Translate this page into:
A case study and review of transient bone marrow edema or transient migratory osteoporosis in the knee
*Corresponding author: Rubén D. Arias Pérez, Department of Trauma and Orthopaedic Surgery, Universidad Pontificia Bolivariana, Medellín, Colombia. ruben.arias@upb.edu.co
-
Received: ,
Accepted: ,
How to cite this article: Jaramillo Quiceno A, Sarmiento Riveros PA, Arias Pérez RD, Vega Arango M, Rodriguez Arguello JL. A case study and review of transient bone marrow edema or transient migratory osteoporosis in the knee. J Musculoskelet Surg Res. doi: 10.25259/JMSR_500_2024
Abstract
Transient bone marrow edema (BME) syndrome, also known as transient migratory osteoporosis, is a rare clinical entity characterized by severe, temporary arthralgia in the lower extremities without trauma history. It presents as focal or regional radiographic osteopenia and as a hallmark BME signal on magnetic resonance imaging (MRI). The syndrome’s idiopathic nature is underscored by its spontaneous resolution and variability in clinical presentations, with inconsistent joint involvement. A clinical case of a 57-year-old male illustrates the condition’s characteristics: Intense, non-traumatic knee pain initially located in the medial femoral condyle with typical imaging findings on MRI, resolved through analgesia and weight-bearing restriction. The patient experienced recurrence in the lateral femoral condyle, again resolving with similar management. This case emphasizes the disorder’s heterogeneity and intends to raise awareness in the medical community, where lack of knowledge and standardized nomenclature has complicated its recognition, leading to unnecessary interventions.
Keywords
Bone marrow
Edema
Knee
Migratory
Osteoporosis
Transient
INTRODUCTION
Within the intricate landscape of musculoskeletal pathology, certain clinical entities emerge as rare enigmas, challenging the diagnostic acumen of physicians. One of those elusive conditions that transcend the realms of rheumatology, orthopedics, and radiology is transient bone marrow edema (BME) syndrome, commonly recognized as transient migratory osteoporosis.[1,2] This puzzling disorder manifests as a clinical rarity, characterized by severe transient and migratory arthralgia in the lower extremities, without trauma history.[1]
Etiology remains unknown, as it typically materializes without identifiable triggering factors,[2] confusing the medical community. Thus, for now, it is still called idiopathic.[3] This condition is most frequent in middle-aged men (40–60 years), with a male-to-female ratio of 3:1, and in pregnant women, usually in the third trimester. The first joint discomfort lasts around six to nine months, with slow, progressive, and finally total remission, and it primarily affects the hips and the knees. The most common physical examination findings are effusion and edema, with no significant limitations in range of motion.[4]
A critical challenge in diagnosing this condition lies in its broad spectrum of differential diagnoses, particularly osteonecrosis and inflammatory arthropathies. Misdiagnosis can result in significant consequences, such as inappropriate invasive interventions for osteonecrosis or unwarranted immunosuppressive therapies for inflammatory conditions. The subtle differences between these conditions and transient BME syndrome underline the necessity for comprehensive laboratory and radiological evaluations. Initial diagnostic efforts often yield normal or non-specific results, with chronic inflammation and negative cultures being common findings in invasive methods such as joint fluid analysis or synovial bone biopsy.[5] Densitometry may demonstrate demineralization, particularly hip involvement, although its utility is limited in other joints, such as the knee. Ultimately, diagnosis ends up being a process of exclusion of more morbid and unmissable entities.[6]
Imaging contributes substantially to the definitive diagnosis. Radiographs exhibit focal osteopenia and can exclude other differential diagnoses.[7] Magnetic resonance imaging (MRI) plays a crucial role, with BME being the most salient feature. BME is a non-specific finding with many possible origins, but localized extension and subchondral sparing raise the suspicion of this disorder.[4] Diagnostic certainty increases when multiple anatomical areas are involved, especially when a migratory pattern to other joints is identified.[5] The clinical manifestation is variable and may manifest in one or more joints concurrently or successively, either within the same limb or extending to the contralateral counterpart, and very rarely affecting a single joint.[7,8]
There is currently no consensus in medical terminology to define it because it is a rare disease and diagnosis by exclusion, given that numerous publications employ terms associated with osteoporosis without significant evidence of bone demineralization.[6] Making its understanding, diagnosis, and treatment even more difficult. Considering the relatively rare nature of this entity, we present the case of a 57-year-old man with transient BME/transient migratory osteoporosis in the knee to present the radiological evolution during this disorder and further discuss the difficulties associated with its diagnosis and treatment.
