Translate this page into:
Causes of anterior cruciate ligament reconstruction failure: A meta-analysis
*Corresponding author: Mohamed Elfekky, Department of Orthopedics, Dubai Health Authority, Dubai, United Arab Emirates. mohamelfekky@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Elfekky M, Mostafa H, Shahi U, Shalaby E, Alharoun M, Elghaish M, et al. Causes of anterior cruciate ligament reconstruction failure: A meta-analysis. J Musculoskelet Surg Res 2022;6:193-9.
Abstract
Anterior cruciate ligament (ACL) injury is one of the most common knee injuries among athletes and during sports activities for which ligament reconstruction is the optimal therapeutic procedure. Functional instability of the knee because of ACL injury is prone to relapse. Relapse is commonly reported following surgery due to various reasons. Knowing the possible causes are major key in the management of patients with an ACL tear after reconstruction. This meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines. PubMed, Cochrane library, and Google Scholar were searched for eligible articles from January 1, 2010, to December 31, 2020. The articles were selected on inclusion and exclusion criteria mentioned in the study protocol. Following the screening of all the articles, the short-listed articles were subjected to full-text review by two independent reviewers. The overall search process gave us 1571 articles in total, from which 13 were selected for meta-analysis. A total of 891 patients were included in the 13 studies evaluated with respect to the factors responsible for failure of the primary ACL reconstructive procedure. Tunnel placement error and traumatic reinjury were the most reported associated factors responsible for primary ACL reconstruction failure. However, the overall summary estimate for the two major etiologies was not significant. The P-value for overall effect was 0.76, along with a Z score of 0.30 and an I2 test value of 91%, indicating high study variability. The odd’s ratio was calculated using the Mantel-Haenszel random effects model for ACL reconstruction failure, which was 0.88. Understanding the cause of primary ACL failure and developing strategies to minimize or avoid it completely will help in reducing the incidence of ACL reconstructive failure and improve patient outcomes.
Keywords
Anterior cruciate ligament reconstruction failure
Anterior cruciate ligament
Primary anterior cruciate ligament reconstruction
Trauma
Tunnel error
INTRODUCTION
Anterior cruciate ligament (ACL) injury is known to be the most common and devastating knee injury occurring during sport athletic participation, especially when participating in pivoting and cutting sports.[1,2] In general, the yearly incidence of primary ACL injury is higher in healthy sportspersons between 1.5% and 1.7%.[3] Ligament reconstruction is the ideal treatment for functional instability of the knee after ACL injury.[4] ACL reconstruction produced great and even excellent long-term outcomes including the improvement of symptoms, restoration of articular stability, and return to pre-injury activities. Yet, patients might experience recurrent instability (failure) reported as rupture of ipsilateral graft or a tear of contralateral native ACL.[5-8] Furthermore, the technical details regarding the anatomy of the ACL, including tunnel placement, are considered a debated topic.[9] A range of patients 0.7–20% experiences reinjury due to graft failure.[4]
Mohan et al. provided insight on the present evidence of revision ACL reconstruction. The authors reported an overall objective failure rate of 6%.[10] Another meta-analysis conducted by Crawford et al. also estimated a low rate (6.2%) of failure in primary ACL reconstruction.[11] Due to the progressive rise in ACL injuries and, therefore, reconstruction surgery, it is expected that the incidence of failure will also rise.[5,7]
Many risk factors were found to be associated with the occurrence of primary knee injury, including age, gender, sports’ intensity, neuromuscular factors, and non-modifiable risk factors, such as anatomical characteristics such as posterior tibial slope, width, size, and limb alignment.[12] Furthermore, risk factors of ACL failure have been suggested to be the mode of reinjury, diameter and type of graft in primary surgery, tunnel positioning, and the period between primary surgery and reinjury. The previous evidence showed that tunnel malposition was the principal cause of ACL reconstruction failure and was suggested to be associated with better outcomes of revision ACL reconstruction. This factor has been presented and known as the “resident ridge pitfall.”[13]
In the past decade, multicenter and population-based studies on revision surgery were a bit sparse. Indeed, the literature has contributed to the understanding of revision ACL reconstruction, still, the body of literature continues to grow. A successful ACL revision surgery needs a systematic approach to identifying and correcting all possible failure origins. Therefore, an updated informative systematic review or meta-analysis on accurate identification of the cause of failure is crucial. This present meta-analysis aims to examine failure etiologies of reconstruction procedures in ACL.
