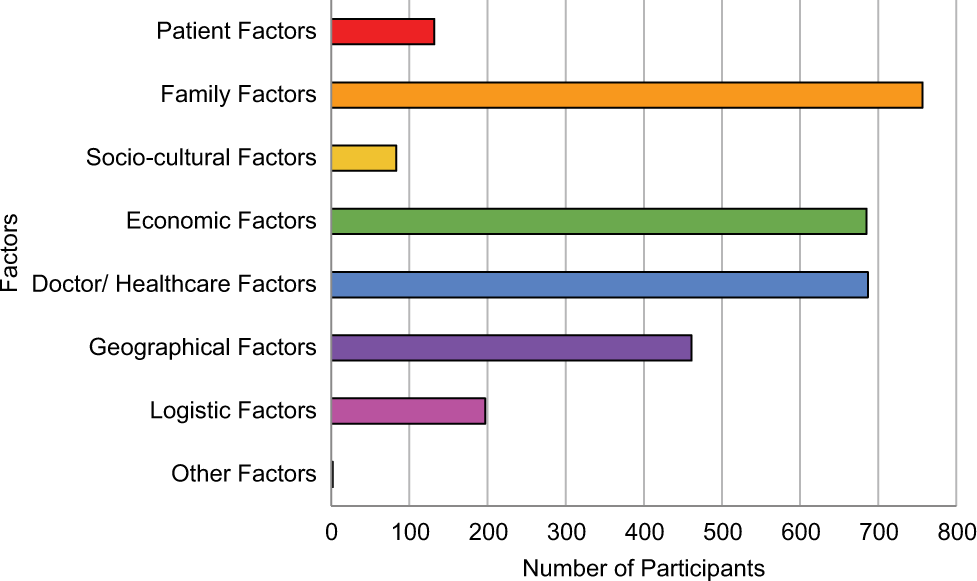
- Bar chart showing barriers to the Ponseti method for children clubfoot management in developing nations.
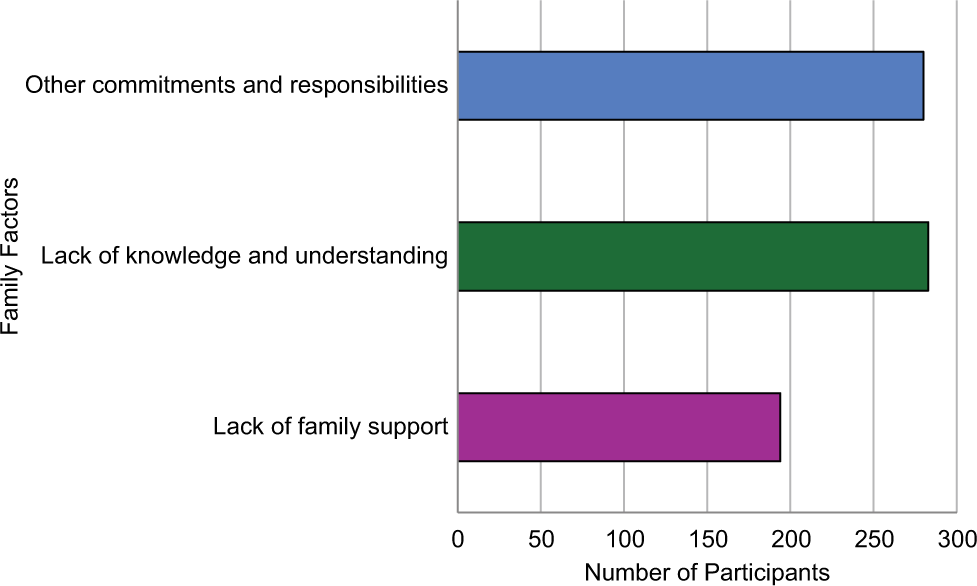
- Bar chart showing subgroups of family factors.
