Translate this page into:
Comparative effects of dry needling and instrument-assisted soft-tissue mobilization on hamstring tightness in patients with posterior pelvic tilt: A pilot study
*Corresponding author: Urooj Manzoor, Department of Physical Therapy, Tres Jolie Medical Center, Fujierah, UAE. uroojsgd2@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Manzoor U, Ilyas M, Kemall F, Ahmed SM. Comparative effects of dry needling and instrument-assisted soft-tissue mobilization on hamstring tightness in patients with posterior pelvic tilt: A pilot study. J Musculoskelet Surg Res. 2024;8:395-402. doi: 10.25259/JMSR_157_2024
Abstract
Objectives:
The objective of this study was to compare the impacts of dry needling (DN) and instrument-assisted soft-tissue mobilization on hip flexion, active knee extension (AKE), and posterior pelvic tilt (PPT) in participants with hamstring tightness.
Methods:
A randomized clinical pilot study was conducted at the District Headquarter Hospital and tertiary hospitals in the District Nankana Sahib, Pakistan. The study’s sample size was 36, and participants were randomized equally into two treatment groups. Group A received DN, and Group B underwent treatment with instrument-assisted soft-tissue mobilization. Hamstring tightness was assessed using an inclinometer to measure the range of motion for AKE and bilateral straight leg raise (BSLR). PPT was measured using an inclinometer at baseline and after treatment of four weeks.
Results:
Both groups showed a significant disparity in the mean of pre-and post-treatment values (P < 0.05) of AKE, BSLR, and PPT. A statistically significant disparity was found between both groups on AKE, BSLR, and PPT (P < 0.05) post-treatment of 4 weeks.
Conclusion:
Both DN and instrument-assisted soft-tissue mobilization were found to be beneficial for enhancing hamstring flexibility by improving hip and knee joint mobility. On the other hand, instrument-assisted soft-tissue mobilization was superior in increasing active knee extension, BSLR, and reducing PPT.
Keywords
Dry needling
Hamstring flexibility
Instrument-assisted soft-tissue mobilization
Posterior pelvic tilt
Tightness
INTRODUCTION
The hamstring muscle complex comprises three muscles that collaborate to move the hip and knee joints: semimembranosus, semitendinosus, and biceps femoris. They start at the hips and extend toward the knee joint on the back of the leg.[1] One study revealed that hamstring tightness was found to be present in 44% of female college students on the right side, and 27.5% of male students had significantly tight left hamstrings.[2] Females have a higher linear prevalence of tight hamstrings than males.[3]
Standing and forward flexion of the trunk are two crucial athletic activity postures that require anatomically correct pelvic position to preserve correct sagittal spine positioning. The posterior pelvic tilt (PPT) is caused by the hips, and the trunk flexes forward. Some authors claim that a structural imbalance brought on by weakened muscles and tension affects neutral lumbopelvic positioning and can result in lower crossing syndrome, spinal asymmetry, and low back pain (LBP). Consequently, several investigations have found that compared to patients without the condition, both athletes and non-athletes with LBP had a higher anterior pelvic tilt.[4,5] Besides limiting mobility, hamstring tightness can lead to several orthopedic issues, including hamstring strain, plantar fasciitis, and LBP. Muscle tightness impairs the hamstring muscles’ capacity to maintain a consistent length-tension connection and absorb force. This diminished flexibility results in a vicious circle of limited range of motion (ROM) and increasing postural abnormalities.[6,7]
