Translate this page into:
Analyzing spinopelvic parameter differences between standing and supine position
*Corresponding author: Arief Prasetya, MD. Doctoral Programme of Health and Medicine, Medical Faculty, Diponegoro University, Semarang, Indonesia. ariefindra.orthopaedi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Prasetya A, Nabih D, Santoso A, Jamari J, Winarni T. Analyzing spinopelvic parameter differences between standing and supine position. J Musculoskelet Surg Res. 2025;9:11-27. doi: 10.25259/JMSR_375_2024
Abstract
This study aimed to investigate the differences in spinopelvic parameters, including pelvic tilt (PT), sacral slope (SS), lumbar lordosis (LL), and pelvic incidence (PI), measured in standing and supine positions using standing computed tomography (CT) scans. Due to the limited availability of standing CT scans in Indonesia, this review analyzed data from combined Web of Science, Scopus, and PubMed databases. Following a comprehensive literature search, the full text of relevant articles was downloaded and evaluated for eligibility based on predefined inclusion and exclusion criteria. The final list of studies included 11 for LL, 8 for SS, 6 for PI, and 11 for PT. The results showed significant differences in SS and PI measurements between standing and supine positions in normal patients (p<0.05). However, no significant differences were found in LL, PT, and all spinopelvic parameters in patients with lumbar disc degeneration (p>0.05). These findings suggest that supine position CT scans can effectively and accurately represent the patient’s condition for certain spinopelvic parameters, particularly in patients with lumbar disc degeneration.
Keywords
Lumbar lordosis
Pelvic tilt
Pelvic incidence
Sacral slope
Spinopelvic parameter
Standing position
Supine position
INTRODUCTION
Spinopelvic parameters are measurement instruments that show the relationship between the patient’s spinal structure and pelvic alignment. They have been accepted as a standard measurement for assessing sagittal spinopelvic balance.[1] Spinopelvic parameters, including pelvic incidence (PI), sacral slope (SS), lumbar lordosis (LL), and pelvic tilt (PT) measurements, are essential for various spinal surgical interventions.[2]
Spinopelvic parameters play a crucial role in various clinical settings, including the diagnosis and management of spinal deformities, degenerative conditions, and other orthopedic disorders. These parameters are integral in pre-surgical planning for conditions such as scoliosis, spondylolisthesis, and adult spinal deformity (ASD), where maintaining or restoring proper sagittal balance is key to reducing pain and improving patient outcomes.[3] Furthermore, post-operative assessments of spinopelvic parameters help predict surgical outcomes and guide rehabilitation strategies, ensuring that spinal alignment remains functional and stable post-surgery.[4]
Spinopelvic parameters can be assessed with the patient in a standing or supine position.[5] Computed tomography (CT) scans, magnetic resonance imaging (MRI), and radiographs are the conventional radiographic systems used to measure the spinopelvic parameter both in the standing or supine position. Among the available radiography equipment options, CT scan is the main choice because of its high accuracy with image transparency features and results that are not dependent on the radiographer’s expertise. Unlike CT scans, estimating radiographic error parameters can be challenging due to their significant dependence on the distance and direction between the radiography system and the patient.
In ASD, standing whole spinal CT scans are commonly used to evaluate spinopelvic parameters because they represent the alignment of the spine under weight-bearing conditions and supine spinal CT scan is particularly useful in cases where weight-bearing is painful or not possible for the patient.[4] Although measuring spinopelvic parameters in a standing CT scan is highly recommended, there are still very few countries that have standing CT scans. Indonesia is one of the countries that have not had standing CT scan facilities thus far. Due to the unavailability of standing CT scans in Indonesia, radiographs are used in standing spinopelvic parameters, and CT scans are used in supine spinopelvic parameters. Therefore, it is critical to understand how much spinopelvic parameter measurements taken in the standing and supine postures may differ.
Numerous studies have compared spinopelvic parameters in lying and standing positions, yet the results still vary significantly. While standing CT scans are considered the gold standard for evaluating these parameters under weight-bearing conditions, the unavailability of such facilities in many regions, including Indonesia, necessitates alternative approaches. Therefore, this review aimed to compile and analyze published data from Web of Science, Scopus, and PubMed to better understand the relationship between supine and standing measurements. By highlighting the differences and potential limitations of using supine measurements, this study provides valuable insights for clinicians in resource-limited settings, serving as a practical guide where standing CT is not accessible.
MATERIALS AND METHODS
A systematic review was carried out following preferred reporting items for systematic reviews and meta-analyses (PRISMA) criteria. The proposed keywords underwent cross-referencing with the International Prospective Register of Systematic Reviews (PROSPERO) database before initiating the formal search to determine if a similar systematic review had already been published or registered. No relevant results were identified during this search. The literature search was conducted following PRISMA principles and was extended until April 8, 2024. In addition, the study protocol has been registered with the PROSPERO under registration number CRD42024552962.
Following a comprehensive preliminary review of the literature, including keywords, titles, and abstracts from three databases – PubMed, SCOPUS, and Web of Science – pertaining to “Lumbar lordosis,” “Sacral slope,” “Pelvic tilt,” and “Pelvic incidence,” the references obtained were further examined through an additional title, keyword and abstract searches. This process aimed to categorize the studies into two distinct groups. The first group included studies that referenced “Standing position,” while the second group comprised those that mentioned “Supine position” or “Lying position.”
The inclusion criteria are outlined as follows: (i) Original and complete studies in humans; (ii) studies can be accessed and written in English; and (iii) containing the degrees of spinopelvic parameters in standing and supine positions. The exclusion criteria are outlined as follows: (i) Post-operative patient, (ii) patient with lumbar spine bone tumor, (iii) patient with lumbar spine infection (e.g., Tuberculosis Spondylitis), (iv) patient with congenital lumbar spine disease (e.g., Scoliosis).
Two separate reviewers made their selections of the papers. At first, case studies, editorials, duplicates, unfinished publications, and non-original research were disqualified. Titles that did not align with our selection criteria were eliminated during the screening process. The publications that met the inclusion and exclusion criteria were fully evaluated following a comprehensive review of their respective abstracts. The reviewers reached a final, independent conclusion. The list of citations was checked to determine which references from each paper should be included in this evaluation.
In assessing the variability among the included studies, we conducted a heterogeneity analysis using I2 statistics to quantify the degree of variation in effect estimates. This approach ensured a comprehensive understanding of how differences among studies could influence the overall findings of this review. In addition, we performed a qualitative assessment by examining the I2 statistics to identify any studies that significantly contributed to increasing the I2 value. Studies with a substantial impact on the I2 statistic were excluded from the analysis to maintain the robustness of the findings.
Review manager 5.4 is used for data processing using “continuous” data analysis, a statistical method of “inverse variance,” an analysis model of “randomized effect,” an effect measure using “mean difference” and a confidence interval of 95%. The statistical values collected from each study are the “mean” and “standard deviation” of the degrees of supine and standing position. After the statistical values are collected, the data is then processed and analyzed in the form of funnel plots and forest plots. A risk of bias assessment was conducted for each included study using the Cochrane Risk of Bias Tool. The findings from the risk of bias analysis are presented in the table of the forest plot, which provides an overview of the quality of the included studies and their potential impact on the overall findings of this review. The AI tool available at https://goblin.tools/Formalizer has been utilized in this study to enhance the formality of the text and reduce grammatical errors.
RESULTS
As of the submission date for this review, no systematic reviews have been registered or published that specifically address the differing effects of standing and supine positions on spinopelvic parameters. The initial stage of our identification process involved searching for papers utilizing the keywords “Lumbar lordosis,” “Sacral slope,” “Pelvic tilt,” and “Pelvic incidence” in the Web of Science databases, Scopus, and PubMed, then adding an additional keyword of “standing position” and “supine position”/”lying position” then the data were exported to EndNote 20 reference manager. A total of 4782 studies were collected (2966 from PubMed, 1705 from Scopus and 111 from Web of Science) for Lumbar lordosis, 2430 studies (1365 from PubMed, 730 from Scopus and 335 from Web of Science) for SS, 11728 studies (8251 from PubMed, 2684 from Scopus and 793 from Web of Science) for PI, and 6227 total studies (3571 from PubMed, 1736 from Scopus and 920 from Web of Science) for PT.
A total of 4782 studies on LL were screened based on established inclusion criteria, resulting in 25 studies being shortlisted. The full texts of these 25 papers were then evaluated for eligibility according to inclusion and exclusion criteria, leading to the selection of 11 studies for inclusion regarding LL [Figure 1]. Similarly, 2340 studies on SSs were screened, yielding 16 relevant studies. The full texts of these 16 papers underwent eligibility assessment based on the same criteria, resulting in 10 studies initially selected, with 2 studies subsequently excluded based on a qualitative assessment to reduce heterogeneity, leading to a final inclusion of 8 studies for SS [Figure 2]. After screening 11,728 studies on PI, 14 studies were identified as potentially relevant. Following a detailed evaluation of these full texts against the inclusion and exclusion criteria, six studies were ultimately selected for inclusion in the analysis of PI [Figure 3]. Finally, 6227 studies on PT were reviewed, with 35 studies meeting the preliminary screening criteria. The full texts of these 35 papers were subsequently evaluated for eligibility, resulting in 11 studies included for PT [Figure 4].
