Translate this page into:
A comprehensive review of rehabilitation strategies post-orthopedic intervention in pediatric cerebral palsy
*Corresponding author: Abdullah Al Shami, Department of AMC Therapy Pediatrics, Hamad Medical Corporation, Doha, Qatar. aalshami1@hamad.qa
-
Received: ,
Accepted: ,
How to cite this article: Al Shami A. A comprehensive review of rehabilitation strategies post-orthopedic intervention in pediatric cerebral palsy. J Musculoskelet Surg Res. 2025;9:42-8. doi: 10.25259/JMSR_204_2024
Abstract
Cerebral palsy (CP) often requires orthopedic surgery to address musculoskeletal issues such as contractures and joint dislocations. Effective post-surgery rehabilitation is crucial for improving functional outcomes and quality of life in pediatric CP patients. This narrative review identifies and evaluates rehabilitation strategies for post-orthopedic surgery in children with CP. A search of databases (PubMed, Google Scholar, and Cochrane Library) focused on articles from the past 20 years using keywords such as “cerebral palsy,” “pediatric rehabilitation,” “post-orthopedic surgery,” and “functional outcomes.” Key rehabilitation components include pre-surgical preparation, acute post-surgical management, sub-acute interventions, and long-term maintenance. Evidence highlights the benefits of a multidisciplinary approach involving physical and occupational therapy. Functional improvements are measured using tools such as the gross motor function measure and the pediatric evaluation of disability inventory. Effective rehabilitation for pediatric CP patients requires a tailored, multidisciplinary approach. Best practices include early mobilization, personalized exercises, and long-term strategies. Future research should optimize protocols and explore innovative techniques to enhance outcomes.
Keywords
Cerebral palsy
Orthopedic intervention
Pediatric
Post-operative care
Rehabilitation
Strategies
INTRODUCTION
Cerebral palsy (CP) is a group of permanent movement disorders that arise in early childhood due to abnormal development or damage to brain regions responsible for movement, balance, and posture.[1] As the most prevalent motor disability in childhood, CP affects approximately 2–3/1000 live births globally.[2] Children with CP often face additional comorbidities, including intellectual disabilities, seizures, visual and auditory impairments, and speech and language disorders.[1]
Motor impairments in CP are categorized based on the nature and distribution of movement difficulties, including spastic, dyskinetic, ataxic, and mixed types, with spastic CP being the most common.[3] The severity of CP varies, ranging from mild motor delays and slight alterations in muscle tone, which may affect tasks such as writing or fine motor activities, to severe forms involving significant muscle spasticity, rigidity, or dyskinesia that impact fundamental movements such as sitting, standing, or walking.[4] Severe cases may also lead to contractures, further restricting mobility.[4]
Post-operative rehabilitation plays a crucial role in optimizing functional outcomes and enhancing the quality of life (QoL) for pediatric CP patients. Effective rehabilitation strategies are essential to address CP’s diverse challenges, including the variability in symptoms, the need for personalized treatment plans, and the aim of maximizing independence and participation in daily activities. Despite the acknowledged importance of post-operative rehabilitation, there remains a lack of consensus on the most effective strategies, resulting in varied practices and outcomes.[5]
This literature review provides a comprehensive analysis of current rehabilitation strategies following orthopedic interventions in pediatric CP patients. By examining existing studies and evidence, we aim to identify effective rehabilitation protocols, highlight gaps in current knowledge, and offer recommendations for future research and clinical practice. This review is motivated by the need to standardize post-operative care to improve functional outcomes and overall QoL for children with CP.[5]
I explored various rehabilitation approaches, including physical therapy, occupational therapy, the use of assistive devices, and innovative therapeutic interventions. In addition, we discuss the role of multidisciplinary teams in delivering holistic care and the importance of individualized treatment plans tailored to each child’s specific needs. Through this comprehensive analysis, we seek to contribute to enhancing post-operative rehabilitation strategies and improving the QoL for pediatric patients with CP.
