Translate this page into:
Staged total hip arthroplasty using a handmade articulating spacer to manage bifocal-infected non-united femoral shaft and neck fractures. A case report and technical note
*Corresponding author: Mostafa A. T. Abdelhafez, Department of Orthopaedic and Trauma Surgery, Faculty of Medicine, Assiut University, Assiut, Egypt. mostafathabet1987@aun.edu.eg
-
Received: ,
Accepted: ,
How to cite this article: Abdelhafez MA, Arafa ME, Adam MF, Moustafa MM. Staged total hip arthroplasty using a handmade articulating spacer to manage bifocal-infected non-united femoral shaft and neck fractures. A case report and technical note. J Musculoskelet Surg Res. doi: 10.25259/JMSR_398_2024
Abstract
The coexistence of infected nonunion in both femoral shaft and neck fractures poses a multifaceted challenge, entailing complexities in approach, cost considerations, and management duration for both the orthopedic surgeon and the patient with limited documented evidence for appropriate management. This case report presents a distinctive instance of concurrent infected nonunion in femoral neck and shaft fractures. The treatment strategy involved a two-stage procedure. In the first stage, a handmade articulating antibiotic spacer was utilized to eradicate infection and achieve osseous union. Subsequently, a conventional primary total hip arthroplasty was performed to restore joint functionality. We suggest that this handmade spacer offers a cost-effective alternative, alleviating the economic burden associated with other revision modalities that tend to be more costly and technically demanding in such clinical scenarios.
Keywords
Arthroplasty
Femoral neck
Fractures
Handmade
Infection
Non-union
Revision
Spacer
Two stages
INTRODUCTION
The incidence of ipsilateral femoral neck and shaft fractures progressing to non-union remains unknown, but it is more likely to occur compared to isolated fractures. This higher likelihood could be attributed to two main factors: First, considerable vascular disruption results from high-energy trauma, and second, the presence of a free segment between the two fracture sites leads to significant soft-tissue disruption and inadequate fracture stability, further hindering proper healing and contributing to the progression to non-union.[1,2]
The non-union scenario is even worse if there is a concomitant fracture-related infection (FRI), and various management protocols are described as single-stage or multi-staged approaches utilizing multiple strategies and devices. Furthermore, antibiotic cement-impregnated intramedullary nails were suggested, with the advantages of antibiotic local delivery, maintaining long bone alignment, and achieving osseous union.[3]
The coexistence of infected nonunion in both femoral shaft and neck fractures is rare. It poses a challenging scenario for both the orthopedic surgeon and the patient with limited documented evidence for appropriate management.[4]
Here, we report a case of bifocal-infected non-union femoral fractures managed successfully using a staged protocol with a handmade articulating cement spacer aiming to eradicate the infection, followed by a second-stage total hip arthroplasty (THA) offers a cost-effective alternative, alleviating the economic burden associated with other revision modalities that tend to be more costly and technically demanding in such clinical scenarios.
CASE REPORT
A 45-year-old male patient, a manual worker, referred to our institute sustained a concomitant infected nonunion femoral shaft fracture with a collapsed femoral neck fracture fixed by three loose pulled-out cannulated screws, impending varus failure [Figure 1].