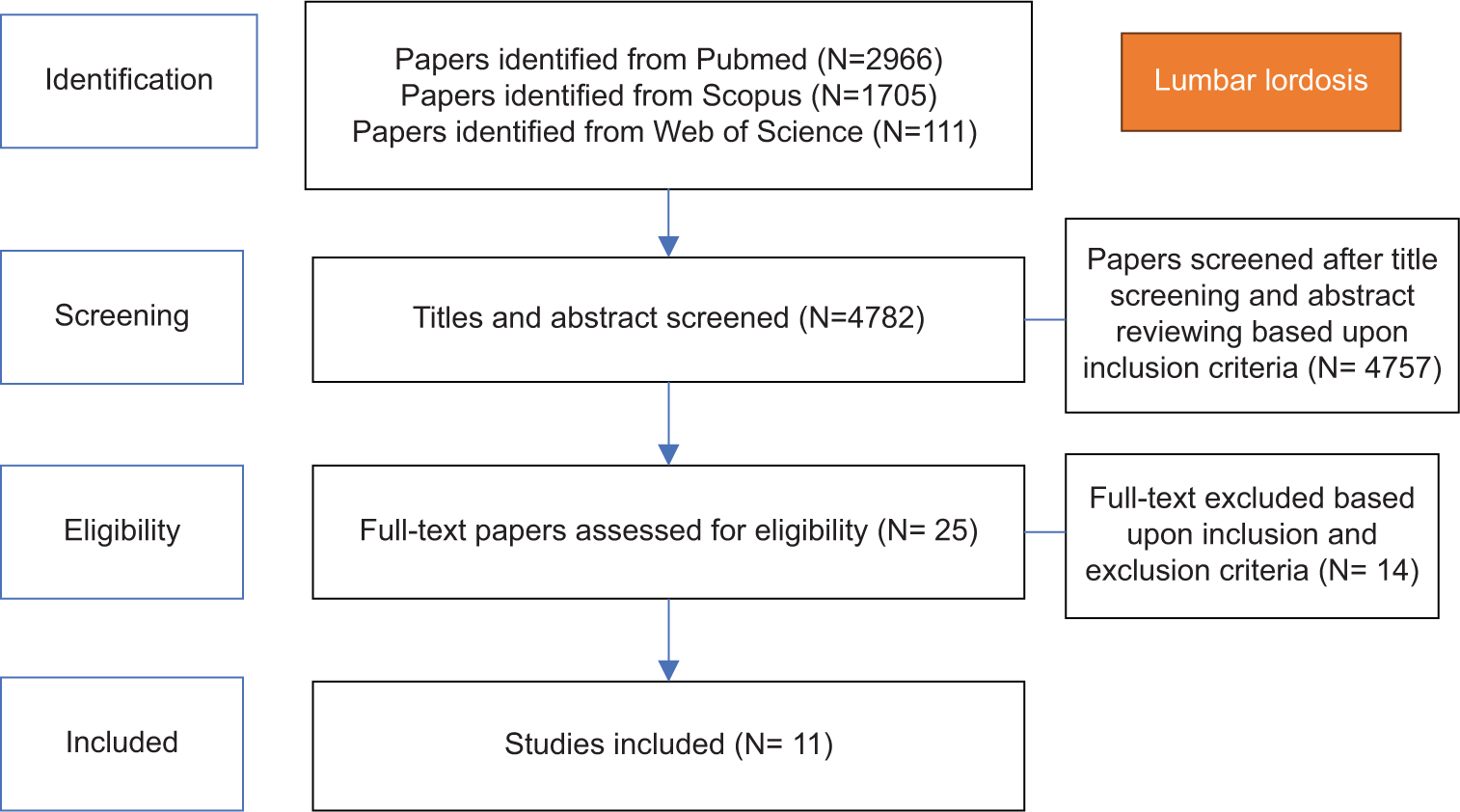
- Preferred reporting items for systematic reviews and meta-analyses approach of lumbar lordosis. N: Number of studies.
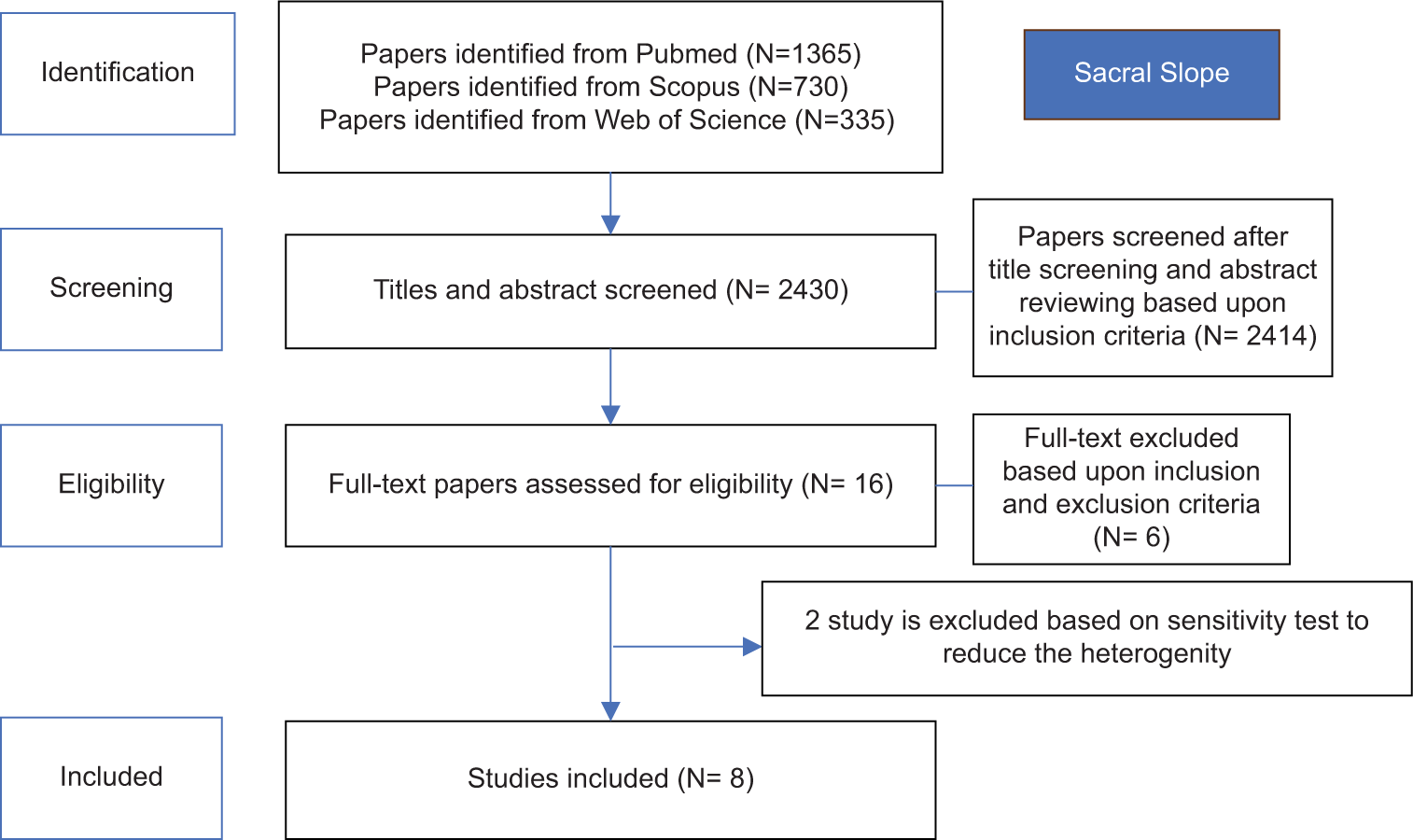
- Preferred reporting items for systematic reviews and meta-analyses approach of sacral slope. N: Number of studies.
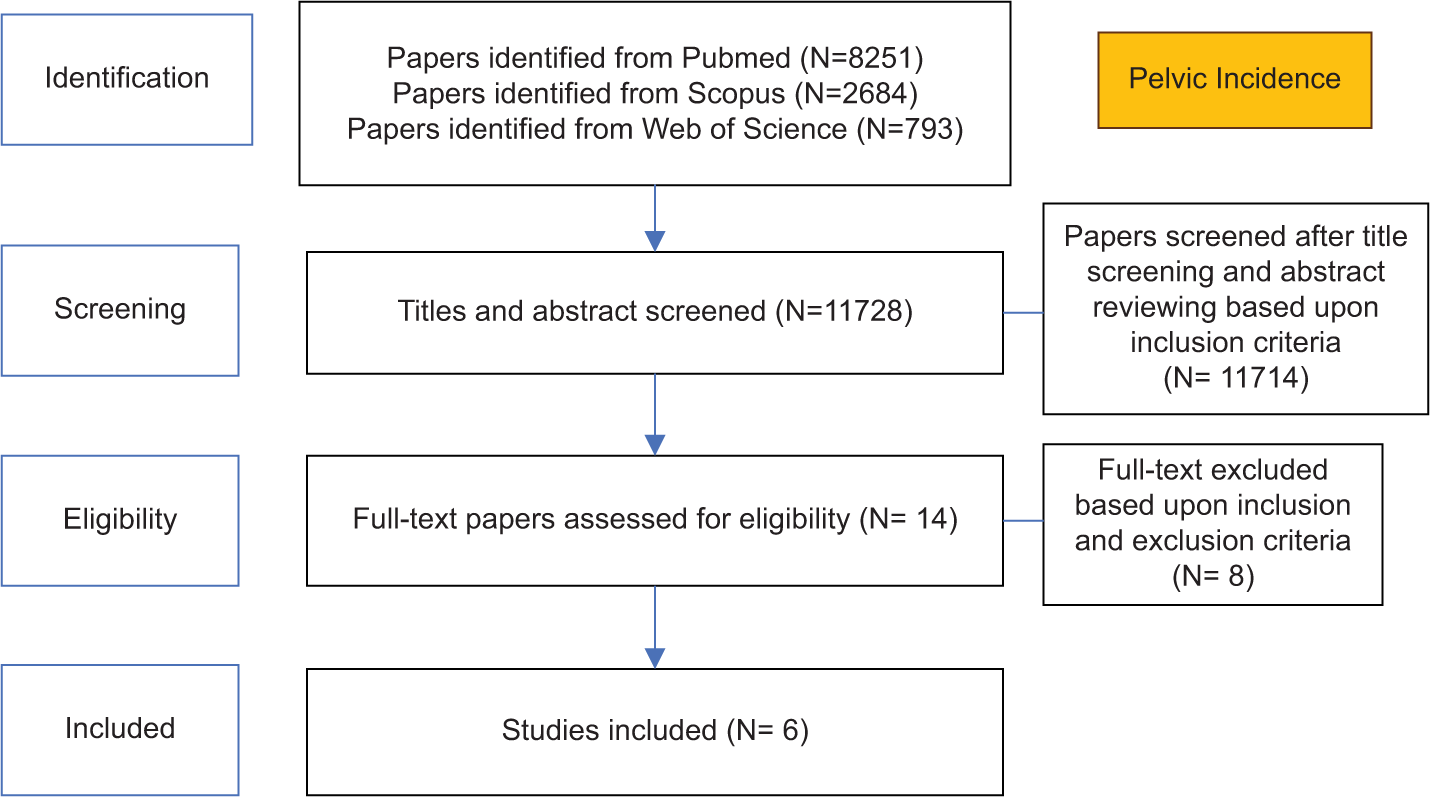
- Preferred reporting items for systematic reviews and meta-analyses approach of pelvic incidence. N: Number of studies.
