Translate this page into:
Advancements in vacuum therapy for musculoskeletal wound care: A comprehensive analysis of chronic wounds and acute injuries
*Corresponding author: Nahla A. Tayyib, PhD, Department of Clinical Nursing, Faculty of Nursing, Umm Al-Qura University, Makkah, Saudi Arabia. natayyib@uqu.edu.sa
-
Received: ,
Accepted: ,
How to cite this article: Tayyib NA. Advancements in vacuum therapy for musculoskeletal wound care: A comprehensive analysis of chronic wounds and acute injuries. J Musculoskelet Surg Res. 2024;8:108-18. doi: 10.25259/JMSR_253_2023
Abstract
Musculoskeletal wounds are challenging to treat. Vacuum therapy (VT), based on the principle of applying negative pressure to a wound, has gained popularity as an adjunctive treatment modality for musculoskeletal wounds. Clinical studies have shown that VT improves wound bed preparation, reduces wound size, accelerates healing rates, and decreases time to wound closure. It is also associated with a lower risk of wound complications, such as infection, dehiscence, and seroma formation. The integration of VT into a comprehensive wound management approach has the potential to improve outcomes for patients with musculoskeletal wounds. This review provides a comprehensive overview of VT for musculoskeletal wound care. The review discusses the current practices, mechanism of action, benefits, risks, and future directions of VT. The review concludes that VT is a valuable tool for the treatment of musculoskeletal wounds, and that it is safe and effective for most patients.
Keywords
Musculoskeletal wounds
Negative pressure wound therapy
Vacuum therapy
Vacuum-assisted closure
Wound healing
Wound management
Wound care
INTRODUCTION
Effective treatment of musculoskeletal wounds requires a comprehensive approach that addresses the underlying cause of the wound, promotes healing, and manages pain and inflammation. This approach often involves a combination of wound dressings, negative pressure wound therapy (NPWT), debridement, and antibiotic therapy. Surgical interventions may sometimes be necessary to restore function and prevent complications. Musculoskeletal wounds, including pressure ulcers, diabetic foot ulcers, traumatic injuries, and surgical wounds, pose significant clinical challenges in terms of healing and functional recovery.[1] Traditional wound care methods often face limitations in promoting wound closure and preventing infection in these complex wounds. Vacuum therapy (VT), also known as NPWT, has emerged as a promising modality in the field of wound care based on the principle of applying negative pressure to a wound.[2,3]
The VT includes using a customized dressing and a vacuum source to apply regulated sub-atmospheric pressure to a wound bed. Through several processes, including improved tissue perfusion, elimination of extra exudate, decrease of edema, promotion of granulation tissue development, and control of inflammatory responses, it generates a milieu that supports wound healing. Studies have examined the use of VT in treating musculoskeletal wounds, emphasizing its beneficial effects on wound healing and functional recovery.[4,5]
Accelerated wound healing, lower infection rates, enhanced granulation tissue production, and a need for fewer surgical interventions have all been observed in clinical trials and case studies.[6] By encouraging early wound bed preparation, minimizing bacterial colonization, and promoting healthy tissue regeneration, VT has also been proven beneficial in treating complicated wounds, such as open fractures and pressure ulcers. However, several factors must be considered, including suitable patient selection, wound cleaning, and application methods.[5,7]
Technological developments and the creation of new VT systems have the potential to significantly improve the efficiency and usefulness of the treatment.[8] In a nutshell, VT has proven to be a useful adjunct in managing musculoskeletal wounds. However, more research is required to develop standardized protocols, assess long-term results, and hone the indications and contraindications for VT in treating musculoskeletal wounds.
This review focuses on the application of VT in musculoskeletal wound care, delving into its current applications, the mechanisms behind its effectiveness, its potential benefits and risks, and futuristic points for future research. It aimed to achieve three key objectives: First, to evaluate VT’s effectiveness in promoting healing for musculoskeletal wounds; second, to analyze existing evidence and established clinical guidelines surrounding its use in this context; and third, to pinpoint areas where further investigation and potential advancements can optimize VT for musculoskeletal wound management. This review aimed to provide a comprehensive and insightful picture of VT’s current and future role in treating musculoskeletal wounds by accomplishing these objectives.
MATERIALS AND METHODS
A comprehensive literature search was conducted in the relevant databases as shown in Figure 1, such as PubMed, Scopus, and Google Scholar, to identify relevant articles using appropriate keywords, such as VT, musculoskeletal wound, wound management, NPWT, chronic wounds, acute injuries, and related terms.[9] A search strategy was developed to identify relevant literature, including databases, conference proceedings, expert opinions, and gray literature sources. Inclusion and exclusion criteria were defined for selecting studies, such as focusing on applying VT in musculoskeletal wound care/management published in the past five years and written in English. Study selection was reviewed to select studies that meet the inclusion and exclusion criteria. The entire literature search, data extraction, critical appraisal, and data synthesis process were performed. The rigorous approach included a thorough literature search, data collection, and removal of duplicate research papers to ensure that the review incorporated only the most relevant and up-to-date evidence on the effectiveness of VT in musculoskeletal wound care. The conclusion was drafted, incorporating my insights and providing recommendations for future research and practice.
