Translate this page into:
Analyzing the immediate and carryover effects of neurodynamics on straight leg raise ranges among acute prolapsed intervertebral disc patients: A randomized control double-blind study
*Corresponding author: Ashwani Bhat, Department of Neurology, Himalayan Institute of Medical Sciences, SRHU, Dehradun, Uttarakhand, India. dr.ashwanibhat@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bahuguna D, Agarwal V, Bhat A, Pandey S. Analyzing the immediate and carryover effects of neurodynamics on straight leg raise ranges among acute prolapsed intervertebral disc patients: A randomized control double-blind study. J Musculoskelet Surg Res. 2024;8:272-80. doi: 10.25259/JMSR_222_2023
Abstract
Objectives:
Prolapsed intervertebral disc (PIVD) is a disease that occurs when the annulus fibrosus ruptures, which leads to an effusion of the nucleus pulposus. The straight leg raise (SLR) test is a neurological test that is used in the physical examination of patients with low back pain to ascertain whether the sciatic nerve has been affected due to irritation of the lumbosacral nerve root. The discomfort or pain caused by sciatic nerve compression can be significantly reduced by neurodynamic mobilization, which lowers inflammatory mediators. The study aimed to analyze the neurodynamic exercises’ immediate and carryover effects, including the static opener and four levels of sliders and tensioners on SLR ranges among acute PIVD patients.
Methods:
A total of 44 subjects with acute PIVD were randomly assigned into two groups. The experimental group (n = 22) received neurodynamics and the control group (n = 22) received conventional therapy. The outcome variables were the visual analog scale (VAS), pain site code (PSC), and SLR test, which were assessed at baseline, post-intervention, and after 72 h (carryover).
Results:
The experimental group showed positive significant effects on VAS score, PSC score, and SLR ranges, whereas the control group showed immediate effects on VAS score, PSC score, and SLR ranges, but the effects were not maintained for a longer duration (72 h).
Conclusion:
Neurodynamics, including the static opener and four levels of sliders and tensioners, showed significant immediate and carryover improvement in VAS, PSC score, and SLR ranges. However, the experimental group was significantly better at improving pain, PSC score, and SLR range than the control group.
Keywords
Low back pain
Neurodynamics
Pain site code
Prolapsed intervertebral disc
Straight leg raise test
Visual analog scale
INTRODUCTION
The prolapsed intervertebral disc (PIVD) is a disease that occurs when the annulus fibrosus ruptures, which leads to an effusion of the nucleus pulposus.[1] In this disease, the posterior longitudinal ligament gives way and the disc material herniates into the spinal canal.[2] Lumbar disc herniation is a frequent condition that affects 5% of adult individuals.[3] In the world, the incidence of PIVD in males is 1.9–7.6%, and in females, it is 2.2–5.0%.[4] The majority of adult individuals are affected between the ages of 30–50. The lumbar area has a higher prevalence of this disease than any other region, with L4–L5 and L5–S1 levels having the highest prevalence. About 10% of the population is affected by this ailment, which is more prevalent among low back pain (LBP) patients.[5] The incidence of LBP with or without radiculopathy has been estimated to be 23%, with a lifetime prevalence of 60–85%.[6] The term “PIVD” refers to a process in which the nucleus pulposus moves inside the intervertebral space after the annular fibers tear, most typically in the posterior and posterolateral direction. It consists of four stages-nucleus degeneration, displacement, protrusion, and extrusion.[7]
The straight leg raise (SLR) test, also referred to as the Lasegue test, is an underlying neurological test used in the physical examination of patients with LBP with radiating symptoms to ascertain whether the sciatic nerve has been affected as a result of lumbar disc hernia.[8] A study has been conducted on the usefulness of various physical examination results.[9] It suggests that the SLR remains the gold standard test for identifying radicular symptoms.[9] Root irritation is typically considered present when the examiner elevates the affected limb and the pain is reproduced or intensified.[10] It is said to be positive when the test reproduces pain in the gluteal or lower leg region and the spine as the examiner passively lifts the affected leg with the hip in flexion and the knee in extension with ankle dorsiflexion.[8,10] The relevance given to the angle of elevation at which the pain is produced varies greatly. McIntosh and Hamilton stated in their study that Brieg and Troups suggested that <70° is clinically relevant.[10] The SLR is a more used and valuable test in differential diagnosis and identifying herniations that require surgery.[11]
Morsi et al. stated in their study that the discomfort or pain caused by sciatic nerve compression could be significantly reduced by neurodynamic mobilization, which also lowers inflammatory mediators.[12] Neurodynamics, a conservative therapeutic option treatment, is an active strategy that is beneficial from a mechanical and physiological perspective. This technique philosophy is based on the notion that the entire nervous system is an incessant structure that slides and moves and that motion is connected to vital physiological processes.[13]
The PIVD propulsion leads to compression, due to which there is compromised distal sliding of neural structures, which, in turn, poses challenges to physiotherapists in treating acute PIVD patients. There is no evidence-based study on neurodynamics exercises, including static openers and four levels of sliders and tensioners, to decrease mechanosensitivity and nerve root irritation among acute PIVD patients. This research aimed to investigate whether neurodynamic exercises, including the static opener four levels of sliders and tensioners, can significantly alter neural mobility, SLR ranges, visual analog scale (VAS), and pain side code (PSC) score.