CASE REPORT
A 57-year-old male patient presented with a sudden onset of unprovoked and intense medial-sided knee pain, lasting for one month, as it progressed until it impaired daily activities. Past medical history was unremarkable, apart from hypertension. On physical examination, he presented an antalgic gait, moderate effusion, and medial-sided pain of the knee. The overall range of motion was preserved, with no ligamentous instability or positive meniscal signs.
Plain radiographs of the knee were normal and presented normal laboratory results: C-reactive protein (CRP) 1 mg/dL, erythrocyte sedimentation rate (ESR) 5 mm/h, rheumatoid factor and anti-citrullinated protein antibodies negative, negative ANA’s, hemogram without alterations. MRI revealed BME within the medial femoral condyle, without other alterations [Figure 1a-c]. The patient was managed with analgesia (Naproxen 500 mg twice daily for 5 days) and weight-bearing restriction with symptomatic improvement at eight weeks. After a three-month interval, a recurrence of severe pain in the same knee prompted further evaluation. A new MRI showed a significant decrease in edema of the medial femoral condyle and pronounced BME now localized to the lateral femoral condyle with edema of adjacent soft tissues [Figure 1d-f]. A complete resolution of the symptoms was achieved with the same management strategy.
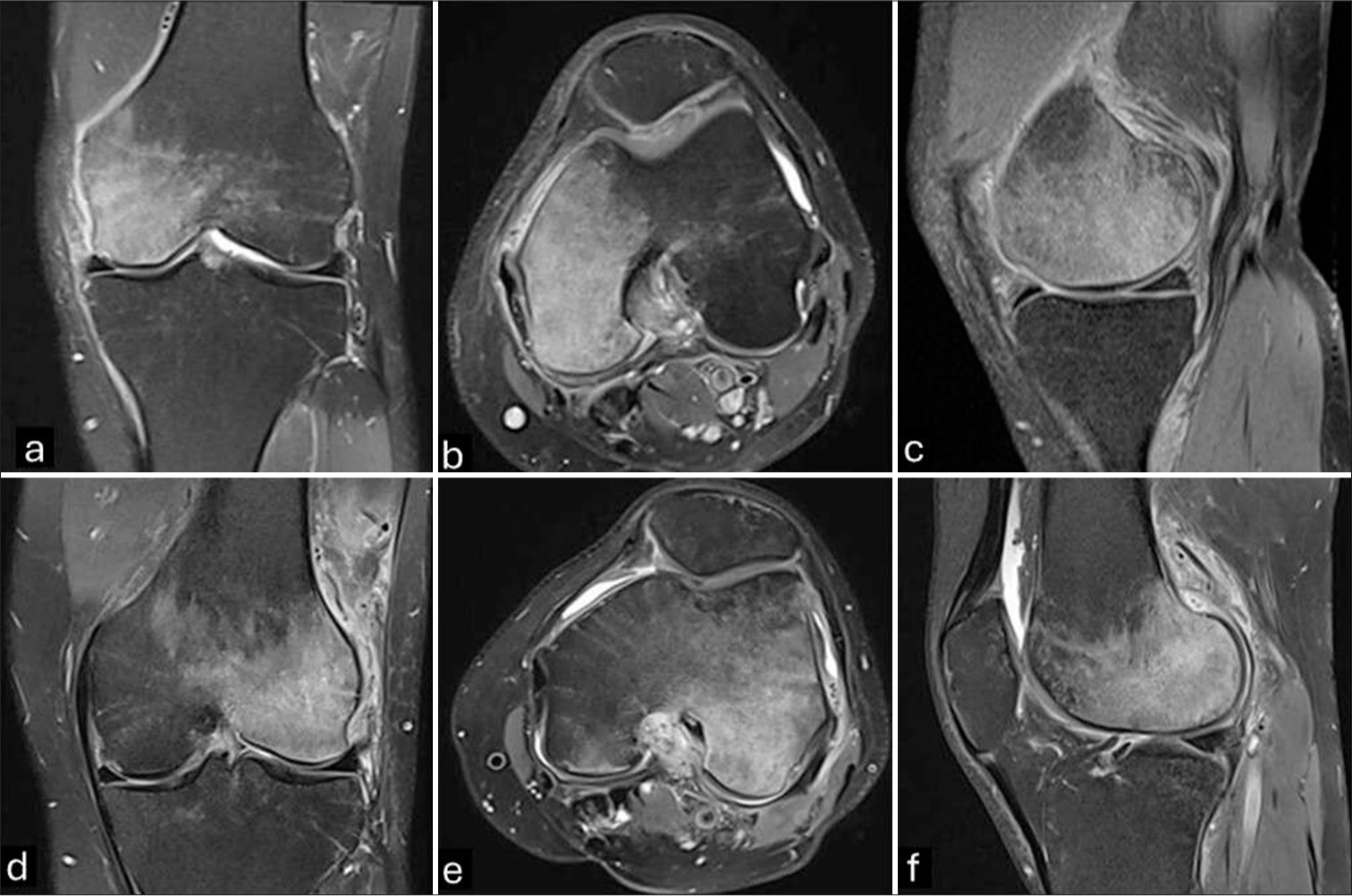