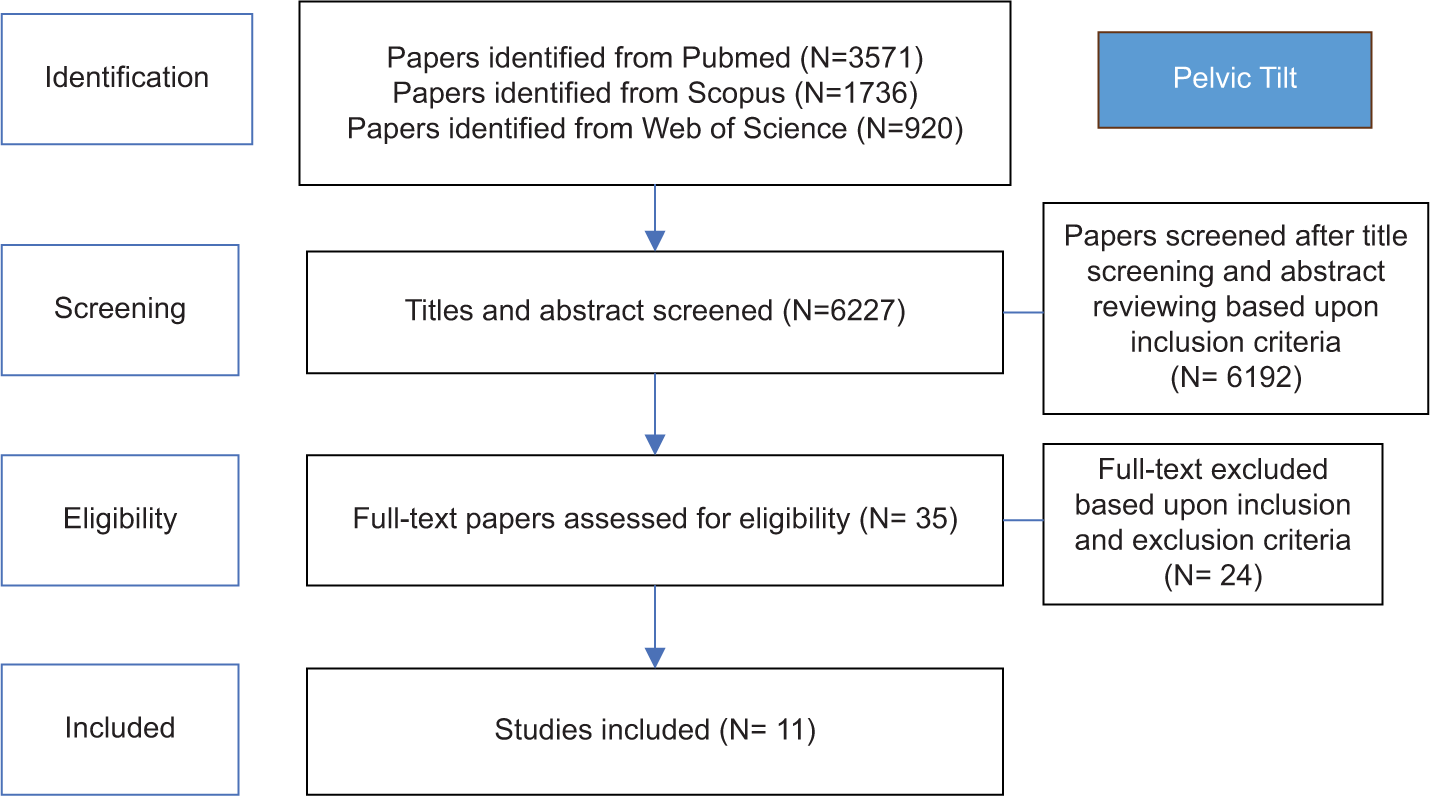
- Preferred reporting items for systematic reviews and meta-analyses approach of pelvic tilt. N: Number of studies.
To assess the consistency and variability of findings across studies, we conducted a heterogeneity analysis using I2 statistics, which quantified the degree of variation in effect estimates for each parameter. During our qualitative assessment, we identified two studies in the SS category that contributed substantially to the I2 value. These two studies were excluded to reduce heterogeneity, resulting in a decreased I2 statistic and improved consistency in SS findings. For LL and PT, removing individual studies did not yield a meaningful decrease in I2. This suggests that variability may stem from inherent study differences rather than any single study’s influence. In addition, no studies were removed from the PT category to avoid overly reducing the sample size, which would compromise the reliability of the findings.
Table 1 provides an overview of the 11 selected references that were analyzed to investigate the differences in lumbar lordosis measurements between standing and supine positions. Table 2 outlines the eight selected references examined to assess variations in SS measurements when comparing standing and supine positions. Table 3 includes the six selected references reviewed to evaluate differences in PI measurements between standing and supine positions. Lastly, Table 4 summarizes the 11 selected references analyzed to examine the differences in PT measurements from standing and supine positions.
| Author, Year | Journal title | Sample | Method | Result | Conclusion | |
|---|---|---|---|---|---|---|
| 1. | Bailey et al. (2016)[6] | Morphological and postural sexual dimorphism of the lumbar spine facilitates greater lordosis in females | 196 (asymptomatic, 75M/121F) | X-ray assessed LL in standing and supine positions | Mean LL in standing position 56.01 SD 1.52° and supine position 47.36 SD 1.6° | Standing>Supine, significant (P<0.05) |
| 2. | Chevillotte et al. (2018)[5] | Influence of posture on relationships between pelvic parameters and lumbar lordosis: Comparison of the standing, seated, and supine positions. A preliminary study | 15 (asymptomatic; 5M/10F) | X-ray assessed LL in standing, seated, and supine positions | Mean LL standing 54.8 SD 9.6°, supine 50.2 SD 9.6° | Standing>Supine, significant |
| 3. | Fan et al. (2023)[7] | Comparison of sagittal spinal alignment on standing plain X-rays and supine MRI in degenerative lumbar disease | 64 (degenerative lumbar disease; 30M/34F) | X-ray and MRI assessed LL in standing and supine positions. | Mean LL standing 40 SD 1.3°, supine 40 SD 1.6° (no significant difference) | LL is slightly greater in supine. |
| 4. | Fei et al. (2017)[8] | Effect of patient position on the lordosis and scoliosis of patients with degenerative lumbar scoliosis | 77 (degenerative lumbar scoliosis; 18M/59F) | MRI assessed LL in standing and supine positions | Mean LL standing 23.5 SD 12.7°, supine 25.5 SD 10.3° | LL increases in supine position in DLS patients. |
| 5. | Hansen et al. (2015)[9] | Effect of Lumbar Disc Degeneration and Low-Back Pain on the Lumbar Lordosis in Supine and Standing: A Cross- Sectional MRI Study | 76 (38 with LBP; 38 back-healthy; 17M/21F) | MRI assessed LL in standing and supine positions | Mean LL standing 55.28 SD 10.86°, supine 48.88 SD 10.89° | Standing>Supine, significant |
| 6. | Hasegawa et al. (2018)[10] | Difference in whole spinal alignment between supine and standing positions in patients with adult spinal deformity using a new comparison method with slot-scanning three-dimensional X-ray imager and computed tomography through digital reconstructed radiography. | 24 (adult spinal deformity; all female) | CT and slot- scanning 3D X-ray assessed LL in standing and supine positions | Standing: 21.8° (SD 25.5°); Supine: 33.1° (SD 17.5°) | Supine>Standing, significant |
| 7. | Hey et al. (2017)[11] | Lumbar spine alignment in 6 common postures - a ROM analysis with implications for deformity correction | 70 (low back pain; 34M/36F) | X-ray assessed LL in six postures including standing and supine | Standing: 48.4° (SD 148°); Supine: 38.1° (SD 18.1°) | Standing>Supine, significant |
| 8. | Lee (2014)[12] | The effect of age on sagittal plane profile of the lumbar spine according to standing, supine, and various sitting positions | 20 (younger and older males) | X-ray assessed LL in multiple positions including standing and supine | LL reduction from standing to supine: 12.04° (younger), 18.78° (older); standing mean 52.20° | Younger males had greater flexibility |
| 9. | Mauch et al. (2010)[13] | Changes in the Lumbar Spine of Athletes From Supine to the True-Standing Position in Magnetic Resonance Imaging Frieder Mauc | 35 (asymptomatic athletes; 20M/15F) | MRI assessed LL in standing and supine positions | Mean LL standing: 52.6° SD 8.9°, supine: 46.3° SD 9.3° | Standing>Supine, significant |
| 10. | Nordberg et al. (2020)[14] | Positional changes in lumbar disc herniation during standing or lumbar extension: a cross- sectional weight-bearing MRI study | 37 (lumbar disc herniation; 19M/18F) | MRI assessed LL in standing and supine positions | Mean LL standing: 48.34° SD 10.28°, supine: 42.73° SD 9.32° | Standing>Supine, significant |
| 11. | Yasuda (2018)[15] | Effect of position on lumbar lordosis in patients with adult spinal deformity | 85 (adult spinal deformity; 11M/74F) | X-ray assessed LL in standing and supine positions pre- operatively | Mean LL standing: 7.8° SD 23, supine: 22.1° SD 17 | Supine>Standing, significant. |
SD: Standard deviation, LL: Lumbar lordosis, MRI: Magnetic resonance imaging, CT: Computed tomography, F: Female, M: Male, DLS: Degenerative lumbar scoliosis, LBP: Low back pain.