MATERIALS AND METHODS
Study design
This study was a double-blinded experimental study.
Study population
All subjects with PIVD taken from Himalayan Hospital were considered as the study population.
Sampling
A random sampling method was performed to select the patient for the individual groups.
Sample size
The sample size was calculated using previous studies’ and outcome variables (VAS and SLR) data. Forty-four subjects were selected according to the inclusion and exclusion criteria.
Inclusion criteria
The study included acute PIVD patients (<3 months) confirmed with magnetic resonance imaging, unilateral radiculopathy, SLR ranges <70°, and age group between 20 and 60 years.
Exclusion criteria
Patients with myotomal involvement power <3, low back surgery in the past year, spondylolisthesis, spinal canal stenosis, sacroiliac joint pain, infection, tumor, and cauda equina syndrome were excluded from the study.
Outcomes variables
Passive SLR test, VAS score, and PSC were the outcome variables in the study.
PROCEDURE
Subjects meeting the inclusion and exclusion criteria were included in the study. Participants were split up into the experimental group and the control group as demonstrated in Figure 1. After collecting the demographic details, subjects were tested for VAS, PSC, and SLR as shown in Figures 2 and 3. The subjects following the inclusion criteria were included in the study.
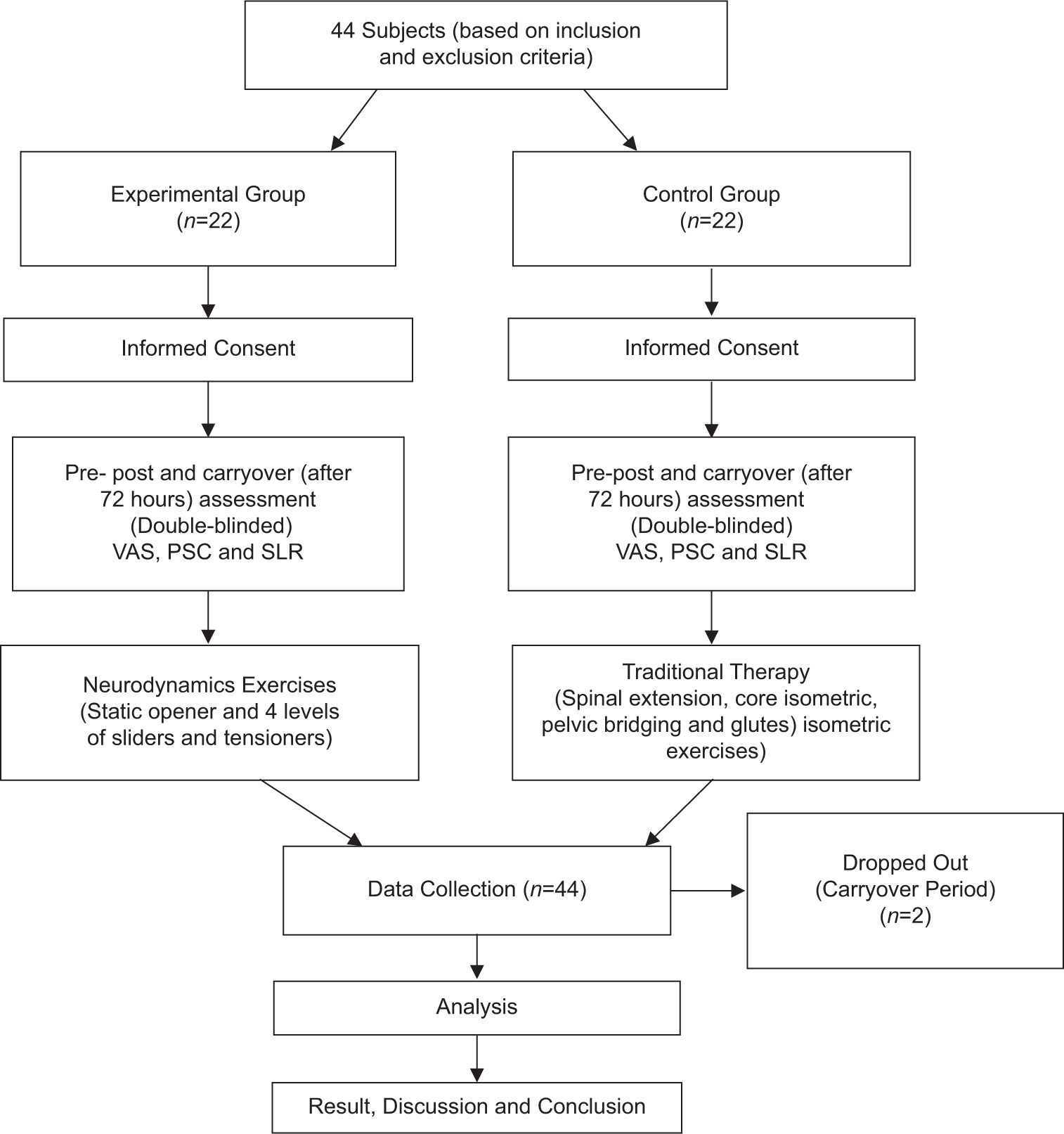
- Protocol. n: Number of participants, VAS: Visual analog scale, PSC: Pain site code, SLR: Straight leg raise.

- Testing of straight leg raise.

- Measuring of straight leg raise range.
Pre- and post-assessment was done by another therapist and the intervention was given by the researcher.
Before screening, the subjects have received a thorough description of the study’s objective.