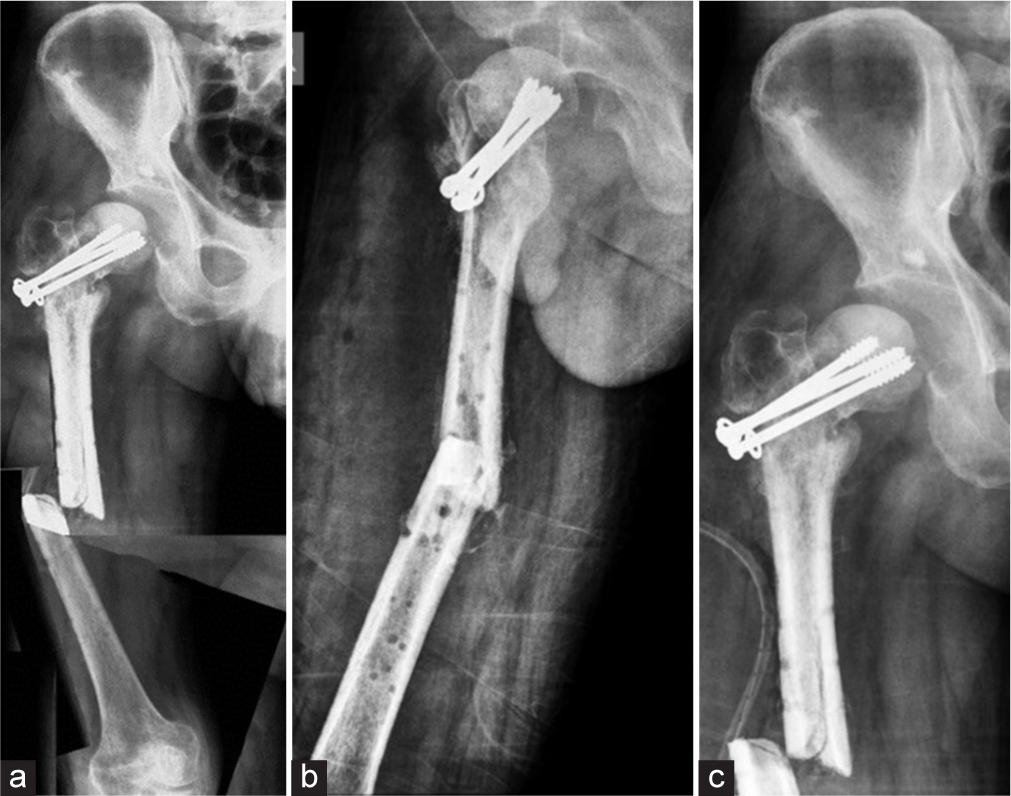
- (a and b) Anteroposterior and lateral radiographs showing nonunion diaphyseal femoral fracture with collapsed femoral neck fracture, (c) loose-pulled out femoral neck screws with varus failure.
The patient’s history revealed a complex injury following a motorbike accident six months ago, including an open grade IIIA fracture of the right femoral shaft and a closed ipsilateral femoral neck fracture, managed surgically in another hospital. The shaft fracture was initially addressed with an external fixator after wound debridement and the neck fracture was stabilized using percutaneous cannulated screws. Subsequently, definitive internal fixation of the femoral shaft was performed with a locked plate four days later.
However, four weeks later, the patient began experiencing night pain, fever, thigh swelling, and a discharging sinus. He was advised to take daily dressing and antibiotics, unfortunately, six weeks after index surgery. Laboratory tests indicated elevated abnormal levels of erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and leukocytosis with radiological evidence of no bridging callus at the fracture sites and heterogeneous periosteal reaction suggesting infected non-union based on FRI definition according to Metsemakers et al.[5] The plate was removed after unsuccessful multiple debridement attempts while the neck screws were retained as infection around the femoral neck fracture was suspicious.
On-admission and preoperative preparation
We planned a meticulous approach to eradicate the infection, and the patient did not report any chronic medical conditions or other injuries. Preoperative laboratory investigations, including CBC, ESR, CRP, liver function, and kidney function, and ensuring a two-week antibiotic-free interval before the surgery to optimize the surgical outcomes.
First-stage surgical intervention
The patient was placed laterally on the operative table under spinal anesthesia; using the previous incisions, the hip joint, and the femur were explored and showed loose pulled-out screws fixing the non-united neck of fracture with purulent discharge extending into the acetabulum, which was occupied by granulation tissue displacing eroded avascular femoral head.
All non-viable-infected tissues were excised and extensively debrided, including the scar tissue, sinus, and femoral head and neck after removal of the screws. The screw tracts were over-reamed. Five tissue specimens were collected from different locations: Subcutaneous tissues, the hip joint, the femoral canal, screw tracks, and the non-union sites for culture and sensitivity to identify potential infecting microorganisms. As part of the debridement, the medullary canal was prepared using a 13 mm reamer to accommodate a larger spacer.
Preparing the handmade spacer was a crucial and intricate step. We utilized a Kuntscher nail measuring 10 mm in diameter and 38 cm in length, estimated by the intramedullary guide length, as a spacer core. A 5 mm Schanz pin was tightened into the nail groove clockwise to create a secure, partially locked rigid construct; in addition, we bent the proximal smooth end of the Schanz pin to mimic a 130° neck-shaft angle [Figure 2].