MATERIALS AND METHODS
Methods
This original review was conducted in August 2023. The author performed a search through PubMed, MEDLINE, Cochrane Library, and Google Scholar using the following keywords: “cerebral palsy,” “rehabilitation,” “orthopedic surgery,” “postoperative care,” “physical therapy,” “occupational therapy,” “assistive devices,” and “multidisciplinary care.”
Inclusion criteria
Population: Pediatric patients aged 0–18 years diagnosed with CP
Intervention: Post-operative rehabilitation following orthopedic interventions
Outcomes: Studies reporting quantitative or qualitative outcomes related to rehabilitation efficacy
Publication Language: Only articles published in English were included
Publication Date: Articles published between 2003 and 2024 were considered to ensure coverage of recent publications
Study Design: A variety of study designs were included, such as randomized controlled trials, cohort studies, case–control studies, observational studies, and narrative reviews to capture a wide range of evidence.
Selection process
The author conducted the literature search. Using Zotero, duplicate articles were identified and removed. After removing duplicates, the remaining articles were screened based on titles and abstracts to ensure eligibility for inclusion.
During the screening process, the authors evaluated the titles and abstracts of the identified articles independently. Studies that did not focus on post-operative rehabilitation for CP were excluded.
Following the initial screening, the full text of the selected articles was reviewed to confirm their eligibility for inclusion in the study [Tables 1 and 2]. Discrepancies between the authors during the screening and full-text review stages were resolved through discussion or consultation with a third reviewer.
| Title of the study | Year of publication | Design | Number of studies included (study types) | Outcome measures reported | Recommendations |
|---|---|---|---|---|---|
| The role of hip surveillance in children with CP (Shore et al.) | 2012 | Review | 12 studies (RCTs, cohort studies and observational study) | Hip displacement monitoring through radiographic measures | Regular hip surveillance is essential for early intervention, reducing complications, and surgeries. |
| Multidisciplinary rehabilitation for patients with CP (Trabacca et al.) | 2016 | Review | 15 studies (4 RCTs, 6 cohort studies, 5 case reports) | QoL, functional independence (PEDI) | Encourages collaborative care models with interdisciplinary teams to improve long-term outcomes. |
| An Interdisciplinary Approach for Treating Children with CP (Keys and Lewis) | 2019 | Review | 10 studies (5 RCTs, 3 cohort studies, 2 qualitative studies) | Coordination of care, motor function (GMFM) | Promotes interdisciplinary teamwork to enhance care quality and child outcomes. |
| Family-centered approach in the management of children with CP (Aydin and Nur) | 2012 | Review | 9 studies (2 RCTs, 4 case studies, 3 qualitative studies) | Family engagement and satisfaction (Family Impact Scale) | Recommends involving families actively in treatment plans for better adherence and outcomes. |
| What’s new in the orthopedic treatment of CP (Aversano et al.) | 2017 | Review | 18 studies (8 RCTs, 7 cohort studies, 3 case reports) | Surgical outcomes (GMFM, hip migration index) | Suggests using updated surgical techniques and post-operative care protocols for better outcomes. |
| Rehabilitative therapies in CP (Damiano) | 2009 | Review | 20 studies (6 RCTs, 8 cohort studies, 6 case studies) | Motor function (GMFM), therapy effectiveness | Encourages evidence-based therapies but highlights the need for further research to optimize protocols. |
| The management of scoliosis in children with CP (Cloake and Gardner) | 2016 | Review | Scoliosis severity index, QoL index | Surgical intervention with 6-month follow-up, focusing on post-surgical rehabilitation | Improved spinal alignment and QoL observed post-surgery. |
CP: Cerebral palsy, PEDI: Pediatric evaluation of disability inventory, GMFM: Gross motor function measure, QoL: Quality of life, RCT: Randomized controlled trial
| Title of the study | Year of publication | Design | Population (number, ages, genders) | Outcome measures (scales/tools) | Intervention protocol (frequency, duration, type) | Results |
|---|---|---|---|---|---|---|
| Recovery of muscle strength following multi-level orthopedic surgery in diplegic CP (Seniorou et al.) | 2007 | Case Study | 24 children with diplegic CP (aged 6–16 years, 15 males, 9 females) | Muscle strength (isokinetic dynamometry), GMFM | Sessions: 3 times/week, Duration: 12–16-week post-surgery, Exercises: Strength training, gait training, functional mobility tasks | Significant improvement in muscle strength and walking ability over time post-surgery. |
CP: Cerebral palsy, GMFM: Gross motor function measure, RCT: Randomized controlled trial
Data extraction and synthesis
Key information was extracted from the included studies using a structured data extraction form. The data collected included:
Study design, sample size, and patient characteristics (age and CP severity).
