Translate this page into:
Anterior ultrasound approach for evaluating posterior shoulder instability in brachial plexus birth palsy: A novel diagnostic technique
*Corresponding author: J. Terrence Jose Jerome, Department of Orthopaedics, Hand and Reconstructive Microsurgery, Olympia Hospital and Research Centre, Trichy, Tamil Nadu, India.terrencejose@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jerome TJ. Anterior ultrasound approach for evaluating posterior shoulder instability in brachial plexus birth palsy: A novel diagnostic technique. J Musculoskelet Surg Res. 2025;9:281-4. doi: 10.25259/JMSR_284_2024
Abstract
Brachial plexus birth palsy (BPBP) often leads to shoulder deformities, such as posterior subluxation and internal rotation of the humeral head, which can severely impact a patient’s quality of life. Traditional imaging techniques such as magnetic resonance imaging, while effective, often require sedation or anesthesia, limiting their routine use in pediatric patients. This technical note explores using ultrasound as a non-invasive alternative for evaluating and monitoring shoulder deformities in BPBP patients. We introduce a novel ultrasound method that focuses on the alignment of the coracoid process and the humeral head, revealing significant differences between affected and unaffected shoulders. This technique offers a reliable and accessible tool for early diagnosis and intervention, improving outcomes for patients with BPBP-related shoulder deformities.
Keywords
Brachial plexus
Birth palsy
Coracoid process
Diagnostic imaging
Humeral head
Musculoskeletal ultrasound
Posterior subluxation
Shoulder deformity
INTRODUCTION
Brachial plexus birth palsy (BPBP) frequently leads to substantial shoulder deformities, notably posterior subluxation and abnormal internal rotation of the humeral head.[1-5] These deformities can severely impair affected individuals’ functional outcomes and quality of life. Magnetic resonance imaging (MRI) is the preferred method for diagnosing and assessing the severity of glenohumeral dysplasia, providing crucial information for surgical planning.[1] MRI is particularly adept at visualizing unossified glenoid structures, which is essential in young patients. However, it is important to note that MRI often necessitates sedation or anesthesia, especially for young children who may find it difficult to remain still during the procedure.[1]
Posterior shoulder subluxation was visually assessed using ultrasound (transverse plane) and quantified using the α angle, as described by Vathana et al.[2] The α angle is formed between the posterior margin of the scapula and a line tangential to the humeral head and posterior glenoid edge. This angle is typically 30° or less in normal shoulders, with the humeral head located anterior to the posterior scapular line. As subluxation severity increases, the α angle widens, and the humeral head shifts further posteriorly relative to this line.
While the α angle provides valuable information, we propose an alternative anterior ultrasound approach assessing the parallelism between the coracoid process and the humeral head. This method offers several advantages:
Ease of use: The anterior approach offers superior visualization and measurement capabilities compared to the posterior approach, particularly in immature skeletons where assessing the humeral head, glenoid, labrum, and α angle can be challenging
Reproducibility: The coracoid process and humeral head are easily identifiable landmarks, leading to more consistent and reproducible measurements
Dynamic assessment: Real-time ultrasound imaging allows for dynamic assessment of shoulder movement and subluxation, providing a more comprehensive evaluation of shoulder instability.
The article aims to use ultrasound (transverse plane) anteriorly and assess the parallelism between the coracoid process and the humeral head. Through this assessment, clinicians can reliably assess posterior shoulder subluxation in BPBP patients, facilitating early diagnosis and intervention to improve long-term outcomes.
INDICATIONS AND CONTRAINDICATIONS
The anterior ultrasound approach is indicated for diagnosing and monitoring shoulder deformities, particularly posterior subluxation and internal rotation abnormalities, in patients with BPBP. This technique leverages the consistent anatomical relationship between the humeral head and coracoid process as reliable landmarks. However, it is contraindicated when adequate ultrasound access to the shoulder joint is limited due to severe tissue swelling, scarring, or significant anatomical variations.
TECHNICAL ASPECTS
Equipment and setup
A high-frequency linear transducer (7–15 MHz) is used to ensure optimal resolution for detailed imaging. The patient is positioned comfortably in a chair with the shoulder in neutral rotation. This setup allows for accurate and stable imaging, facilitating a clear view of the relevant anterior anatomical structures.
Procedure
Position the high-frequency ultrasound probe transversely over the anterior shoulder to visualize both the coracoid process and the humeral head. On the ultrasound image, the humeral head and its ossified nucleus appear as hyperechoic (brighter) structures. The coracoid process, located medially, is also hyperechoic (brighter). These two consistent bony landmarks serve as essential reference points for accurately assessing the anterior shoulder
Measurement
In affected shoulders, the coracoid process and the humeral head align along the same plane, which is indicative of posterior subluxation of the humeral head [Figure 1].
