Translate this page into:
Narrow DCP application during intertrochanteric fracture fixation to serve as a fracture reduction maintenance tool and a trochanteric stabilization plate
*Corresponding author: Ahmed A. Khalifa, Department of Orthopaedics, Qena Faculty of Medicine and University Hospital, South Valley University, Qena, Egypt. khalifaahmed8486@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Refai OA, Khalifa AA. Narrow DCP application during intertrochanteric fracture fixation to serve as a fracture reduction maintenance tool and a trochanteric stabilization plate. J Musculoskelet Surg Res. 2025;9:285-91. doi: 10.25259/JMSR_464_2024
Abstract
Intertrochanteric fractures (ITFs) could be treated efficiently using various devices, including dynamic hip screws, proximal femoral nails, and proximal femoral locking plates. To guard against femoral shaft medialization in unstable ITFs, a trochanteric stabilization plate (TSP) could be added as a supplementary fixation, produced by different companies and in various shapes. We describe a simplified technique using a narrow dynamic compression plate (DCP) (applied anterolaterally or posterolaterally) to act as a preliminary or permanent fracture reduction maintenance tool and serve as a TSP. The technique is simple and affordable, as a narrow DCP is available in most orthopedic operating theaters. Furthermore, this option could be a rescue plan if an original TSP is unavailable or cannot be applied.
Keywords
Dynamic compression
Femur
Fracture
Intertrochanteric
Medialization
Plate
Proximal femoral stabilization
Trochanteric stabilization
Unstable
INTRODUCTION
Unstable intertrochanteric fractures (ITFs) are among the most common fractures around the hip, with the elderly population being more susceptible due to the increased risk of falls combined with osteoporosis.[1,2] Optimum management will reduce morbidity and mortality risks, leading to early rehabilitation with better functional and quality-of-life outcomes.[1-3]
Management options for ITFs include either fracture fixation, which could be obtained by various implants [dynamic hip screws (DHS), proximal femoral nails (PFN), and proximal femoral locking plates (PFLP)], or hip replacement (which could be either total or partial).[2,4-10]