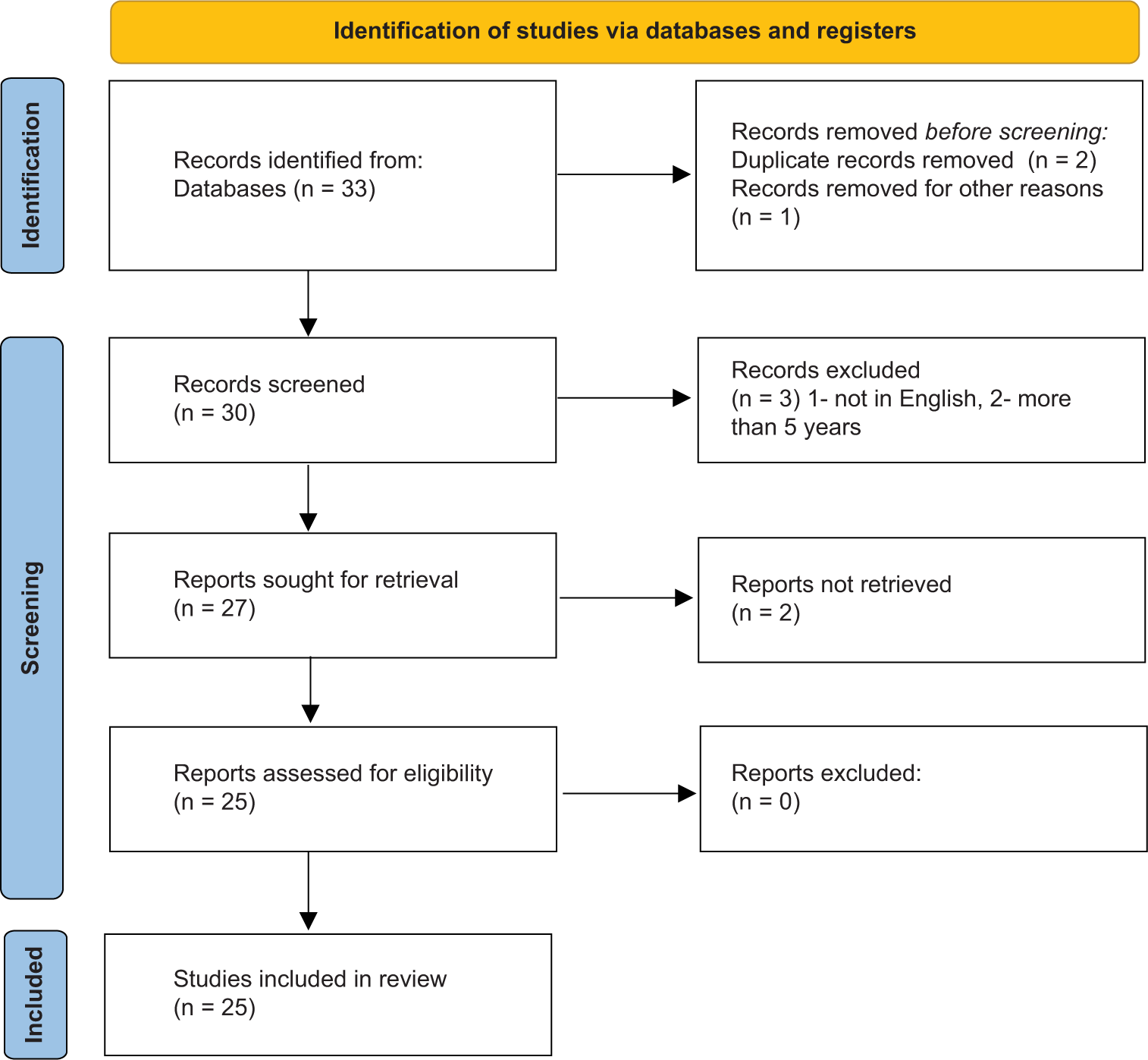
- The PRISMA flowchart.
The important research studies on NPWT are summarized in Table 1. It shows mixed results on benefits such as infection rate, healing time, and hospital stay.