- MRI of the left knee. Initial MRI of the left knee. Bone marrow edema signal involving the medial femoral condyle, without subchondral bone plate or cartilage abnormalities. Pericapsular edema and synovitis are noted. (a) Coronal PD FS. (b) Axial PD FS. (c) Sagittal PD FS. (d) Three-month follow-up MRI of the left knee. There is complete resolution of the BME signal in the medial femoral condyle with extensive bone marrow edema involving the lateral counterpart. There is capsulitis, synovitis, and soft-tissue edema. Coronal PD FS. (e) Axial PD FS. (f) Sagittal PD FS. (MRI: Magnetic resonance imaging, PD: Proton density, FS: Fat-saturated, BME: Bone marrow edema).
At three months of follow-up, the patient was asymptomatic with no significant findings at physical examination. However, due to the history of severe pain without apparent cause, the following paraclinical tests were ordered. All were within normal ranges, PTH: 21 pg/mL; TSH: 1.6 IU/L; 24 h urine calcium: 120 mg/24 h; serum calcium: 10.3 mg/dL; serum phosphorus: 3.2 mg/dL; Vitamin D (25-OH-D): 32 ng/mL; alkaline phosphatase: 90 U/L; total serum proteins 6.83 g/dL; CRP: 2 mg/dL; ESR 8 mm/h; and hemogram without alterations. An MRI demonstrated a significant improvement of the previously observed abnormalities in the femoral condyles, little joint effusion, and minimal subchondral edema in the lateral tibial plateau [Figure 2].

- Last magnetic resonance imaging of left knee. A three-month follow-up. (a and b) Complete resolution of the bone marrow edema signal is noted. (c and d) A residual irregularity and flattening of the subchondral bone plate is seen at the weight-bearing area of both lateral and especially medial femoral condyles.