Unstable ITFs with lateral wall involvement (either preoperatively or occurring intraoperatively, or posteromedial comminution) are vulnerable to excessive femoral shaft medialization, fixation failure, and eventual poor outcomes.[11,12] To guard against displacement, implants preventing such medialization or secondary displacement are advisable, i.e., trochanteric stabilization plate (TSP), which buttresses the lateral wall with subsequent femoral medialization prevention.[13-15] Furthermore, this concept could be applied while using DHS or PFN.[16,17]
Although multiple manufacturers provide various TSP designs, they may not be available for all surgeons. Hence, we aimed to describe the technique of using a narrow dynamic compression plate (DCP) for the preliminary fixation and acting as a TSP during ITF management using DHS.
SURGICAL TECHNIQUE
Installation and procedure
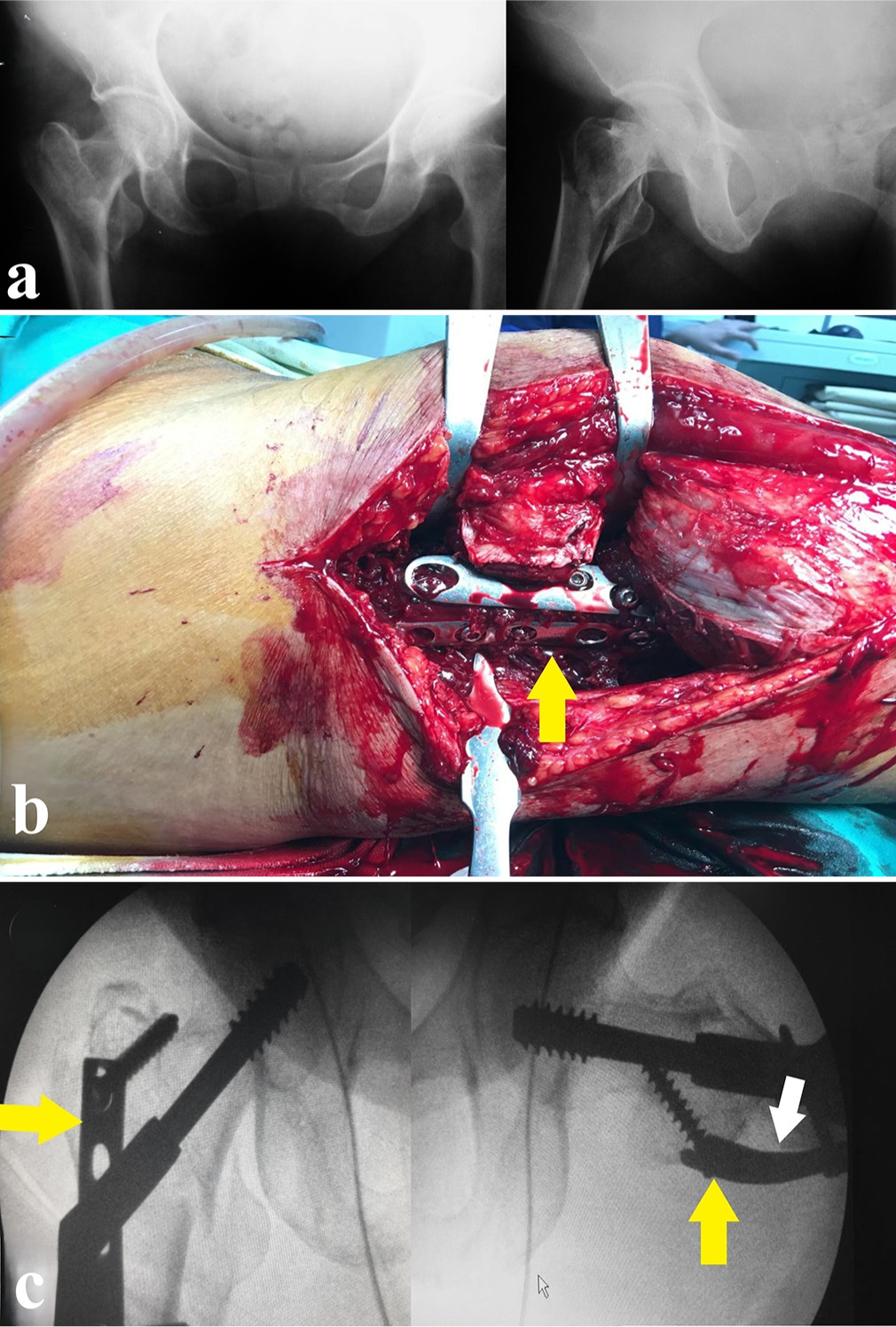
Preferably, all surgeries are performed under spinal anesthesia unless contraindicated according to the patient’s general condition or medical comorbidities. In cases with ITFs [Figure 1a], we operate while the patient is supine on a regular radiolucent operating table (we do not use a specified traction table. However, we rely on manual traction, which is described later). The surgical field sterilization and draping are performed, and then, under fluoroscopic control, a preliminary fracture reduction trial is usually performed by gentle axial traction, slight hip abduction, and internal rotation [Figure 1b and c].
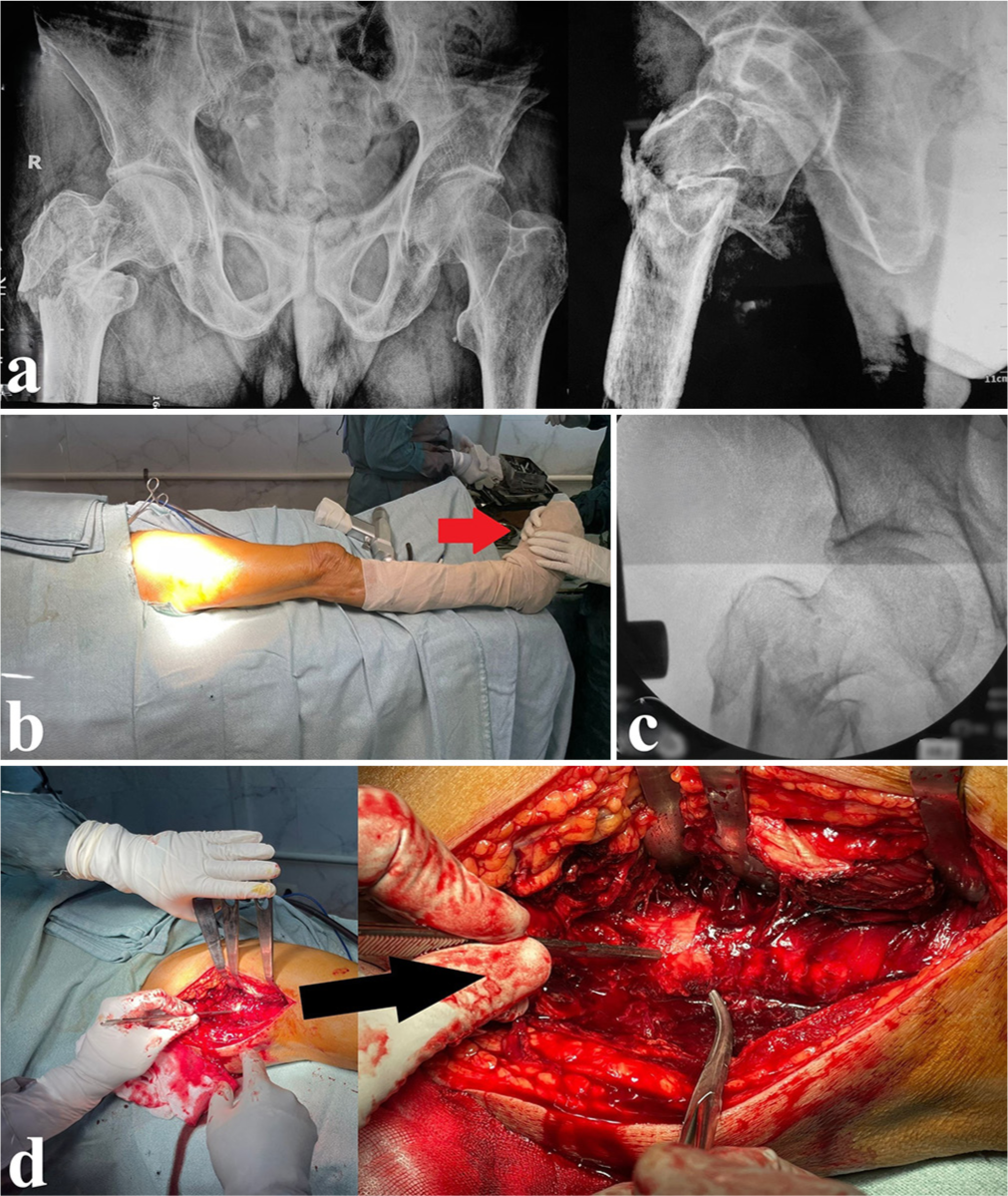
- Demonstration case of a male patient, 80 years old, presented with unstable intertrochanteric fracture (classified as AO/31A2). (a) Preoperative anteroposterior (AP) and lateral views showing the fracture configuration. (b) After draping, the assistant holds the lower limb with gentle traction after performing a trial of fracture reduction (red arrowhead). (c) A fluoroscopic AP view showing the irreducibility of the fracture. (d) Surgical approach and finding the key fragment to achieve proper fracture reduction (black arrowhead).