| S. No. | Type of the Paper | Title | Authors | Publication Year | Number of patients included | Demographics | Result |
|---|---|---|---|---|---|---|---|
| 1. | Research Paper | VAC therapy versus standard wound therapy for open musculoskeletal injuries | Sinha et al.[10] |
2013 | 30 | Mean age: 39 years old (range 18–76); open musculoskeletal injuries of upper and lower limbs |
Size of soft-tissue defects reduced more than 5 mm to 25 mm after VAC therapy |
| 2. | Research Paper | Negative-pressure wound therapy versus standard dressings for adults with an open lower limb fracture: the WOLLF RCT | Costa et al.[16] |
2018 | 460 | Adults (≥16 years old) with severe open fracture of the lower limb | No evidence of a difference in the patients’ DRI at 12 months. There was no difference in HRQoL and no difference in the number of surgical site infections or other complications at any point in the 12 months after surgery. NPWT did not reduce the cost of treatment. |
| 3. | Research Paper | A randomized controlled trial to assess the cost-effectiveness of a novel, simple modification to the NPWT system. | Albayati et al.[24] |
2021 | Not mentioned | Patients with acute or chronic wounds requiring surgery | Modified VAC system with reusable canister reduced consumable cost compared to standard system, while maintaining effectiveness. |
| 4. | Research Paper | Effect of electrical stimulation on blood flow velocity and vessel size. | Jin et al.[28] |
2017 | 45 | Healthy adult males and females | Electrical stimulation altered blood flow velocity and vessel size. Changes were significant immediately and 30 min after stimulation |
| 5. | Meta- analysis | NPWT in patients with wounds healing by secondary intention: A systematic review and meta-analysis of randomized controlled trials. | Zens et al.[14] |
2020 | 4315 (Evaluable)/Potentially 5701 (Total) | Patients with wounds healing by secondary intention | Low-quality evidence suggests NPWT improves wound closure and shortens hospital stay compared to standard wound therapy. No impact on mortality or adverse events found. |
| 6. | Meta- analysis | NPWT versus conventional wound dressings in treatment of open fractures: A systematic review and meta-analysis. | Liu et al.[15] | 2018 | 909 (421 RCT, 488 retrospective) | Open fracture patients | NPWT reduced infection rate, shortened healing time and hospital stay, and lowered amputation rate. No significant difference in flap surgery or fracture non-union rate. |
VAC: Vacuum assisted closure, RCT: Randomized clinical trial, NPWT: Negative pressure wound therapy, DRI: Disability rating index, HRQoL: Health-related quality of life.
MUSCULOSKELETAL WOUNDS AND CHALLENGES
Fractures, deep lacerations, crush injuries, open fractures, and post-surgical wounds are just a few of the many types of injuries that can be classified as musculoskeletal wounds. These wounds are difficult to heal because they frequently include complicated tissue damage, a weakened blood supply, and possible infection.[10] Controlling infections, maintaining soft tissue and bone viability, preventing non-union or delayed union of fractures, and optimizing functional results are critical concerns in caring for musculoskeletal wounds. The selection of a management method is influenced by several variables, including the size, depth, location, amount of contamination, and patient characteristics.
TRADITIONAL WOUND MANAGEMENT APPROACHES
Traditional wound care methods, including wound debridement, irrigation, dressings, and surgical procedures like primary closure or skin grafting, were historically used to treat musculoskeletal wounds. These methods remain vital, but they might not always be sufficient to handle the unique problems that musculoskeletal wounds present. Musculoskeletal tissues, especially bone, have a restricted ability to recover due to things such as low vascularity, mechanical instability, and microbial colonization.[10]
VT IN WOUND CARE
The VT, also known as negative pressure wound therapy (NPWT), has drawn more attention recently as a viable supplementary treatment option for musculoskeletal wounds. This non-invasive approach promotes wound healing through several processes by applying regulated negative pressure to the wound bed. The VT aids in removing extra wound fluid, lowering edema, improving local blood flow, triggering the creation of granulation tissue, and promoting wound contraction. In addition, it can make it easier to remove infectious materials and encourage the creation of a friendlier wound environment.[11]
POTENTIAL APPLICATIONS OF VT IN MUSCULOSKELETAL WOUND CARE
Using VT in treating musculoskeletal wounds has yielded encouraging results in various therapeutic settings. The VT for open fractures can aid in fracture stability, control soft-tissue injury, and lessen bacterial burden. The VT has been shown to be effective in improving wound healing and minimizing complications in chronic wounds linked to ailments such as diabetic foot ulcers or pressure injuries. The VT may also be used to treat post-operative wounds, helping to prepare the wound bed better and promote tissue regeneration.[12]
MECHANISM OF VT
By increasing blood flow, lowering edema, eliminating excess exudate, encouraging the creation of granulation tissue, assisting wound contraction, and stimulating cellular activity, VT generates an environment that favors wound healing. It has been shown to be a successful method of treating musculoskeletal wounds, promoting faster healing and better patient results.[12]
The following are some of the parts of a typical VT system:
Wound dressing: The wound site is covered with a specific covering. The dressing is made of porous foam or gauze that has been custom-cut to match the size of the wound. The wound and the vacuum source are connected with this dressing. Transparent film: To establish a sealed environment, a transparent film is applied over the wound dressing. The negative pressure is maintained because the film is impermeable to air and liquids.