Orthopedic intervention type and the post-operative rehabilitation strategies employed.
Outcomes reported, such as motor function improvements, QoL, or use of assistive devices.
Outcome measurement tools used, including the gross motor function measure (GMFM).
Follow-up duration and outcome measurement tools used (e.g., GMFM).
Given the heterogeneity in study designs and rehabilitation interventions, a narrative synthesis approach was employed. Studies were grouped according to common themes, such as rehabilitation modalities (e.g., physical therapy and occupational therapy) and outcome types (e.g., motor function and QoL). Patterns and discrepancies were identified to provide meaningful insights into post-operative care for pediatric CP patients.
Quality Assessment: Although a formal meta-analysis was not conducted, the quality of studies was considered by looking at each study’s methodology and outcome measures. Moreover, studies were also categorized based on levels of evidence (e.g., randomized controlled trials and observational studies).
RESULTS
Results: Rehabilitation strategies post-orthopedic intervention in pediatric CP
Pediatric CP often results in a range of orthopedic complications that can significantly impact mobility and QoL. The GMFCS is instrumental in assessing these mobility challenges, providing a framework for categorizing the gross motor abilities of children aged 2–18 years with CP. This system not only aids in understanding individual capabilities but also informs the planning and implementation of rehabilitation strategies post-orthopedic intervention.[6,7]
Orthopedic challenges in pediatric CP
Children with CP commonly face orthopedic issues stemming from muscle spasticity, weakness, and abnormal muscle tone, leading to conditions such as contractures, hip displacement, scoliosis, and foot and ankle deformities.[8]
These complications include:[8]
Contractures: The permanent shortening of muscles or tendons around joints, leading to stiffness and limited movement[8]
Hip Displacement: Hip subluxation or dislocation due to muscle imbalances around the hip joint, which can cause pain and affect mobility[8]
Scoliosis: Abnormal curvature of the spine, which can impact posture and respiratory function[8]
Foot and Ankle Deformities: Conditions such as equines (tiptoe walking) that affect gait and overall mobility.[8]
These complications necessitate timely orthopedic interventions, which, when followed by structured rehabilitation strategies, can significantly enhance functional outcomes and overall QoL for affected children.[5]
Early detection and intervention
The importance of early detection of CP cannot be overstated, as timely identification enables healthcare providers to implement preventive strategies against orthopedic complications.[9]
Recent advancements in diagnostic tools, including clinical assessments and neuroimaging, facilitate the early intervention necessary to mitigate the impact of musculoskeletal issues on mobility and functional abilities.[9] The significance of early detection and intervention in CP extends beyond neurological considerations to encompass the prevention and management of orthopedic conditions commonly associated with the disorder. Timely identification of CP allows healthcare providers to implement proactive strategies to address musculoskeletal issues, such as muscle contractures, joint deformities, and impaired mobility, which can significantly impact a child’s functional abilities and QoL.[9]
For instance, hip surveillance protocols that involve regular monitoring can lead to timely interventions, such as physical therapy or surgical procedures, thereby preventing the onset of severe hip dislocation.[10,11]
Treatment objectives for patients with CP
The treatment objectives for children with CP differ significantly between ambulatory and non-ambulatory patients. Understanding these distinctions is essential for formulating effective rehabilitation strategies.