In unaffected shoulders, the coracoid process is positioned superior to the humeral head, with the two structures remaining parallel [Figure 2].
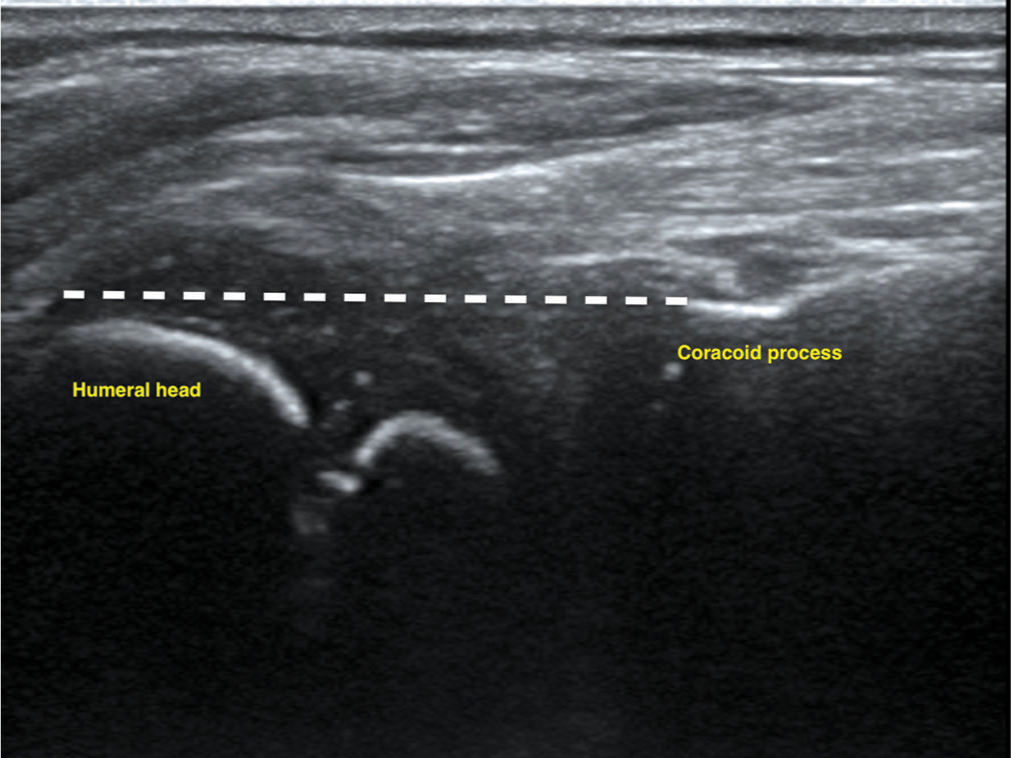
- Ultrasound image of a brachial plexus birth palsy-affected shoulder, showing the coracoid process and humeral head aligned within the same plane, indicative of posterior subluxation.
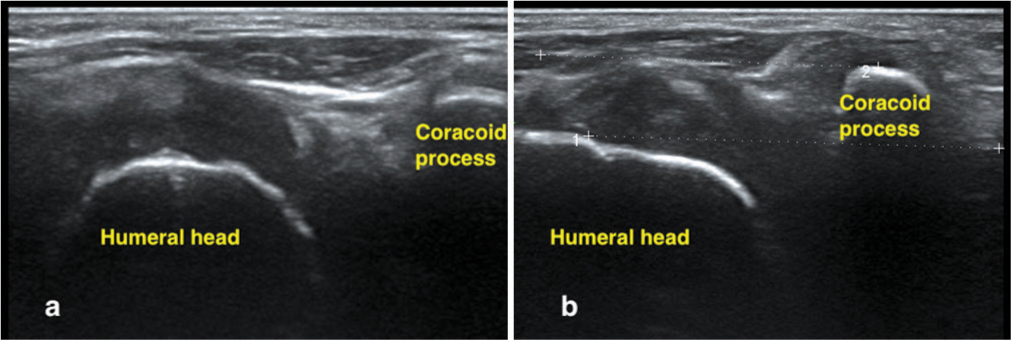
- Ultrasound image of a normal shoulder (a,b) highlighting the coracoid process positioned superior to and parallel to the humeral head, reflecting typical anatomical alignment.
WHY ANTERIOR ULTRASOUND?
The anterior ultrasound approach is chosen to assess posterior shoulder subluxation in BPBP due to the distinct anatomical correlation between the humeral head and the coracoid process. In this approach, these structures serve as reliable landmarks because they maintain a consistent spatial relationship in both normal and dislocated shoulders. The coracoid process, a stable bony prominence, acts as a fixed reference point and is considered the lighthouse of the shoulder. By visualizing its position relative to the humeral head in real-time ultrasound, we can accurately measure the degree of posterior displacement, providing a quantifiable assessment of shoulder instability. Furthermore, the anterior approach allows for direct visualization of the glenohumeral joint, enabling us to evaluate the integrity of the anterior capsule, ligaments, and tendons, which are crucial for maintaining shoulder stability. This comprehensive assessment aids in diagnosing and guiding the management of posterior shoulder subluxation.