| Author, Year | Journal title | Sample | Method | Result | Conclusion | |
|---|---|---|---|---|---|---|
| 1. | Chevillotte et al. (2018)[5] | Influence of posture on relationships between pelvic | 15 (asymptomatic; | X-ray assessed SS | Mean SS standing: 37.1° | Supine>Standing, not significant |
| parameter and lumbar lordosis: | 5M/10F) | in standing, | SD 6.3°, supine: | |||
| Comparison of the standing, | seated, | 41.0° SD 7.2° | ||||
| seated, and supine positions. A | and supine | |||||
| preliminary study | positions | |||||
| 2. | Fan et al. (2023)[7] | Comparison of sagittal spinal | 64 | X-ray and | Mean SS | Supine>Standing, not |
| alignment on standing plain | (degenerative | MRI assessed | standing: 33° | significant | ||
| X-rays and supine MRI in | lumbar disease; | SS in standing | SD 11°, supine: | |||
| degenerative lumbar disease | 30M/34F) | and supine | 35° SD 9° | |||
| positions | ||||||
| 3. | Hasegawa et al., 2018[10] | Difference in whole spinal alignment between supine and | 24 (adult spinal deformity; all | CT and slot- scanning | Mean SS standing: | Supine>Standing, significant (P=0.0003) |
| standing positions in patients | female) | 3D X-ray | 27.0° SD 14.1°, | |||
| with adult spinal deformity using | assessed SS | supine: 34.1° | ||||
| a new comparison method with | in standing | SD 10.5° | ||||
| slot-scanning three-dimensional | and supine | |||||
| X-ray imager and computed | positions | |||||
| tomography through digital | ||||||
| reconstructed radiography. | ||||||
| 4. | İplikçioğlu and Karabağ, 2022[16] | Validity and Reliability of Spinopelvic Parameters | 33 (healthy volunteers; | X-ray and CT | Mean SS standing: 35.3°, | Supine>Standing, not significant |
| Measured on computed tomography | 18M/15F) | assessed SS in standing | supine: 36.2° | |||
| and supine | ||||||
| positions | ||||||
| 5. | İplikçioğlu and Karabağ, 2023[17] | Posterior Pubic Incidence: A Novel Morphologic Spinopelvic | 104 (healthy volunteers; | X-ray and CT | Mean SS standing: | Supine>Standing, significance unknown |
| Parameter Nearly Equal to Pelvic Incidence | 57M/47F) | assessed SS in standing | 36.47° SD 7.85°, supine: | |||
| and supine | 39.92° SD 8.50° | |||||
| positions | ||||||
| 6. | Karabag et al., 2022[18] | Pelvic incidence measurement with supine magnetic resonance | 26 (asymptomatic | MRI assessed SS | Mean SS standing: | Supine>Standing, not significant |
| imaging: A validity and reliability | volunteers; | in standing | 36.85° SD | |||
| study | 14M/12F) | and supine positions | 4.04°, supine: 39.35° SD 5.53° | |||
| 7. | Park et al., 2017[19] | Changes of spinopelvic parameters in different positions | 71 (healthy volunteers; 21M/50F) | SS measured in X-ray standing and | Mean SS standing: 34.7° SD 9.8°, supine: | CT Supine>X-ray Standing, significant (P<0.001) |
| CT supine | 39.6° SD 8.3° | |||||
| positions | ||||||
| 8. | Philippot et al., 2008[20] | Pelvic balance in sagittal and Lewinnek reference planes in | 67 (elderly patients with | X-ray assessed SS in standing, | Mean SS standing: | Supine>Standing, not significant |
| the standing, supine and sitting | coxarthrosis; | sitting, | 42.4° SD 12.6°, | |||
| positions | 41M/26F) | and supine positions | supine: 43.9° SD 11.1° |
SD: Standard deviation, SS: Sacral slope, MRI: Magnetic resonance imaging, CT: Computed tomography, F: Female, M: Male
| Author, Year | Journal title | Sample | Method | Result | Conclusion | |
|---|---|---|---|---|---|---|
| 1. | Bao et al., 2021[21] | Position-related Change of PI | 131 | X-ray | Mean PI | Standing>Supine, |
| Depends on the Non-fused | (degenerative | and CT | standing: | significant (P<0.001) | ||
| Sacroiliac Joint in Patients with | spinal disease; | assessed PI | 53.68° SD | |||
| Degenerative Spinal Diseases | all female) | in standing | 6.28°, supine: | |||
| and supine | 47.17° SD 6.24° | |||||
| positions | ||||||
| 2. | Chevillotte et al. (2018)[5] | Influence of posture on relationships between pelvic | 15 (asymptomatic; | X-ray assessed PI | Mean PI standing: | Supine>Standing, not significant |
| parameters and lumbar lordosis: | 5M/10F) | in standing, | 49.3° SD 8.1°, | |||
| Comparison of the standing, | seated, | supine: 50.4° | ||||
| seated, and supine | and supine | SD 6.7° | ||||
| positions | ||||||
| 3. | Hasegawa et al. (2018)[10] | Difference in whole spinal alignment between supine and standing | 24 (adult spinal deformity; all | CT and slot- scanning | Mean PI standing: | Standing>Supine, significant |
| positions in patients with adult spinal | female) | 3D X-ray | 57.7° SD 10.9°, | (P=0.0013) | ||
| deformity using a new comparison | assessed PI | supine: 53.4° | ||||
| method with slots canning three- | in standing | SD 9.2° | ||||
| dimensional X-ray imager and | and supine | |||||
| computed tomography through digital reconstructed radiography | positions | |||||
| 4. | Mikula et al., 2021[22] | Change in PI between the supine and standing positions in patients | 73 (SI joint vacuum; | X-ray and CT | Mean PI standing: 52° | Standing>Supine, significant |
| with bilateral sacroiliac joint vacuum signs | 43M/30F) | assessed PI in standing | SD 14°, supine: 48° SD 12° | |||
| and supine | ||||||
| positions | ||||||
| 5. | Philippot et al., 2008[20] | Pelvic balance in sagittal and Lewinnek reference planes in | 67 (elderly patients with | X-ray assessed PI | Mean PI standing: | Supine>Standing, not significant |
| the standing, supine and sitting | coxarthrosis; | in standing, | 59.6° SD 6.86°, | |||
| positions | 41M/26F) | sitting, | supine: 59.8° | |||
| and supine | SD 12.8° | |||||
| positions | ||||||
| 6. | Xu et al., 2020[23] | Correlation and Differences in | 105 | X-ray | Mean PI | Standing>Supine, |
| Lumbopelvic Sagittal Alignment | (degenerative | and MRI | standing: | significant (P<0.001) | ||
| Parameters Between Lumbar | lumbar disease; | assessed PI | 56.9° SD 15.6°, | |||
| Radiographs and Magnetic Resonance Images | 47M/58F) | in standing and supine positions | supine: 50.2° SD 16.7° |
PI: Pelvic incidence, SD: Standard deviation, MRI: Magnetic resonance imaging, CT: Computed tomography, F: Female, M: Male
| Author, Year | Journal title | Sample | Method | Result | Conclusion | |
|---|---|---|---|---|---|---|
| 1. | Buckland et al., 2019[24] | Effects of sagittal spinal alignment on postural pelvic mobility in total | 288 (total hip arthroplasty | X-ray assessed PT in supine, | Mean PT standing: | Standing>Supine, significant |
| hip arthroplasty candidates | candidates; 147M/141F) | standing, seated, and | 15.09° SD 8.24°, supine: | (P<0.001) | ||
| stepping-up | 9.59° SD 6.61° | |||||
| positions | ||||||
| 2. | Chevillotte et al., 2018[5] | Influence of posture on relationships between pelvic | 15 (asymptomatic; | X-ray assessed PT in standing, | Mean PT standing: 12.1° | Standing>Supine, significant |
| parameters and lumbar lordosis: | 5M/10F) | seated, | SD 6.3°, supine: | |||
| Comparison of the standing, | and supine | 9.5° SD 5.1° | ||||
| seated, and supine positions. A | positions | |||||
| preliminary study | ||||||
| 3. | Hasegawa et al. (2018)[10] | Difference in whole spinal alignment between supine and | 24 (adult spinal deformity; all | CT and slot- scanning 3D | Mean PT standing: | Standing>Supine, significant |
| standing positions in patients with | female) | X-ray assessed | 30.7° SD 10.6°, | (P<0.0001) | ||
| adult spinal deformity using a new | PT in standing | supine: 19.2° | ||||
| comparison method with slot- | and supine | SD 7.5° | ||||
| scanning three-dimensional X-ray | positions | |||||
| imager and computed tomography | ||||||
| through digital reconstructed | ||||||
| radiography. | ||||||
| 4. | İplikçioğlu and Karabağ, 2022 | Validity and Reliability of Spinopelvic Parameters Measured on Computed | 33 (healthy volunteers; 18M/15F) | X-ray and CT assessed PT in standing | Mean PT standing: 10° SD 6.7°, supine: | Standing>Supine, not significant |
| and supine | 8.2° SD 5.7° | |||||
| positions | ||||||
| 5 | Karabag et al., 2022 | Pelvic incidence measurement with supine magnetic resonance imaging: A validity and reliability study | 26 (asymptomatic volunteers; 14M/12F) | MRI assessed PT in standing and supine positions | Mean PT standing: 15.23° SD 4.73°, supine: 12.07° SD 3.9° | Standing>Supine, significant (P<0.05) |
| 6 | Klemt et al., 2020[25] | Effect of postural changes | 48 (THA | CT and | Supine: −16.6° | Standing>Supine, |
| on in vivo PT and functional | with/without | fluoroscopy | (severe lumbar | significant | ||
| component anteversion in total | lumbar DDD; | assessed PT | DDD) versus | |||
| hip arthroplasty patients with lumbar disc degenerations | 9M/39F) | in supine and upright postures | −12.3° (control group); Upright: 1.0° | |||
| versus −3.6° | ||||||
| 7. | Mikula et al., 2021 | Change in pelvic incidence | 73 (SI joint | X-ray and CT | Mean PT | Standing>Supine, |
| between the supine and standing | vacuum; | assessed PT | standing: 23° | significant | ||
| positions in patients with bilateral sacroiliac joint vacuum signs | 43M/30F) | in standing and supine | SD 10°, supine: 17° SD 8° | |||
| positions | ||||||
| 8. | Park et al., 2017 | Changes of spinopelvic parameters in different positions | 71 (healthy volunteers; 21M/50F) | X-ray and CT assessed PT in standing | Mean PT standing: 18.6° SD 9.9°, supine: | Standing>Supine, significant (P<0.001) |
| and supine | 12.0° SD 6.8° | |||||
| positions | ||||||
| 9 | Tachibana, 2019[26] | Does Acetabular Coverage Vary | 65 (hip | X-ray and CT | Mean PT | Standing>Supine, |
| Between the Supine and Standing | dysplasia; | assessed PT | standing: 15° | significant | ||
| Positions in Patients with Hip Dysplasia? | 4M/61F) | in standing and supine positions | SD 7°, supine: 9° SD 5° | (P<0.001) | ||
| 10 | Xu et al., 2020 | Correlation and Differences in | 105 | X-ray and MRI | Mean PT | Standing>Supine, |
| Lumbopelvic Sagittal Alignment | (degenerative | assessed PT | standing: | significant | ||
| Parameters Between Lumbar | lumbar disease; | in standing | 18.5° SD 10.4°, | (P<0.05) | ||
| Radiographs and Magnetic | 47M/58F) | and supine | supine: 16.3° | |||
| Resonance Images | positions | SD 8.8° | ||||
| 11 | Yun et al., 2017[27] | Effect of PT and rotation on cup | 68 (total hip | CT assessed | Mean PT | Supine>Standing, |
| orientation in both supine and | arthroplasty | PT pre- | standing: -1.6° | significant | ||
| standing positions | patients; 25M/43F) | and post- operatively in | SD 8.3°, supine: 3.1° SD 8.1° | (P<0.05) | ||
| standing and | ||||||
| supine |
PT: Pelvic tilt, SD: Standard deviation, MRI: Magnetic resonance imaging, CT: Computed tomography, F: Female, M: Male, THA: Total hip arthroplasty, Degenerative disc disease, SI: Sacroiliac.
Figure 5 showed an asymmetrical funnel plot for lumbar lordosis, suggesting a low sample size or publication bias in the studies. The forest plot for lumbar lordosis Figure 6 showed a P-value of P = 0.33 for the overall effect, indicating an insignificant difference in standing and supine position for the LL angle. Figure 7 showed a symmetrical funnel plot for the SS, suggesting minimal publication bias and indicating that the sample size across studies is sufficient. The forest plot for the SS Figure 8 showed a P-value of P < 0.00001 for the overall effect, indicating significant differences in standing and supine position for the SS angle. Figure 9 showed a mild asymmetrical funnel plot for PI, suggesting a low sample size or publication bias in the studies. The forest plot for PI Figure 10 showed a P-value of P = 0.007 for the overall effect, indicating significant differences in standing and supine position for PI angle. Figure 11 showed an asymmetrical funnel plot for PT, suggesting a low sample size or publication bias in the studies. The forest plot for PT Figure 12 showed a P-value of P = 0.18 for the overall effect, indicating that there are no significant differences in standing and supine position for PT angle.