MATERIALS AND METHODS
Protocol and reporting
The study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. A summary of the methodology with respect to search strategy for inclusion and exclusion of studies is depicted in Figure 1 in the form of a PRISMA flowchart.

- Preferred Reporting Items for Systematic Reviews and Meta-analyses flowchart.
Eligibility criteria/study selection
Studies mentioning the factors responsible for ACL reconstruction failure were considered to be eligible for the meta-analysis. The following points were considered for the inclusion criteria: Studies that enlisted reasons for the failure of ACL reconstruction following athletic injury, trauma, fall from height, or history of trivial injury, all of them requiring ACL reconstruction, studies that included various medical conditions (lack of graft incorporation, graft rejection, and autoimmune diseases) requiring primary ACL reconstruction, and studies that commented on revision ACL reconstruction in patients with prior primary ACL reconstruction but with failed outcomes following initial reconstruction. Reports of primary ACL reconstruction failure and reasons for revision ACL surgery in patients subjected to primary ACL reconstruction by the health-care professionals working in trauma care department were also considered to be included in our analysis. The exclusion criteria included studies requiring revision ACL reconstruction in case of patients due to non-medical reasons (RTA’s and interpersonal fights), and studies commenting on the factors responsible for failure of ACL reconstructive surgery in the form of review articles. Furthermore, studies that satisfied the selection criteria but were available only in the form of abstracts and incomplete studies such as those with missing results, duplicates, and unpublished articles were excluded from the study. Finally, all the eligible articles available in the English language were selected for evaluation.
Data sources and search strategy
Search terminology was defined according to the protocol of the meta-analysis that involved the identification of the search terms with respect to the factors responsible for primary and revision ACL reconstruction failure. The words were used with the Boolean operator AND to sort out the related articles. Free text search utilized the words such as ACL, reconstruction, revision ACL reconstruction along with the Boolean operator OR in-between them, and in association with primary failure with the Boolean operator AND. The controlled language search, on the other hand, included the following Medical Subject Headings terms: “ACL,” “primary failure,” “reconstruction,” and “revision ACL reconstruction.”
Databases such as PubMed, Cochrane library, and Google Scholar were searched for eligible articles from January 1, 2010, to December 31, 2020. The references of all the studies that were included were rechecked to make sure they were all eligible. Databases were searched for possible studies, and then, the title and abstract of the articles were checked by independent reviewers to see if they met the criteria.
Data extraction and risk of bias assessment
Two impartial reviewers each collected data on their own and documented it on a bespoke data extraction form that they had created. The discrepancy regarding whether to include a particular study was settled by discussion or, if required, arbitration by an additional reviewer. Once the preliminary study selection was made based on the selection criteria, the entire text of the articles was assessed to evaluate the content after which, the study was considered to be included in the review. Important information pertaining to various medical conditions, (lack of graft incorporation, graft rejection, and autoimmune diseases) risks, and patient factors responsible for failure of primary reconstruction of the ACL in patients were extracted and analyzed. The risk of bias evaluation was carried out separately on each paper by two reviewers blindly.
Data synthesis and statistical analysis
A descriptive analysis of the extracted data was performed. Similar findings from the studies were identified and analyzed qualitatively, which were then represented accordingly. The meta-analysis was carried out with the help of the RevMan software version 5.3. Due to the high level of heterogeneity among the included studies with I2 value exceeding 50%, data were pooled using the random effects model. Forest plots mentioning the relative risk (RR) of the point estimates along with 95% CI of the factors responsible for primary and revision ACL reconstruction failure have been depicted.