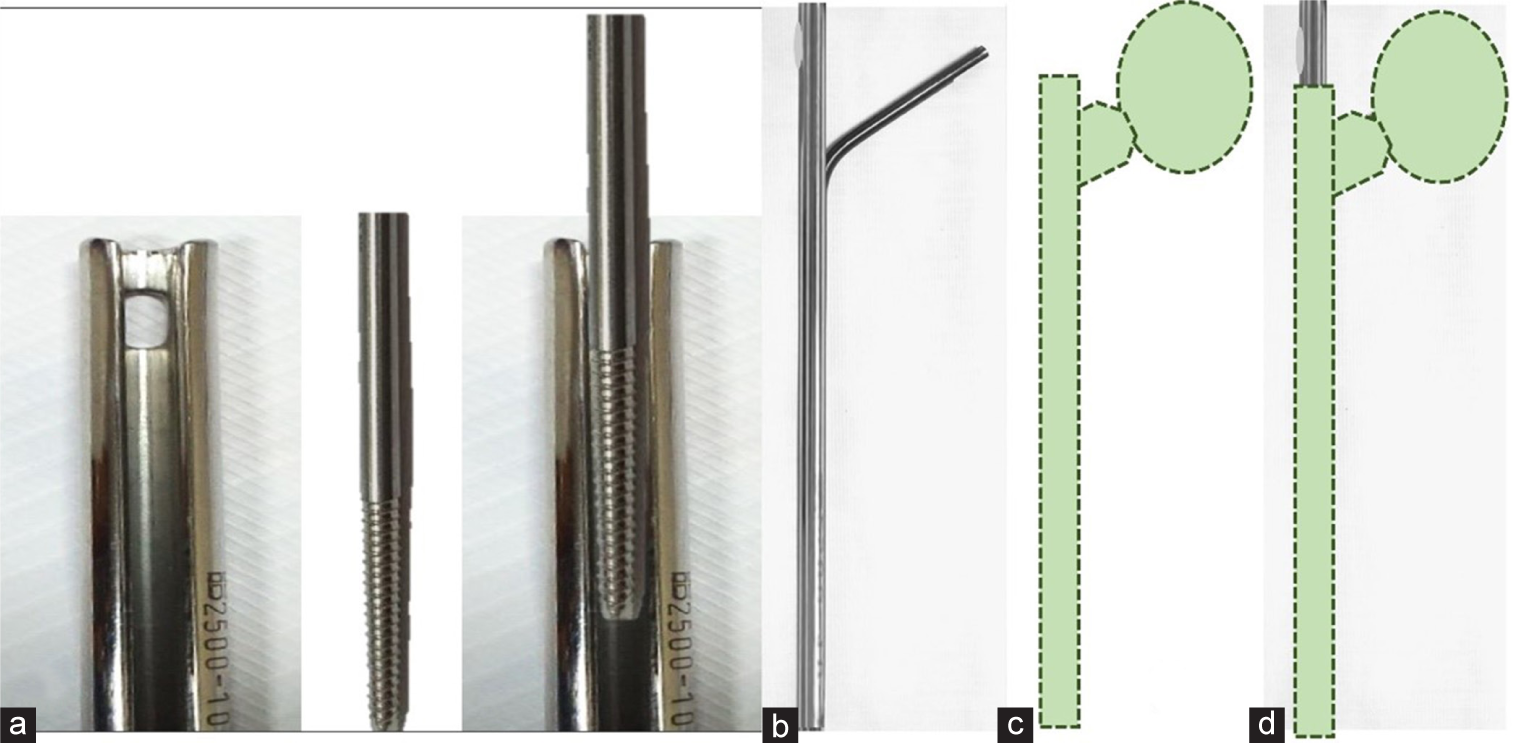
- (a) Threaded 5 mm Schanz screw was tightened through the Kuntscher nail groove, (b) the proximal smooth Schanz end was bent 130° to mimic the neck-shaft angle, (c and d) the diagram shows a handmade spacer, Kuntscher nail coated with cement.
As a coating, we mixed 4 g of thermostable vancomycin with two packages of polymethylmethacrylate (PMMA), each of 40 g. It was carefully molded using a 12 Fr chest tube to ensure a uniform coating, with the proximal part fabricated to match the geometry of the head and neck without cementing the nail eye [Figure 2]. Once the cement was set, the fracture ends were held in a reduced position, and the spacer was introduced into the medullary canal in an antegrade manner and was relocated into the acetabulum. The hip spacer was relatively stable upon testing, offering an acceptable range of motion with no impingement [Figure 3].