![Funnel plot of lumbar lordosis. X-axis: Mean difference (MD) between the two groups, Y-axis: Standard error of mean difference [SE(MD)], Blue line: Line of no effect, indicating no significant difference between the groups. Circle on the plot: Study included in the meta-analysis. Position of the circle along X-axis indicates the mean difference found in that study, and the distance of the circle from the line of no effect represents the standard error of that mean difference.](/content/136/2025/9/1/img/JMSR-9-011-g005.png)
- Funnel plot of lumbar lordosis. X-axis: Mean difference (MD) between the two groups, Y-axis: Standard error of mean difference [SE(MD)], Blue line: Line of no effect, indicating no significant difference between the groups. Circle on the plot: Study included in the meta-analysis. Position of the circle along X-axis indicates the mean difference found in that study, and the distance of the circle from the line of no effect represents the standard error of that mean difference.
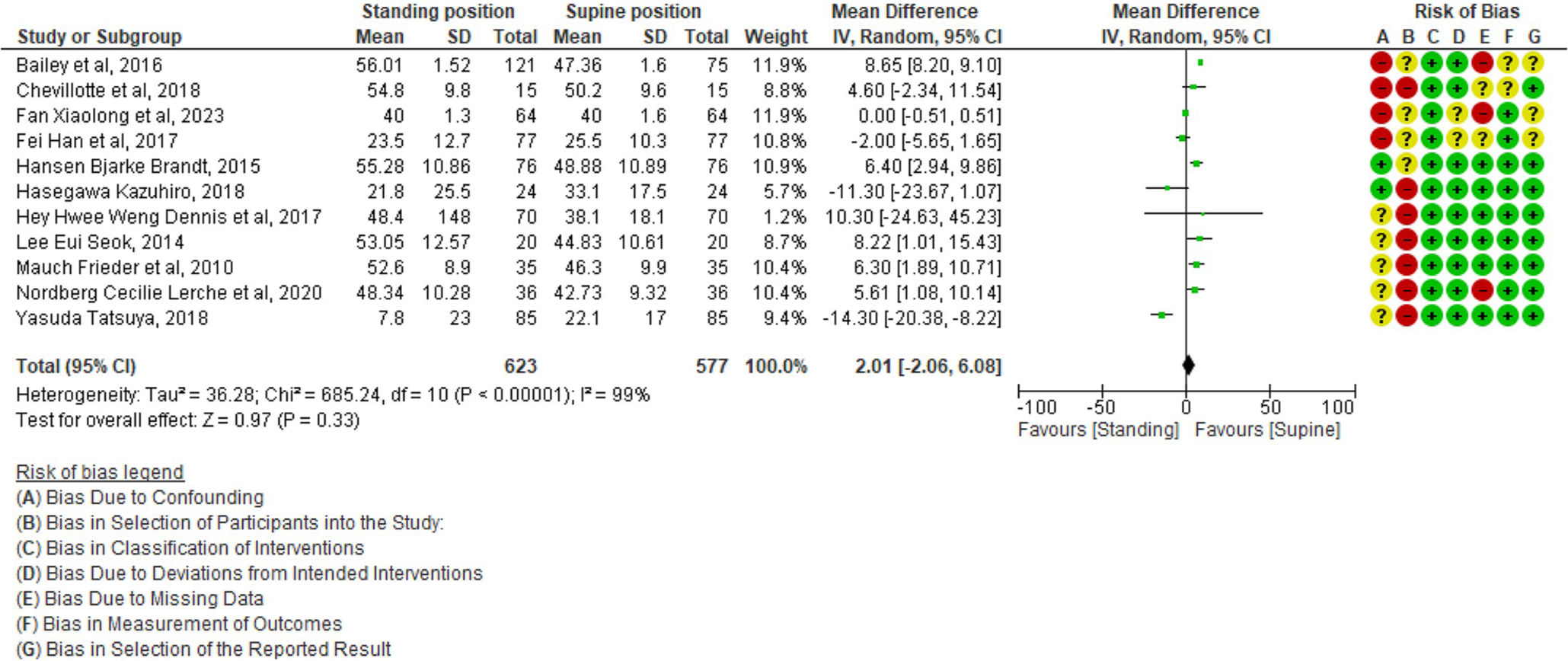
- Forest plot of lumbar lordosis. SD: Standard deviation, IV: Inverse variance, CI: Confidence interval, df: Degrees of freedom Tau2: Measures between-study heterogeneity, Chi2: Statistical test for heterogeneity, I2: Percentage of variation due to heterogeneity, Z: Overall effect of intervention, green circles with plus signs: Low risk of bias, red circles with minus signs: High risk of bias, yellow circles with question marks: Unclear risk of bias.
![Funnel plot of sacral slope. X-axis: Mean difference (MD) between the two groups, Y-axis: Standard error of mean difference [SE(MD)], Blue line: Line of no effect, indicating no significant difference between the groups. Circle on the plot: Study included in the meta-analysis. Position of the circle along X-axis indicates the mean difference found in that study, and the distance of the circle from the line of no effect represents the standard error of that mean difference.](/content/136/2025/9/1/img/JMSR-9-011-g007.png)
- Funnel plot of sacral slope. X-axis: Mean difference (MD) between the two groups, Y-axis: Standard error of mean difference [SE(MD)], Blue line: Line of no effect, indicating no significant difference between the groups. Circle on the plot: Study included in the meta-analysis. Position of the circle along X-axis indicates the mean difference found in that study, and the distance of the circle from the line of no effect represents the standard error of that mean difference.
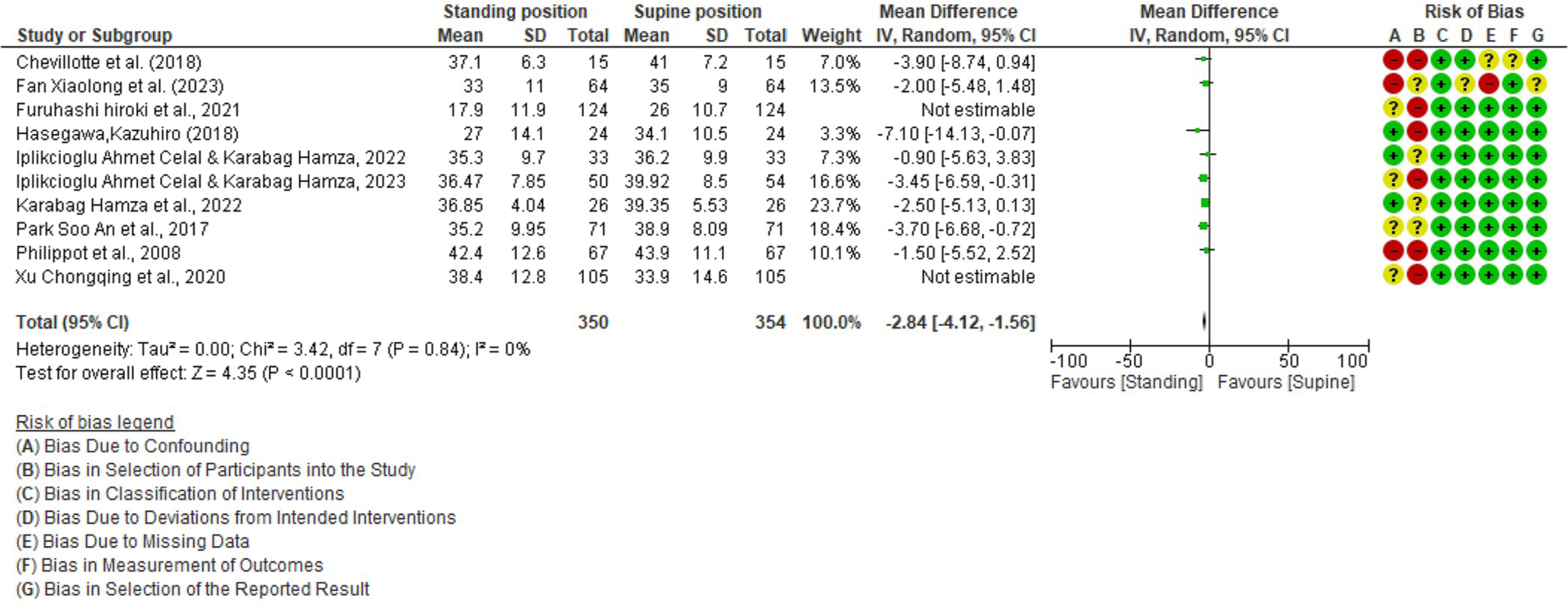
- Forest plot of sacral slope. SD: Standard deviation, IV: Inverse variance, CI: Confidence interval, df: Degrees of freedom Tau2: Measures between-study heterogeneity, Chi2: Statistical test for heterogeneity, I2: Percentage of variation due to heterogeneity, Z: Overall effect of intervention, green circles with plus signs: Low risk of bias, red circles with minus signs: High risk of bias, yellow circles with question marks: Unclear risk of bias.
![Funnel plot of pelvic incidence. X-axis: Mean difference (MD) between the two groups, Y-axis: Standard error of mean difference [SE(MD)], Blue line: Line of no effect, indicating no significant difference between the groups. Circle on the plot: Study included in the meta-analysis. Position of the circle along X-axis indicates the mean difference found in that study, and the distance of the circle from the line of no effect represents the standard error of that mean difference.](/content/136/2025/9/1/img/JMSR-9-011-g009.png)
- Funnel plot of pelvic incidence. X-axis: Mean difference (MD) between the two groups, Y-axis: Standard error of mean difference [SE(MD)], Blue line: Line of no effect, indicating no significant difference between the groups. Circle on the plot: Study included in the meta-analysis. Position of the circle along X-axis indicates the mean difference found in that study, and the distance of the circle from the line of no effect represents the standard error of that mean difference.