Tubing: A tube is attached to the sealed dressing to establish a vacuum. The tube’s opposite end is attached to a vacuum pump or a device used specifically for VT. Vacuum pump or unit: This part produces the therapeutically necessary negative pressure. Depending on the application, it can be a bigger vacuum machine or a compact battery-powered device.[13]
The following are the theories put up as to how VT improves the healing of musculoskeletal wounds.[6,7] Increased blood flow: Applying negative pressure to a wound causes vasodilation, which boosts blood flow there. Increased blood flow helps the wound heal by supplying it with nutrients and oxygen. In addition, it aids in the removal of waste and pollutants, lowering the chance of illness. Edema is lessened due to negative pressure, which helps drain extra fluid from the wound and surrounding tissues. Edema, or swelling, can obstruct the passage of nutrients and oxygen, which can slow the healing process. The VT encourages a more ideal environment for wound healing by minimizing edema. Elimination of extra exudate: Exudate, a surplus of fluid produced by wounds, can hinder healing and raise infection risks. The continual suction produced by VT helps eliminate this extra exudate, allowing the wound healing process. Promotion of granulation tissue formation: Granulation tissue is a crucial component of the healing process and is stimulated by negative pressure. The granulation tissue that covers the wound bed comprises new blood vessels, collagen, and connective tissue. It offers a support structure for further tissue regeneration and wound healing.
Wound contraction: The VT, especially for bigger wounds, can help in wound contraction. The negative pressure applied to the margins of the wound forces them together, making the wound smaller and speeding up healing. Cellular activity stimulation: The mechanical forces that negative pressure exerts on the wound bed’s cells can cause cellular reactions that encourage tissue development and healing. This entails stimulating endothelial cells, which aid in forming new blood vessels and the activation of fibroblasts, which are in charge of creating collagen.
EVIDENCE FOR VT IN MUSCULOSKELETAL WOUND CARE
The evidence of VT in musculoskeletal wound care is shown in Table 2. Several clinical studies and trials have been conducted to evaluate the effectiveness of VT in musculoskeletal wound management.[14-18] Here is a review of the evidence regarding its benefits and limitations:
| S. No. | Characteristics | Description with references |
|---|---|---|
| 1. | Wound closure rates | Numerous studies have reported improved wound closure rates with the use of VT. For example, a systematic review published by Zens et al.[14] found that NPWT significantly increased the rate of wound closure in musculoskeletal wounds compared to traditional dressings. The review included studies involving open fractures, pressure ulcers, and soft-tissue defects. |
| 2. | Reduction in wound size | VT has been shown to reduce wound size in musculoskeletal wounds effectively. Liu et al.[15] examined the use of NPWT in the treatment of complex open fractures. The authors found that NPWT resulted in a significant reduction in wound size compared to standard wound dressings. |
| 3. | Time to healing | VT has demonstrated the potential to accelerate wound healing in musculoskeletal injuries. A randomized controlled trial by Costa et al.[16] compared NPWT to standard dressings in the management of open tibia fractures. The study reported a significantly shorter time to wound healing in the NPWT group compared to the standard dressing group. |
| 4. | Advantages | VT has several benefits for the treatment of musculoskeletal wounds. It offers a beneficial moist wound environment that is for the best possible wound healing.[5] The wound is helped to heal by the negative pressure, which also encourages the growth of granulation tissue. In addition, NPWT makes it easier to get rid of extra fluid, which lessens edema and enhances local blood flow. According to certain theories, VT may also have antimicrobial benefits by lowering bacterial colonization in the wound bed.[17] |
| 5. | Limitations | VT has been effective in treating musculoskeletal wounds, but it is not without restrictions. Specialized equipment is necessary for the therapy, but it can be expensive and not always easily available in healthcare facilities. Applying NPWT might take some time, and it needs frequent dressing changes. In other circumstances, such as those involving wounds with exposed blood arteries or organs or when an infection is active, the use of VT may also be inappropriate.[6,18] |
VT: Vacuum therapy, NPWT: Negative pressure wound therapy
APPLICATIONS OF VT IN MUSCULOSKELETAL WOUND CARE
These are some specific forms of musculoskeletal wounds that VT may treat, as well as how it can solve certain problems with musculoskeletal wound care:
Pressure ulcers
Pressure ulcers, sometimes referred to as bedsores, are a serious problem for those with restricted movement. Due to persistent pressure, these lesions frequently develop over bony prominences and can be challenging to treat. The VT can be beneficial by encouraging the growth of granulation tissue, eliminating extra fluid, and lowering edema. In addition, it aids in bacterial load reduction and offers a moist environment for wound healing, which promotes wound closure.[16]
Diabetic foot ulcers
Diabetes frequently results in diabetic foot ulcers, which can be particularly difficult to treat due to compromised wound healing mechanisms. By encouraging angiogenesis, eliminating excessive exudate, and assisting the development of healthy granulation tissue, VT can address the particular difficulties associated with diabetic foot ulcers. In addition, the negative pressure aids in increasing wound contraction, enhancing local blood flow, and minimizing edema.[2]
Surgical wounds
Musculoskeletal surgical wounds can be intricate and present particular wound management issues. These wounds can get VT to lessen post-operative problems, including infection, seroma, and hematoma development. Controlled negative pressure aids in dilating the blood vessels in the wound bed, eliminating extra fluid, and encouraging healthy tissue growth. In addition, it can aid in encouraging primary or secondary wound closure and lowering the risk of wound dehiscence.[14]
CHALLENGES UNIQUE TO MUSCULOSKELETAL WOUND CARE
Wound depth
Musculoskeletal wounds that include deeper tissues, including pressure ulcers or surgical wounds, may necessitate specialized care techniques. By encouraging wound contraction, granulation tissue creation, and increasing angiogenesis, which are essential for healing deep wounds, VT can assist in overcoming these difficulties.[19-21]
Anatomical constraints
Musculoskeletal wounds can develop in regions with complicated anatomical features, challenging applying conventional bandages or keeping ideal wound conditions. The VT offers a remedy using specifically created wound dressings and vacuum-assisted devices that may adapt to different anatomical locations and administer negative pressure directly to the wound bed.[21]
Complicated wound etiology
Complex etiologies, such as the interaction of pressure, ischemia, and infection, are frequently present in musculoskeletal wounds. By lowering bacterial loads, increasing tissue perfusion, and allowing the drainage of surplus wound fluid, which may include inflammatory mediators, VT aids in addressing these multifactorial wound etiologies.[19]
OPTIMAL IMPLEMENTATION OF VT IN MUSCULOSKELETAL WOUND CARE
When choosing patients and wounds, administering the therapy, and handling any consequences, several factors must be considered to conduct VT as effectively as possible.[22]
Patient and wound selection
Patient factors: The VT is inappropriate for many individuals or wound types. The patient’s general health, capacity to adhere to therapeutic requirements, and tolerance of negative pressure are all things to be considered. Patients with uncontrolled bleeding problems or a weakened blood supply to the wound region may not be candidates for VT.