The technique of using a narrow DCP as a TSP could be applied while using either DHS or PFN; however, we are describing the technique while using a DHS for fracture fixation.
Why, where, when, and how can the narrow DCP be applied?
Why and where
The narrow DCP serves two principal functions; first, it could be used as a temporary or permanent fracture reduction stabilizer (which was described in previous studies dealing with various fractures[18,19]). As it is relatively small in width, it could be applied on either the anterolateral (AL) or the posterolateral (PL) femoral surfaces besides the proposed DHS side plate location. It could be applied initially (before DHS application after an initial fracture reduction) and fixed with screws [the order, position, and length of which could be changed later on based on the screws applied to fix the DHS side plate and if the greater trochanter (GT) fixation is required or feasible] to hold the fracture in a reduced position till DHS final fixation. Second, its placement on the AL or PL aspects enables the plate to act as a TSP (whether proximal screws fixation was applied or not), as the proximal segment of the plate (above the DHS barrel level) is in contact against the anterior or posterior segment of the GT (according to the plate location).
When
As mentioned earlier, the surgeon could apply the plate initially before proceeding with the DHS procedure. Or, it could be applied after securing the DHS in place (as the technique described in the literature with other TSPs); this timing is preferable for using the narrow DCP on the PL surface, as after securing the DHS in place, the surgeon could confidentially rotate the hip internally to obtain better visualization of the PL surface.
How
In general, we followed the principles of fracture fixation and the principle for the application of DCPs.[20]
If the surgeon is applying an AL plate before performing DHS (as in the provided case demonstration)
The femur is approached through a direct lateral approach centered over the femoral shaft lateral aspect [Figure 1d].[21] After careful placement of retractors for better visualization of the fracture configuration, a trial of fracture reduction under fluoroscopic control is carried out. After obtaining an acceptable reduction, a very crucial step to mention (as we did not use a traction table and relied on manual traction only) is the assistant who holds the lower limb from the foot, as he/she should keep a steady position and maintain gentle traction (in the reduced fracture position) till preliminary fixation is obtained.
The surgeon could reduce the fracture to near an anatomical position using various reduction tools and clamps. A narrow DCP of 6–8 holes is needed (it could be longer according to the fracture distal extension), and the proximal plate segment could be contoured to accommodate the prominent anterior segment of the GT. The plate is applied to the AL femoral surface to ensure that it does not impinge on the proposed DHS side plate position. If the fracture reduction is acceptable, the surgeon starts fixation by application of the distal screws, followed by the proximal ones [Figure 2a]. The direction of the distal screws (in the shaft area) from AL to posteromedial (which could be changed if needed after DHS application), as for the proximal screws (cortical 4.5 or cancellous 6.5), these could be applied according to the nature of the fracture comminution and aiming for the best location of generous bone stock for better screws purchase. The initial fracture reduction and the AL plate fixation are checked under fluoroscopy in the anteroposterior (AP) [Figure 2b] and lateral [Figure 2c and d] views. One vital point to clarify is obtaining a lateral view without using a traction table; the operating surgeon holds the lower limb in a frog leg-like position (by hip flexion, abduction, and external rotation) [Figure 2c].