Ambulatory patients
For ambulatory children (GMFCS Levels I–III), the primary treatment goals focus on enhancing mobility, improving balance and coordination, and promoting independence in activities of daily living. These objectives aim to facilitate participation in educational and recreational activities, fostering social interaction and emotional well-being.[11]
Specific strategies may include:
Muscle Strength and Power: Targeted physical therapy programs designed to strengthen lower extremity muscles and posture[11]
Gait Patterns: Utilizing assistive devices and gait training techniques to enhance walking efficiency and endurance[11,12]
Functional Mobility: Practicing specific tasks such as climbing stairs, transitioning from sitting to standing, and navigating various environments.[11,12]
Non-ambulatory patients
In contrast, treatment for non-ambulatory children (GMFCS Levels IV and V) often emphasizes improving functional abilities, preventing secondary complications, and enhancing overall QoL. Goals include:
Maximizing Range of Motion: Regular stretching and passive range-of-motion exercises to prevent contractures and maintain joint health[12]
Adaptive Equipment: Implementing wheelchairs and other assistive devices that promote mobility and independence in various settings[12]
Seating and Positioning: Employing specialized seating systems to support postural alignment and comfort, reducing the risk of pressure sores[12]
Enhancing Communication and Social Skills: Engaging in therapies focusing on communication, sensory integration, and social interaction to foster emotional and psychological development.[11]
By tailoring treatment objectives to the specific needs of ambulatory and non-ambulatory patients, rehabilitation can more effectively improve functional outcomes and enhance the overall QoL for children with CP.
Comprehensive rehabilitation strategies
Rehabilitation following orthopedic interventions in pediatric CP involves several stages, each vital for optimizing functional outcomes:
Pre-orthopedic intervention rehabilitation
Preparation through prehabilitation is critical for maximizing the effectiveness of orthopedic interventions.[13] Strategies may include strengthening exercises and range-of-motion activities designed to enhance muscle function and joint mobility while empowering families to participate actively in the recovery process.[14]
Acute post-surgical management
The immediate recovery phase requires meticulous attention to pain management, wound care, and early mobilization to prevent complications.[14] Incorporating physical therapy during this phase, even at a gentle level, can facilitate healing and mitigate the risk of contractures.[14]
Sub-acute therapeutic interventions
Intensive rehabilitation is crucial during the weeks following surgery. Physical and occupational therapy focuses on restoring mobility, improving strength and flexibility, and promoting independence in activities of daily living.[15]