Wound characteristics
Wounds with extensive exudate, deep cavities, undermining, or exposed bone benefit most from VT. It may be used on several musculoskeletal wounds, including osteomyelitis, pressure ulcers, diabetic foot ulcers, surgical wounds, and wounds from trauma. To decide whether VT is the best option, a thorough wound examination is essential.
VT Application
Wound preparation: The wound should be carefully cleaned and debrided before beginning VT to remove necrotic tissue, foreign objects, and excessive exudate. Better wound healing results are encouraged by proper wound bed preparation.
Dressing selection
Various dressings, including foam dressings, gauze dressings, and specialist dressings with antimicrobial qualities, are available for VT. The parameters of the wound, such as depth and exudate level, affect the dressing choice. Foam dressings are frequently used because they can adapt to unusual wound forms and encourage the growth of granulation tissue.
Negative pressure settings
The amount of negative pressure used should be determined by the demands of the particular patient and the wound. The recommended range is typically between −75 mmHg and −125 mmHg.[6] Depending on the needs of the wound and the patient’s comfort, the therapy might be continuous or intermittent.
MONITORING AND MANAGEMENT
Regular dressing changes
The dressings should be changed regularly, which can range from daily to every few days, depending on the exudate level of the wound. The wound should be re-evaluated for indications of infection, complications or indicators of healing progress during dressing changes.[23]
Infection prevention
The VT can aid in the reduction of bacterial loads in wounds, but it should not be used in place of proper wound infection care. It is important to take preventative steps, such as using an aseptic technique when changing dressings, giving antibiotics as needed, and closely watching for infection symptoms.
Complications of treatment and their prevention
The VT has several potential side effects, including bleeding, discomfort, tissue damage, infection, and slow wound healing. It is crucial to keep a close eye on the wound and the patient’s overall health to spot and treat these issues as soon as they arise. Potential problems can be avoided and managed by providing patients and caregivers with enough knowledge and follow-up.[23] The comparison of wound bed score between the standard and modified vacuum-assisted closure (VAC) groups is shown in Figure 2.[24]

- Comparison of wound bed score between the standard and modified vacuum-assisted closure (VAC) groups.
COMPARISON WITH CONVENTIONAL WOUND CARE MODALITIES
The comparison of VT with conventional wound modalities is represented in Table 3. There are many things to be considered when contrasting VT with conventional wound care methods, including dressings, debridement, and unloading procedures, efficacy, cost-effectiveness, and patient comfort.[10]
| Vacuum therapy | Standard wound care | |
|---|---|---|
| Efficacy | Through several processes, including the elimination of extra fluid, enhanced blood flow, increased oxygenation, and encouragement of tissue development, enhance wound healing. Aids in granulation tissue production, wound closure, and the reduction of wound size [Figure 2] | Dressings, debridement, and offloading methods, among other conventional procedures, are effective in managing wounds. Dressings can shield the area from outside pollutants and offer a moist environment for healing. Debridement eliminates sick or dead tissue, accelerating the healing process. Techniques called “offloading” relieve pressure on wounds, especially in cases like diabetic foot ulcers. |
| Cost- effectiveness | This can be more expensive than conventional wound care treatments since it requires more expensive specialist dressings and equipment. However, it has been demonstrated to possibly lower total treatment costs by encouraging quicker recovery and shortening hospital stays. | Since traditional methods do not need specialist equipment, they could be initially more affordable. The total cost, however, may change based on the intricacy and length of the wound healing process, as well as how frequently dressings and debridement are needed. |
In recent years, VT has become a viable method for managing and treating musculoskeletal wounds. Applying negative pressure to the wound bed has demonstrated important advantages, such as enhanced wound healing, decreased wound size, increased creation of granulation tissue, and encouragement of angiogenesis. The comparison of the decrease in wound size in the VAC group as compared with standard wound care is shown in Figure 3.[25] The VT’s effectiveness and applicability might yet be improved with further study and innovation in this area. Future studies could concentrate on finding ways to extend and apply negative pressure more frequently. While the advantages of VT are well acknowledged, research is currently being done to determine the best frequency and length of treatment. To find the best strategy, future research might examine several protocols and look at the impacts of various treatment durations and breaks.