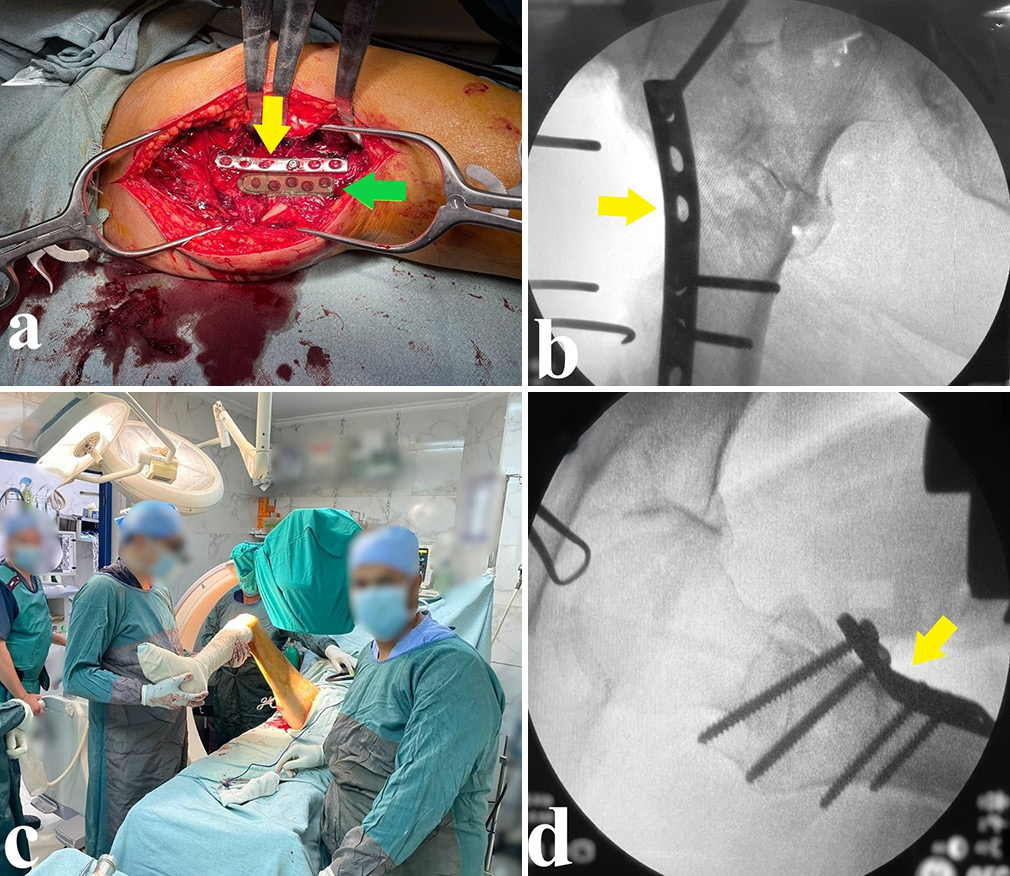
- (a) After initial near anatomical fracture reduction, preliminary fixation using an anterolateral narrow DCP (yellow arrowhead) was performed (the plate position is selected not to interfere with the position of the dynamic hip screw side plate, shown as a green overlay and indicated by the green arrowhead). (b) Checking the fracture reduction, anterolateral plate position (yellow arrowhead), and fracture initial fixation in the anteroposterior view. (c) Obtaining a lateral view by hip flexion, abduction, and external rotation. (d) Checking the fracture reduction and anterolateral plate position in the lateral view (yellow arrowhead). DCP: Dynamic compression plate.
Then, the DHS steps are followed using the technique described in the literature.[21,22] After the initial guidewire application [Figure 3a], an AP and lateral view are obtained to confirm the position of the guidewires in the same manner as described earlier [Figure 3b-d]. Supplementary support could be obtained while obtaining the lateral position using fracture reduction clamps if required. After ensuring the proper position of the guidewires, the DHS procedure is completed in the usual fashion [Figure 4a and b]. Regarding the AL narrow DCP final fixation, the same screws used initially could be left in place, changed, or further supplementary screws are used, which is according to the fracture stability and at the surgeon’s discretion [Figure 4c and d].
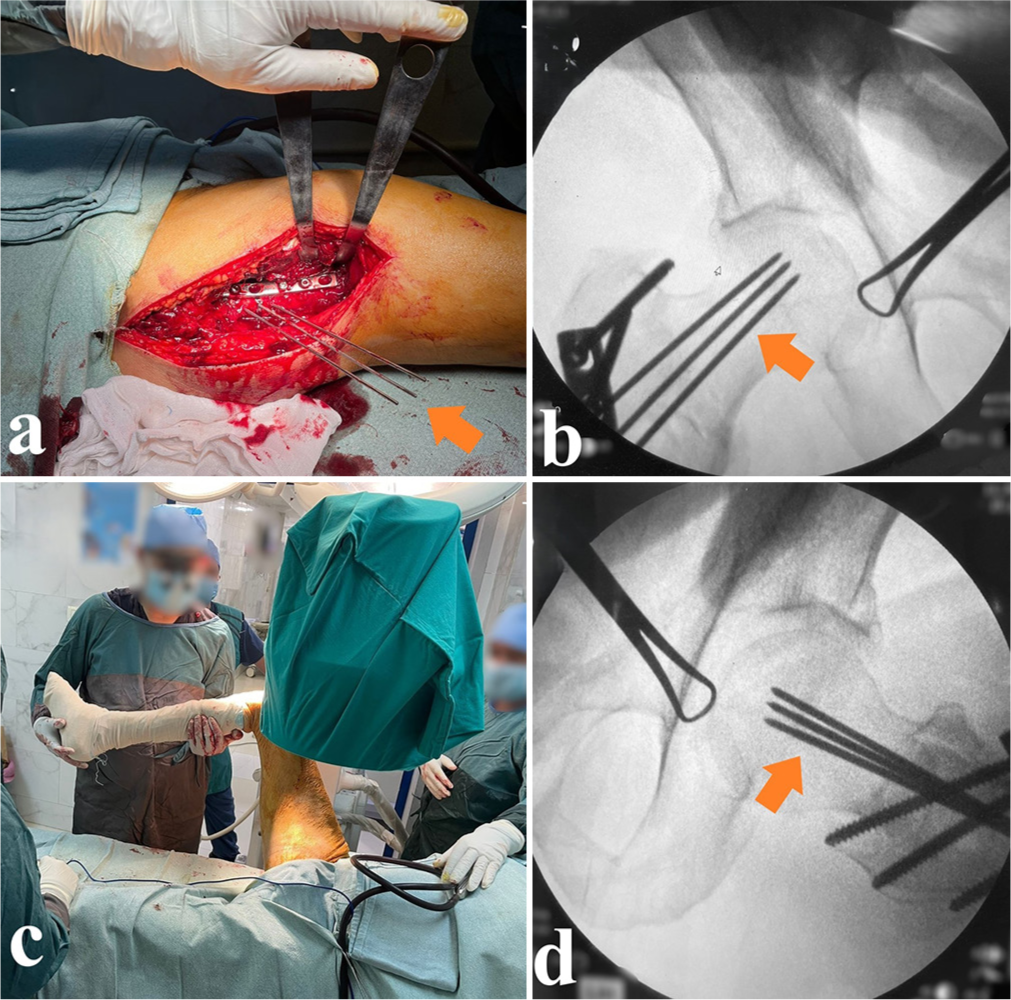
- Definitive fracture fixation using dynamic hip screw (DHS) plate. (a) The application of guidewires as an initial step to determine proper DHS lag screw position (orange arrowheads). (b) An anteroposterior fluoroscopic view showing the proper guidewires positioning (orange arrowhead). (c) The position for obtaining a lateral view for guidewires position assessment. (d) A fluoroscopic lateral view showing proper guidewires position (orange arrowhead).
