Translate this page into:
A rare case of infective spondylodiscitis in an 18-month-old infant: Clinical presentation and management
*Corresponding author: Calogero Velluto, Department of Aging, Orthopaedic and Rheumatological Sciences, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy. calogerovelluto@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Velluto C, Inverso M, Borruto MI, Messina D, Bocchino G, Perna A, et al. A rare case of infective spondylodiscitis in an 18-month-old infant: Clinical presentation and management. J Musculoskelet Surg Res. 2024;8:160-5. doi: 10.25259/JMSR_211_2023
Abstract
Spondylodiscitis is a rare inflammatory condition predominantly observed in adults and presents unique challenges when encountered in infants. Diagnosis in this population is complicated by non-specific symptoms necessitating a high index of suspicion and comprehensive clinical evaluation. This case study reports an exceptional spondylodiscitis case in an 18-month-old infant presented with prolonged asthenia, refusal to walk, loss of appetite, and fever. Physical examination revealed general well-being, good hydration, and bilateral tonsillar hypertrophy. The pain was noted in the right hip joint and thoracolumbar spine while hip joint mobility was unrestricted. Initial investigations were conducted including blood tests, ultrasound of the right hip, and lumbosacral spine radiography, all within normal limits. Magnetic resonance imaging indicated spondylodiscitis. Empiric antibiotic therapy was administered. The fever subsided, and the patient’s condition improved leading to conservative treatment with a custom-fitted orthosis. After 15 days of hospitalization, the patient was discharged. This case report aimed to underscore the importance of early recognition and appropriate intervention as well as the need for multidisciplinary collaboration in managing pediatric spondylodiscitis.
Keywords
Discitis
Infant
Osteomyelitis
Spine infection
Spondylodiskitis
INTRODUCTION
Spondylodiscitis is a rare inflammatory condition affecting the vertebral bodies and intervertebral discs of the spine. It is predominantly observed in adults, whereas in children, the estimated incidence is 1–2 cases/year for every 32,500 pediatric hospital evaluations[1] representing approximately 3% of all the cases of osteoarticular infections.[2] However, encountering spondylodiscitis in infants remains an unusual and intricate clinical scenario. Unlike adults, no clinical evidence-based guidelines are available for managing pediatric spondylodiscitis (PSD)[3] including guidelines on the duration and choice of antibiotic therapy. This lack of guidelines often results in later developing severe complications such as spinal deformities and epidural abscesses, which affect 4–38% of PSD cases necessitating urgent surgical intervention.[4]
The diagnosis of spondylodiscitis in infants poses a significant challenge due to its infrequency and the limited ability of young children to express their symptoms effectively. In contrast to adults, who typically exhibit localized back pain and discomfort, infants often display non-specific signs including fever, irritability, and reluctance to move. This case underscores the critical importance of maintaining a high index of suspicion and conducting a comprehensive clinical evaluation when assessing pediatric patients, who present with seemingly unrelated symptoms. In this paper, we present an exceptional case of spondylodiscitis in an 18-month-old infant shedding light on its clinical presentation, diagnostic complexities, and the therapeutic strategies employed to manage this unusual pediatric condition.
This report aspires to enrich the existing literature by offering insights into the presentation, diagnostic challenges, and therapeutic considerations associated with spondylodiscitis in infants. Ultimately, comprehending the distinctive aspects of this condition in the pediatric population is paramount for optimizing clinical outcomes and safeguarding the well-being of affected infants.
CASE REPORT
An 18-month-old male patient arrived at the Emergency Care Unit of our Hospital for prolonged asthenia lasting about three days associated with refusal to walk and loss of appetite, fever for two days (maximum temperature 38.6°C), and productive cough. No trauma was reported. He was a full-term newborn delivered vaginally without the need for neonatal intensive care post-delivery. He received the three mandatory vaccinations according to Italian legislation (at 3, 5, and 11 months of age), namely, the hexavalent vaccine containing polio, diphtheria, pertussis, Haemophilus influenzae type B, and hepatitis B antigens. Both the mother and father were in excellent health and had no known hereditary diseases. The child’s development followed physiological percentiles, and there were no reported health issues before the following situation.
Physical examination showed good general clinical conditions. The skin and mucous membranes showed good hydration status. The temperature was 38.6°C with no meningeal signs.