Several methods have been recommended to treat hamstring tightness. It has been demonstrated that stretching activities, particularly eccentric training, enhance hamstring flexibility. Regular massage, physiotherapy, and kinesiotaping can also help relieve muscular tension and increase ROM.[8] Hamstring stretching enhances hamstring flexibility while simultaneously improving balance, resulting in a positive connection between hamstring stiffness and balance.[9,10] Nutrition is also important for muscular health. A protein-rich balanced diet with other necessary nutrients, as well as enough water, can assist in maintaining muscular flexibility and avoid tightness.[8]
The American Physical Therapy Association defines the technique of dry needling (DN) as an adept intervention for relieving neuromusculoskeletal pain and activity restrictions. It involves using a small filiform needle that can seep into the layer of skin and stimulate that underlies trigger points in the myofascial tissues, muscular, and connective tissues.[11] DN increases blood flow to tissue and reduces trigger points.[12] Instrument-assisted soft-tissue mobilization (IASTM) is a useful treatment intervention for various conditions affecting the spine, upper extremity, and lower extremity over a treatment period of <3 months to reduce pain and improve function.[13]
The present study aimed to evaluate and compare the effects of DN and IASTM on hip and knee ROM in patients with hamstring tightness presenting with PPT. A literature gap existed, lacking a robust comparison between DN therapy and IASTM for addressing tightness of the hamstring along with the PPT. Despite their known efficacy in musculoskeletal contexts, there was a scarcity of direct comparisons within the realm of PPT-related hamstring tightness. This gap posed a practical challenge for evidence-based clinical decision-making, leaving clinicians without definitive guidelines for selecting the most effective intervention. The present study aimed to fill this void by scrutinizing and comparing the impacts of DN and IASTM on PPT-related hamstring tightness, providing essential insights for optimized treatment strategies in this specific population.
MATERIALS AND METHODS
Study design and population
The study was a randomized clinical pilot study. The study was conducted at District Headquarter Hospital and tertiary hospitals in District Nankana Sahib, Pakistan. The study was completed in 9 months, from July 2023 to January 2024. The study’s participants were recruited using a convenient sampling technique and were divided into two groups by lottery method. The calculated sample size was 30 and was calculated using Epitool software.[14] With a 20% attrition rate, the final sample size was 36.
Selection criteria
Participants were screened as per the inclusion and exclusion criteria.
Inclusion criteria
Females and male sex, age 18–40 years, lack of ≥20° of supine active knee extension (AKE), passive SLR ≤75°, atraumatic back or knee pain ≥2 weeks, individuals who are willing to engage in the required therapy sessions and subsequent evaluations, and having PPT of 8.9±4.5° were included in the study.
Exclusion criteria
A history of a lumbar disc herniation or lumbar radiculopathy, any previous surgery of back, hip, or knee region, self-reported pregnancy, a history of active infection, or any blood-borne pathogens and infectious disorders, any known allergy to metals, an indication of ligamentous tear or positive instability tests, and an indication of meniscal tears or positive meniscal tear tests were excluded from the study.
Data collection procedure
Once the patients fulfilled the selection criteria listed above, all 32 participants were included in the study. Informed consent was obtained in written form from each participant before the treatment technique was performed. Participants were randomly allocated into Groups A and B using a lottery method. On the primary visit, patients were evaluated and assessed thoroughly. Hamstring tightness was assessed using an inclinometer to measure the ROM for AKE and BSLR. PPT was measured using an inclinometer before and after the 4-week treatment period.