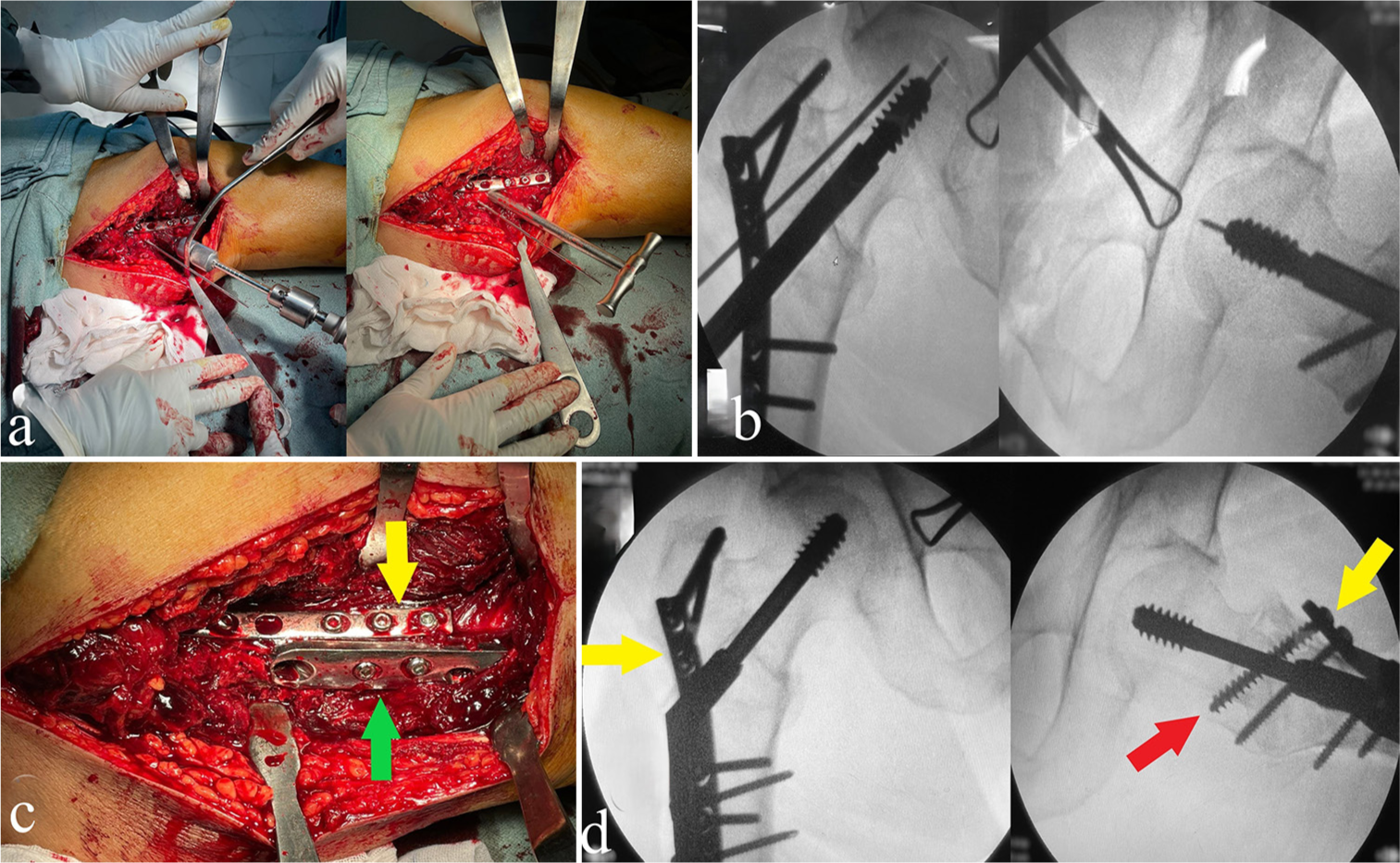
- (a) Reaming and application of dynamic hip screw (DHS) lag screw. (b) An anteroposterior (AP) and lateral fluoroscopic views confirming the lag screw proper position within the femoral neck and head. (c) Definitive plate application and fixation, showing the relative position of the anterolateral narrow DCP (yellow arrowhead) to the DHS side plate (green arrowhead). (d) Final AP and lateral fluoroscopic views after definitive fixation showing the proper plates position (yellow arrowhead), fracture reduction, and optimum fixation (the red arrow indicates changing the proximal screw in the anterolateral plate from a cortical 4.5 to a fully threaded cancellous 6.5 screw).