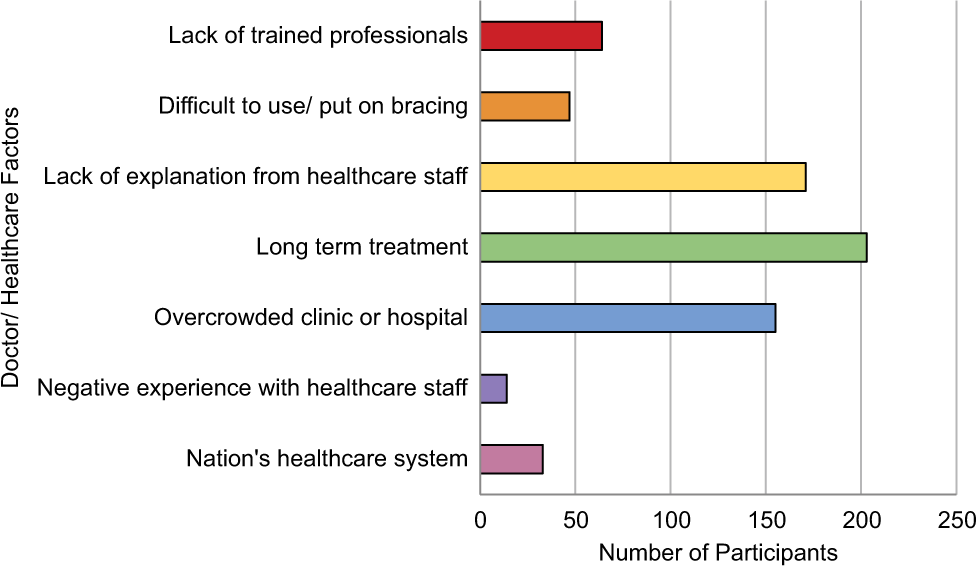
- Bar chart showing subgroups of doctor or healthcare factors.
DISCUSSION
The Ponseti casting and bracing method has gained widespread acceptance in clubfoot treatment because it is minimally invasive, affordable, and associated with excellent clinical results.[1,2] Despite the proven efficacy of the Ponseti method, obstacles such as barriers to successful implementation and adherence to treatment still need to be resolved, specifically in developing countries. Various studies in the literature have explored the barriers caregivers and physicians encounter in delivering Ponseti treatment in several developing nations, such as India, Uganda, Bangladesh, Peru, Brazil, China, Chile, and Guatemala.[2,3,8-20] Regardless of the variation in population, cultures, and healthcare system, the barriers recognized are identical in all these countries. Obstacles to clubfoot treatment established by the studies have comprised the following: Patient-level factors such as child discomfort with cast or brace; family-level factors such as other commitment or responsibilities of family members, lack of knowledge and understanding, and lack of family support; socio-cultural factors such as cultural beliefs; economic-level factors such as financial problem; doctor or healthcare-level factors such as lack of trained professionals, difficult to use or put on bracing or frequent changing of casts and cast care, lack of explanation from healthcare staff, long-term treatment, overcrowded clinic or hospital, negative experience with healthcare staff, nation’s healthcare system; geographical-level factors such as distance to treatment is far; logistics-level factors such as transportation problem; and other factor such as esthetic reasons.
Family-level factors were the most widely acknowledged barriers to Ponseti treatment. Gadhok et al.[16] found that many neglected cases were mainly due to insufficient public awareness about clubfoot. Some villagers thought that clubfoot was a polio deformity, and people from villages were often inattentive to the available treatments for complete correction of their children’s deformities. Poudel et al.[11] claimed that some parents incorrectly thought a subsequent follow-up was unnecessary as the foot presented as “normal.” However, Kazibwe and Struthers[10] stated that despite the limited knowledge of clubfoot before the diagnosis, they had studied clubfoot, its management, and the complications of not following the prescribed management. Thus, the research found no notable correlation between the parents’ knowledge of clubfoot and their adherence to the care plan.