Group A
The multimodal physical therapy program included hurdler hamstring stretch, extended triangular pose, and DN therapy using 50 mm or 60 mm-sized needles, depending on the person’s muscle bulk. The hamstring muscles presenting with tightness were treated with targeted DN. The patients were in the prone position. The hamstrings were manually palpated on both sides. Following palpation, a firm monofilament needle was inserted into the skin. The needle was then “pistoned” (inserted and withdrawn quickly into each point) multiple times without removing it completely from the skin to induce a localized twitch reaction. The fast in-fast out cone-shaped approach was used to perform DN on three different hamstring muscles of the lower limbs bilaterally, each for 1 min.[15,16]
Group B
The second group of participants underwent the same multimodal physical therapy approach, including hurdler hamstring stretch, extended triangular pose, and IASTM tools. The IASTM tools were utilized instead of DN. Subjects had been directed to lie down in a prone. To reduce friction, lubricant was applied. The orientation and shape of the hamstring muscle fibers determined the direction of the IASTM application. The IASTM was used from top to bottom in a longitudinal vertical motion. For about 10 s, light pressure was applied and then advancing strokes were increased to moderate pressure, with 10–30 s of localized treatment.[7]
Data collection tools
Inclinometer
The caliper-based inclinometer was used to measure PPT. To compensate for posture-related swinging, each participant stands with their feet on a 30 cm wide surface and is instructed to stare forward at a single place of reference. The subjects assumed an upright position with their weight evenly distributed and their forearms crossed over their chest, while the researcher felt the posterior superior iliac spine (PSIS) and anterior superior iliac spine (ASIS). The ASIS was initially palpated by moving the thumbs from lower to higher while focusing on the ASIS’s most noticeable bulge, which was labeled with a felt tip. The PSIS was then detected and labeled by first locating the iliac crest dorsally and then moving the thumbs upward and horizontally from the sacral edge to its most noticeable point. After palpating the labeled landmarks, the tips of the inclinometer caliper were placed over them. The angle generated by a horizontal line drawn between ASIS and PSIS was used to determine the standing pelvic tilt. To get an average, three readings were taken for each side.[17,18]
AKE test
Participants were lying down in a supine position to measure AKE. The hip joint was moved actively to 90°. Then, a crossbar was set to hold the hip at 90°. To guarantee isolated hip motion, their trunk was fastened to the table’s surface by a belt just proximal to the ASIS. The patients were instructed to extend their knee as much as possible while maintaining a 90° hip flexion. An inclinometer was placed immediately distal to the tibial tuberosity to measure the ROM of knee extension. The highest scores obtained were analyzed.[19,20]
Bilateral SLR test
Subjects were lying supine with a waist belt just proximal to the ASIS, with slack removed to prevent excessive pelvic rotation. The inclinometer was placed directly distal to the participant’s tibial tuberosity to measure hip flexion. The ROM was recorded and analyzed.[19,20]
Statistical analysis
The Statistical Package for the Social Sciences version 26 was used to enter and analyze data. The statistical significance was determined using a significance threshold of P = 0.05. Descriptive statistics are used to summarize measurements performed within and between groups over time. Before inferential analysis, the data’s normality was determined to decide whether parametric or non-parametric tests should be used.
The CONSORT flow diagram is described in Figure 1. According to protocol analysis, one dropout in Group A and two dropouts in Group B were managed.

- Consolidated standards of reporting trails (CONSORT) flow diagram.
RESULTS
Demographic data reveal that 44.4% of the study participants were male and 55.6% were female. The graphical representation of the age distribution is given in Figure 2. The mean age of the participants with hamstring tightness was 30.44 ± 7.27.
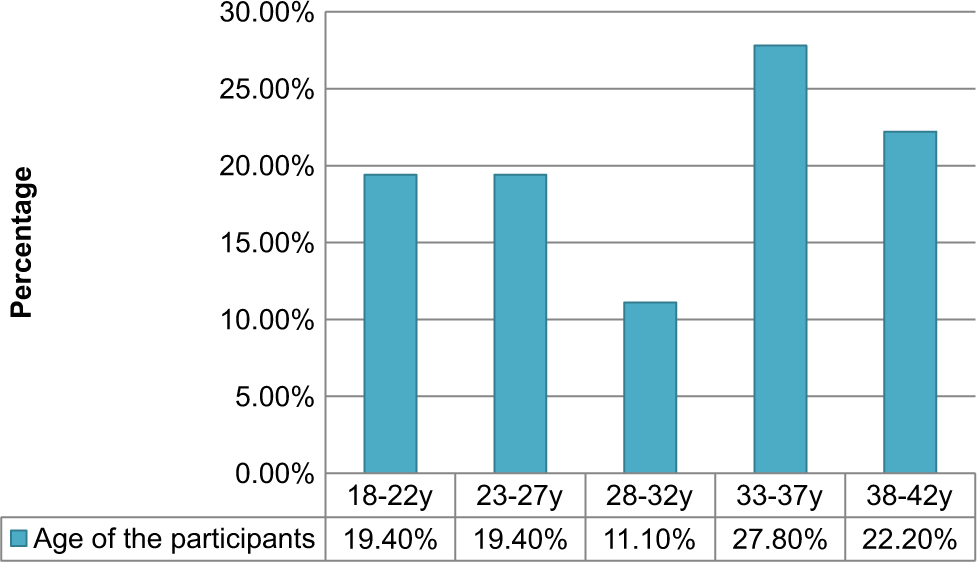
- Age distribution of study participants.