- (a and b) Immediate postoperative radiograph shows a handmade spacer with proper offset. (c and d) The last follow-up radiograph shows a consolidated mid-diaphyseal osseous union.
Postoperative course
The patient was encouraged to toe-touch weight-bearing using crutches as much as pain tolerated. Broad-spectrum antibiotic (Sulperazon) was started immediately postoperatively while waiting for the culture and sensitivity results, which 36 h. later revealed methicillin-resistant Staphylococcus aureus infection. Antibiotics (vancomycin + Sulperazon) were administered for six weeks.
The patient was advised to have ESR and CRP assessments every two weeks during the follow-up period. When these results showed normalization, a second stage and conversion to THA were decided after six weeks.
Unfortunately, the patients skipped follow-up visits and attended the clinic fully painless weight-bearing walking with a cane three months after the first stage. The ESR (20 mm/h) and CRP (4 mg/L) were normal, and the radiographs showed a maintained spacer position and satisfactory union of femoral midshaft fracture with a bridging callus [Figure 3].
Second-stage surgical intervention
After optimization of the patient’s general condition, the surgery was performed under spinal anesthesia through a modified direct lateral approach to the hip; the articulating spacer was dislocated by gentle rotation of the whole limb. Samples were obtained for culture from the acetabular side, the femoral shaft, and tissues around the spacer to ensure the eradication of infection. Further debridement of any suspicious tissues was performed.
To avoid undue torsion of the femoral shaft while preparing the femoral canal, which could lead to femoral refracture, the operating surgeon preferred to prophylactically fix the femoral shaft with a plate using a minimally invasive percutaneous plate osteosynthesis technique. The proximal screws were initially unicortical. Then, THA was performed using a cementless implant and a standard-size femoral stem; after ensuring the proper position and the reduction of the implant, the proximal screws of the plate were changed to longer screws. By the end of the surgery, 2 g of vancomycin were inserted into the wound [Figure 4].
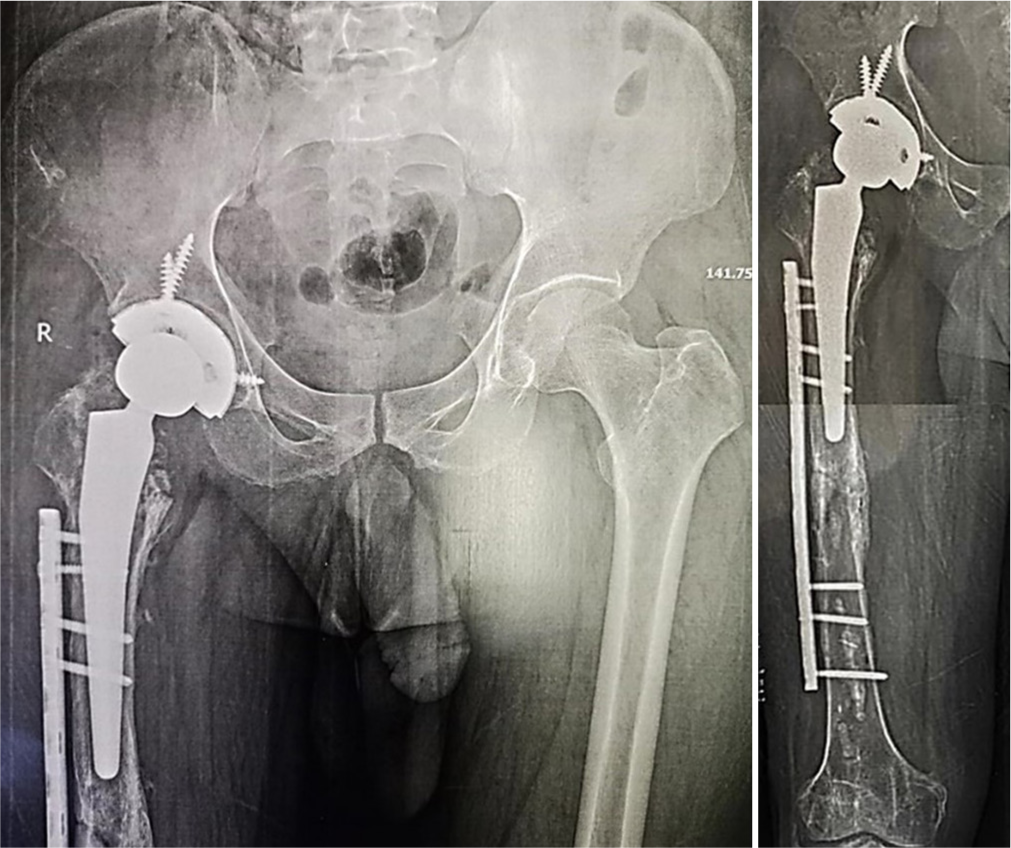
- Second-stage cementless total hip replacement with a prophylactic plate for femoral fracture.