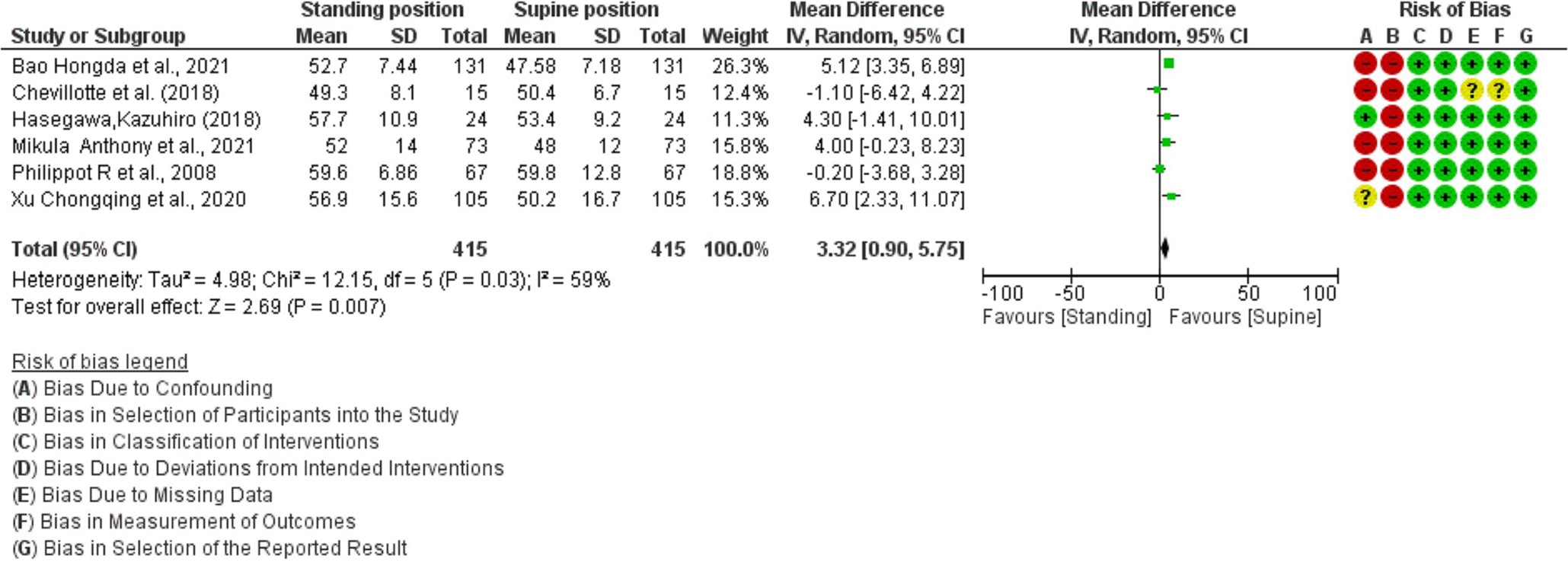
- Forest plot of pelvic incidence. SD: Standard deviation, IV: Inverse variance, CI: Confidence interval, df: Degrees of freedom Tau2: Measures between-study heterogeneity, Chi2: Statistical test for heterogeneity, I2: Percentage of variation due to heterogeneity, Z: Overall effect of intervention, green circles with plus signs: Low risk of bias, red circles with minus signs: High risk of bias, yellow circles with question marks: Unclear risk of bias.
![Funnel plot of pelvic tilt. X-axis: Mean difference (MD) between the two groups, Y-axis: Standard error of mean difference [SE(MD)], Blue line: Line of no effect, indicating no significant difference between the groups. Circle on the plot: Study included in the meta-analysis. Position of the circle along X-axis indicates the mean difference found in that study, and the distance of the circle from the line of no effect represents the standard error of that mean difference.](/content/136/2025/9/1/img/JMSR-9-011-g011.png)
- Funnel plot of pelvic tilt. X-axis: Mean difference (MD) between the two groups, Y-axis: Standard error of mean difference [SE(MD)], Blue line: Line of no effect, indicating no significant difference between the groups. Circle on the plot: Study included in the meta-analysis. Position of the circle along X-axis indicates the mean difference found in that study, and the distance of the circle from the line of no effect represents the standard error of that mean difference.
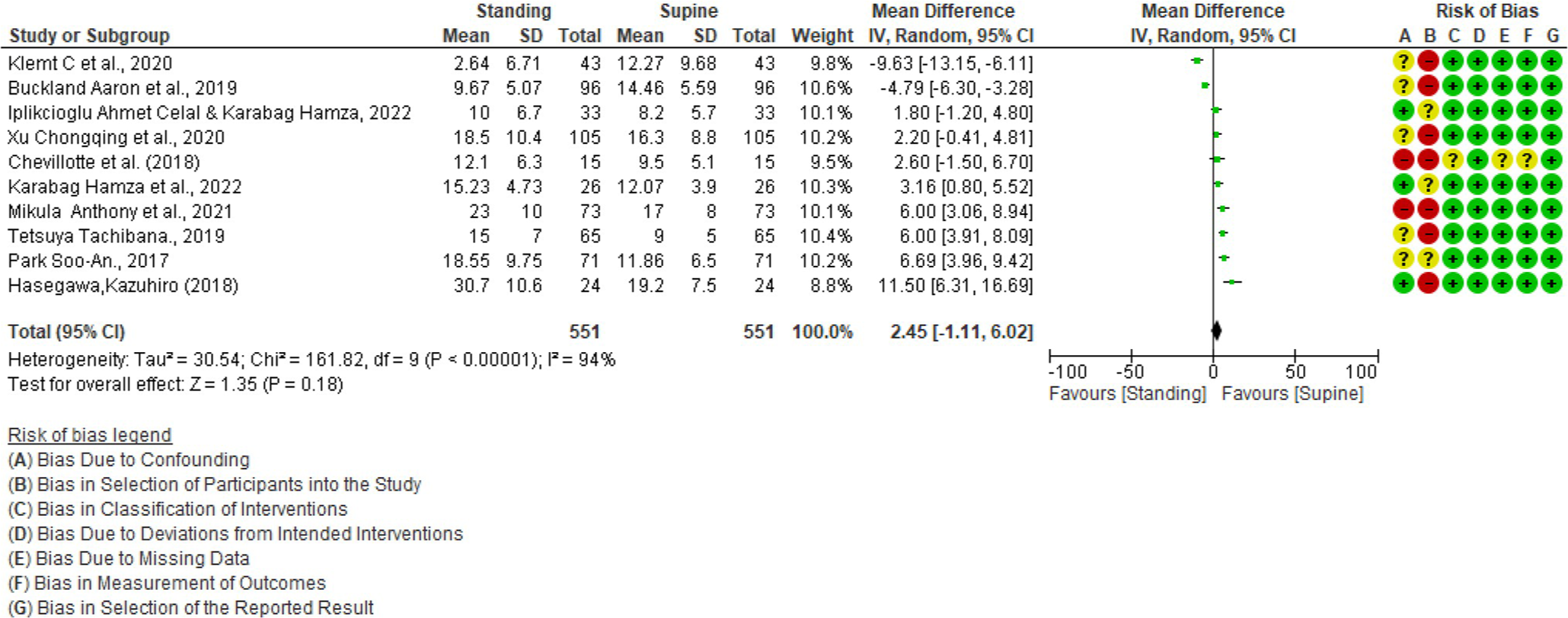
- Forest plot of pelvic tilt. SD: Standard deviation, IV: Inverse variance, CI: Confidence interval, df: Degrees of freedom Tau2: Measures between-study heterogeneity, Chi2: Statistical test for heterogeneity, I2: Percentage of variation due to heterogeneity, Z: Overall effect of intervention, green circles with plus signs: Low risk of bias, red circles with minus signs: High risk of bias, yellow circles with question marks: Unclear risk of bias.
DISCUSSION
The lumbar spine, sacrum, pelvis, and hip joint are all part of one unit. Any change in body posture or movement will alter the position of the lumbar, sacrum, pelvis, and hip joints, influencing the biomechanics and forces that occur in the structures listed above. There are anatomical parameters in the form of angular measurements formed from various aspects of the relationship between the structures above which are known as Spinopelvic Parameters.[28] The positional parameters indicate the extent of pelvic rotation around the hip axis, with SS being a commonly used measurement followed by other spinopelvic parameters, namely PI, PT, and LL.[29] Understanding these parameters is essential, as they help determine the spinopelvic region’s overall balance and biomechanical functionality.[28]
The observed differences in spinopelvic parameters between supine and standing positions are clinically significant, particularly in the context of surgical planning for spinal deformity correction. Standing parameters more accurately reflect the natural load-bearing alignment of the spine, which is crucial for planning surgeries that aim to restore sagittal balance. Relying solely on supine measurements may underestimate deformities or misrepresent spinal alignment, potentially leading to suboptimal surgical outcomes. Furthermore, these differences could influence post-surgical prognosis, as achieving proper sagittal balance is associated with improved functional outcomes and reduced pain. Sagittal plane imbalance is a recognized cause of pain and disability, and its correction is a primary goal in many spinal surgeries.[3] Clinically, these findings highlight the importance of pre-operative assessments that account for both supine and standing positions to optimize surgical planning and long-term prognosis. The increasing prevalence of concurrent hip and spinal pathologies underscores the need for a comprehensive understanding of spinopelvic mobility in surgical planning.[30] Accurate measurement of these parameters is essential, and studies have explored the validity and reliability of different imaging modalities in assessing spinopelvic alignment.[4]
The LL angle is defined as the angle formed between the superior endplate of the second lumbar vertebra (L2) and the superior endplate of the sacrum (S1), as observed in the mid-sagittal imaging.[9] A normal lordotic curve is characterized by an average lumbosacral angle of 39°–53°. This natural curve of the spine’s lower back (lumbar) area is essential for maintaining proper posture and spinal alignment. The degree of LL is affected by various factors, including lumbar and pelvic anatomy, as well as thoracic kyphosis, which can typically exceed LL by approximately 30°.[31] The LL angle is classified according to the Roussouly sagittal classification system, which delineates four types based on the orientation of the SS. Types 1 and 2 are characterized by an SS of <35°, type 3 has an SS between 35° and 45°, and type 4 is defined by an SS >45°. Typically, PI is lower in types 1 and 2, while it is higher in type 3. In type 1, the apex of the LL is located at the center of the L5 vertebral body. In type 2, the apex is at the base of the L4 vertebral body. In type 3, the apex is located at the center of the L4 vertebral body, and in type 4, it is either at the center of the L4 vertebral body or higher.[32] Other classifications of LL are categorized depending on the PI into hypolordotic, normal lordotic, or hyperlordotic.[33] Loss of lordotic curve/hypolordotic is a condition in which the natural inward curve in the lower back, also known as LL, is reduced or eliminated. This may be attributed to various factors, including lumbar spine fusion, which can contribute to chronic low back pain, a positive sagittal balance with forward inclination of the trunk, and degeneration of adjacent segments.[34] On the other hand, a hyperlordotic curve is a condition where the LL is exaggerated, causing the lower back spine to curve excessively inward. Hyperlordosis can result from various factors, including being overweight, which can contribute to the transition from a normal curve to a hyperlordotic one.[35]
The SS angle is a crucial parameter in understanding the alignment and positioning of the pelvis and spine. It is defined as the angle between the superior endplate of the sacrum (S1) and a horizontal line.[36,37] The SS and PT are directly associated with the PI angle, which is the algebraic sum of these two angles.[38] The importance of the SS angle lies in its influence on lumbar curvature and its relationship with various spinopelvic parameters.[39,40] Since the SS is a position-dependent parameter, it can be affected by different factors, resulting in changes to the overall spinal alignment and posture. Numerous factors can affect the SS angle, including anatomical variations, age, and certain medical conditions. Some primary factors responsible for deformity or changes in the SS angle are osteoporosis, trauma, infection, and iatrogenic factors.[37] Anatomical variations, such as the presence of developmental dysplasia of the hip, can also significantly impact the SS angle.[40]
Various measurement techniques can be utilized to assess the SS angle accurately. One effective technique entails drawing a tangent line to the upper S1 endplate and a horizontal line; the angle between these lines indicates the SS.[41] Another approach referred to as the anatomical SS, assesses the angle between the superior endplate of S1 and a horizontal reference line, independent of the measurement of femoral head centers.[36,40] The SS not only affects LL but also significantly contributes to spinal stability. A study examining the impact of SS on the biomechanical responses of the lumbar spine observed that variations in the SS can result in directional biomechanical changes in the shape of the L5-S1 disc. These changes can affect the spine’s stability, particularly in the lower lumbar region.[42]
The PI angle is a crucial anatomical parameter that facilitates consistent analysis of the pelvis in the sagittal plane.[38,43] This angle is the benchmark pelvic parameter and is utilized to categorize spinal configurations into Roussouly types.[44] PI is defined as the angle formed between a line perpendicular to the sacral plate’s midpoint and a line extending from that same midpoint to the hip axis.[45] The PI angle’s importance lies in its ability to provide valuable insight into an individual’s spinal alignment and potential predisposition to spinal disorders. The PI angle can be measured through various techniques, such as CT.[46] The algebraic sum of two complementary angles determines the angle: PT and SS.[38] The clinical significance of PI in spinal pathologies lies in its importance as a critical component in the analysis of sagittal balance.[47] PI, also known as the pelvisacral angle, is defined as the angle formed between the line perpendicular to the midpoint of the sacral plate and the line connecting this point to the hip axis.[45] In the context of spinal surgery, PI has emerged as one of the key sagittal parameters.[43] Assessing the pelvic axis and PI is of primary importance to planning an appropriate treatment regimen for symptomatic ASD.[48]
The PT is an essential component in comprehending the body’s alignment and posture as it pertains to the spatial orientation or movement of the pelvis relative to the rest of the body in the sagittal plane. There are two primary types of PT: Anterior and posterior. Anterior PT is observed when the anterior superior iliac spine is positioned lower than the posterior superior iliac spine (PSIS) in the sagittal plane, or when it rotates inferiorly in relation to the PSIS.[49] This condition is often caused by excessive sitting or a lack of physical activity, and it can impact posture and the spine’s shape. On the other hand, a posterior PT is characterized by a posterior rotation of the innominates, resulting in a flat back appearance. The consequences of PT on overall body posture and health cannot be overlooked, as this postural deviation can lead to various issues. A tilted pelvis can cause imbalance and misalignment of the spine, which may result in low back pain and poor posture. Furthermore, high PT can serve as a compensatory mechanism, affecting the apparent alignment of the spine and potentially masking underlying spinal deformities.[50] It has also been suggested that imbalances in PT are a significant factor in low back pain.[51]