PITFALLS AND PEARLS
While ultrasound offers several advantages, being aware of potential pitfalls is important. Operator dependency can introduce variability in measurements, highlighting the need for proper training and standardization of techniques. In addition, visualizing landmarks can be challenging in patients with severe deformities or substantial soft-tissue swelling. To overcome these limitations, ensure consistent patient positioning to achieve reproducible measurements and utilize real-time imaging to dynamically assess shoulder movement and subluxation, enhancing the accuracy and reliability of ultrasound-guided evaluations.
DISCUSSION
Ultrasound offers a valuable tool for assessing shoulder deformities in patients with BPBP. The novel alignment of the coracoid process and humeral head in the same plane serves as a reliable indicator of internal rotation and posterior subluxation, significantly enhancing the diagnostic and monitoring capabilities for these deformities in a non-invasive manner. This method offers a straightforward and effective approach for clinicians to assess and track shoulder alignment, providing crucial insights into the severity and progression of the condition. This allows for timely and appropriate interventions, potentially improving patient outcomes.
The anterior ultrasound approach to assess the humeral head and shoulder deformities is a significant advancement. This method involves visualizing the alignment of the coracoid process and the humeral head. In affected shoulders, the coracoid process and the humeral head align on the same plane, indicating posterior subluxation of the humeral head. In contrast, the coracoid process in unaffected shoulders is positioned superior to the humeral head, with both structures remaining parallel. This approach is straightforward and can be easily implemented, making it a practical tool for clinicians.
Posterior subluxation of the shoulder is a recognized phenomenon in BPBP, but there is no consensus on the mechanics and timing of its development. Zancolli suggested that shoulder deformities result directly from birth injuries to the proximal humeral physis and shoulder muscles.[3] In contrast, Gilbert proposed that muscle imbalance in the rotator cuff due to neural injury leads to internal rotation contracture and glenohumeral deformity.[4] Using ultrasound to detect posterior shoulder instability was first demonstrated by Hunter et al.,[5] with Moukoko et al. verifying this through a lateral ultrasound approach.[6] However, the posterior approach later became favored due to better visualization [Figure 3]. Despite its advantages, the posterior approach requires a learning curve, particularly in understanding the osseous anatomy and accurately measuring the α angle.
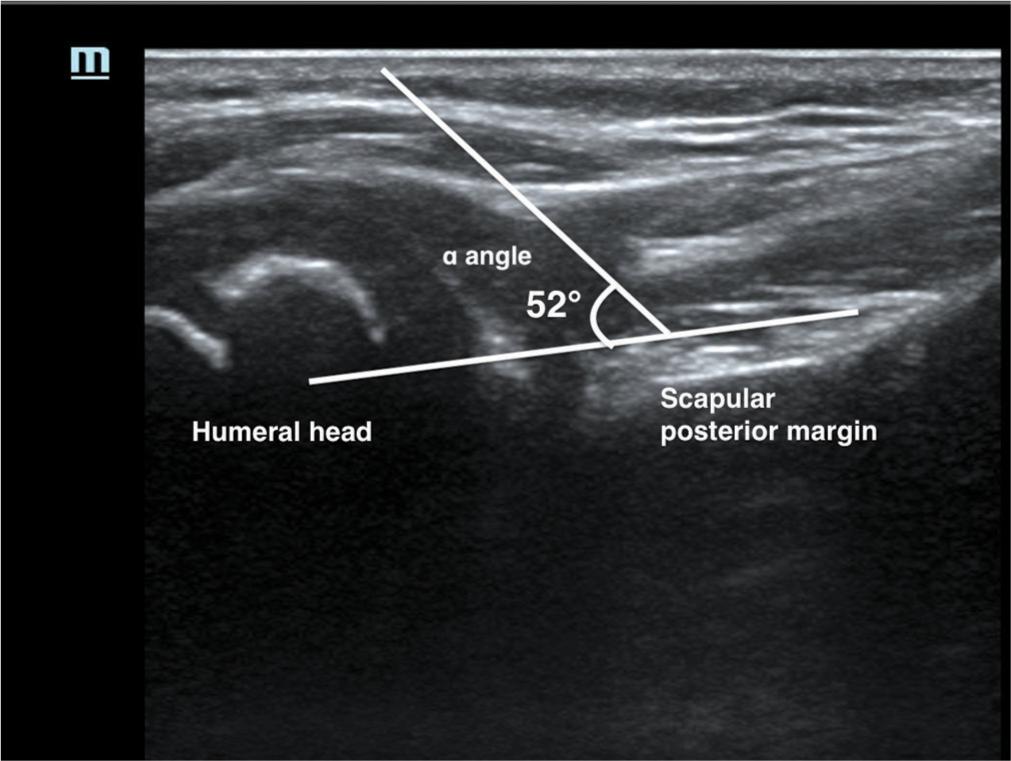
- Depiction of the α angle, formed between the posterior margin of the scapula and a line tangential to the humeral head and posterior glenoid edge.