If the surgeon applies an AL or PL plate after performing DHS
The surgeon will proceed with all steps of the DHS procedure. After finalizing the fixation, if a TSP is required, the AL or PL narrow DCP will be applied anteriorly or posteriorly [Figure 5] to the DHS side plate (after contouring if needed), respectively.
- A female patient, 75 years old, presented with an unstable intertrochanteric fracture (classified as AO/31A2). (a) Preoperative anteroposterior (AP) and lateral views. (b) An intraoperative image showing the application and position of a posterolateral narrow DCP (yellow arrowhead). (c) Intraoperative AP and lateral fluoroscopic views show the position of the dynamic hip screw and the posterolateral narrow DCP (yellow arrowhead); furthermore, the white arrowhead indicates the location of narrow DCP contouring to accommodate this specific anatomical location configuration. DCP: Dynamic compression plate.
The wound is closed in layers, and the postoperative rehabilitation protocol is the same as usual DHS surgeries.
DISCUSSION
Selecting the optimum management option and fixation device while treating ITFs is still debatable, which relies on various factors, including fracture nature (classification, stability, comminution), surgical team competence for specific management techniques (such as performing hip replacement, and the required specific trochanteric wiring techniques), and the availability of specific implants (sometimes due to economic restrictions).[8,10,11,13,14,23-26] Furthermore, various options were suggested for managing unstable ITFs, such as fixation only without additives (either DHS or PFN alone) or adding TSP for fixation augmentation and prevention of secondary displacement.[11,13,14]
The technique we described is feasible, simple, and effective as a TSP alternative [Figure 6]. TSP works by offering a secondary point of fixation, especially in cases where the lateral wall is not intact; it prevents excessive femoral shaft medialization by buttressing the lateral wall; furthermore, it provides an anti-rotation function of the proximal femur during hip joint motion with less non-union risk.[23,27]
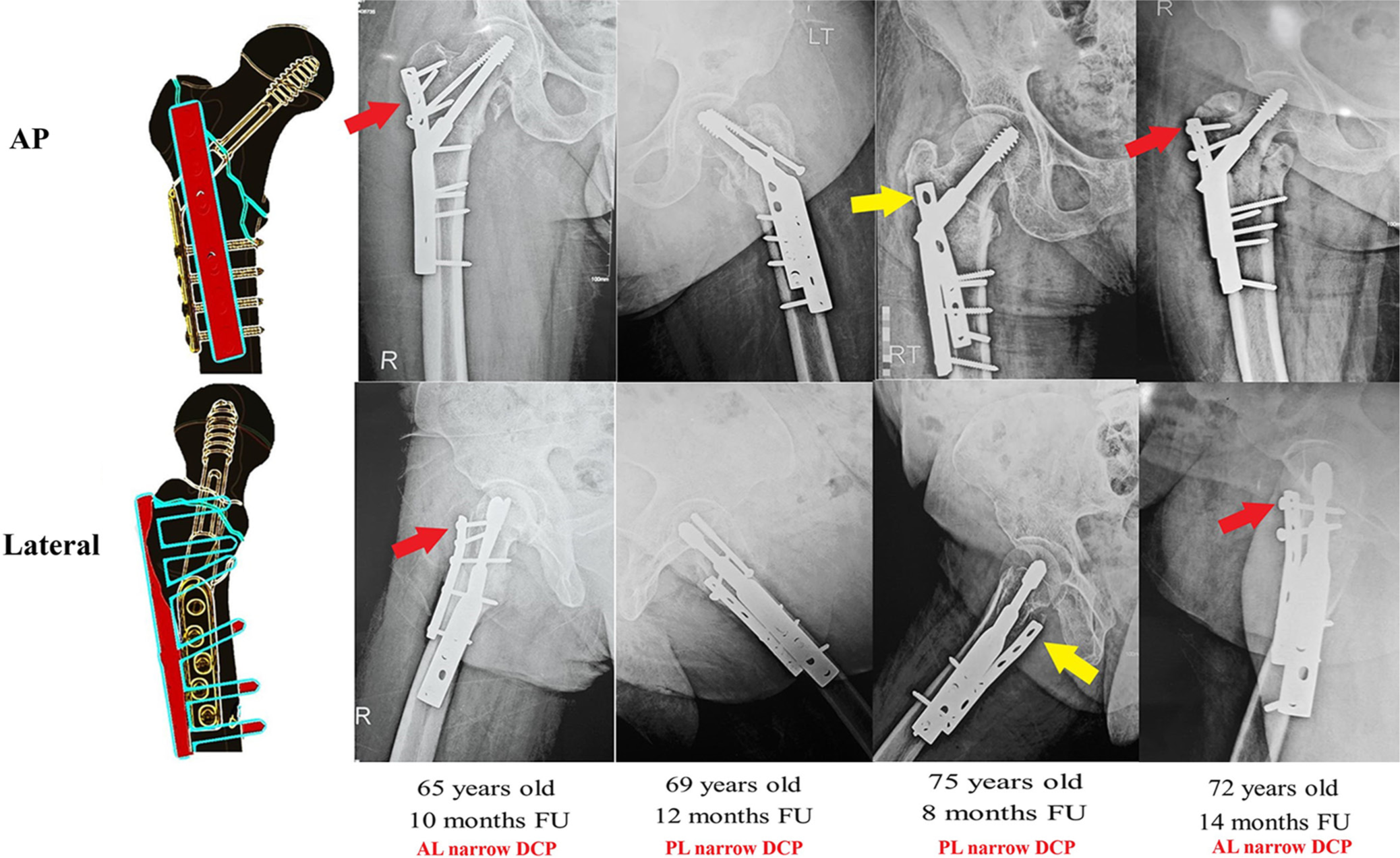
- A schematic diagram and follow-up radiographs of previous cases showing the relation of the dynamic hip screw side plate to the anterolateral narrow DCP plate; furthermore, it shows the optional anterolateral plate proximal fixation (indicated by red arrows) or leaving it without screws (indicated by yellow arrows). AL: Anterolateral, PL: Posterolateral, FU: Follow-up, DCP: Dynamic compression plate.