The experimental group received a neurodynamics intervention (Static Opener and four-level neurodynamics). They were given three sets of 15–20 repetitions of four levels of neurodynamics with 1 min of static opener, including rest periods (15–20 s).
Intervention
Static opener: For 1 min [Figure 4].

- Static opener.
Four levels of neurodynamics
Position: Supine lying
Level 1: Position away→Move away [Figure 5]
- Neurodynamics level 1.
Passive neck flexion, along with hip and knee flexion
Level 2: Position toward→Move away
Neck extension along with hip and knee flexion
Level 3: Position away→Move toward neck flexion along with hip and knee extension→followed by C/L SLR→B/L SLR→Affected SLR→
Level 4: Position toward→Move toward
Neck extension along with hip and knee extension followed by C/L SLR→B/L SLR→Affected SLR [Figure 6].

- Neurodynamics level 4 (c).
Control group intervention
Spinal extension exercise, core isometric exercise, glutes isometric exercise, and pelvic bridging exercise. Three sets of 15 repetitions of each exercise were performed, including a rest period (10–15 s) [Figure 7].

- Pelvic bridging exercise.
Data analysis
Data analysis was performed using the Statistical Package for the Social Sciences (Version 20) for Windows. The mean and standard deviation (SD) for the demographic variables and outcome variables were calculated using descriptive statistics. Shapiro–Wilk test was performed to check the normality of the data. In the control group, only pre-VAS and pre-SLR followed normality in the data. Wilcoxon signed-ranks test was used to determine the difference in outcome variable scores within groups for VAS, PSC, and SLR. A paired t-test was used to determine the difference between the VAS and SLR variables in the control group as it followed normality. Mann–Whitney U-test was performed to find out the difference in scores between the groups for VAS, PSC, and SLR.