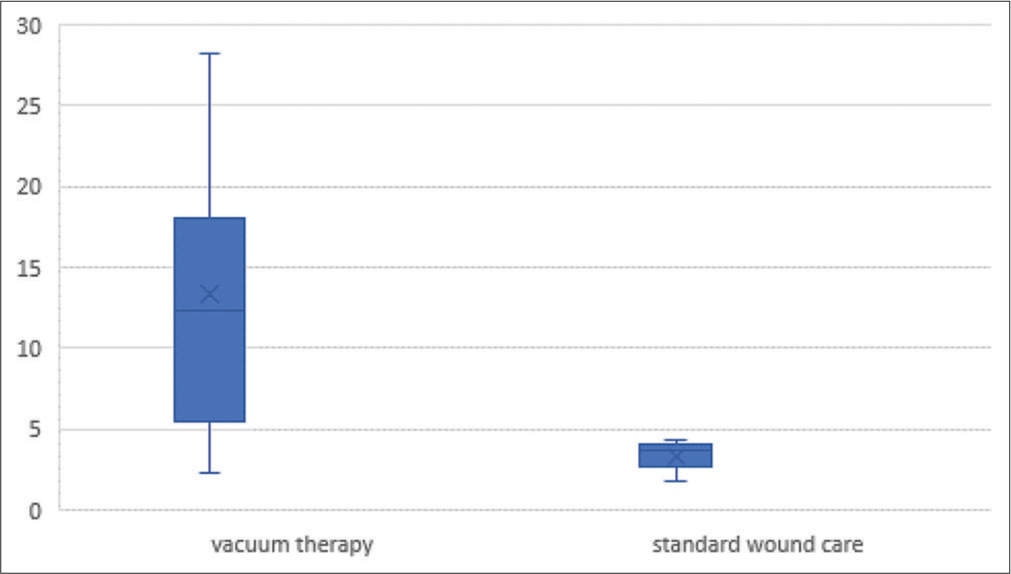
- Box plot comparing the decrease in wound size in the vacuum-assisted closure group and standard wound care.
An additional investigation into the mechanisms of action underpinning VT is also necessary. Although VT has shown promising therapeutic results, the precise molecular mechanisms and cellular reactions at play are still poorly understood.[26] Innovations in this field could offer insightful information about the underlying mechanisms and aid in improving treatment methods. The efficacy of VT in promoting wound healing can be attributed to a combination of cellular and molecular mechanisms that collectively contribute to tissue regeneration and restoration of function. These mechanisms can be broadly categorized into four main areas.
Cellular responses to mechanical stress
The VT exerts its therapeutic effects by creating a controlled mechanical stress environment within the wound bed. This mechanical stress triggers a cascade of cellular responses that promote wound healing. Applying negative pressure induces the activation of signaling pathways, such as the MEK/ERK and PI3K/AKT pathways, which regulate cellular proliferation, migration, and differentiation. This enhanced cellular activity is crucial for forming granulation tissue, a provisional matrix that supports the migration of fibroblasts, endothelial cells, and keratinocytes into the wound bed.[27]
Modulation of blood flow and oxygenation
The negative pressure applied during VT induces vasodilation of surrounding blood vessels, increasing the delivery of oxygen and nutrients to the healing tissues. This improved perfusion not only supports cellular proliferation and migration but also contributes to the reduction of edema, which is a common feature of musculoskeletal wounds.[28]
Reduction of bacterial colonization
The controlled environment created by VT can also contribute to the reduction of bacterial colonization, a major factor impeding wound healing. The negative pressure applied during VT can directly disrupt bacterial biofilms, while the increased blood flow and oxygenation enhance the activity of immune cells involved in bacterial clearance. This reduction in bacterial burden promotes a more favorable healing environment and reduces the risk of infection.[29]
Modulation of inflammatory mediators
The VT has also modulated inflammatory mediators’ expression within the wound bed. The controlled mechanical stress environment can downregulate the production of pro-inflammatory cytokines, such as tumor necrosis factor-alpha and interleukin-1b, and upregulate the production of anti-inflammatory cytokines, such as interleukin-10. This shift in the cytokine profile promotes a more balanced inflammatory response, which is essential for optimal wound healing.[30]
Creating and upgrading more sophisticated and user-friendly VAC systems is another area for advancement. Increased sealing mechanisms, increased negative pressure management, and improved monitoring capabilities might be the main areas of innovation for VAC devices. In addition, creating wearable and portable VAC devices may allow patients to get their treatments with increased comfort and mobility.[31] Further studies investigating the use of VT for certain musculoskeletal wound types, such as pressure ulcers, diabetic foot ulcers, and surgical wounds, might be advantageous regarding wound-specific research. In these situations, VT has unique advantages and difficulties that should be understood to develop more specialized and efficient treatment modalities.