RESULTS
Search results and study characteristics
The overall search process gave us 1571 articles, which on removal of the duplicates which were reduced to 649. Eligibility screening yielded 41 studies, which were then subjected to full-text review. Finally, 13 articles were selected for the meta-analysis [4,13-24] after subjecting the individual studies to screening and eligibility assessment by two independent reviewers. A total of 891 patients included from the 13 studies were assessed with respect to the factors responsible for the failure of primary ACL reconstruction.
The main causes of ACL reconstruction failure were identified according to the nature of the trauma to the knee and anatomical tunnel errors occurring during the reconstruction surgery.
Quality assessment of included studies
Because none of the included research was a randomized study, the quality of the included studies was assessed using the Methodological Index for Non-randomized Studies checklist. The checklist was developed with eight items for non-comparative studies (max score of 16) and 12 for comparative studies (max score of 24), rated between 0 and 2 each. Significant attention was drawn to the study purpose, participants, prospective design, appropriate endpoints, objective assessment, follow-up, dropout rate, and sample size calculation. Regarding comparative studies, the additional items included adequate control group, contemporary groups, baseline group equivalence, and adequate statistical analysis. Disagreement was discussed between reviewers. Four of the 13 studies included were of level III evidence due to the presence of a control group of primary ACL reconstruction. The average methodological score was 8.8 for the nine non-comparative studies, while it was 15.25 for the remaining comparative studies.
Factors for ACL reconstruction failure
The overall summary estimate as per the forest plot for the factors causing failure of primary ACL reconstruction between trauma and anatomical tunnel errors during surgery was not significant [Figure 2]. Seven studies raised questions about the tunnel error occurring during the operative procedure being more likely associated with failure.[13,14,16,17,19,20,23] In contrast, the remaining six studies mentioned trauma to be more likely associated with the reconstructive failure.[4,15,18,21,22,24] The p-value for overall effect was 0.76, along with a Z score of 0.30 and an I2 test value of 91%, indicating high study variability. The 95% CI of individual studies was widely spread apart from each other, thus adding to the heterogeneity. The odd’s ratio was calculated using the Mantel-Haenszel random effects model for ACL reconstruction failure, which was 0.88.

- Forest plot.
Exploration of heterogeneity and publication bias
In addition to the funnel plot, Egger’s test was employed to analyze the heterogeneity of the study results in this investigation [Figure 3]. The issue of publication bias was addressed during the process of study selection, as evidenced by the inverted funnel plot. The studies, however, showed considerable variation as ascertained by the I2 test with a value of 91%.
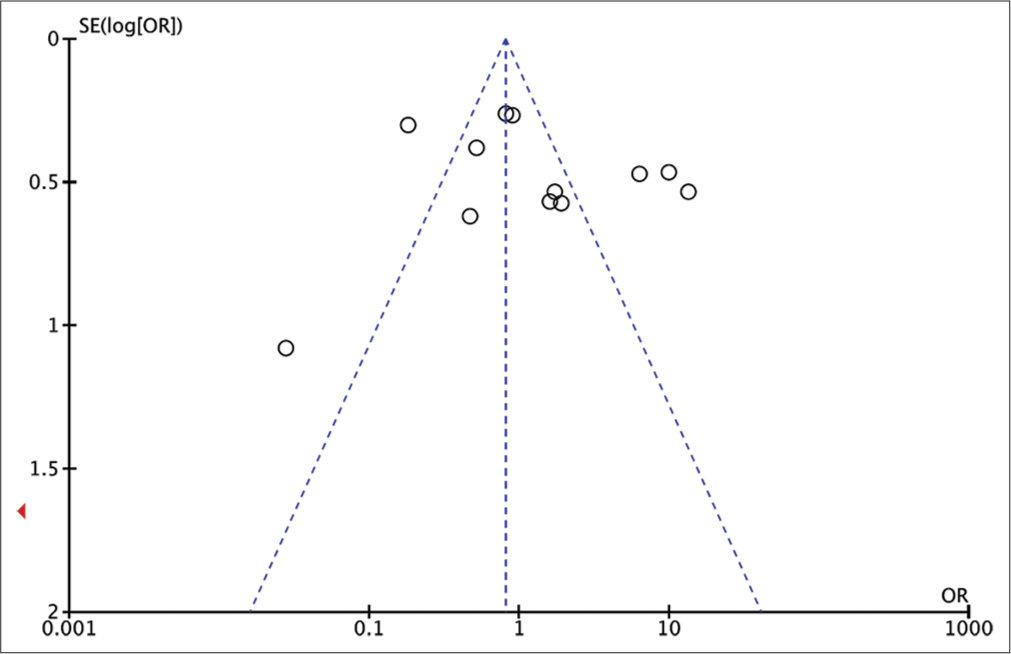
- Funnel plot.