Within-group interpretation
The interpretation of the descriptive statistics and Wilcoxon signed-rank test of AKE and PPT within the group is shown in Table 1.
| n | Mean | Std. Deviation | Median | Asymp. Sig. (two-tailed) | |
|---|---|---|---|---|---|
| Dry needling (Group A) | |||||
| Right AKE at baseline | 18 | 21.94 | 2.01 | 21.00 | |
| Right AKE after 4 weeks | 17 | 11.70 | 1.64 | 12.00 | 0.00 |
| IASTM (Group B) | |||||
| Left AKE at baseline | 18 | 21.94 | 2.12 | 21.00 | 0.00 |
| Left AKE after 4 weeks | 17 | 11.88 | 1.83 | 12.00 | |
| Dry needling (Group A) | |||||
| Right AKE at baseline | 18 | 22.00 | 1.68 | 21.50 | |
| Right AKE after 4 weeks | 16 | 10.00 | 1.36 | 10.00 | 0.00 |
| IASTM (Group B) | |||||
| Left AKE at baseline | 18 | 22.22 | 2.01 | 22.00 | 0.00 |
| Left AKE after 4 weeks | 16 | 9.93 | 1.43614 | 10.00 | |
| Dry needling (Group A) | |||||
| PPT at baseline | 18 | 12.16 | 1.20 | 12.00 | |
| PPT after 4 weeks | 17 | 10.11 | 0.85 | 10.00 | 0.00 |
| IASTM (Group B) | |||||
| PPT at baseline | 18 | 11.88 | 1.13 | 12.00 | |
| PPT after 4 weeks | 16 | 9.25 | 1.00 | 9.00 | 0.00 |
AKE: Active knee extension, IASTM: Instrument-assisted soft-tissue mobilization, PPT: Posterior pelvic tilt, Asymp. Sig: Asymptotic Significance or p-value.
The statistical details and paired samples t-test of bilateral straight leg raise (BSLR) for individuals in Groups A and B are indicated in Table 2.
| n | Mean | Std. Deviation | Asymp. Sig. (two-tailed) | |
|---|---|---|---|---|
| Dry needling (Group A) | ||||
| Right SLR at baseline | 18 | 64.38 | 6.51 | 0.000 |
| Right SLR after 4 weeks | 17 | 76.94 | 6.50 | |
| Left SLR at baseline | 18 | 63.55 | 5.11 | 0.000 |
| Left SLR after 4 weeks | 17 | 79.88 | 3.96 | |
| IASTM (Group B) | ||||
| Right SLR at baseline | 18 | 63.83 | 5.20 | 0.000 |
| Right SLR after 4 weeks | 16 | 83.18 | 4.81 | |
| Left SLR at baseline | 18 | 64.61 | 5.23 | 0.000 |
| Left SLR after 4 weeks | 16 | 86.00 | 5.16 |
IASTM: Instrument-assisted soft-tissue mobilization, SLR: Straight leg raise, Asymp. Sig: Asymptotic Significance or p-value.