PRACTICE POINTS FOR HEALTH-CARE PROFESSIONALS AND NURSES
This comprehensive review of VT for musculoskeletal wounds provides valuable insights and practical guidance for health-care professionals in various care settings. By understanding the mechanisms of action, evidence-based efficacy, and potential benefits of VT, health-care professionals can make informed decisions about its suitability for individual patients with acute or chronic musculoskeletal wounds, considering each case’s specific characteristics and challenges.
Effectively implement VT by following best practices for patient selection, wound preparation, dressing application, and monitoring. Optimize wound care by integrating VT into a comprehensive treatment plan that includes other appropriate modalities, such as debridement, offloading, and nutritional support.
Educate patients and families about the role of VT in wound healing and provide clear instructions for self-care or home management when applicable. Advocate for evidence-based care by promoting the use of VT when appropriate and sharing their knowledge and experience with other health-care professionals.
STUDY LIMITATIONS ASSOCIATED WITH RESEARCH ON VT IN MUSCULOSKELETAL WOUND CARE
The body of evidence on using VT in musculoskeletal wound care is growing. However, several limitations should be considered when interpreting the findings of existing studies.
Small sample sizes
Many studies on VT have involved small sample sizes, which can limit the generalizability of the findings. This is especially true for studies of VT for specific types of musculoskeletal wounds, such as open fractures and pressure ulcers.
Short study duration
Many studies on VT have been of short duration, which makes it difficult to assess the long-term effects of the treatment. It is important to note that wound healing is a complex process that can take several months or even years to complete.
Heterogeneity of studies
There is great heterogeneity in the types of VT systems used, the wound types studied, and the outcome measures assessed. This makes it difficult to compare the results of different studies and to draw firm conclusions about the overall effectiveness of VT.
Lack of standardization
There is no standardized protocol for using VT in musculoskeletal wound care. This can make it challenging to interpret study results and compare the effectiveness of different treatment approaches.
Potential for bias
Some studies on VT have been funded by the manufacturers of VT devices. This raises the potential for bias in the study design and results. In addition to these general study limitations, some specific limitations are associated with research on VT in different types of musculoskeletal wounds. For example, in studies of VT for the treatment of open fractures, a limitation is that it is difficult to control for the severity of the fracture and the presence of other factors that can affect wound healing, such as infection and malnutrition.
Despite these limitations, the body of evidence on using VT in musculoskeletal wound care is growing. Overall, the evidence suggests that VT can be an effective treatment for various musculoskeletal wounds. However, more research is needed to develop standardized protocols, assess the long-term effects of the treatment, and identify the optimal patient populations and wound types that benefit most from VT.
FUTURE RESEARCH POINTS
Despite the growing body of evidence on using VT in musculoskeletal wound care, there are still many areas where further research is needed. These include:
Developing standardized protocols: There is a need to develop standardized protocols for using VT in different types of musculoskeletal wounds. This would make comparing different studies’ results easier and identify the most effective treatment approaches. Assessing the long-term effects of VT: More research is needed to assess the long-term effects of VT on wound healing and functional outcomes. This is especially important for patients with complex wounds, such as open fractures and pressure ulcers. Identifying the optimal patient populations and wound types for VT: More research is needed to identify the optimal patient populations and wound types that benefit most from VT. This would help ensure the treatment is used as effectively and efficiently as possible.
Investigating the use of VT in combination with other treatments: More research is needed to investigate the use of VT in combination with other treatments, such as antibiotics, growth factors, and stem cells. This could lead to even more effective treatment strategies for musculoskeletal wounds.
Developing new and improved VT systems: New and improved VT systems need to be more user-friendly and effective. This could include developing systems that are more portable and affordable and that can be used to treat a wider range of wounds.
In addition to these general future research points, some specific research questions need to be addressed. For example, more research is needed to investigate the optimal timing and duration of VT for different types of wounds. In addition, more research is needed to develop methods for predicting, which patients are most likely to benefit from VT.
CONCLUSION
This narrative review explored the application of VT in musculoskeletal wound care and management. The VT has been shown to enhance wound healing by promoting angiogenesis, granulation tissue formation, and wound contraction. It has also been found to reduce wound size, promote the formation of healthy granulation tissue, and decrease the risk of infection. Adequate patient selection, appropriate wound preparation, and proper technique and equipment usage are key factors for achieving optimal outcomes.
Recommendations
Further research is warranted to establish standardized protocols and guidelines, as well as to investigate their long-term efficacy and cost-effectiveness. The VT has the potential to enhance outcomes further and improve the quality of life for patients with musculoskeletal wounds.
ETHICAL APPROVAL
The Institutional Review Board approval is not required.
DECLARATION OF PATIENT CONSENT
Patient’s consent not required as there are no patients in this study.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- The treatment of impaired wound healing in diabetes: Looking among old drugs. Pharmaceuticals (Basel). 2020;4:60.