He presented with bilateral tonsillar hypertrophy and intense hyperemia without exudate. The otoscopy was negative. The chest, cardiac, and abdominal examinations were within normal limits. There was no restriction of both hip joint movements. There was no swelling or pain in the knees, ankles, wrists or elbows. However, apparent pain was observed in the right hip joint area when sitting or standing with a load-bearing component. In addition, the pain was elicited on palpation and during flexion movements of the thoracolumbar spine. No inguinal lymphadenopathy was present.
The patient presented with age-appropriate behavior exploring the environment with curiosity. The posture was symmetrical, and there were no noticeable abnormalities in movements. Muscle tone was within normal limits, and there was a smooth transition during passive movements of the lower limbs. The patient exhibited appropriate resistance during range of motion testing. The patellar reflex was present and symmetrical. Achilles reflex response was observed bilaterally and was within normal limits. Furthermore, the Babinski reflex was normal: The toes exhibited a normal flexor response when the sole was stroked.
Furthermore, the patient reacted appropriately to a gentle touch on the lower limbs showing no signs of hypersensitivity or numbness. No signs of musculoskeletal abnormalities were observed, and joint movements appeared normal. Gait was steady with a normal walking pattern for their age.
At the beginning, complete blood examinations were performed including arterial blood gas with normal results for age: pH 7.38, K+ 3.8 mmol/L, Na+ 133 mmol/L, Ca++ 5.06 mg/dL, Cl− 99 mmol/L, glucose 84 mg/dL, lactates 1.6 mmol/L, EB −5.6 mmol/L, HCO3 −19.9 mmol/L. Complete blood count was performed within normal limits for age (WB 12.96 × 109/L, Neu 7.75 × 109/L) except for mild thrombocythemia (559 × 109/L). Hematochemical tests were also performed within normal limits.
The C-reactive protein (CRP) levels were slightly elevated measuring 5.3 mg/dL. A procalcitonin blood test was also performed, and the value was negative (<0.03 mg/dL). Ultrasound examination of the right hip revealed no signs of inflammation. The appearance was symmetrical compared to the contralateral hip. There was also no soft-tissue collection in the local or regional area. Radiography of the lumbosacral spine was normal as shown in Figure 1.

- Lateral plain radiographs show no structural alterations of the spine.
Ear examination was normal, and the nasopharyngeal swab test for respiratory viruses yielded negative results. Finally, two sets of blood cultures were performed, and the results were also negative. Subsequently, he was admitted to the pediatric ward for treatment and necessary investigations.
Clinical progression
Due to apparent back pain, a spinal surgery consultation was requested for the patient, according to which magnetic resonance imaging (MRI) of the lumbosacral spine was prescribed. The MRI revealed disc edema and the upper L1 and lower T12 vertebral body consistent with spondylodiscitis [Figure 2]. A complete set of lateral and anterior-posterior plain spine radiographs was also performed, which showed the absence of any apparent structural modifications within the spinal column [Figure 1].