These interventions are tailored based on the child’s specific orthopedic challenges and overall health status.[16]
Long-term maintenance therapy
Sustaining gains achieved post-intervention is essential. Ongoing therapy sessions are critical for preventing secondary complications and addressing any residual impairments.[13] Home exercise programs further reinforce therapy goals and encourage continued progress.[16]
Use of assistive devices
Incorporating assistive devices, such as orthotics and mobility aids, plays a significant role in enhancing function and independence for children with CP.[5] These tools support safe mobility and help optimize participation in social and recreational activities.[16] By integrating these comprehensive rehabilitation strategies into the post-operative care plan, healthcare providers can optimize functional outcomes, promote independence, and improve the overall well-being of children with CP following orthopedic intervention. The inclusion of pre-orthopedic intervention rehabilitation as the initial stage underscores the importance of proactive preparation and sets the stage for successful orthopedic outcomes.[9]
Multidisciplinary and family-centered care
Effective rehabilitation post-orthopedic intervention hinges on a multidisciplinary approach that integrates various specialties.[11] A cohesive team comprising orthopedic surgeons, physical therapists, occupational therapists, and other professionals ensures a holistic evaluation and tailored treatment plan that addresses the complex needs of each child [Figure 1].[11] This collaborative model not only enhances the quality of care but also promotes better communication with families, who play a crucial role in setting realistic rehabilitation goals and expectations.[11]
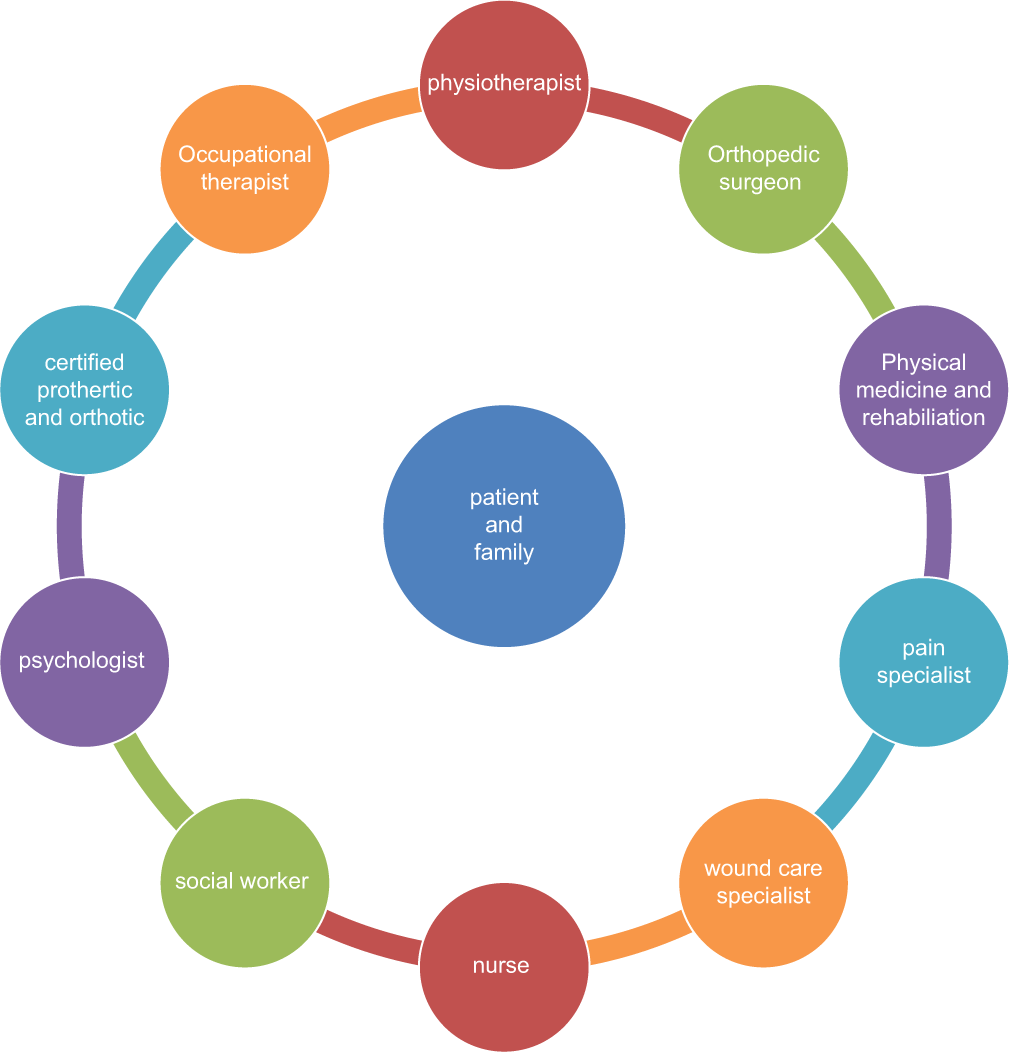
- The multidisciplinary team approach in managing pediatric orthopedic conditions associated with cerebral palsy.
Moreover, educating families about the rehabilitation process is imperative.[15,17] Providing information on therapeutic goals, proper exercise techniques, and adaptive strategies empowers families to support their child’s recovery and navigate the challenges of daily life effectively.[15,17] In addition, families are provided with resources and support to navigate the continuum of care and advocate for their child’s needs.[15,17]
Orthopedic interventions for CP
Orthopedic interventions play a critical role in managing musculoskeletal complications associated with CP. Given the complex nature of CP, which often results in muscle imbalances, joint deformities, and functional limitations, these interventions aim to improve mobility, enhance functional abilities, and promote overall QoL. The choice of orthopedic intervention is influenced by several factors, including the child’s age, the severity of CP, and specific orthopedic issues.