RESULTS
A total of 44 patients were enrolled in the research. Of these patients, 22 patients were enrolled in the experimental group and 22 in the control group. Among them, 20 were male and 24 were female. Two patients dropped out from the experimental group during the carryover effect period.
In the study, the M ± SD for age is 39.14 ± 9.833 and for side is 1.50 ± 0.521.
The changes in VAS, PSC, and SLR scores of the experimental group post-data are demonstrated in Table 1 using the Wilcoxon signed-rank test.
| S. No. | Variables | Pre M±SD (median) | Post M±SD (median) | P-value |
|---|---|---|---|---|
| 1. | VAS | 5.95±0.844 (6.000) | 3.68±1.129 (4.000) | <0.001 |
| 2. | PSC | 5.36±0.790 (5.500) | 3.73±1.386 (3.500) | <0.001 |
| 3. | SLR | 49.45±9.635 (54.000) | 58.18±14.608 (63.000) | 0.002 |
M: Median, SD: Standard deviation, VAS: Visual analog scale, PSC: Pain site code, SLR: Straight leg raise
In the experimental group, there was a decrease in the VAS score (P < 0.001) from 5.95 with an SD of 0.844 to the post-VAS score of 3.68 with an SD of 1.129. The PSC score was reduced from 5.36 with an SD of 0.790 to the post-PSC score of 3.73 with an SD of 1.386 (P < 0.001). The SLR score was increased from 49.45 with an SD of 9.635 to a post-SLR score of 58.18 with an SD of 14.608 (P = 0.002).
The changes in the VAS, PSC, and SLR scores in the carryover data in the experimental group are demonstrated in Table 2 using the Wilcoxon signed-rank test.
| S. No. | Variables | Post M±SD (median) | Carryover M±SD (median) | P-value |
|---|---|---|---|---|
| 1. | VAS | 3.68±1.129 (4.000) | 2.60±1.465 (2.500) | 0.002 |
| 2. | PSC | 3.73±1.386 (3.500) | 3.05±1.395 (2.500) | 0.032 |
| 3. | SLR | 58.18±14.608 (63.000) | 70.70±10.623 (72.000) | <0.001 |
M: Median, SD: Standard deviation, VAS: Visual analog scale, PSC: Pain site code, SLR: Straight leg raise
The post-VAS score in the experimental group was reduced from 3.68 with an SD of 1.129 to a carryover VAS score of 2.60 with an SD of 1.465 (P = 0.002). The post-PSC score was reduced from 3.733 with an SD of 1.386 to carry over the PSC score of 3.05 with an SD of 1.395 (P = 0.032). The post-SLR score was increased from 58.18 with an SD of 14.608 to a score of 70.70 with an SD of 10.623 (P < 0.001).
The changes in the VAS, PSC, and SLR scores in the post-data group are demonstrated in Table 3 using the Wilcoxon signed-rank test.
| S. No. | Variables | Pre M±SD (median) | Post M±SD (median) | P-value |
|---|---|---|---|---|
| 1. | VAS | 6.14±1.283 (6.000) | 4.73±1.667 (5.000) | <0.001 |
| 2. | PSC | 5.32±0.780 (5.500) | 4.55±1.335 (5.000) | 0.007 |
| 3. | SLR | 48.78±8.708 (49.000) | 54.32±11.623 (55.000) | 0.007 |
M: Median, SD: Standard deviation, VAS: Visual analog scale, PSC: Pain site code, SLR: Straight leg raise
In the control group, the pre-VAS score was reduced from 6.14 with an SD of 1.283 to a post-VAS score of 4.73 with an SD of 1.667 (P < 0.001). The PSC score was reduced from 5.32 with an SD of 0.780 to a post-PSC score of 4.55 with an SD of 1.335 (P = 0.007). The SLR score was increased from 48.783 with an SD of 8.708 to a post-SLR score of 54.32 with an SD of 11.623 (P = 0.007).