DISCUSSION
This case involves a male with migratory BME of the knee, a rare and diagnostically challenging condition. Initial MRI findings showed BME localized in the medial femoral condyle, which later shifted to the lateral femoral condyle and subsequently to the lateral tibial plateau. The dynamic and migratory nature of the edema, despite conservative treatment and weight-bearing restrictions, suggests a more complex underlying pathophysiology than is typically seen in transient BME syndrome or osteoporosis. This highlights the importance of considering such migratory patterns in both diagnosis and treatment planning. Migratory BME is an uncommon phenomenon often observed in the hip, although its appearance in the knee has been documented in a few case reports and small series.[1,2] The shifting pattern observed in this patient’s MRI images mirrors findings from studies where migratory BME is noted to change location within the same joint or even in contralateral joints.[3] Such migration is atypical for conditions such as osteonecrosis or inflammatory arthropathies, further supporting the diagnosis of transient migratory BME. Recognizing this migratory nature is critical for treatment decisions, as it underscores the need for careful monitoring and a tailored management approach that avoids unnecessary or aggressive interventions.
Moreover, transient BME is typically self-limiting and often resolves within months, which aligns with the improvement seen in this case. However, the recurrence and intercompartmental migration add complexity to the diagnosis and suggest that underlying factors, potentially biomechanical or vascular in origin, may contribute to the unusual presentation.[4] Cases like this also highlight the potential utility of serial imaging in monitoring the progress and resolution of BME, as initial imaging may not fully capture the evolving nature of the condition.
The absence of persistent symptoms despite ongoing imaging abnormalities emphasizes the need to consider clinical presentation alongside imaging findings. This case also underscores the importance of avoiding aggressive intervention in transient BME cases, as conservative treatment and patient monitoring can lead to resolution without invasive measures.[8] The diagnosis of this entity results from the process of excluding other more frequent pathologies, such as infection, osteonecrosis, inflammatory arthropathy, and stress fractures, among others.[4] It requires a complete investigation, including multiple laboratory and imaging examinations. As a primary diagnostic tool, basic radiographs may not reveal changes in the early stages but typically manifest alterations between three and six weeks after the onset of symptoms, characterized by signs of regional bone demineralization or osteopenia.[4]
On the other hand, MRI emerges as the most informative imaging study to evaluate this condition.[4] Key findings include focal BME with subchondral sparring. However, BME, especially when confined to a specific area, can be seen in trauma, tumors, infections, osteonecrosis, or other arthropathies. Thus, due to its lack of specificity, it is imperative to rule them out.[3] This necessitates a thorough interrogation, a comprehensive physical examination, and other relevant tests to ensure the prudence of avoiding therapeutic interventions that might impose additional morbidity on the patient.[1]
While this pathology is considered self-limiting and exhibits a favorable response to conservative management involving analgesics and weight-bearing restriction, various therapeutic approaches have been proposed.[8,9] One such approach involves the use of iloprost (a synthetic analog of prostacyclin that has vasodilatory, vascular remodeling, and anti-inflammatory effects and inhibits platelet aggregation), which is associated with reductions in symptom duration and MRI-detected abnormalities. Its proposed mechanism – enhancing venous drainage and reducing intramedullary pressure through vasodilatory and anti-inflammatory effects – addresses the hypothesized vascular component of this pathology.[9] While promising, the risks of iloprost, such as potential systemic side effects, including hypotension and gastrointestinal symptoms, must be carefully weighed against its benefits.
Other therapeutic options include bisphosphonates, which aim to mitigate focal low bone density changes, and extracorporeal shock wave therapy, which is proposed to stimulate osteoblastic activity and regeneration.[10] For more invasive cases, surgical decompression has been suggested to address elevated intramedullary pressure, though this is reserved for refractory cases due to the morbidity associated with the proposed surgery.[8] It is important to note that, despite these proposed interventions, the self-limiting nature of the disease and the efficacy of conservative measures underscore the importance of carefully weighing the potential benefits against the morbidity associated with more aggressive therapeutic approaches.[5] Since physicians do not know enough about the disease, it is easy to make misdiagnoses and mistreatments that could end up worsening the progression of the disease and impairing the patient’s quality of life.