Types of orthopedic interventions
Soft-tissue procedures
Soft tissue interventions often involve the lengthening or releasing of tight muscles or tendons to alleviate spasticity and improve joint range of motion. Common procedures include:
Muscle Lengthening: Surgery, such as hamstring lengthening or adductor release, reduces muscle tightness and increases joint mobility.[18]
Tendon Release: Procedures aimed at releasing tension in specific tendons, such as the Achilles tendon, to facilitate more normal ankle function and prevent equinus deformities.[18]
Bone procedures
These procedures aim to correct bone structural deformities to improve alignment and function. Common bone surgeries include:
Surgical stabilization
Surgical stabilization may be necessary for children with significant deformities. Techniques such as hip stabilization surgery can help prevent or correct hip dislocation, which is a common issue in children with CP.[18]
Use of implants
In some cases, orthopedic implants, such as plates, screws, or rods, may be used to provide stability to bones post-surgery.[18,19] These implants can help maintain alignment and support healing, allowing for more effective rehabilitation.
Selectively neurolytic procedures
In certain cases, selective dorsal rhizotomy may be performed to alleviate spasticity by severing specific nerve roots in the spinal cord. While not strictly orthopedic, this procedure often works in conjunction with orthopedic interventions to enhance mobility and functional outcomes.[18]
Post-operative rehabilitation
Effective rehabilitation is essential to ensure optimal recovery and functional improvement following orthopedic surgery. Key components of post-operative rehabilitation include:
Pain Management: Effective pain control is crucial in the early postoperative period to facilitate engagement in rehabilitation activities[20]
Physical Therapy: Tailored physical therapy programs focus on restoring range of motion, strengthening muscles, and improving functional abilities. This may include exercises specific to the surgical procedure, such as gait training following lower extremity surgery[14]
Occupational Therapy: Occupational therapists work on activities of daily living, enhancing independence and functional performance[14]
Family Education and Involvement: Involving families in the rehabilitation process helps reinforce therapeutic goals and ensures that exercises and interventions are continued at home.[8,17]
Outcomes of rehabilitation strategies
Research indicates that a comprehensive, multidisciplinary approach to rehabilitation post-orthopedic intervention can lead to substantial improvements in functional abilities, mobility, and overall QoL for children with CP.[11] For example, studies have shown that early and consistent physical therapy post-surgery enhances recovery, reduces pain, and increases independence in activities of daily living.[11] Furthermore, family involvement in the rehabilitation process has been associated with better adherence to therapy regimens and improved outcomes.[11]
DISCUSSION
The results underscore the significant role of structured rehabilitation strategies in improving outcomes for children with CP post-orthopedic intervention. Early detection and intervention, particularly hip surveillance, have been shown to reduce severe complications such as hip dislocation. These findings are consistent with literature highlighting early orthopedic management’s importance in mitigating musculoskeletal challenges.
Ambulatory and non-ambulatory patients require distinct approaches, as the results confirm. Ambulatory patients benefit from muscle strengthening and gait training, while non-ambulatory patients require interventions to prevent contractures and maintain joint health. These treatment objectives align with previous studies emphasizing the need for personalized rehabilitation plans based on the patient’s functional level.
The importance of a multidisciplinary and family-centered care model is well documented in the results. A cohesive team ensures holistic treatment, while family involvement promotes adherence to therapy. These strategies have been shown to enhance functional outcomes and improve QoL, consistent with evidence from other studies on the impact of family-centered care on rehabilitation success.
The use of assistive devices plays a crucial role in improving mobility and participation in daily activities, further supporting the notion that comprehensive, individualized rehabilitation plans are essential for optimal outcomes in pediatric CP patients. Ongoing research should explore the long-term effects of these strategies and investigate emerging techniques such as robotics and virtual reality in rehabilitation settings.