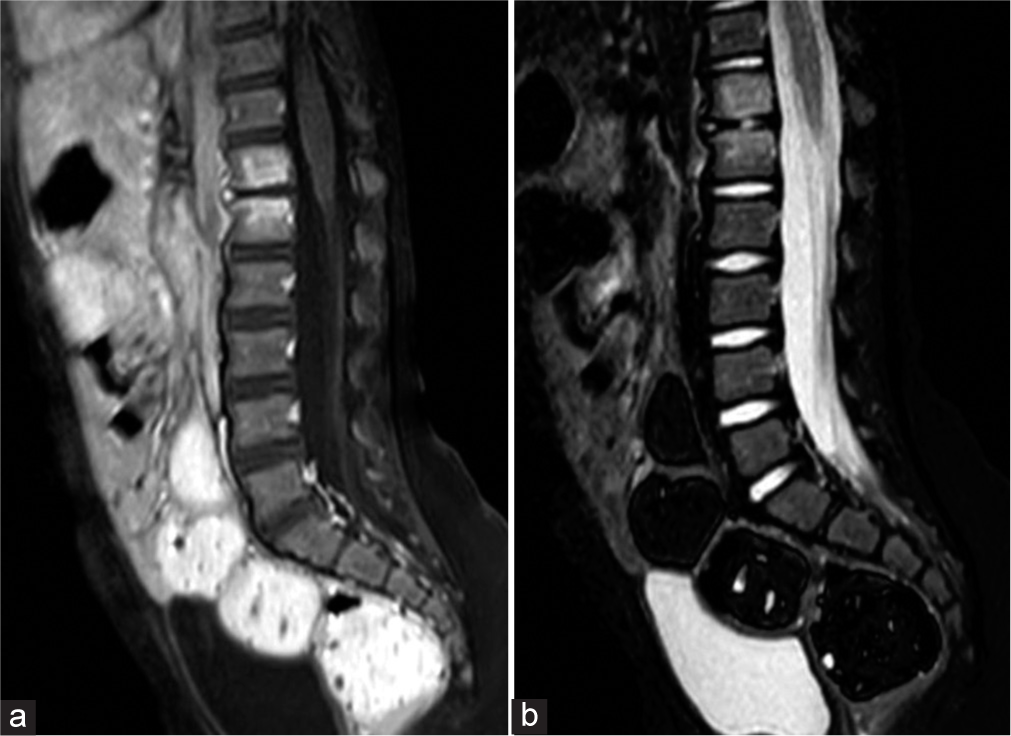
- (a) Sagittal T1- and (b) T2-weighted magnetic resonance images of the lumbar spine demonstrate T1 hypointensity and T2 hyperintensity centered around the T12–L1 disc space consistent with bone marrow edema and intervertebral disc space fluid.
According to the infection disease specialist, empiric oral antibiotic therapy with amoxicillin-clavulanic acid was administered for five days and changed to ceftriaxone intravenous (IV) for 10 days. After 10 days of antibiotic therapy, the values of CPR decreased to <2.0 mg/dL.
Considering the suspected spondylodiscitis outbreak, maintaining IV antibiotic therapy was deemed essential. Consequently, a central line was inserted under sedation in the pediatric intensive care unit.
During his hospital stay, his condition and clinical examinations progressively improved. The patient presented several fever peaks (maximum temperature reached 39°C). Considering the patient’s stable radiographic findings and improved condition, a fully conservative treatment approach was chosen to prevent possible neurological deficits and their subsequent serious consequences. This approach entailed prescribing and custom-fitted orthosis. Given the patient’s young age, this approach was deemed the most convenient and practical for daily pediatric care. Surgical intervention was not deemed necessary, as there was no evidence of significant spinal cord compression or neurological deficits. Following a 10-day course of antibiotic therapy, during which the CPR values showed a decline, the infectious disease specialist advised the patient to continue the antibiotic treatment for an additional seven days. Subsequently, the antibiotic therapy was suspended, and the patient proceeded solely with conservative treatment using a brace.
Considering his clinical improvements and the results of the diagnostic tests, the decision was made to discharge the patient after a 15-day hospitalization.
The patient underwent close monitoring with frequent follow-ups, and after 1 month, an MRI was repeated. The new examination showed the presence of edema at the T12–L1 level with no evidence of paraspinal abscesses or spinal cord compressions and no increase in thoracolumbar junction kyphosis or any other morphostructural changes [Figure 3]. Therefore, conservative bracing treatment was continued for a total of three months.