Between groups interpretation
The interpretation of the Mann–Whitney U-test statistics of AKE and PPT between Groups A and B is given below [Table 3].
| Right AKE at baseline | Right AKE after 4 weeks | |
|---|---|---|
| Mann–Whitney U | 151.500 | 56.000 |
| Wilcoxon W | 322.500 | 192.000 |
| Z | −0.340 | −2.984 |
| Asymp. Sig. (two-tailed) | 0.734 | 0.003 |
| Left AKE at baseline | Left AKE after 4 weeks | |
| Mann–Whitney U | 149.000 | 56.000 |
| Wilcoxon W | 320.000 | 192.000 |
| Z | −0.416 | −2.921 |
| Asymp. Sig. (two-tailed) | 0.677 | 0.003 |
| PPT at baseline | PPT after 4 weeks | |
| Mann–Whitney U | 144.000 | 72.000 |
| Wilcoxon W | 315.000 | 208.000 |
| Z | −0.602 | −2.407 |
| Asymp. Sig. (two-tailed) | 0.547 | 0.016 |
AKE: Active knee extension, PPT: Posterior pelvic tilt, Z value/Z score: represents how many standard deviations the observed U statistic is from the mean U under the null hypothesis, indicating the significance of the difference between the two groups, Asymp. Sig: Asymptotic Significance or p-value.
The test statistics of independent samples t-test BSLR are shown in Table 4.
| n | Mean | Std. Deviation | Asymp. Sig. (two-tailed) | |
|---|---|---|---|---|
| Right SLR at baseline | ||||
| Group A: DN | 18 | 64.38 | 6.51 | 0.77 |
| Group B: IASTM | 18 | 63.83 | 5.20 | |
| Right SLR after 4 weeks | ||||
| Group A: DN | 17 | 76.94 | 6.50 | 0.004 |
| Group B: IASTM | 16 | 83.18 | 4.81 | |
| Left SLR at baseline | ||||
| Group A: DN | 18 | 63.55 | 5.11 | 0.54 |
| Group B: IASTM | 18 | 64.61 | 5.23 | |
| Left SLR after 4 weeks | ||||
| Group A: DN | 17 | 79.88 | 3.96 | 0.001 |
| Group B: IASTM | 16 | 86.00 | 5.16 |
IASTM: Instrument-assisted soft-tissue mobilization, SLR: Straight leg raise, DN: Dry needling, Asymp. Sig: Asymptotic significance or p-value.
DISCUSSION
The present investigation found that both DN therapy and IASTM were useful for enhancing hamstring flexibility by improving hip and knee joint ROM. IASTM, on the other hand, was shown to be more beneficial in enhancing AKE, bilateral hip flexion, and decreasing PPT.
In 2023, Fayyiz et al. reported that IASTM substantially impacted pain, function, and mobility in individuals with knee osteoarthritis (OA).[21] In the present study, the targeted population was people with hamstring tightness and increased PPT. However, similar results were found in the present study. IASTM showed beneficial effects in improving AKE and hip flexion ROM. A study by Khan et al. found that functional DN can enhance hamstring length and improve functional activities.[22] In the present study, the effects of DN were compared with IASTM. Although DN was found to be effective in improving all outcomes of the study, IASTM was found to be more effective than DN in terms of improvement in AKE, BSLR, and PPT.
A study by Nazary-Moghadam et al. revealed that IASTM was just as efficient as hold-relax and muscle energy technique (MET) at enhancing hamstring muscular extensibility. Unlike proprioceptive neuromuscular facilitation and MET, which both have substantial energy needs and the possibility of muscular cramping, IASTM has none of these disadvantages.[23] Shah et al. found that IASTM is a better intervention for trigger point release than the active release technique because it results in a rise in ankle dorsiflexion and considerable pain relief.[24] In the present study, IASTM was compared with DN, and it was found to be more effective in improving the flexibility of hamstring muscle and PPT than DN. In line with the results of the present study, Gupta et al., in 2023, reported that when compared to stretching, IASTM with foot exercises or myofascial release method dramatically improves flexibility, foot posture, foot function, and dynamic balance, making it a therapy choice for patients with a flexible pronated foot.[25]
In the present study, IASTM was discovered to be more beneficial than DN in rising AKE, BSLR, and PPT. In support of these findings, in 2022, Ajmera and Patil revealed that the IASTM group fared considerably better in terms of increasing ROM, regaining the proper angle of costo-vertebral angle, and minimizing limitations in functioning.[26] Another research by Emshi et al. revealed that there was no significant disparity in pain intensity, pain pressure threshold, or neck impairment between the IASTM and DN. However, IASTM had greater results for improving active contralateral flexion of the cervical area. Both therapies were proven to be beneficial in individuals suffering from upper trapezius trigger points.[27] Similar results were seen in the present study, but the targeted muscle in the study was the hamstring muscle.