Another added advantage of applying TSPs is the increased fixation strength, as shown in a biomechanical study by Su et al., where the authors compared fixation using DHS alone to DHS with TSP in specimens of unstable trochanteric fracture after applying 10,000 cycles at 750-newton load, the authors reported that fracture displacement was significantly less in DHS with TSP group compared to fixation using DHS alone.[28] Applying a narrow DCP as an adjuvant to DHS fixation and an alternative to TSPs while managing unstable ITFs could serve most of the abovementioned functions regarding TSPs.
However, the results regarding which construct is superior for unstable ITF fixation are inconclusive, as some authors suggested the superiority of PFN over DHS/TSP;[15] furthermore, Alm et al. suggested no added value of using TSP/DHS over DHS alone.[29] At the same time, Geetala et al. reported better outcomes and lower costs with DHS/TSP than PFN.[23] Selim et al. reported the superiority of DHS/TSP over PFLP for unstable ITF fixation.[8]
In a scoping review by Alm et al. evaluating the role of TSP in unstable ITFs, the authors included 24 studies (six biomechanical and 18 clinical) where DHS/TSP was compared to various fixation devices. Of the 1.091 cases identified in clinical studies, 4% had mechanical failure and non-union, while 8% required implant removal (about a quarter were routine implant removal).[14] The authors reported that the available literature has no conclusive evidence regarding the absolute indications for using TSP or the clinical outcomes of its usage compared to other fixation devices. However, they stated that DHS/TSP is a more robust construct when compared to DHS alone, with better resistance to femoral shaft medialization and screw sliding; moreover, it could be a better option for unstable ITFs when PFN is unavailable.[14]
One of the advantages of using a narrow DCP, due to its low profile, is that it is versatile and can be applied easily on either the AL or PL surfaces (no specific anatomical location is necessary as with available TSPs), enabling surgeons to place the plate where they think it serves a better function, getting more robust screw purchase; furthermore, it could be bent or contoured to accommodate various trochanteric area anatomical configuration. The narrow DCP could function as a fracture reduction and fixation supplementary tool besides acting as a TSP, and if applied to the PL aspect, it could compensate and support the possible PL comminution. As the plate is placed in another plane and not over the DHS side plate, this could lead to less lateral prominence and less soft tissue irritation. Finally, although we did not perform a proper cost analysis, a narrow DCP could be cheaper and more affordable than the original TSPs. Furthermore, it is nearly available in most orthopedic theaters and could be used as a rescue plan if the prepared TSP could not be obtained or failed for any reason.
We admit that the current technique has some limitations. First, we did not offer biomechanical evaluation and comparison of the construct we described to other fixation devices. Second, if screw locations (for the narrow DCP and DHS side plate) were not correctly selected, changing the screw holes could further weaken the bone. Third, in cases where the trochanteric area is multi-fragmentary, the proximal segment of the narrow DCP could fail to buttress all fragments. Last, clinical data supporting the proper functionality of this construct are still to be provided.
CONCLUSION
Our proposed technique of using an AL or PL narrow DCP as a supplementary fixation tool acting as a preliminary fracture reduction maintenance tool and serving TSP function is viable, affordable, and easy to apply. However, a comparative study with other fixation methods is warranted to clarify probable technical difficulties and complications.
Authors’ contribution
OR: Carried out the idea and performed the surgery. AAK: Performed the literature search, drafted the manuscript, and designed the figures. OR: Did the critical revision. Both authors discussed and commented on the manuscript. Both authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
Ethical approval
Our institution’s ethical committee waived the requirement for ethical approval for this technical note, as it was deemed part of patient care. No new or experimental instruments were utilized in treating the patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Conflicts of interest
There are no conflicting relationships or activities.
Financial support and sponsorship: This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- All-cause mortality risk in aged femoral intertrochanteric fracture patients. J Orthop Surg Res. 2021;16:727.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fractures: Data from the Swedish fracture register. BMC Musculoskelet Disord. 2018;19:369.
- [CrossRef] [PubMed] [Google Scholar]
- Mortality incidence and its determinants after fragility hip fractures: A prospective cohort study from an Egyptian level one trauma center. Afr Health Sci. 2021;21:806-16.
- [CrossRef] [PubMed] [Google Scholar]
- Intramedullary nailing versus sliding hip screw for A1 and A2 trochanteric hip fractures. Bone Joint J. 2021;103B:775-81.