The lumbar disc, sacrum, pelvis, and hip joint anatomical structures are intricately related, with each component playing a crucial role in maintaining spinal alignment and stability.[52] As we age, degenerative processes take place within these structures, causing changes in the measurements of spinopelvic parameters. For instance, the LL and SS may decrease, while the PT and sagittal vertical axis may increase in older patients.[53] This decline in LL often leads to a compensatory increase in PT, allowing individuals to maintain sagittal balance despite the degenerative changes.[54] Consequently, the impact of the degenerative process on spinopelvic measurements must be considered when assessing spinal alignment and planning interventions, such as spinal surgery.[55]
One widely employed method for assessing spinopelvic parameters is the use of standard lumbosacral radiographs. Typically, these radiographs are performed with the patient standing, although in certain cases, they may be done with the patient lying down to ensure their comfort. Another examination option is a 3D lumbosacral CT Scan, which is typically conducted with the patient in a supine position.[5] In numerous hospitals, the option of standing CT scans is not widely accessible, and in Indonesia, particularly, there is a lack of CT scans designed to accommodate the standing position.
The lack of access to standing CT scans is not unique to Indonesia but is a challenge many developing countries face. In such settings, clinicians often rely on supine imaging, which may not fully capture the functional alignment of the spine. This limitation can affect surgical planning and clinical decision-making, as the inability to assess spinopelvic parameters in a weight-bearing position could lead to an underestimation of spinal deformities.[56] The findings of this study are highly relevant to these regions, as they underscore the importance of considering alternative strategies for evaluating spinopelvic parameters when standing CT is unavailable. Clinicians in developing countries may need to combine supine imaging with functional assessments, such as physical examination or radiographs, to approximate standing parameters and improve patient outcomes. Typically, standing position CT scans are primarily found in research centers, especially those focused on investigating the biomechanics of the human body in various anatomical positions, including standing position.
After conducting a thorough systematic review, we discovered notable variations in the spinopelvic elements when comparing standing and supine positions, particularly in PI and SS. Conversely, we found no substantial disparity in LL and PT measurements between the two positions.
Patients with significant lumbar disc degeneration and low back pain tend to exhibit reduced lordosis in both the supine and standing positions. However, our analysis found no significant difference between these two positions for LL.[9] Another study discovered that when degenerative lumbar scoliosis patients were positioned from standing to supine, the LL rose somewhat but not significantly.[8] One study indicates that supine MRI can be effectively translated into sagittal alignment angle values obtained from standing radiographs, achieving an acceptable level of accuracy for patients with degenerative lumbar conditions.[7]
The differences in spinopelvic parameter measurements in the standing and supine positions will be of particular concern in measuring the forces that occur, especially in research that uses 3D CT scan data. Finite element analysis (FEA) is a computational method used to predict a body’s behavior under various load and boundary conditions. This technique is particularly useful in studying spinal biomechanics, as it allows researchers to develop detailed models of the spine and surrounding structures using data from CT scans.[57] In the context of spinopelvic parameters, FEA can provide valuable insights into the complex relationships between spinal curvature, pelvic orientation, and leg position, which are all factors that can influence an individual’s spinal alignment and overall postural stability.[58] One of the primary challenges in spinopelvic parameter measurement is accounting for the differences in spinal alignment between the supine and standing positions. FEA can be employed to address this issue by adjusting angles within the analysis process to account for the observed discrepancies. For example, the following angle adjustments can be made to improve the accuracy of spinopelvic parameter measurements: Adjusting the LL angle to account for differences in sagittal spinal curvature between supine and standing positions; Modifying the SS angle to represent better the relationship between the sacrum and pelvis in different postures;[59] Altering the PT and PI angles to reflect changes in pelvic orientation due to variations in hip and leg positions.[58] By incorporating these angle adjustments into the FEA process, researchers can generate more accurate representations of spinopelvic parameters in both standing and supine positions, ultimately enhancing the clinical utility of this powerful analytical tool.
Aside from LL, the spinopelvic parameter PT also did not exhibit any significant changes. PT is a component of the spinopelvic parameter that is related to the position of the pelvis and is ultimately related to the position of the hip joint. Despite the differences in lumbar curvature due to changes in body position, there is no significant difference in the angle of the pelvis when lying on the back (supine) or standing. This can be attributed to the fact that the spatial position or motion of the pelvis in the sagittal plane remains relatively stable, regardless of the rest of the body’s position.[49] As a result, while lumbar curvature and PT angles may vary between body positions, the overall impact on the angle that occurs in the pelvis remains minimal.
The body has a compensation mechanism for axial load distribution by concentrating the load at a central point in front of the promontory, which will remain static even if there is a change in a person’s LL angle. A study from CT data from 28 asymptomatic individuals revealed that for each degree increase in LL, there was a corresponding decrease in the compressive force within the intervertebral disc between the L5 vertebra and the sacrum by 2.8 N, suggesting that a more pronounced lumbar curvature could mitigate the compressive stresses on spinal structures.[60] In this context, while some studies report significant differences in LL between lying and standing positions, our analysis indicates that these differences are not statistically significant, especially given the older patient population. In other words, although the LL angle may appear to vary between positions, the functional implications on force distribution, particularly on the hip joint, remain minimal.
In other words, although there are significant differences in the LL angle in the lying and standing positions, relatively constant results will be obtained when measuring the force distribution, especially the force acting on the hip joint.
According to the various explanations above, despite significant differences in measuring several aspects of spinopelvic parameters, 3D lumbosacral CT scan data obtained in the supine position can still be utilized to measure forces, particularly in the hip joint and lower extremities.
Several limitations must be considered when interpreting the results of this meta-analysis. First, there were notable differences in the study populations, including variations in age, underlying spinal conditions, and body mass index, which may have influenced the observed spinopelvic parameters. In addition, differences in methodologies, such as the type of imaging used (radiographs vs. CT scans) and the positioning protocols during supine and standing assessments, may have introduced measurement variability. These heterogeneities across studies likely contributed to the high I2 value, indicating substantial variability between study results.
Furthermore, The asymmetrical funnel plots observed for LL, SS, PI, and PT parameters suggest potential publication bias, which is typical in meta-analyses. This bias occurs when studies with significant findings are more likely to be published, potentially leading to overestimating the true effect size. While this bias is difficult to eliminate entirely, future studies could apply regression meta-analysis.
In addition, language restrictions and the exclusion of non-English studies may limit the thoroughness of this review. While subgroup analyses based on variables such as age, sex, or the presence of spinal pathologies (e.g., lumbar disc degeneration) would offer a more nuanced understanding of the factors influencing spinopelvic parameters, the data available in the included studies did not permit such detailed analyses. To enhance the comprehensiveness of future reviews, it is recommended that subgroup analyses be conducted to examine variability across studies and that research published in other languages be incorporated.
CONCLUSION
In this comprehensive study, assessments of SS and PI differed significantly between standing and supine postures. Meanwhile, when measuring the LL and PT of normal patients and the spinopelvic parameters of patients with degenerative lumbar disease, no significant differences were found between the standing and supine positions, indicating that a CT scan in the supine position can accurately describe the patient’s condition. However, the clinical importance of standing measurements in surgical planning cannot be overlooked, as they more accurately reflect the spine’s load-bearing alignment. Relying solely on supine measurements may underestimate deformities, potentially leading to suboptimal outcomes. These findings are particularly relevant for regions where standing CT scans are unavailable. Future research should focus on developing alternative methods, such as combining supine imaging with functional assessments, to approximate standing parameters and improve clinical decision-making in resource-limited settings.
AUTHORS’ CONTRIBUTION
AP, AS, JJ, and TW: Conducted research and conceived and designed the study. AP: Provided research materials and collected and organized data. AP and DN: Analyzed and interpreted data. DN: Wrote the initial and final draft of the article and provided logistic support. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
Institutional Review Board approval is not required.