DISCUSSION
This present meta-analysis assessed the etiology of the failure of primary ACL surgery, which can be sub-grouped into technical issues, biological failure, and traumatic injury. Technical errors are generally related to reconstruction failure occurring following 6-month postoperatively.[25] Errors arising out of the surgical technique constitute the highest proportion (77–95%) causing instability following ACL reconstruction resulting in ACL failure, in which non-anatomic inaccurate tunnel placement was the most reported technical error (70–80%).[26,27] This finding was consistent with the results of our meta-analysis mentioning relatively more studies holding tunnel errors responsible for primary ACL reconstruction failure. As for biological failure, it usually includes a lack of graft incorporation, infection, and allograft rejection.[25] However, these factors do not constitute the main chunk for ACL repair failure and, therefore, can best be avoided by adhering to the general patient management guidelines for infection and pharmacotherapy following graft introduction.[12] The incidence of primary ACL failure due to traumatic causes was reported from 5 to 10%. In our study, six out of 13 included studies commented on trauma being the most common and most important cause responsible for failure of primary ACL reconstruction surgery.
Among the technical errors, femoral tunnel malposition was the main cause of primary ACL failure, seen in 166 cases of revision ACL reconstruction.[28-30] Furthermore, the femoral tunnel during surgery gets placed anteriorly to an extreme degree in the majority of the cases due to the difficulty in the visualization of the “over the top” position of the femur during endoscopic ACL procedures.[31] This technical error was well-described in the previous evidence, yet, it remains the main source of ACL reconstruction failure. The anterior malposition of the femoral tunnel not only results in flexion due to the graft being already under excessive tension at 90° of flexion[32] and predisposes to knee instability when an extremely short intra-articular graft is used.
Another finding evidenced by this meta-analysis is that the incidence of traumatic reinjury of a well-positioned and well-fixed graft is similar to that of the femoral tunnel problem. It has been reported that trauma is responsible of around 30% of the cases of primary ACL failure.[22,33] There are two main factors that can explain this observation. First, there is an increasing demand for the patients to go back to sports with the same level and intensity following ACL reconstructive procedures and second, over-aggressive rehabilitation, which can turn out as contrary to the ACL graft integration[34] and, therefore, to the ligamentization process. This can happen due to over aggressive fixation of the tissue which might hamper with the joint and tissue stability and interfere with the process of graft integration. Recently, Shelbourne and Nitz[35] defined accelerated rehabilitation and validated it in primary ACL reconstruction cases, but may be questionable in revision ACL reconstruction cases.