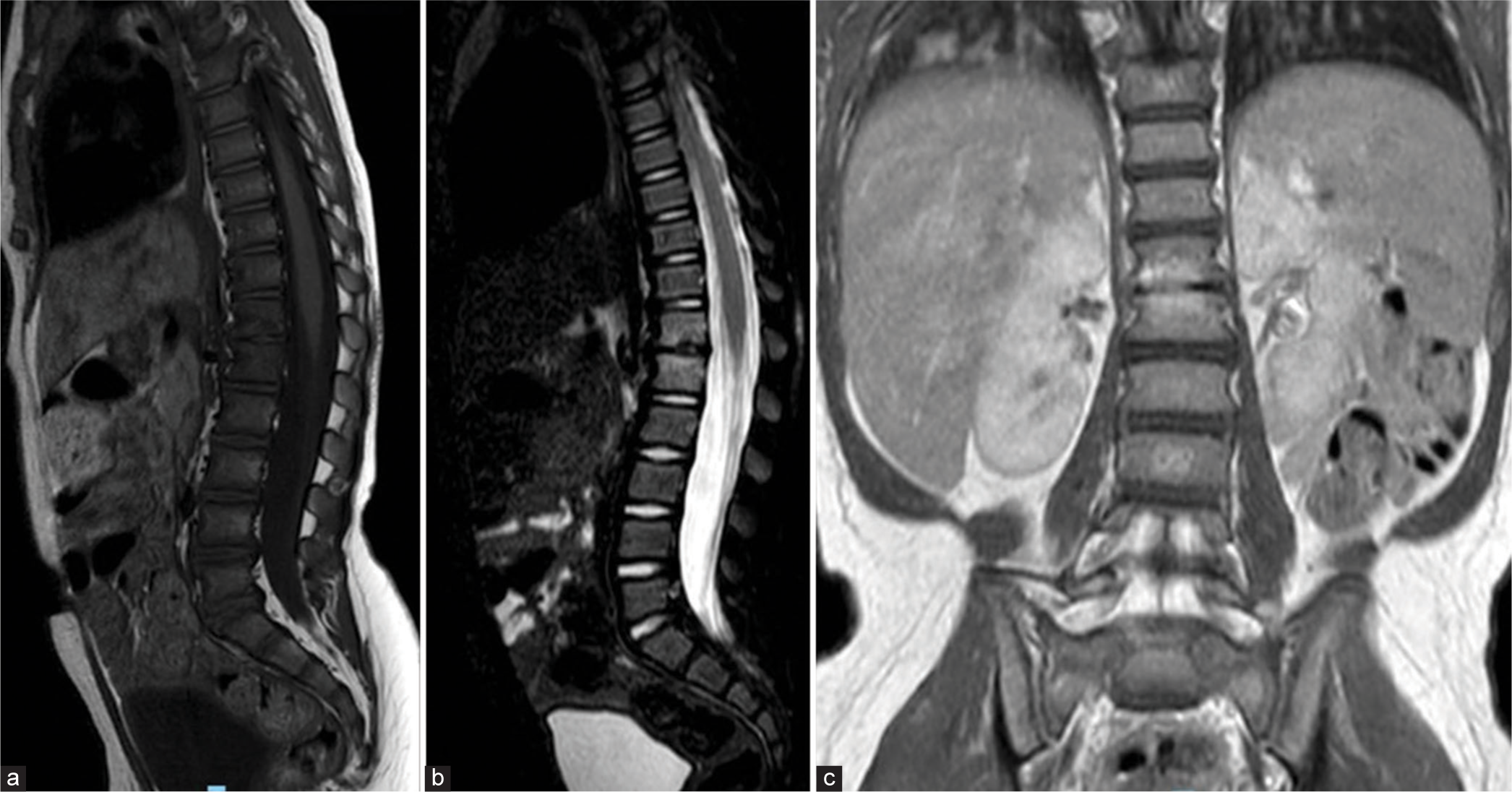
- One-month follow-up sagittal (a) T1, (b) T2-weighted, and (c) coronal T1-weighted magnetic resonance images of the lumbar spine reveal hyperintensity centered around the T12–L1 disc space consistent with bone marrow edema and no evidence of paraspinal abscesses, spinal cord compressions or increase in thoracolumbar junction kyphosis.
DISCUSSION
The etiology of spondylodiscitis in infants remains poorly understood with congenital, hematogenous, and post-infectious pathways, all considered potential causative factors.[5] Gaining insight into the underlying mechanisms responsible for spondylodiscitis in this age group is imperative for enhancing diagnostic accuracy and tailoring effective treatment strategies. The age distribution of PSD follows a triphasic pattern: the first peak occurs in early childhood (79%), between the ages of six months and four years; a smaller peak emerges in the juvenile and adolescent group (20%); and exceptional infections are observed in children aged under six months (1%).[6]
The limited utility of traditional imaging modalities such as plain radiographs further complicates the diagnostic process in infants. An MRI has emerged as the gold standard for diagnosis offering unparalleled sensitivity in detecting early vertebral and disc involvement.[7] Furthermore, MRI is crucial for the differential diagnosis of rare vertebral tumors that may also occur in infants.[8] Our case report underscores the pivotal role of MRI in achieving precise and timely diagnoses of spondylodiscitis in pediatric patients.