An improvement in the VAS and SLR score in the carryover data is demonstrated in Table 4 using the Wilcoxon signed-rank test.
| S. No. | Variables | Post M±SD (Median) | Carryover M±SD (Median) | P-value |
|---|---|---|---|---|
| 1. | VAS | 4.73±1.667 (5.000) | 4.50±1.504 (5.000) | 0.424 |
| 2. | PSC | 4.55±1.335 (5.000) | 4.77±1.193 (5.000) | 0.340 |
| 3. | SLR | 54.32±11.623 (55.000) | 52.41±12.458 (56.000) | 0.388 |
M: Median, SD: Standard deviation, VAS: Visual analog scale, PSC: Pain site code, SLR: Straight leg raise
In the control group, the post-VAS was reduced from 4.73 with an SD of 1.667 to a carryover VAS score of 4.50 with an SD of 1.504, which was not statistically significant (P = 0.424). The post-PSC score was increased from 4.55 with an SD of 1.335 to carryover 4.77 with an SD of 1.193, which was not statistically significant (P = 0.340). The post-SLR score was reduced from 54.32 with an SD of 11.628 to a carryover SLR score of 52.41 with an SD of 12.458, which was not statistically significant (P = 0.388).
The experimental and control groups for VAS, PSC, and SLR scores in the carryover data are compared in Table 5 using the Mann–Whitney U-test. The mean post-VAS score in the experimental group was 3.681 with an SD of 1.129 and the mean of VAS post in the control group was 4.727 with an SD of 1.66, which was statistically significant. The mean score of VAS carryover was 2.600 with an SD of 1.465 and the mean of VAS carryover in the control group was 4.500 with an SD of 1.50 (P < 0.001). The mean of post-PSC in the experimental group was 3.727 with an SD of 1.386 and the mean of post-PSC in group 2 was 4.545 with an SD of 1.335, which was not statistically significant (P = 0.054). The mean of carryover PSC in the experimental group was 3.050 with an SD of 1.394 and the mean of carryover PSC in the control group was 4.772 with an SD of 1.192, which was statistically significant (P < 0.001). The mean of post-SLR in the experimental group was 58.181 with an SD of 14.608 and the mean of post-SLR in the control group was 54.318 with an SD of 11.622, which was not statistically significant (P = 0.200). The mean of carryover SLR in the experimental group was 70.700 with an SD of 10.623 and the mean of carryover SLR in the control group was 52.409 with an SD of 12.458, which was statistically significant (P < 0.001).
| S. No. | Variable | Experimental group M±SD | Control group M±SD | P-value |
|---|---|---|---|---|
| 1. | VAS pre | 5.954±0.843 | 6.142±1.314 | 0.626 |
| 2. | VAS post | 3.681±1.129 | 4.727±1.66 | 0.029 |
| 3. | VAS carryover | 2.600±1.465 | 4.500±1.50 | <0.001 |
| 4. | PSC pre | 5.363±0.789 | 5.318±0.779 | 0.816 |
| 5. | PSC post | 3.727±1.386 | 4.545±1.335 | 0.054 |
| 6. | PSC carryover | 3.050±1.394 | 4.772±1.192 | <0.001 |
| 7. | SLR pre | 49.454±9.634 | 48.727±8.707 | 0.750 |
| 8. | SLR post | 58.181±14.608 | 54.318±11.622 | 0.200 |
| 9. | SLR carryover | 70.700±10.623 | 52.409±12.458 | <0.001 |
M: Median, SD: Standard deviation, VAS: Visual analog scale, PSC: Pain site code, SLR: Straight leg raise
DISCUSSION