Besides that, Iqbal et al. stated that insufficient familial support and familial resistance are the obstacles to treatment.[18] This is because caregivers had no option but to follow the wishes of elders in the family who disagreed with the treatment. The same has been emphasized by Pinto et al., in which the authors have recommended improving family support by involving the extended family in the management plan.[2] For instance, counseling sessions can be done before and throughout the treatment, focusing on the principal caregivers. Counseling extended family members through telephone or video calls during parent sessions and providing brochures in native languages for family discussion may help them feel involved and increase their support for childcare and compliance with follow-up.
Moreover, caregivers’ commitments and responsibilities are crucial in determining clubfoot treatment. According to Iqbal et al., many reported that bringing their children for routine treatment was difficult as they had other duties and commitments.[18] For example, if they attend the treatment, they have to skip work and leave behind other family dependents, which will disturb their daily routines in the household and workplace. Therefore, family-level factors are vital in affecting caregivers’ compliance with clubfoot treatment.
The second most common barrier to clubfoot treatment is doctor and healthcare-related factors. Alam et al.[20] stated that the leading subgroup in the healthcare factor is that patients do not adhere to the treatment due to the length of the treatment plan. This is compounded by the second most common barrier identified under the healthcare factors: A lack of proper explanation given to the patients by the healthcare providers. In another study by Alam et al., the third leading healthcare factor is the overcrowding of hospitals and healthcare facilities.[13] The three factors mentioned in the studies that were cited make up most of the barriers under the healthcare factors that prove to be a barrier to the treatment of clubfoot, and we can see that there is a strong correlation between these factors and the consequence of using the Ponseti method for the therapy of clubfoot.
Furthermore, financial problems were the third most common barrier to treating clubfoot. Poverty presents a prominent obstacle to accessing treatment, as many families are compelled to value survival above addressing a non-life-threatening condition.[8] Kazibwe and Struthers stated that despite free treatment, some patients could not obtain financial support to travel to and from the hospital.[10] To offset this difficulty, having a travel voucher would be a cheaper alternative to hospitalization.
Next, geographical factors also significantly impact the treatment of clubfoot. This is supported by the fact that 11 out of 15 studies associated geographical factors with problems receiving treatment, such as people not having access to proper healthcare in rural areas. Dreise et al.[8] reported that one of the reasons parents of children face difficulties in attending clinic appointments is the long travel time to the hospital caused by poor road conditions and heavy traffic. Besides that, logistic factors also contribute significantly to treating clubfoot in children, and 8 out of 15 studies support this. According to Palma et al., 94% of healthcare professionals reported that geographical distance and transportation to healthcare centers were obstacles to the Ponseti method in Peru.[12] This is because patients from rural areas must travel at least 10 h by bus to reach the clinic weekly during the casting phase of treatment. One physician also highlighted that it is nearly impossible for patients living far away to come every week.
In addition, one of the barriers in the treatment of clubfoot is patient-level factors such as child discomfort with a cast or brace. Pinto et al. explained that older children tend to be more energetic and may not accept casts and braces as infants do.[2] Thus, starting treatment at an older age is a potential warning sign for potential dropout. Hence, more watchful observation is required to ensure adherence with such patients.
Cultural beliefs were the least common factor compared to other barriers to clubfoot treatment, as 9 out of 15 studies had 0 statistics for socio-cultural factors. Iqbal et al. highlighted the association between caregivers’ understanding of clubfoot and their encounters with social stigma as an obstacle to treatment.[18]
Other factors, such as aesthetic reasons, were identified as minor barriers to clubfoot treatment, as seen in the study by Nogueira et al.[3] However, this factor was only identified in one study, and more data are needed about whether it plays an actual role in being a barrier to clubfoot treatment in other countries. This factor may have a more significant role in more developed countries.
Different studies propose solutions to overcome the barriers to clubfoot treatment. First, Dreise et al. suggested a teach-back method to ensure the caregivers understand the critical importance of bracing.[8] For instance, after healthcare professionals have explained the information to caregivers, they have to ask them to repeat it to ensure they have confidently and accurately articulated it. Besides that, both Boardman et al. and Gadhok et al. suggested using paper, electronic media, nationwide publicity campaigns, and health visitors to increase awareness of appropriate clubfoot recognition.[15,16] Each of these tools and approaches is thought to have unique advantages, and integrating them can result in a comprehensive and effective strategy.