Staphylococcus aureus is the leading cause of the etiology accounting for approximately 80–90% of cases.[9] Other less frequently identified agents include coagulase-negative Staphylococcus, a-hemolytic Streptococcus, Streptococcus pneumoniae, Escherichia coli, and Salmonella spp. Literature reports other rare bacterial pathogens such as Kingella kingae, group B streptococci, Listeria species, H. influenzae, Neisseria meningitidis, and Brucella species. [6]
Tuberculosis (TB) is reported as latent TB in infants.[10] The incidence of spinal TB in children varies. It is reported as 58% of all spine TB cases in Korea, 1/3rd of all patients as reported from Chennai, India, and 26% in Hong Kong.[11] This condition leads to severe bone loss and growth impairment; therefore, the sequelae are serious. The vertebral bodies in children are cartilaginous. Consequently, when a tubercular infection affects the vertebral bodies, cartilage loss occurs rapidly leading to severe deformities within a short period compared to adults. In most patients, pathogens reach the spine through the hematogenous route initially affecting the intervertebral disc and subsequently involving the adjacent vertebral endplates through blood supply vessels that typically persist until the seventh year of life.[12]
Furthermore, as reported in a recent systematic review of the literature on spondylodiscitis in infants by Lashkarbolouk et al.,[13] discitis in children is typically benign in contrast to adults due to a better blood supply, and it should recover without complications. Nevertheless, a delay in diagnosis can lead to persistent unpleasant side effects, drug resistance, and invasive treatments such as surgery in patients. According to Lashkarbolouk et al.,[13] surgery was performed only in five studies due to clinical indications. In all the other studies, early antibiotic therapy was initiated followed by immobilization contributing to a better clinical outcome.
Moreover, in our case, the patient’s clinical condition spontaneously resolved with antibiotic therapy and conservative treatment, even though we could not identify the causative agent. In fact, CRP values normalized with antibiotic therapy decreasing from the initial 5.3 mg/dL to <2 mg/dL after 10 days of IV antibiotic therapy. Nevertheless, this highlights the importance of a multidisciplinary approach in managing spondylodiscitis in infants, with antibiotic therapy as the foundation. The selection of antibiotics, treatment duration, and the potential necessity for surgical intervention all depend on the clinical severity and the causative microorganism highlighting the need for tailored care plans for each patient. Surgical treatment is generally reserved for patients with severe neurological symptoms and deficits that could compromise the clinical outcome in terms of development. However, evidence supports the efficacy of non-operative treatments such as orthotic bracing in managing this condition in infants.[14] In the case of our 18-month-old patient, implementing a custom-fitted orthosis played a crucial role in managing the condition. This conservative approach allowed spinal stabilization and pain relief and facilitated natural healing. The patient’s improved clinical progression and the absence of significant spinal cord compression or neurological deficits reinforced the viability of this non-surgical approach.
During antibiotic therapy, the use of cast braces helps prevent back pain, vertebral collapse, and associated neurological complications. In addition, it mitigates the risk of secondary spinal deformities while facilitating patient mobility as reported by Romano et al.[15] In cases of acute neurological impairment or severe kyphosis, it is crucial to perform open spinal decompression and stabilization as soon as possible.[15] Surgical treatment for PSD is often similar to congenital forms in terms of the type of deformity, radiological aspect, and indications for treatment with all the risks concerning a surgical approach in young patients.[16]
One of the key takeaways from our study is the importance of early intervention and multidisciplinary collaboration in managing PSD. Early recognition of the symptoms enabled by a high index of suspicion is paramount. When non-specific symptoms such as fever, irritability, and reluctance to move are observed in infants, and there is no evidence of other possible causes, healthcare providers should consider spondylodiscitis in their differential diagnosis.