When the data were analyzed in the experimental group, it was found that the VAS score was statistically reduced when we compared the pre-post data (P < 0.001) and the post-carryover data (P = 0.002). In 2019, 2017, 2020, and 2023, different studies suggested that neurodynamics helps reduce pain by developing centralization.[8,14-16] A study conducted in 2021 found that patients receiving sliders and tensioners showed significant improvement in pain.[17] Another study conducted in 2019 suggested that the sliders’ neural mobilization exercises are efficacious in reducing pain immediately.[18] The PSC score was statistically reduced when we compared the pre-post data (P < 0.001) and the post-carryover data (P = 0.032). In 2021, Shah and Soni conducted a study and it concluded that the radiating symptoms may be centralized using neurodynamics.[6] In the present study, the SLR range was increased when we compared the pre-post data (P = 0.002) and the post-carryover data, which was statistically significant (P < 0.001). A study in 2015 suggested that the butler’s neural mobilization showed significant improvement in SLR ranges immediately after the session, but it was not maintained for 24 h.[19] Another research conducted in 2012 suggested that neurodynamics treatment effectively improves SLR ranges in patients with radiating low backaches.[20]
When the data was analyzed in the control group, it was found that the VAS score was statistically reduced when the pre-post data was compared (P < 0.001), but it was not maintained for a long time when we compared the post-carryover data (P = 0.424). A study conducted in 2018 concluded that McKenzie extension exercises were efficacious in decreasing LBP in patients with PIVD.[21] Other studies in 2014 and 2017 suggested that core exercises are efficacious in improving pain in patients with chronic LBP.[22,23] The PSC score was reduced when we compared the pre-post data (P < 0.007) but not in the post-carryover data (P = 0.340). This might be because the VAS was reduced, which can alter the pain sensitivity so the patient can experience improved radiating pain. It was not maintained in carryover effect due to the reason that the intervention was given only for one session, but if we give the intervention in continuation for a week, it might show the improvement in the PSC score. A 2018 study concluded that McKenzie extension exercises yield results in 3–4 days, whereas core strengthening exercises yield results in 10 days.[21] A case series was studied in 2015, and it was found that core strengthening exercises are useful in reducing nerve root irritation and decreasing radiating pain.[24] In 2014 and 2021, Bakhtiary et al. and Parkhi et al. studies revealed that lumbar stabilization effectively reduces pain in patients with lumbar disc herniation.[25,26] In the present study, the SLR range was increased when we compared the pre-post data (P < 0.007) but not in the post-carryover data (P = 0.388). A study in 2016 revealed that Mackenzie’s exercises show improvement in reducing VAS, SLR, and lumbar range of motion.[27] This indicates that the core strengthening exercises can reduce the pain immediately, which will cause the patient to get relief from radiating pain. The SLR range will increase, but the effect will be brief.
In the present study, when we compared the data between the groups, we learned that there were significant immediate and carryover improvements in VAS scores in the experimental group [Figure 8]. The previous studies suggested that neurodynamics is efficacious in reducing pain in patients with lumbar radiculopathy.[6,8,19-22] The experimental and control group had an immediate effect in reducing the PSC score, but only in the experimental group, it was maintained for a long period (P < 0.001). The SLR range was increased immediately in both the groups, but only in the experimental group. It was maintained for a long period (P < 0.001). From the previous studies, many authors suggested that neurodynamics can alter neural mobility, centralize pain, increase SLR ranges, and improve functional ability.[21,22]