RESULTS AND FINAL FOLLOW-UP
The patient was allowed partial weight-bearing for the initial six weeks. The sutures were removed at two weeks, and the wound healed properly. The results of tissue cultures revealed no bacterial growth.
At the last follow-up (12 months postoperatively), the patient walked without support, and the radiographs showed the optimum implant position. Functional assessment was satisfactory, with the Oxford Hip Score, EQ-5D, and EQ-Visual Analog Scale being 43, 0.864, and 84, respectively.
DISCUSSION
Concomitant-infected non-union femoral shaft and neck of femur fractures are rare but pose a challenging scenario. The outcomes are difficult to predict, considering the rarity of published evidence in dealing with such scenarios. Two-stage management is considered the gold standard for eradicating the infection, followed by obtaining fracture union for infected non-united long bone fractures.[6,7]
In the current case, we achieved satisfactory outcomes. We regained optimum hip joint function after using a handmade articulating spacer to eradicate infection and successfully achieving mid-diaphyseal osseous union as a first stage by utilizing cheap implants. This was followed by a successful second-stage THA surgery using a cementless implant and a usual-sized femoral stem.
First, we believed that the handmade spacer had the advantages of PMMA-mediated local delivery of antibiotics and reduced dead space. We added more antibiotics to the cement, which could be adjusted by the surgeon, unlike the readymade spacers, which come with a predetermined dose of antibiotics; this will lead to higher antibiotic concentration at the surgical site.[8]
Second, the spacer we used is articulating (by the 130° bent cement coated Schanz) and relatively long, preservation of soft tissue balance/tension at both the hip joint and the mid-shaft fracture levels and reduces complications such as leg length deficiency following second-stage surgery with minimal chance of cement mantle debonding because the characteristic clubs-shaped cross-section of the nail strongly bonds the cement to its folds; furthermore, it was easily extracted using hook extractor through the nail eye [Figure 5].
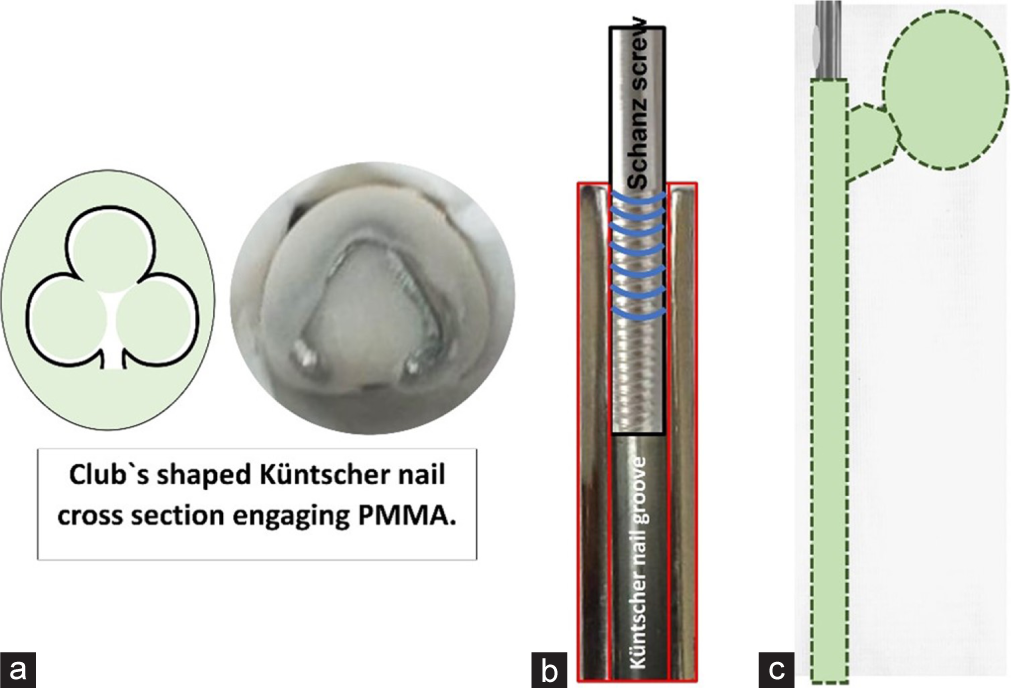
- The illustrated diagram shows (a) cement nail bonding, (b) Schanz-nail locking mechanism, and (c) handmade space and nail eye for extraction.