While our current case provides valuable insights into the non-operative treatment of PSD with orthotic bracing, it is essential to acknowledge its limitations. This is a single case report, and while it demonstrates positive outcomes, a larger sample size is necessary to draw more robust conclusions about the effectiveness of the conservative approach presented in the case. Moreover, the study was unable to identify the causative agent of spondylodiscitis. Understanding the specific pathogen responsible for the infection is crucial for tailoring treatment strategies and improving diagnostic accuracy. However, this case underscores the importance of meticulous clinical evaluation encompassing comprehensive medical history and physical examination when rare conditions are suspected. Timely and precise diagnosis, in fact, facilitated by advanced imaging techniques and microbiological analyses, is fundamental for identifying the causative pathogen and customizing the treatment protocol. The successful outcome of this case achieved through a combination of appropriate antimicrobial therapy without surgical intervention underscores the necessity of a personalized treatment plan for each patient considering the severity of the infection, the age of the patient, and the potential for complications as severe kyphosis with consequent neurological deficits as reported by Romano et al.[15] Furthermore, it emphasizes the importance of vigilant long-term follow-up to monitor disease recurrence and assess the child’s neurodevelopmental progress.
CONCLUSION
The successful diagnosis and treatment in this 18-month-old case underscore the importance of a multidisciplinary approach. Collaboration among pediatricians, orthopedic surgeons, radiologists, and infectious disease specialists plays a pivotal role in achieving optimal outcomes. Conservative treatment involving custom-made orthoses and antibiotic therapy is a valid option in patients without neurological deficits.
RECOMMENDATIONS
Continued research and collaborative efforts within the medical community are essential to further enhance our understanding of the pathogenesis, diagnostic strategies, and treatment approaches for spondylodiscitis in the pediatric population, ultimately improving the outcomes and quality of life for affected children.
AUTHORS’ CONTRIBUTIONS
LP and CV conceived and designed the study. CV and MI wrote the original draft. MIB, DM, and GB: edited the final draft. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
ETHICAL APPROVAL
No ethical approval was required for the publication of this case report.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient’s parents have given their consent for the patient’s images and other clinical information to be reported in the journal. The parents understand that the patient’s name and initials will not be published, and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Prospective survey of acute osteoarticular infections in a French paediatric orthopedic surgery unit. Clin Microbiol Infect. 2013;19:822-8.
- [CrossRef] [PubMed] [Google Scholar]
- 2015 Infectious Diseases Society of America (IDSA) clinical practice guidelines for the diagnosis and treatment of native vertebral osteomyelitis in adults. Clin Infect Dis. 2015;61:e26-46.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical Practice Guideline by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America: 2021 guideline on diagnosis and management of acute hematogenous osteomyelitis in pediatrics. J Pediatric Infect Dis Soc. 2021;10:801-44.
- [CrossRef] [PubMed] [Google Scholar]
- Spinal infections in children: A multicentre retrospective study. Bone Joint J. 2018;100:542-8.
- [CrossRef] [PubMed] [Google Scholar]
- Hematogenous pyogenic spinal infections and their surgical management. Spine (Phila Pa 1976). 2000;25:1668-79.
- [CrossRef] [PubMed] [Google Scholar]
- Infectious discitis and spondylodiscitis in children. Int J Mol Sci. 2016;17:539.
- [CrossRef] [PubMed] [Google Scholar]
- Pott disease in a 13monthold: Case report. Neurosurgery. 2011;68:E148590.
- [CrossRef] [PubMed] [Google Scholar]
- Tubercular spondylitis in children. Indian J Orthop. 2014;48:136-44.
- [CrossRef] [PubMed] [Google Scholar]
- Characteristics, management and outcomes of spondylodiscitis in children: A systematic review. Antibiotics (Basel). 2021;10:30.
- [CrossRef] [PubMed] [Google Scholar]
- Understanding the management of pediatric spondylodiscitis based on existing literature; A systematic review. BMC Pediatr. 2023;23:578.
- [CrossRef] [PubMed] [Google Scholar]
- Spondylodiscitis in children: A retrospective study and comparison with non-vertebral osteomyelitis. Front Pediatr. 2021;9:727031.
- [CrossRef] [PubMed] [Google Scholar]
- Infectious spondylodiscitis and kyphosis correction in an infant: A case report. Ital J Pediatr. 2021;47:152.
- [CrossRef] [PubMed] [Google Scholar]
- The surgical management of congenital kyphosis and kyphoscoliosis. Spine (Phila Pa 1976). 2001;26:2146-54. discussion 2155
- [CrossRef] [PubMed] [Google Scholar]