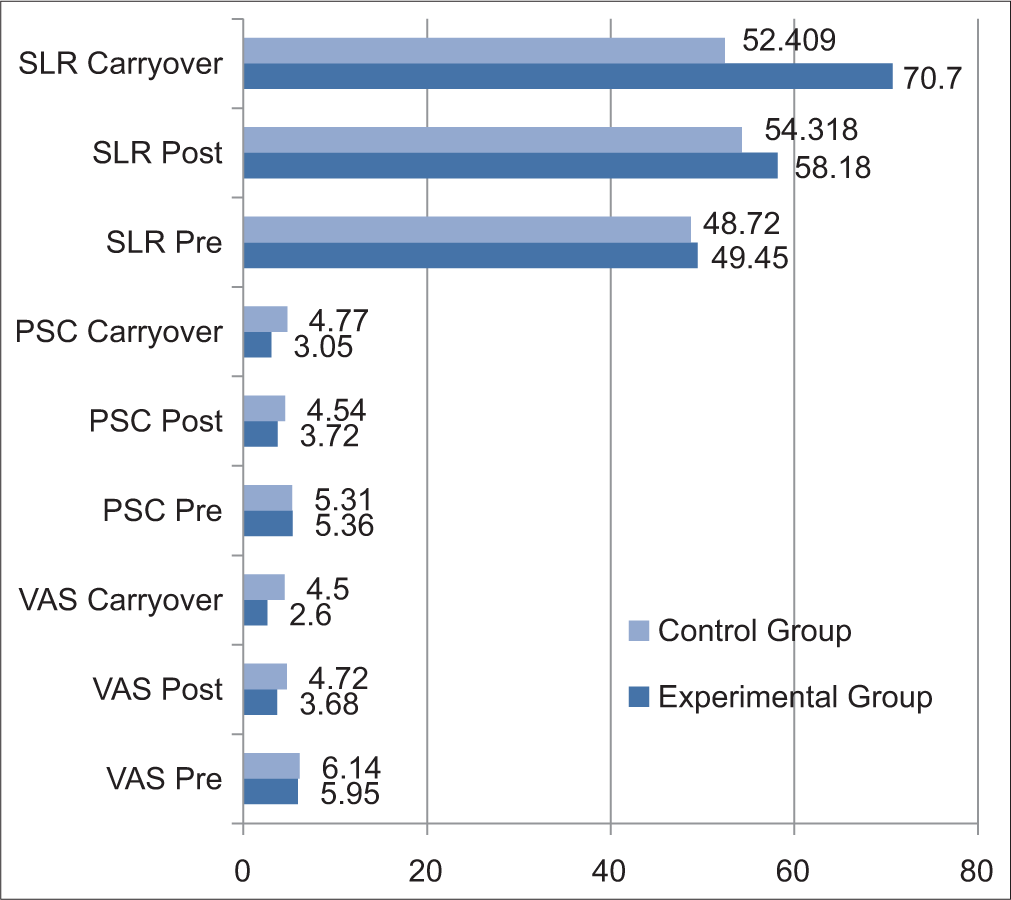
- Difference between experimental and control group.
Limitations
This study was carried out over a short time and had a limited sample size.
CONCLUSION
The neurodynamics, including the static opener and four levels of sliders and tensioners, showed significant immediate and carryover improvement in VAS, PSC score, and SLR ranges. Conventional treatment, including spinal extension exercises, core isometric exercises, pelvic bridging exercises, and glutes isometric exercises, showed significant improvement immediately on VAS, PSC score, and SLR ranges, but it was not maintained in the carryover period.
However, on comparison, the experimental group improved pain, PSC score, and SLR range better than the control group in terms of duration and intensity.
Recommendations
This study can be carried out on a larger sample size and for a longer duration.
The study can be further carried out by combining neurodynamics exercises with McKenzie, core isometric exercises along with different outcome variables.
This study can be further carried out by comparing age and sex using two different interventions and their effectiveness can be seen in longer periods.
ACKNOWLEDGEMENT
Abhishek Sharma: Guidance in providing the concept and idea. Akansha Uniyal: Helped to analyze the result, interpret the data, and provide the plagiarism report. Abhinav Bahuguna: Helped to analyze the result. Pragya Sharma: Helped write the article and provide the references. Anjali Rawat: Helped to conduct a double-blinded study by being a second therapist.
AUTHORS’ CONTRIBUTIONS
DB: Involved in conducting the research, collecting, and assembling the data. Involved in writing and editing the manuscript and publication. AB: Reference of patients, guidance in editing manuscript and publication. VA: Guidance in methodology, reference of patients. SP: Reference of patients and guidance in the manuscript. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The research/study approved by the Institutional Review Board at Himalayan Institute of Medical Sciences, SRHU, number SRHU/HIMS/ETHICS/2022/106B, dated September 14, 2022.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- The effectiveness of exercise program after lumbar discectomy surgery. J Clin Orthop Trauma. 2021;16:99-105.
- [CrossRef] [PubMed] [Google Scholar]
- Prolapsed herniated or extruded intervertebral disc-treatment by only stabilization. J Craniovertebr Junction Spine. 2018;9:133-4.
- [CrossRef] [PubMed] [Google Scholar]
- Spontaneous regression of a large sequestered lumbar disc herniation: A case report and literature review. J Int Med Res. 2021;49:3000605211058987.
- [CrossRef] [PubMed] [Google Scholar]
- A case study on Prolapsed Lumbar Intervertebral Disease (PLID) acupuncture treatment in Bangladesh. J Adv Med Sci. 2023;3:1-3.
- [Google Scholar]
- A systematic review and meta-analysis on the efficacy of physiotherapy intervention in management of lumbar prolapsed intervertebral disc. Int J Health Sci. 2021;15:49-57.