However, the abovementioned factors can occur simultaneously and contribute to a failure. Before primary ACL reconstruction, the patient has the right to have accurate information regarding different possible surgical techniques. Their characteristics, such as reduced joint mobility due to contracture, may require additional procedures, including debridement either during surgery or as a separate operation.[8] A large scar or capsular contracture is more effectively treated conducting a different surgical operation following the rehabilitation period before reconstruction of primary ACL injury. The significance of being able to do a complete range of motion before revision must be considered to render the operative procedure beneficial. It must be noted that errors in tunnel size or placement can result in an additional surgery by transplanting some bone to fill possible defects, causing 6–12 weeks of revision delay.[8]
This study’s significance is the evaluation of different studies mentioning various reasons for the failure of primary ACL repair. The most common factors identified for failure were tunnel positioning errors and traumatic injury, which was well aligned with findings from different studies. The strength of this meta-analysis is that it has helped us to identify the common areas that have been neglected during the process of ACL reconstruction itself and during rehabilitation in the form of tunnel placement and traumatic injuries following surgery, respectively. Identifying these loopholes will not only aid in improving the surgical procedure for primary ACL reconstruction by improving the operative management of patients but also help change the post-operative rehabilitation approach.
Limitations of the study
First, included studies were very heterogeneous regarding outcomes. In addition, studies time was long (2004–2016), while surgical procedures and indications were evolving. Furthermore, inclusion of only three databases for inclusion of studies was a limitation.
CONCLUSION
Understanding the cause of primary ACL failure and developing strategies to minimize or avoid it completely will help in reducing the incidence of ACL reconstructive failure and improve patient outcomes.
ACKNOWLEDGEMENT
We would like to thank Dr. Yakub Sayyad from India for his great support and assistance in writing of the manuscript, data extraction and statistical analysis for this Meta-analysis paper.
AUTHORS’ CONTRIBUTIONS
ME conceived and designed the study, conducted research, provided research materials, and collected and organized data. HM analyzed and interpreted data. US and ES wrote the initial and MA and ME wrote final draft of the article, EA and SA provided logistic support. SA and AHA did all data entry and cleaning of final data. FN performed all statistical analysis. PT did finalization of the content. Finally, all authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The ethics committee approval was not required for this research paper as there is no direct patient involvement in this study.
DECLARATION OF PATIENT CONSENT
Patient’s consent not required as there are no patients in this study.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
References
- Basic science of anterior cruciate ligament injury and repair. Bone Joint Res. 2014;3:20-31.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012;22:116-21.
- [CrossRef] [PubMed] [Google Scholar]
- Contralateral anterior cruciate ligament injury after anterior cruciate ligament reconstruction: A case controlled study. Sports Med Arthrosc Rehabil Ther Technol. 2012;4:46.
- [CrossRef] [PubMed] [Google Scholar]
- Causes of failure of anterior cruciate ligament reconstruction and revision surgical strategies. Knee Surg Relat Res. 2016;28:319-24.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of allograft versus autograft anterior cruciate ligament reconstruction graft survival in an active adolescent cohort. Am J Sports Med. 2014;42:2311-8.
- [CrossRef] [PubMed] [Google Scholar]
- Revision anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39:199-217.
- [CrossRef] [PubMed] [Google Scholar]
- Functional outcomes of anterior cruciate ligament reconstruction with tibialis anterior allograft. Bull Hosp Jt Dis. 2013;71:138-43.
- [Google Scholar]
- Pre-operative planning in anterior cruciate ligament reconstruction revision surgery. Joints. 2013;1:25-33.
- [Google Scholar]
- The anatomy of the anterior cruciate ligament and its relevance to the technique of reconstruction. Bone Joint J. 2016;98:1020-6.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical outcomes in revision anterior cruciate ligament reconstruction: A meta-analysis. Arthroscopy. 2018;34:289-300.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term failure of anterior cruciate ligament reconstruction. Arthroscopy. 2013;29:1566-71.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: Prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43:1583-90.
- [CrossRef] [PubMed] [Google Scholar]
- Causes for failure of ACL reconstruction and influence of meniscectomies after revision. Knee Surg Sports Traumatol Arthrosc. 2011;19:196-201.
- [CrossRef] [PubMed] [Google Scholar]
- Osteoarthritic changes after anterior cruciate ligament reconstruction using bone-patellar tendon-bone or hamstring tendon autografts: A retrospective, 7-year radiographic and clinical follow-up study. Arthroscopy. 2008;24:899-908.