On the other side, in medical literature, various terms are employed to denote the same pathological condition, including transient osteoporosis, migratory regional osteoporosis, pregnancy- and lactation-associated osteoporosis, and transient BME syndrome.[6] A contentious issue persists regarding whether these designations delineate distinct entities or represent a continuum within the spectrum of a single disease. Nevertheless, commonalities in MRI characteristics are evident across these terminologies.[6] Clinically, patients typically present with progressive arthralgia in the lower extremity, which spontaneously improves, only to recur in a migratory fashion, affecting either different joints or distinct regions within the same joint.[3]
The nomenclature “osteoporosis” is a subject of ongoing debate due to the lack of consistent evidence supporting the presence of osteoporosis in affected cases.[5,6] Many studies relying on the subjective interpretation of radiographic demineralization or MRI contribute to this ambiguity.[6] Consequently, some authors, based on the clinical attributes of the phenomenon, prefer to designate it as transient BME syndrome. The absence of a standardized term for this entity in the International Classification of Diseases, 11th Revision (ICD-11), coupled with the absence of a universally accepted definition, hampers effective communication. The current terminology employed for these closely interrelated entities not only presents a perplexing array but also lacks standardization.[6] This absence of formalized definitions impedes the precise diagnosis, exploration of disease mechanisms, and formulation of effective treatment strategies. Without a clear definition of the ICD-11, advancing research, exploring pathophysiology, and designing targeted treatments remain difficult. Given the self-limiting nature of this condition and the effectiveness of conservative treatment, carefully weighing the benefits and risks of any intervention is essential.
CONCLUSION
This case report and literature review highlight the diagnostic challenges of the knee’s transient BME syndrome or transient migratory osteoporosis. The case exemplifies the condition’s complex presentation of severe, migratory joint pain without clear cause, underscoring MRI’s role in diagnosis and the effectiveness of conservative management. The lack of standardized terminology, with terms such as “transient osteoporosis” and “transient bone marrow edema syndrome,” complicates clinical communication. This ambiguity points to the need for unified terminology to improve diagnosis, research, and treatment approaches for this self-limiting condition.
Authors’ contributions
AJQ, PAS, and RDA: Participated in all stages of writing this manuscript. MVA: Participated in the systematic reading of diagnostic images and manuscript preparation. JLR: Participated in reviewing the topic and preparing the manuscript draft. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published, and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI
Conflicts of interest
There are no conflicting relationships or activities.
Financial support and sponsorship: This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Regional migratory osteoporosis of the knee: A literature overview. Musculoskelet Surg. 2023;107:159-64.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of Vitamin D and C on bone marrow edema syndrome-A scoping review of the literature. J Clin Med. 2022;11:6820.
- [CrossRef] [PubMed] [Google Scholar]
- Transient migratory osteoporosis in lower limbs. Reumatol Clin. 2019;15:246-8.
- [CrossRef] [PubMed] [Google Scholar]
- Transient osteoporosis: Not just the hip to worry about. Bone Rep. 2016;5:308-11.
- [CrossRef] [PubMed] [Google Scholar]
- The terminologies of transient, migratory, or localized osteoporosis, and bone marrow edema syndrome: A scoping review. Osteoporos Int. 2024;35:217-26.
- [CrossRef] [PubMed] [Google Scholar]
- Regional migratory osteoporosis-a rare cause of knee pain (case report) J Orthop Case Rep. 2023;13:145-8.
- [CrossRef] [PubMed] [Google Scholar]
- How we manage bone Marrow Edema-an interdisciplinary approach. J Clin Med. 2020;9:551.
- [CrossRef] [PubMed] [Google Scholar]
- Management of transient bone osteoporosis: A systematic review. Br Med Bull. 2023;147:79-89.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of various treatment modalities for the management of bone marrow edema syndrome/transient osteoporosis in men and non-pregnant women: A systematic review. Osteoporos Int. 2023;34:269-90.
- [CrossRef] [Google Scholar]