- [CrossRef] [PubMed] [Google Scholar]
- New evidence-based therapies for complex diabetic foot wounds. Compendia. 2022;2:1-23.
- [CrossRef] [PubMed] [Google Scholar]
- Recent technological advances in the management of chronic wounds: A literature review. Health Sci Rep. 2022;3:e641.
- [CrossRef] [PubMed] [Google Scholar]
- Vacuum assisted closure (VAC)/negative pressure wound therapy (NPWT) for difficult wounds: A review. J Clin Orthop Trauma. 2019;10:845-8.
- [CrossRef] [PubMed] [Google Scholar]
- A review of current advancements for wound healing: Biomaterial applications and medical devices. J Biomed Mater Res B Appl Biomater. 2022;110:2542-73.
- [CrossRef] [PubMed] [Google Scholar]
- The role of vacuum technology in proton-based therapy systems. Available from: https://www.agilent.com/about/features/en/vacuum-proton-therapy.html [Last accessed on 2023 Jun 02]
- [Google Scholar]
- The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
- [CrossRef] [PubMed] [Google Scholar]
- Vacuum assisted closure therapy versus standard wound therapy for open musculoskeletal injuries. Adv Orthop. 2013;2013:e245940.
- [CrossRef] [PubMed] [Google Scholar]
- Innovative treatment strategies to accelerate wound healing: Trajectory and recent advancements. Cells. 2022;11:2439.
- [CrossRef] [PubMed] [Google Scholar]
- Filling the vacuum: Role of negative pressure wound therapy in open wound management in cats. J Feline Med Surg. 2021;23:823-33.
- [CrossRef] [PubMed] [Google Scholar]
- Wound VAC process, benefits, side effects, complications and cost. Available from: https://www.healthline.com/health/wound-vac [Last accessed on 2023 Jun 02]
- [Google Scholar]
- Negative pressure wound therapy in patients with wounds healing by secondary intention: A systematic review and meta-analysis of randomised controlled trials. Syst Rev. 2020;9:238.
- [CrossRef] [PubMed] [Google Scholar]
- Negative pressure wound therapy versus conventional wound dressings in treatment of open fractures: A systematic review and meta-analysis. Int J Surg. 2018;53:72-9.
- [CrossRef] [PubMed] [Google Scholar]
- Negative-pressure wound therapy versus standard dressings for adults with an open lower limb fracture: The WOLLF RCT. Health Technol Assess. 2018;22:1-162.
- [CrossRef] [Google Scholar]
- Negative pressure wound therapy: Mechanism of action and clinical applications. Semin Plast Surg. 2021;35:164-70.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term risk of hysterectomy and ectopic pregnancy among Vietnamese women using the quinacrine hydrochloride pellet system vs. intrauterine devices or tubal ligation for contraception. Eur J Contracept Reprod Health Care. 2018;23:105-15.
- [CrossRef] [PubMed] [Google Scholar]
- Healing chronic wounds: Current challenges and potential solutions. Curr Dermatol Rep. 2018;7:296-302.
- [CrossRef] [PubMed] [Google Scholar]
- Key challenges in wound care management and how to solve them. 2021. Available from: https://www.medicaldevice-network.com/sponsored/key-challenges-in-wound-care-management [Last accessed on 2023 Jun 02]
- [Google Scholar]
- Challenges and management in wound care. Plast Reconstr Surg. 2021;147:9S-15.
- [CrossRef] [PubMed] [Google Scholar]
- Breakthrough treatments for accelerated wound healing. Sci Adv. 2023;9:eade7007.
- [CrossRef] [PubMed] [Google Scholar]
- The effectiveness of negative pressure therapy: Nursing approach. J Pers Med. 2022;12:1813.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized controlled trial to assess the cost-effectiveness of a novel, simple modification to the negative pressure wound therapy system. Plast Reconstr Surg Glob Open. 2021;9:e3787.
- [CrossRef] [PubMed] [Google Scholar]
- Vacuum assisted closure therapy versus standard wound therapy for open musculoskeletal injuries. Adv Orthop. 2013;2013:e245940.
- [CrossRef] [PubMed] [Google Scholar]
- Physical mechanisms underpinning the vacuum permittivity. 2021. Available from: http://arxiv.org/abs/2110.07223 [Last accessed on 2023 Jun 02]
- [Google Scholar]
- Negative pressure wound therapy In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK576388 [Last accessed on 2023 Sep 04]
- [Google Scholar]
- Effect of electrical stimulation on blood flow velocity and vessel size. Open Med (Wars). 2017;12:5-11.
- [CrossRef] [PubMed] [Google Scholar]
- Wound dressings and comparative effectiveness data. Adv Wound Care (New Rochelle). 2014;3:511-29.
- [CrossRef] [PubMed] [Google Scholar]
- Immunology of acute and chronic wound healing. Biomolecules. 2021;11:700.
- [CrossRef] [PubMed] [Google Scholar]
- Endoluminal vacuum therapy (E-Vac): A treatment option in oesophagogastric surgery. World J Surg. 2018;42:2507-11.
- [CrossRef] [PubMed] [Google Scholar]