Furthermore, Pinto et al. and Gadhok et al. proposed a solution by offering incentives for proper follow-up or compensation for missed workdays.[2,16] Although offering incentives or compensation is a temporary solution, it may help alleviate this issue. Moreover, family support can be improved by involving the extended family in the management plan. For instance, counseling sessions could be organized before and during treatment, focusing on the caregivers. Counseling extended family members through telephone or video calls during parent sessions and providing educational leaflets in the native language for family discussion may help them feel involved in the child’s treatment, enhancing their support for child care and adherence to follow-up appointments.[2]
In addition, Boardman et al. recommended that low-cost braces could be produced.[15] This is because it can help eliminate the financial burden the current bracing system places on families. Boardman et al. also claimed that getting government agencies to acknowledge the Ponseti method as the gold standard is vital and providing financial support for treatment costs is critical.[15]
One of the proposed solutions for doctor and healthcare factors is integrating the Ponseti method into the medical school curriculum and residency and fellowship training.[15,16] In addition, four studies suggested that increasing training opportunities can increase the number of Ponseti providers. This would ensure that rural providers have the chance to be trained.[8,14-16] Moreover, improving communication between physicians and parents is important by providing informational pamphlets with photographs and directions and translating them into as many native dialects as possible.[15] Therefore, parents can understand more clearly. Besides that, Dreise et al. advised healthcare professionals to be present and equipped with all essential supplies and begin their clinics punctually to ensure efficient operations.[8] Dreise et al. also suggested introducing more clinic days by adding a “brace” day or dispersing brace management to health facilities closer to the patients.[8] Thus, this can improve workflow, enhance efficiency, and ensure smooth communication.
A transport subsidy system can be established to overcome geographical and logistic factors.[8] Finally, Pinto et al. and Gadhok et al. suggested that Ponseti treatment could be implemented through a hub-and-spoke organizational model, where a central institute (Hub) provides full services and specialists. At the same time, secondary centers (Spokes) deliver more commonly needed services, like brace follow-up, which can be assigned to support staff.[2,16] Although many solutions are provided for overcoming the barriers, addressing these barriers requires customized strategies that account for the unique challenges of each context to ensure the effective delivery of clubfoot treatment worldwide.
Limitations
We acknowledge some limitations to this systematic review. Overall, three out of 15 studies were retrospective with no randomized or non-randomized controlled trials, which introduces possible bias and results in weaker evidence. Our systematic review involves a wide range of geographical regions with various epidemiologies such as differences in population, cultures, and resources. Furthermore, few reports notably address the challenges of clubfoot treatment in developing nations. Many vital data, including the complete recovery of clubfoot using the Ponseti method and the average recovery duration, still need to be included. Our study compiles the available reliable evidence to guide future efforts in introducing the Ponseti method to developing nations and, finally, the limits of language in English literature.
CONCLUSION
Although the Ponseti method has been proven to be an efficient non-surgical treatment option that offers a high success rate when implemented correctly, our literature assessment identified many barriers to delivering the method. These include patient and family, socio-economic, healthcare, and geographical and logistical factors.
RECOMMENDATIONS
Understanding the barriers is vital as this leads to the successful implementation of treatment programs. From this, we can recognize a need for proper public education, which government health education campaigns can address. Other standard solutions to the barriers were proposed, focusing on handling the financial barriers, such as the cost of treatment and transportation. Increased training of healthcare providers and allocation of healthcare resources can significantly benefit addressing some of the barriers identified in this study. Ultimately, we recognize that changes need to be implemented at the national level and by individuals in the community to achieve the proven effectiveness of the Ponseti method seen in other countries worldwide.
AUTHORS’ CONTRIBUTIONS
MAI and OJX: Contributed to the conception of the idea, literature search, and data extraction. LJY, ST, and MUBMI: Contributed to the literature search, data extraction, and quality assessment of articles. All authors participated in drafting the work, conducting critical revisions, and giving final approval for the version to be published. They also agreed to take responsibility for all aspects of the work to ensure that any questions regarding the accuracy of any part of the work are properly investigated and addressed. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
Institutional Review Board approval is not required.