- [Google Scholar]
- Effect of neurodynamic techniques on radiating symptoms and mechanosensitivity of neural tissue in subjects with lumbosacral radiculopathy: A double-blind randomized controlled trial. Int J Med Sci Public Health. 2021;2:1.
- [CrossRef] [Google Scholar]
- The effect of Mckenzie approach and Mulligan's mobilisation (SNAGS) in lumbar disc prolapse with unilateral radiculopathy. Int J Res. 2014;3:59-63.
- [Google Scholar]
- Extending the straight leg raise test for improved clinical evaluation of sciatica: Reliability of hip internal rotation or ankle dorsiflexion. BMC Musculoskelet Disord. 2021;22:303.
- [CrossRef] [PubMed] [Google Scholar]
- Dejong's the neurologic examination. (7th ed). Netherlands: Wolter Kluwer; 2020. p. :816. Ch. 47
- [Google Scholar]
- Passive straight leg raise test: Definition, interpretation, limitations and utilization SPINE HEALTH. J Curr Clin Care. 2014;4:25-32.
- [Google Scholar]
- The sensitivity and specificity of the Slump and the Straight Leg Raising tests in patients with lumbar disc herniation. J Clin Rheumatol. 2008;14:87-91.
- [CrossRef] [PubMed] [Google Scholar]
- Difference between neurodynamic mobilization and stretching exercises for chronic discogenic sciatica. Med J Cairo Univ. 2021;89:1869-76.
- [CrossRef] [Google Scholar]
- Effectiveness of nerve flossing technique in chronic lumbar radiculopathy. Indian J Physiother Occup Ther. 2017;11:44-9.
- [CrossRef] [Google Scholar]
- Effect of neurodynamic mobilization on pain and function in subjects with lumbo-sacral radiculopathy. Med Sci Int J. 2017;6:8664.
- [CrossRef] [Google Scholar]
- Comparison of conservative treatment with and without neural mobilization for patients with low back pain: A prospective, randomized clinical trial. J Back Musculoskelet Rehabil. 2020;33:969-75.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of spinal manipulation or mobilization as an adjunct to neurodynamic mobilization for lumbar disc herniation with radiculopathy: A randomized clinical trial. J Man Manip Ther. 2023;31:408-20.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of neural mobilization exercises in patients with low back-related leg pain with peripheral nerve sensitization: A prospective, controlled trial. J Chiropr Med. 2021;20:59-69.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative study on immediate effect of two different neural, mobilisation techniques on pain and knee extension range in patients with lumbosacral radiculopathy. Int J Recent Sci Res. 2019;10:31855-61.
- [Google Scholar]
- Effect of Butler's neural tissue mobilization and Mulligan's bent leg raise on pain and straight leg raise in patients of low back ache. J Bodyw Mov Ther. 2016;20:280-5.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of bent leg raise technique and neurodynamics in patients with radiating low back pain. Pak J Med Sci. 2022;38:47-51.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of the effectiveness of core strengthening exercise and McKenzie extension exercise on the pain functional disability in lumbar PIVD condition. Physiother Occup J. 2018;11:67-79.
- [Google Scholar]
- Effects of the CORE exercise program on pain and active range of motion in patients with chronic low back pain. J Phys Ther Sci. 2014;26:1237-40.
- [CrossRef] [PubMed] [Google Scholar]
- Core stability exercise versus general exercise for chronic low back pain. J Athl Train. 2017;52:71-2.
- [CrossRef] [PubMed] [Google Scholar]
- Is McKenzie method with core exercise effective for patients with disc derangement? A case series. VIMS Health Sci J. 2015;2:26-31.
- [Google Scholar]
- Lumbar stabilizing exercises improve activities of daily living in patients with lumbar disc herniation. J Back Musculoskelet Rehabil. 2005;18:55-60.
- [CrossRef] [Google Scholar]
- Comprehensive physiotherapy management in PIVD patient. A case report. J Med Pharm Allied Sci. 2021;10:3640-2.
- [CrossRef] [Google Scholar]
- Effect of Mckenzie method with tens on lumbar radiculopathy. A randomized control trial. Int J Physiother. 2016;3:94-9.
- [CrossRef] [Google Scholar]