Early detection of shoulder instability is crucial for preventing joint deterioration and allows for early treatment[7] Despite this, ultrasound screening is recommended only for patients with persistent BPBP symptoms, as those who fully recover do not develop shoulder instability.[8] Studies indicate a significant incidence of posterior shoulder dislocation in BPBP patients, emphasizing the importance of ultrasound in the early and accurate diagnosis.[9]
To the best of our knowledge, the anterior ultrasound method presented in this article is a novel technique that could offer a simple and effective approach for diagnosing shoulder deformities in patients with BPBP. While the standard posterior ultrasound approach remains essential, augmenting it with an anterior shoulder ultrasound to assess the alignment of the humeral head and coracoid process can offer surgeons a more comprehensive understanding of the complex shoulder pathology in BPBP. This combined approach enhances the ability to diagnose and monitor subtle changes in shoulder anatomy, contributing to more informed surgical planning and better patient outcomes.
Future research is warranted to standardize the anterior ultrasound technique, validate its accuracy against other imaging modalities, and establish its efficacy in larger patient populations. Integrating ultrasound assessment of both a and anterior shoulder ultrasound into routine clinical practice could significantly enhance diagnosing, monitoring, and treating shoulder deformities in BPBP.
CONCLUSION
Ultrasound proves to be an invaluable tool in assessing shoulder deformities associated with BPBP. Ultrasound offers a noninvasive, reliable method for early diagnosis and intervention in shoulder pathology, particularly in assessing posterior subluxation and internal rotation of the humeral head, which are critical for preventing long-term complications. The anterior shoulder ultrasound technique introduced in this article, which emphasizes the alignment between the coracoid process and the humeral head, represents a significant advancement in diagnostic accuracy. This innovative approach enhances the ability to detect subtle anatomical changes, facilitating more timely and effective treatment strategies.
Recommendations
Future research should aim to standardize this technique and further compare it with other imaging modalities to confirm its efficacy. Overall, incorporating ultrasound into routine clinical practice can enhance the management and outcomes of patients with shoulder deformities due to BPBP.
Ethical approval
Ethical approval was obtained from the Ethical Committee Board at the Olympia Hospital and Research Centre, reference number 10/2024, dated July 2, 2024.
Declaration of patient consent
The author certifies that he has obtained all appropriate patient consent forms. In the form, the patient’s parents have given the consent for the images and other clinical information to be reported in the journal. The patient’s parents understand that the name and initials will not be published, and due efforts will be made to conceal the patient’s identity, but anonymity cannot be guaranteed.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Conflicts of interest
There are no conflicting relationships or activities.
Financial support and sponsorship: This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Brachial plexus birth injury: US screening for glenohumeral joint instability. Radiology. 2010;254:253-60.
- [CrossRef] [Google Scholar]
- Intraobserver and interobserver reliability of two ultrasound measures of humeral head position in infants with neonatal brachial plexus palsy. J Bone Joint Surg Am. 2007;89:1710-5.
- [CrossRef] [Google Scholar]
- Palliative surgical procedures in sequelae of obstetrical palsy In: Tubiana R, ed. The hand. Vol 4. Philadelphia, PA: Saunders; 1993. p. :602-23.
- [Google Scholar]
- Obstetrical brachial plexus palsy In: Tubiana R, ed. The hand. Vol 4. Philadelphia, PA: Saunders; 1993. p. :575-601.
- [Google Scholar]
- The ultrasound diagnosis of posterior shoulder dislocation associated with Erb's palsy. Pediatr Radiol. 1998;28:510-1.
- [CrossRef] [Google Scholar]
- Posterior shoulder dislocation in infants with neonatal brachial plexus palsy. J Bone Joint Surg Am. 2004;86:787-93.
- [CrossRef] [Google Scholar]
- Ultrasound diagnosis of shoulder congruity in chronic obstetric brachial plexus palsy. J Bone Joint Surg Br. 2002;84:100-3.
- [CrossRef] [Google Scholar]
- Glenoid deformity secondary to brachial plexus birth palsy. J Bone Joint Surg Am. 1998;80:659-67. [Published correction appears in J Bone Joint Surg Am 1998;80:1555-9.]
- [CrossRef] [Google Scholar]
- Clinical presentations, differential diagnosis and management of obstetric brachial palsy. Rev Neurol. 1998;27:258-63.
- [Google Scholar]