- [CrossRef] [PubMed] [Google Scholar]
- Dynamic hip screws versus cephalocondylic intramedullary nails for unstable extracapsular hip fractures in 2021: A systematic review and meta-analysis of randomised trials. J Orthop. 2023;36:88-98.
- [CrossRef] [PubMed] [Google Scholar]
- Prospective research comparing different trochanteric fracture fixation techniques. Cureus. 2024;16:e67774.
- [CrossRef] [Google Scholar]
- Should trochanteric fractures in elderly patients be treated by arthroplasty or internal fixation? Orthop Traumatol Surg Res. 2024;110:103778.
- [CrossRef] [PubMed] [Google Scholar]
- Management of unstable pertrochanteric fractures, evaluation of forgotten treatment options. SICOT J. 2020;6:21.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome of primary cemented bipolar hemiarthroplasty in older patients with unstable hip fracture: A prospective study. J Musculoskelet Surg Res. 2019;3:196.
- [CrossRef] [Google Scholar]
- Comparative evaluation of proximal femoral nail anti-rotation versus dynamic hip screw for stable intertrochanteric femoral fractures: A meta-analysis of clinical outcomes. J Musculoskelet Surg Res. 2024;8:335-48.
- [CrossRef] [Google Scholar]
- Femoral medialization, fixation failures, and functional outcome in trochanteric hip fractures treated with either a sliding hip screw or an intramedullary nail from within a randomized trial. J Orthop Trauma. 2016;30:642-6.
- [CrossRef] [PubMed] [Google Scholar]
- Does intramedullary nail have advantages over dynamic hip screw for the treatment of AO/OTA31A1-A3? A meta-analysis. BMC Musculoskelet Disord. 2023;24:588.
- [CrossRef] [PubMed] [Google Scholar]
- Implants for trochanteric fractures in Norway: The role of the trochanteric stabilizing plate-a study on 20,902 fractures from the Norwegian hip fracture register 2011-2017. J Orthop Surg Res. 2021;16:26.
- [CrossRef] [PubMed] [Google Scholar]
- Trochanteric stabilizing plate in the treatment of trochanteric fractures: A scoping review. Acta Orthop. 2021;92:733-8.
- [CrossRef] [PubMed] [Google Scholar]
- Functional and radiological outcomes of dynamic hip screw with trochanteric stabilizing plate versus short proximal femoral nail in management of unstable trochanteric fractures: A randomized-controlled trial. Jt Dis Relat Surg. 2022;33:531-7.
- [CrossRef] [PubMed] [Google Scholar]
- Augmentation of intramedullary nail in unstable intertrochanteric fractures with plate or cable. Front Surg. 2024;11:1293049.
- [CrossRef] [PubMed] [Google Scholar]
- Trochanter stabilising plate improves treatment outcomes in AO/OTA 31-A2 intertrochanteric fractures with critical thin femoral lateral walls. Injury. 2015;46:1047-53.
- [CrossRef] [PubMed] [Google Scholar]
- Expanding the indications for mini plates in the orthopedic trauma scenario: A useful alternative technique for maintaining provisional reduction and improving stability for complex periarticular fracture fixation of the upper limbs. J Orthop Case Rep. 2018;8:42-6.
- [Google Scholar]
- Temporary intra-operative reduction techniques for tibial fracture fixation: A review of the literature. Injury. 2010;41:1228-33.
- [CrossRef] [PubMed] [Google Scholar]
- General principles of orthopaedic plating and overview In: Banerjee A, Biberthaler P, Shanmugasundaram S, eds. Handbook of orthopaedic trauma implantology. Singapore: Springer Nature; 2023. p. :211-25.
- [CrossRef] [Google Scholar]
- AO surgery reference. 2022. Available from: https://surgeryreference.aofoundation.org/orthopedic-trauma/adult-trauma/proximal-femur/trochanteric-fracture-simple-pertrochanteric-with-posteromedial-involvement/sliding-hip-screw?searchurl=/searchresults [Last accessed on 2024 Oct 12]
- [Google Scholar]
- Comparison of intra-operative outcomes following internal fixation with trochanteric stabilisation plate or intramedullary nail in intertrochanteric fractures. Eur J Orthop Surg Traumatol. 2024;34:1193-9.
- [CrossRef] [PubMed] [Google Scholar]
- The clinical and economic impact of generic locking plate utilization at a level II trauma center. J Orthop Trauma. 2016;30(Suppl 5):S32-6.
- [CrossRef] [PubMed] [Google Scholar]
- The socioeconomic impact of orthopaedic trauma: A systematic review and meta-analysis. PLoS One. 2020;15:e0227907.
- [CrossRef] [PubMed] [Google Scholar]
- Provisional fixation of unstable femoral neck basicervical fractures: A web-based survey and biomechanical assessment using a sliding hip screw construct. J Musculoskelet Surg Res. 2022;6:70-6.
- [CrossRef] [Google Scholar]
- Unstable trochanteric fractures: The role of lateral wall reconstruction. Int Orthop. 2010;34:125-9.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of an attachable lateral support plate on the stability of intertrochanteric fracture fixation with a sliding hip screw. J Trauma. 2003;55:504-8.
- [CrossRef] [PubMed] [Google Scholar]
- No benefit of the trochanteric stabilizing plate on loss of fracture reduction in AO/OTA 31-A2 trochanteric fractures. Bone Jt Open. 2024;5:37-45.
- [CrossRef] [PubMed] [Google Scholar]