Third, allowing early weight-bearing is a significant achievement to improve outcomes and avoids disuse osteopenia following the first stage as the nail groove catches the threaded Schanz end, providing some sort of locking to achieve a rigid construct with a diameter matching the narrowest part of the medullary canal that resists rotational displacement through three-point fixation and interdigitation of the fracture ends that is added to achieve osseous union.[9]
Fourth, a standard cementless THA was performed. We achieved proper initial fracture union at the midshaft femoral fracture site, enabling to use of a usual length femoral stem and avoiding using a longer stem or revision THA implants with the addition of a protection plate through a minimally invasive technique bypass of both the united mid-diaphyseal fracture and the stem tip to decrease stress riser and guard against the risk of stress fracture allowing immediate safe weight-bearing postoperatively.
Although we did not report on the cost of the spacer we fabricated, however, Moerenhout et al. compared the cost of handmade or readymade cement spacers, and they reported that the handmade spacers are 40–50% cheaper than the readymade ones.[8]
CONCLUSION
A two-stage approach successfully managed a rare case of infected non-united bifocal femoral fracture (neck and midshaft). The first stage was performed by a handmade articulating cement spacer loaded with antibiotics, utilizing relatively cheap implants available in most orthopedic operative theaters. Furthermore, efficient first-stage surgery enabled the operating surgeon to use the usual cementless THA implants and avoid using revision or long-stem prostheses.
Authors’ contributions
MTA: Conceived and designed the study, conducted research, and provided research materials. MEA: Collected and organized data and provided logistic support. MFA: Analyzed and interpreted data. MAM: Wrote the initial and final draft of the article and provided logistic support. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published, and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Use of artificial intelligence (ai)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Conflicts of interest
There are no conflicting relationships or activities.
Financial support and sponsorship: This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Concomitant ipsilateral femoral neck and femoral shaft fracture nonunions: A report of three cases and a review of the literature. Iowa Orthop J. 2006;26:112-8.
- [Google Scholar]
- Delayed recognition of an ipsilateral femoral neck and shaft fracture leading to preventable subsequent complications: A case report. Patient Saf Surg. 2017;11:20.
- [CrossRef] [PubMed] [Google Scholar]
- Can antibiotic impregnated cement nail achieve both infection control and bony union in infected diaphyseal femoral non-unions? Injury. 2017;48:S66-71.
- [CrossRef] [PubMed] [Google Scholar]
- Salvaging chronic nonunion of femoral neck and infected nonunion of ipsilateral femoral shaft fracture using intramedullary antibiotic cement spacer and external fixator alone. Cureus. 2021;13:e12665.
- [CrossRef] [Google Scholar]
- Fracture-related infection: A consensus on definition from an international expert group. Injury. 2018;49:505-10.
- [CrossRef] [PubMed] [Google Scholar]
- A comparative study of treatment with external fixator versus antibiotic coated intramedullary nail in infected non-union long bones. Cureus. 2022;14:e29659.
- [CrossRef] [Google Scholar]
- Management of infected nonunion of the long bones by a multidisciplinary team. Bone Joint J. 2015;97B:814-7.
- [CrossRef] [PubMed] [Google Scholar]
- Economic advantage of “self-made” antibiotic-loaded spacer compared to prefabricated antibiotic-loaded spacer and spacer molds in two-staged revision arthroplasty. Acta Orthop Belg. 2021;87:557-62.
- [CrossRef] [PubMed] [Google Scholar]
- Kuntscher nail: A forgotten entity yet a reliable modality in treatment of winquist type I and II closed femoral shaft fractures. Cureus. 2020;12:e10608.
- [CrossRef] [PubMed] [Google Scholar]