Doeringer et al. conducted a study on hamstring stiffness in 2022 with the goal of comparing the benefits of therapeutic cupping (TC) with IASTM. The study discovered that IASTM and TC both influenced hamstring mobility and had favorable results.[28] In the present study, when IASTM was compared with DN, IASTM was found to be more beneficial than DN in improving hamstring flexibility, ROM, and PPT.
One limitation of the study was the small sample size, which may have affected its generalizability. The data for this trial was collected from only the District Headquarter Hospital and tertiary hospitals in District Nankana Sahib, Pakistan. The long-term effects of interventions were not examined. Another limitation was the researcher’s limited control over external variables, such as patients engaging in additional therapies, activities, or home treatments outside the study protocol.
CONCLUSION
Both DN and IASTM were found to be efficient in increasing hamstring flexibility by improving the ROM of hip and knee joints in patients with hamstring tightness with PPT. IASTM was found to be more efficient in enhancing AKE and bilateral SLR and reducing PPT.
RECOMMENDATIONS
More research is needed to determine the long-term effects of interventions with a longer follow-up period beyond four weeks and a larger sample size. Therapists should incorporate these interventions into clinical practice for better outcomes in patients with hamstring stiffness.
ACKNOWLEDGMENT
We would like to thank all study participants who voluntarily participated.
AUTHORS’ CONTRIBUTION
UM was involved in conception and design. MI and FK contributed to data acquisition, data analysis, and statistical analysis. UM and FK was involved in clinical and experimental studies, UM and SMA contributed to literature research. SMA contributed to manuscript preparation, manuscript editing, and review. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The trial was registered on clinical trial.gov (Clinical trial number: NCT05931120). The study got approval from IRB and the research committee of Riphah International University Lahore campus with Ref. No REC/RCR & AHS/23/0149 on August 03, 2023.
DECLARATION OF PARTICIPANT CONSENT
The authors certify that they have obtained all appropriate participant consent forms. In the form, the participants have given their consent for their images and other clinical information to be reported in the journal. The participants understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Prevalence of hamstring tightness in physically active and inactive college going students. Research Square 2023
- [CrossRef] [Google Scholar]
- Hamstrings stiffness and landing biomechanics linked to anterior cruciate ligament loading. J Athl Train. 2013;48:764-72.
- [CrossRef] [Google Scholar]
- Prevalence and severity of hamstring tightness among college students: A cross sectional study. Int J Clin Biomed Res. 2018;4:65-8.
- [CrossRef] [Google Scholar]
- The potential role of hamstring extensibility on sagittal pelvic tilt, sagittal spinal curves and recurrent low back pain in team sports players: A gender perspective analysis. Int J Environ Res Public Health. 2021;18:8654.
- [CrossRef] [Google Scholar]
- Comparison of Q angle and tibial torsion among premier league futsal players with and without hamstring tightness. Phys Treat Spec Phys Ther J. 2016;6:51-8.
- [CrossRef] [Google Scholar]
- Evaluating the relationship between clinical assessments of apparent hamstring tightness: A correlational analysis. Int J Sports Phys Ther. 2019;14:253-63.
- [CrossRef] [Google Scholar]
- Instrument assisted soft tissue mobilization (IASTM) versus stretching: A comparison in effectiveness on hip active range of motion, muscle torque and power in people with hamstring tightness. J Bodyw Mov Ther. 2021;27:200-6.
- [CrossRef] [Google Scholar]
- Association of hamstring tightness with lower extremity injuries in athletes (analytical cross-sectional study) Pak J Med Health Sci. 2023;17:575.