CONCLUSION
The successful rehabilitation of pediatric patients following orthopedic interventions for CP requires a structured, comprehensive approach that emphasizes early detection, multidisciplinary collaboration, and active family participation. By implementing evidence-based rehabilitation strategies tailored to the individual needs of children with CP, healthcare providers can significantly enhance functional outcomes and QoL. Future research should continue to explore innovative rehabilitation techniques and their long-term impacts on mobility and overall well-being in this population.
ETHICAL APPROVAL
Institutional Review Board approval is not required.
DECLARATION OF PATIENT CONSENT
Patient’s consent not required as there are no patients in this study.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Cerebral palsy: Current opinions on definition, epidemiology, risk factors, classification and treatment options. Neuropsychiatr Dis Treat. 2020;16:1505-18.
- [CrossRef] [PubMed] [Google Scholar]
- An update on the prevalence of cerebral palsy: A systematic review and meta-analysis. Dev Med Child Neurol. 2013;55:509-19.
- [CrossRef] [PubMed] [Google Scholar]
- A report: The definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007;109:8-14.
- [Google Scholar]
- Development of the gross motor function classification system for cerebral palsy. Dev Med Child Neurol. 2008;50:249-53.
- [CrossRef] [PubMed] [Google Scholar]
- Recovery of muscle strength following multi-level orthopaedic surgery in diplegic cerebral palsy In: Miller F, Bachrach S, Lennon N, O'Neil ME, eds. Gait and posture. Netherlands: Elsevier; 2007. p. :475-81.
- [CrossRef] [PubMed] [Google Scholar]
- Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214-23.
- [CrossRef] [PubMed] [Google Scholar]
- Tachdjian's pediatric orthopaedics: From the Texas Scottish rite hospital for children Netherlands: Elsevier Health Sciences; 2015.
- [Google Scholar]
- Early, accurate diagnosis and early intervention in cerebral palsy: Advances in diagnosis and treatment. JAMA Pediatr. 2017;171:897-907.
- [CrossRef] [PubMed] [Google Scholar]
- Do not neglect the hips in cerebral palsy! J Musculoskelet Surg Res. 2023;7:223-4.
- [CrossRef] [Google Scholar]
- Multidisciplinary rehabilitation for patients with cerebral palsy: Improving long-term care. J Multidiscip Healthc. 2016;9:455-62.
- [CrossRef] [PubMed] [Google Scholar]
- The role for hip surveillance in children with cerebral palsy. Curr Rev Musculoskelet Med. 2012;5:126-34.
- [CrossRef] [PubMed] [Google Scholar]
- An interdisciplinary approach for treating children with cerebral palsy. J Interprof Pract Collab. 2019;1:1-7.
- [Google Scholar]
- Rehabilitative therapies in cerebral palsy: The good, the not as good, and the possible. J Child Neurol. 2009;24:1200-4.
- [CrossRef] [PubMed] [Google Scholar]
- Describing the delivery of evidence-based physical therapy intervention to individuals with cerebral palsy. Pediatr Phys Ther. 2021;33:65-72.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical therapy services for adults with cerebral palsy In: Miller F, Bachrach S, Lennon N, O'Neil ME, eds. Cerebral palsy. Cham: Springer; 2020.
- [CrossRef] [Google Scholar]
- A systematic review of interventions for children with cerebral palsy: State of the evidence. Dev Med Child Neurol. 2013;55:885-910.
- [CrossRef] [PubMed] [Google Scholar]
- Family-centered approach in the management of children with cerebral palsy (Serebral palsili çocuklarin tedavisinde aile odakli yaklasim) Turk Fiz Tip Rehabil Derg. 2012;58:229-35.
- [CrossRef] [Google Scholar]
- Orthopedic surgery in cerebral palsy: Instructional course lecture. Indian J Orthop. 2017;51:240-55.
- [CrossRef] [PubMed] [Google Scholar]
- The management of scoliosis in children with cerebral palsy: A review. J Spine Surg. 2016;2:299-309.
- [CrossRef] [PubMed] [Google Scholar]
- What's new in the orthopaedic treatment of cerebral palsy. J Pediatr Orthop. 2017;37:210-6.
- [CrossRef] [PubMed] [Google Scholar]