- [CrossRef] [PubMed] [Google Scholar]
- Revision anterior cruciate ligament reconstruction: Three-to nine-year follow-up. Arthroscopy. 2005;21:418-23.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament revision reconstruction: Results in 107 patients. Am J Sports Med. 2008;36:851-60.
- [CrossRef] [PubMed] [Google Scholar]
- Inferior results after revision ACL reconstructions: A comparison with primary ACL reconstructions. Knee Surg Sports Traumatol Arthrosc. 2013;21:2011-8.
- [CrossRef] [PubMed] [Google Scholar]
- Revision anterior cruciate ligament reconstruction with doubled semitendinosus and gracilis tendons and lateral extra-articular reconstruction. J Bone Joint Surg Am. 2006;88:2373-9.
- [CrossRef] [PubMed] [Google Scholar]
- Revision of anterior cruciate ligament reconstruction with patellar tendon allograft and autograft: 2-and 5-year results. Arch Orthop Trauma Surg. 2012;132:867-74.
- [CrossRef] [PubMed] [Google Scholar]
- Medium to long-term follow-up after ACL revision. Knee Surg Sports Traumatol Arthrosc. 2012;20:166-72.
- [CrossRef] [PubMed] [Google Scholar]
- A cross-sectional study comparing the rates of osteoarthritis, laxity, and quality of life in primary and revision anterior cruciate ligament reconstructions. Arthroscopy. 2013;29:898-905.
- [CrossRef] [PubMed] [Google Scholar]
- Revision anterior cruciate ligament reconstruction with hamstring tendon autograft: 5-to 9-year follow-up. Am J Sports Med. 2006;34:1604-14.
- [CrossRef] [Google Scholar]
- Revision anterior cruciate ligament reconstruction using a 2-stage technique with bone grafting of the tibial tunnel. Am J Sports Med. 2005;33:1701-9.
- [CrossRef] [PubMed] [Google Scholar]
- Revision arthroscopically assisted anterior cruciate ligament reconstruction with previously unharvested ipsilateral autografts. Am J Sports Med. 2004;32:1833-41.
- [CrossRef] [PubMed] [Google Scholar]
- Revision anterior cruciate ligament reconstruction with a reharvested ipsilateral patellar tendon. Am J Sports Med. 2001;29:746-50.
- [CrossRef] [PubMed] [Google Scholar]
- Femoral tunnel malposition in ACL revision reconstruction. J Knee Surg. 2012;25:361-8.
- [CrossRef] [PubMed] [Google Scholar]
- Revision anterior cruciate ligament reconstruction. Sports Health. 2014;6:504-18.
- [CrossRef] [PubMed] [Google Scholar]
- Revision ACL reconstruction using autogenous patellar tendon graft. Knee Surg Sports Traumatol Arthrosc. 2000;8:290-5.
- [CrossRef] [PubMed] [Google Scholar]
- Revision ACL reconstruction using contralateral hamstrings. Knee Surg Sports Traumatol Arthrosc. 2013;21:690-5.
- [CrossRef] [PubMed] [Google Scholar]
- Revision anterior cruciate ligament surgery. A review of the literature and results of our own revisions. Scand J Med Sci Sports. 2001;11:163-9.
- [CrossRef] [PubMed] [Google Scholar]
- Loss of motion after anterior cruciate ligament reconstruction. Am J Sports Med. 1992;20:499-506.
- [CrossRef] [PubMed] [Google Scholar]
- Revision anterior cruciate ligament reconstruction. J Knee Surg. 2004;17:127-32.
- [CrossRef] [PubMed] [Google Scholar]
- Integration of hamstring tendon graft with bone in reconstruction of the anterior cruciate ligament. Arthroscopy. 1997;13:641-3.
- [CrossRef] [Google Scholar]
- Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med. 1990;18:292-9.
- [CrossRef] [PubMed] [Google Scholar]