- [CrossRef] [Google Scholar]
- The immediate effect of static hamstring stretching on dynamic balance and gait biomechanical variables in athletes with hamstring tightness: A preliminary study. J Modern Rehabil. 2021;15:141-50.
- [CrossRef] [Google Scholar]
- Comparison between static stretching and proprioceptive neuromuscular facilitation on hamstring flexibility: Systematic review and meta-analysis. Eur J Physiother. 2018;20:12-9.
- [CrossRef] [Google Scholar]
- Dry needling: A clinical commentary. Int J Sports Phys Ther. 2022;17:551-5.
- [CrossRef] [Google Scholar]
- Instrument assisted soft-tissue mobilization: A commentary on clinical practice guidelines for rehabilitation professionals. Int J Sports Phys Ther. 2019;14:670-82.
- [CrossRef] [Google Scholar]
- Comparative effect of Graston technique and muscle energy technique on the flexibility of hamstring muscle. Int J Clin Skills. 2022;16:255.
- [Google Scholar]
- The effectiveness of dry needling and stretching vs. stretching alone on hamstring flexibility in patients with knee pain: A randomized controlled trial. Int J Sports Phys Ther. 2016;11:672-83.
- [CrossRef] [Google Scholar]
- Acute and short-term effects of dry needling in patients with chronic nonspecific low back pain and hamstring tightness: A pilot study. Scientific World Journal. 2021;2021:7259956.
- [CrossRef] [Google Scholar]
- Effect of muscle energy technique v/s static stretching on tight hamstring muscles length and pelvic inclination amongst asymptomatic adults. Int J Acad Res Dev. 2020;5:31-5.
- [Google Scholar]
- Assessment of the degree of pelvic tilt within a normal asymptomatic population. Man Ther. 2011;16:646-8.
- [CrossRef] [Google Scholar]
- Effect of core stability exercises versus Surya Namaskar on hamstring tightness in healthy adults using active knee extension test at the end of 6 weeks: A comparative study. IJAR. 2020;6:386-90.
- [Google Scholar]
- Acute and residual effects of IASTM and roller massage stick on hamstring range of motion. J Allied Health. 2020;49:e51-5.
- [Google Scholar]
- Effectiveness of instrument assisted soft tissue mobilization technique on hamstring flexibility in patients with knee osteoarthritis-a non-randomized trial. Ann Punjab Med Coll. 2023;17:84-7.
- [Google Scholar]
- Immediate effect of functional dry needling on the length of shortened hamstring muscle; a quasi-experimental study. J Riphah Coll Rehabil Sci. 2023;11
- [CrossRef] [Google Scholar]
- Comparison of utilizing modified hold-relax, muscle energy technique, and instrument-assisted soft tissue mobilization on hamstring muscle length in healthy athletes: Randomized controlled trial. J Bodyw Mov Ther. 2023;35:151-7.
- [CrossRef] [Google Scholar]
- Comparison between the immediate effects of instrument assisted soft tissue mobilization and active release technique in individuals wearing high heels. Int J Health Sci Res. 2021;11:186-95.
- [CrossRef] [Google Scholar]
- Instrument-assisted soft tissue mobilization technique versus static stretching in patients with pronated dominant foot: A comparison in effectiveness on flexibility, foot posture, foot function index, and dynamic balance. Healthcare. 2023;11:785.
- [CrossRef] [Google Scholar]
- Effect of dry needing and IASTM in chronic upper trapezitis: A randomised controlled trial. IJPTRS. 2022;1:1-11.
- [Google Scholar]
- Comparison of the effects of instrument assisted soft tissue mobilization and dry needling on active myofascial trigger points of upper trapezius muscle. Med J Islam Repub Iran. 2021;35:59.
- [CrossRef] [Google Scholar]
- Instrument-assisted soft tissue mobilization increased hamstring mobility. J Sport Rehabil. 2023;32:165-9.
- [CrossRef] [Google Scholar]