DECLARATION OF PATIENT CONSENT
Patient’s consent is not required, as there are no patients in this study.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- The impact of socio-economic factors on parental non-adherence to the Ponseti protocol for clubfoot treatment in low-and middle-income countries: A scoping review. EClinicalMedicine. 2022;48:101448.
- [CrossRef] [PubMed] [Google Scholar]
- Factors causing dropout from treatment during the Ponseti method of clubfoot management: The caregivers' perspective. J Foot Ankle Surg. 2021;61:730-4.
- [CrossRef] [PubMed] [Google Scholar]
- The Ponseti method of treatment for clubfoot in Brazil: Barriers to bracing compliance. Iowa Orthop J. 2013;33:161-6.
- [Google Scholar]
- Worldwide spread of the Ponseti method for clubfoot. World J Orthop. 2014;5:585-90.
- [CrossRef] [PubMed] [Google Scholar]
- Understanding the barriers to clubfoot treatment adherence in Uganda: A rapid ethnographic study. Disabil Rehabil. 2007;29:845-55.
- [CrossRef] [PubMed] [Google Scholar]
- The global challenges of surgical congenital anomalies: Evidence, models, and lessons. Semin Pediatr Surg. 2023;32:151348.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers affecting clubfoot treatment in Sarawak. J Health Transl Med. 2018;21:15-22.
- [Google Scholar]
- Exploring bracing adherence in Ponseti treatment of clubfoot: A comparative study of factors and outcomes in Uganda. Int J Environ Res Public Health. 2023;20:6396.
- [CrossRef] [PubMed] [Google Scholar]
- A community audit of 300 “drop-out” instances in children undergoing Ponseti clubfoot care in Bangladesh-what do the parents say? Int J Environ Res Public Health. 2021;18:1-12.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers experienced by parents of children with clubfoot deformity attending specialised clinics in Uganda. Trop Doct. 2009;39:15-8.
- [CrossRef] [PubMed] [Google Scholar]
- Factors affecting compliance to hospital visit among clubfoot patients: A cross-sectional study from a tertiary referral clubfoot clinic in the developing country. J Orthop Surg (Hong Kong). 2019;27:2309499019825598.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers to the Ponseti method in Peru: A two-year follow-up. Iowa Orthop J. 2013;33:172-7.
- [Google Scholar]
- Assessing knowledge on clubfoot among parents having children with clubfoot deformity. Chatt Maa Shi Hosp Med Coll J. 2015;14:42-6.
- [CrossRef] [Google Scholar]
- From cutting to casting: Impact and initial barriers to the Ponseti method of clubfoot treatment in China. Iowa Orthop J. 2010;30:1-6.
- [Google Scholar]
- The Ponseti method in Latin America: Initial impact and barriers to its diffusion and implementation. Iowa Orthop J. 2011;31:30-5.
- [Google Scholar]
- Qualitative assessment of the challenges to the treatment of idiopathic clubfoot by the Ponseti method in urban India. Iowa Orthop J. 2012;32:135-40.
- [Google Scholar]
- Factors affecting parents to 'drop-out' from Ponseti method and children's clubfoot relapse. Orthop Res Online J. 2020;6:601-9.
- [CrossRef] [Google Scholar]
- Assessment of awareness and barriers to clubfoot treatment in the Indian scenario. J Family Med Prim Care. 2021;10:4229-35.
- [CrossRef] [PubMed] [Google Scholar]
- Quantitative analysis of barriers to clubfoot treatment experienced at a tertiary care institute in India. Cureus. 2022;14:e25782.
- [CrossRef] [Google Scholar]
- Barriers facing by the parents during clubfoot treatment of children with clubfoot deformity. MOJ Orthop Rheumatol. 2014;1:22-6.
- [CrossRef] [Google Scholar]
- Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1-9.
- [CrossRef] [PubMed] [Google Scholar]