DECLARATION OF PATIENT CONSENT
Patient’s consent is not required, as there are no patients in this study.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The AI tool available at https://goblin.tools/Formalizer has been utilized in this study to enhance the formality of the text and reduce grammatical errors.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Measurement of spinopelvic parameters in healthy adults of Indian origin-A cross sectional study. J Clin Orthop Trauma. 2020;11:883-8.
- [CrossRef] [PubMed] [Google Scholar]
- Sacrum morphometry and spinopelvic parameters among the Indonesian population using computed tomography scans. Medicine (Baltimore). 2021;100:e27955.
- [CrossRef] [PubMed] [Google Scholar]
- The Role of spinopelvic parameters in clinical outcomes of spinal osteotomies in patients with sagittal imbalance. Arch Bone Jt Surg. 2018;6:324-30.
- [Google Scholar]
- Determining the validity and reliability of spinopelvic parameters through comparing standing whole spinal radiographs and upright computed tomography images. BMC Musculoskelet Disord. 2021;22:899.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of posture on relationships between pelvic parameters and lumbar lordosis: Comparison of the standing, seated, and supine positions. A preliminary study. Orthop Traumatol Surg Res. 2018;104:565-8.
- [CrossRef] [PubMed] [Google Scholar]
- Morphological and postural sexual dimorphism of the lumbar spine facilitates greater lordosis in females. J Anat. 2016;229:82-91.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of sagittal spinal alignment on standing plain x-rays and supine MRI in degenerative lumbar disease. Front Surg. 2023;10:1103952.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of patient position on the lordosis and scoliosis of patients with degenerative lumbar scoliosis. Medicine (Baltimore). 2017;96:e7648.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of lumbar disc degeneration and low-back pain on the lumbar lordosis in supine and standing: A cross-sectional MRI study. Spine (Phila Pa 1976). 2015;40:1690-6. Accessed 2024-07-05
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Difference in whole spinal alignment between supine and standing positions in patients with adult spinal deformity using a new comparison method with slot-scanning three-dimensional X-ray imager and computed tomography through digital reconstructed radiography. BMC Musculoskelet Disord. 2018;19:437.
- [CrossRef] [PubMed] [Google Scholar]
- Lumbar spine alignment in six common postures: An ROM analysis with implications for deformity correction. Spine (Phila Pa 1976). 2017;42:1447-55.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of age on sagittal plane profile of the lumbar spine according to standing, supine, and various sitting positions. J Orthop Surg Res. 2014;9:11.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in the lumbar spine of athletes from supine to the true-standing position in magnetic resonance imaging. Spine. 2010;35:1002-7.
- [CrossRef] [PubMed] [Google Scholar]
- Positional changes in lumbar disc herniation during standing or lumbar extension: A cross-sectional weight-bearing MRI study. Eur Radiol. 2021;31:804-12.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of position on lumbar lordosis in patients with adult spinal deformity. J Neurosurg Spine. 2018;29:530-4.
- [CrossRef] [PubMed] [Google Scholar]
- Validity and reliability of spinopelvic parameters measured on computed tomography. Int J Spine Surg. 2022;16:875-80.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior pubic incidence: A novel morphologic spinopelvic parameter nearly equal to pelvic incidence. World Neurosurg. 2023;172:e100-6.
- [CrossRef] [PubMed] [Google Scholar]
- Pelvic incidence measurement with supine magnetic resonance imaging: A validity and reliability study. Clin Neurol Neurosurg. 2022;222:107424.
- [CrossRef] [PubMed] [Google Scholar]
- Changes of spinopelvic parameters in different positions. Arch Orthop Trauma Surg. 2017;137:1223-32.
- [CrossRef] [PubMed] [Google Scholar]
- Pelvic balance in sagittal and Lewinnek reference planes in the standing, supine and sitting positions. Orthop Traumatol Surg Res. 2009;95:70-6.
- [CrossRef] [PubMed] [Google Scholar]
- Position-related change of pelvic incidence depends on the nonfused sacroiliac joint in patients with degenerative spinal diseases. Spine (Phila Pa 1976). 2021;46:796-802.
- [CrossRef] [PubMed] [Google Scholar]
- Change in pelvic incidence between the supine and standing positions in patients with bilateral sacroiliac joint vacuum signs. J Neurosurg Spine. 2021;34:617-22.
- [CrossRef] [PubMed] [Google Scholar]
- Correlation and differences in lumbopelvic sagittal alignment parameters between lumbar radiographs and magnetic resonance images. Global Spine J. 2022;12:79-84.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of sagittal spinal alignment on postural pelvic mobility in total hip arthroplasty candidates. J Arthroplasty. 2019;34:2663-8.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of postural changes on in vivo pelvic tilt and functional component anteversion in total hip arthroplasty patients with lumbar disc degenerations. Bone Joint J. 2020;102:1-7.
- [CrossRef] [PubMed] [Google Scholar]
- Does acetabular coverage vary between the supine and standing positions in patients with hip dysplasia? Clin Orthop Relat Res. 2019;477:2455-66.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of pelvic tilt and rotation on cup orientation in both supine and standing positions. J Arthroplasty. 2018;33:1442-8.
- [CrossRef] [PubMed] [Google Scholar]
- From the spinopelvic parameters to global alignment and proportion scores in adult spinal deformity. Neurospine. 2023;20:467-77.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of spinopelvic parameters in patients with lumbosacral transitional vertebra: A cross sectional and comparative study. Am J Neurodegener Dis. 2023;12:123-32.
- [Google Scholar]
- The impact of spinopelvic mobility on arthroplasty: Implications for hip and spine surgeons. J Clin Med. 2020;9:2569.
- [CrossRef] [PubMed] [Google Scholar]
- Spine sagittal balance In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024.
- [Google Scholar]
- Radiological analysis of upper lumbar disc herniation and spinopelvic sagittal alignment. Eur Spine J. 2016;25:1382-8.
- [CrossRef] [PubMed] [Google Scholar]
- Optimal lumbar lordosis correction for adult spinal deformity with severe sagittal imbalance in patients over age 60: Role of pelvic tilt and pelvic tilt ratio. Spine (Phila Pa (1976). 2021;46:E1246-53.
- [CrossRef] [PubMed] [Google Scholar]
- Current strategies for the restoration of adequate lordosis during lumbar fusion. World J Orthop. 2015;6:117-26.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of William training on lumbosacral muscles function, lumbar curve and pain. J Back Musculoskelet Rehabil. 2015;28:591-7.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomical sacral slope, a new pelvic parameter, is associated with lumbar lordosis and pelvic incidence in healthy Japanese women: A retrospective cross-sectional study. J Orthop Surg (Hong Kong). 2020;28
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of intervertebral disc prostheses. Diagn Interv Imaging. 2012;93:10-21.
- [CrossRef] [PubMed] [Google Scholar]
- Pelvic parameters: Origin and significance. Eur Spine J. 2011;20(Suppl 5):564-71.
- [CrossRef] [PubMed] [Google Scholar]
- A study on difference and importance of sacral slope and pelvic sacral angle that affect lumbar curvature. Technol Health Care. 2014;22:467-72.
- [CrossRef] [PubMed] [Google Scholar]
- Correlation of the anatomical sacral slope with pelvic incidence in female patients with developmental hip dysplasia: A retrospective cross-sectional study. J Orthop Surg Res. 2020;15:486.
- [CrossRef] [PubMed] [Google Scholar]
- The role of sacral slope in the progression of a bilateral spondylolytic defect at L5 to spondylolisthesis: A biomechanical investigation using finite element analysis. Global Spine J. 2018;8:460-70.
- [CrossRef] [PubMed] [Google Scholar]
- Pelvic incidence variation among individuals: Functional influence versus genetic determinism. J Orthop Surg Res. 2018;13:59.
- [CrossRef] [PubMed] [Google Scholar]
- Pelvic index: A new pelvic parameter for assessing sagittal spinal alignment. N Am Spine Soc J. 2023;16:100274.
- [CrossRef] [PubMed] [Google Scholar]
- Sagittal spinal alignment in asymptomatic patients over 30 years old in the Korean population. Acta Neurochir (Wien). 2017;159:1119-28.
- [CrossRef] [PubMed] [Google Scholar]
- Description of a new method of measuring the pelvic incidence angle through computed tomography. Coluna Columna. 2020;19:30-3.
- [CrossRef] [Google Scholar]
- How do pelvic parameters correlate with postoperative outcomes when the parameters are not measured preoperatively in patients undergoing instrumented lumbar fusion? Cureus. 2021;13:e16885.
- [CrossRef] [Google Scholar]
- The impact of preoperative supine radiographs on surgical strategy in adult spinal deformity. J Neurosurg Spine. 2022;36:71-7.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical measures of pelvic tilt in physical therapy. Int J Sports Phys Ther. 2021;16:1366-75.
- [CrossRef] [PubMed] [Google Scholar]
- Radiographic assessment of the spine In: Spine secrets plus. Netherlands: Elsevier Health Sciences; 2012. p. :70-9.
- [CrossRef] [Google Scholar]
- Effects of pelvic-tilt imbalance on disability, muscle performance, and range of motion in office workers with non-specific low-back pain. Healthcare (Basel). 2023;11:893.
- [CrossRef] [PubMed] [Google Scholar]
- From the spinopelvic parameters to global alignment and proportion scores in adult spinal deformity. Neurospine. 2023;20:467-77.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between paravertebral muscle degeneration and spinal-pelvic sagittal parameters in patients with lumbar disc herniation. Sci Rep. 2024;14:192.
- [CrossRef] [PubMed] [Google Scholar]
- Spinopelvic parameters: Lumbar lordosis, pelvic incidence, pelvic tilt, and sacral slope: What does a spine surgeon need to know to plan a lumbar deformity correction? Neurosurg Clin N Am. 2018;29:323-9.
- [CrossRef] [PubMed] [Google Scholar]
- Pelvic incidence variation among individuals: Functional influence versus genetic determinism. J Orthop Surg Res. 2018;13:59.
- [CrossRef] [PubMed] [Google Scholar]
- Turning a blind eye: The mobilization of radiology services in resource-poor regions. Global Health. 2010;6:18.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical implications of spinopelvic alignment on femoral head cartilage and the proximal femoral physis in slipped capital femoral epiphysis: A theoretical finite element analysis. bioRxiv [Preprint]; 2024
- [CrossRef] [Google Scholar]
- Spinal balance/alignment-clinical relevance and biomechanics. J Biomech Eng. 2019;141:70805.
- [CrossRef] [PubMed] [Google Scholar]
- Spinopelvic alignment in patients with osteoarthrosis of the hip: A radiographic comparison to patients with low back pain. Spine (Phila Pa 1976). 2005;30:1650-7.
- [CrossRef] [PubMed] [Google Scholar]
- Load distribution in the lumbar spine during modeled compression depends on lordosis. Front Bioeng Biotechnol. 2021;9:661258.
- [CrossRef] [PubMed] [Google Scholar]






