Translate this page into:
Comparative evaluation of proximal femoral nail anti-rotation versus dynamic hip screw for stable intertrochanteric femoral fractures: A meta-analysis of clinical outcomes
*Corresponding author: Edi Mustamsir, Department of Orthopaedic and Traumatology, Faculty of Medicine, Brawijaya University, Saiful Anwar State General Hospital, Malang, East Java, Indonesia. edimustamsir@ub.ac.id
-
Received: ,
Accepted: ,
How to cite this article: Mustamsir E, Aji AP, Fernando A. Comparative evaluation of proximal femoral nail anti-rotation versus dynamic hip screw for stable intertrochanteric femoral fractures: A meta-analysis of clinical outcomes. J Musculoskelet Surg Res. 2024;8:335-48. doi: 10.25259/JMSR_141_2024
Abstract
In this study, a meta-analysis was conducted to compare the efficacy of proximal femoral nail anti-rotation (PFNA) and dynamic hip screw (DHS) as the treatment of stable intertrochanteric femoral fractures (AO type 31-A1). The comparison was focused on perioperative outcomes, Harris hip scores (HHSs), and major orthopedic complications. PubMed, Cochrane, ProQuest, and ScienceDirect were searched for studies comparing PFNA and DHS for stable intertrochanteric femoral fractures. The authors conducted separate screenings to determine eligible studies for this meta-analysis. The risk of bias was assessed using the Risk of Bias Tool for Randomized Trials 2 and the Risk of Bias in Non-randomized Studies–of Interventions-I. All outcomes were analyzed using Review Manager software version 5.4 and presented as forest plots. Ten studies were included in this analysis (three randomized controlled trials and seven observational studies) with 1149 patients. For the intraoperative parameters, PFNA had shorter mean operative time (mean difference [MD] −18.63, 95% interval [CI] [−27.92–−9.34], P < 0.0001) and led to less intraoperative blood loss (MD −88.84, 95% CI [−158.03–−19.65], P = 0.01). No significant differences in HHSs and complications were found between PFNA and DHS, and leg length discrepancy (risk ratio 0.40, 95% CI [0.17–0.92], P < 0.03) favoring PFNA. Overall, these two surgical methods have no meaningful differences in long-term functional outcomes and complications. The PFNA may be more beneficial in the perioperative aspect, including shorter surgical duration and lesser blood loss due to its minimally invasive nature.
Keywords
Anti-rotation
Dynamic hip screw
Intertrochanteric fractures
Meta-analysis
Proximal femoral nail
Stable
INTRODUCTION
Intertrochanteric femoral fractures are proximal femur fractures between the greater and lesser trochanters.[1] Most of these fractures often result from low-impact trauma due to falls in elderly individuals with weakened bones. These fractures can vary in stability depending on the fracture fragments’ displacement and alignment. According to the newest AO fracture classification, A1 is considered stable intertrochanteric fractures, while unstable intertrochanteric fractures are classified into A2 and A3.[2]
Surgery is still the primary treatment for intertrochanteric fractures. Many clinicians use extramedullary or intramedullary fixations as the main treatment for the intertrochanteric fracture.[3] This device works based on the tension band principle and permits the screw to slide within the barrel to enable dynamic compression of the fracture when the patient begins to bear weight. This compression promotes fracture healing.[4,5] In contrast, proximal femoral nail anti-rotation (PFNA) is an intramedullary nail that is inserted into the intramedullary canal of the femur. The PFNA was introduced in early 2003 after its development from the previous conventional proximal femoral nail (PFN), which was first introduced in 1996. The main difference lies in the design and mechanism, usually in the form of a helical blade or threaded screw. This design engages with the femoral head to resist rotation and promote stability more effectively.[6]
The DHS has traditionally been regarded as the primary method for stabilizing intertrochanteric fractures. However, several experts now believe intramedullary implants such as PFNA to be the most reliable and widely accepted approach.[4] The American Academy of Orthopedic Surgeons guidelines recommend either extramedullary or intramedullary fixation for stable fractures and only intramedullary fixation for unstable fractures.[7,8]
Multiple published literature have supported and advocated using PFNA over DHS to treat unstable fractures, indicating its superiority.[3,9-11] However, comparing these two fixation methods is not established for stable fractures, as such fractures can be easily overlooked. Moreover, in recent years, more orthopedic surgeons have favored the newer PFNA devices over DHS in managing stable intertrochanteric fractures.[12] This meta-analysis aimed to compare the functional outcomes using Harris hip scores (HHSs) between PFNA and DHS in treating stable intertrochanteric fractures (according to AO classification). In addition, the study examined whether there are any differences between the major orthopedic complications and the perioperative outcomes when using the PFNA or the DHS.
MATERIALS AND METHODS
Search strategy
This study followed the protocols outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement.[13] The study protocol was registered at the International Prospective Register of Systematic Reviews (CRD42024532329) before conducting this study. PubMed, Cochrane, ProQuest, and ScienceDirect were searched for relevant studies before April 2024. The search was conducted utilizing the Medical Subject Headings (MeSH) terms, combined with free words: (“PFNA” or “proximal femoral nail anti-rotation”), (“DHS” or “dynamic hip screw”), (“Stable intertrochanteric fractures” or “Stable extracapsular hip fractures” or “Stable trochanteric fractures” or “Stable peritrochanteric fractures”). A flowchart summarizes the details of the selection process, as depicted in Figure 1.
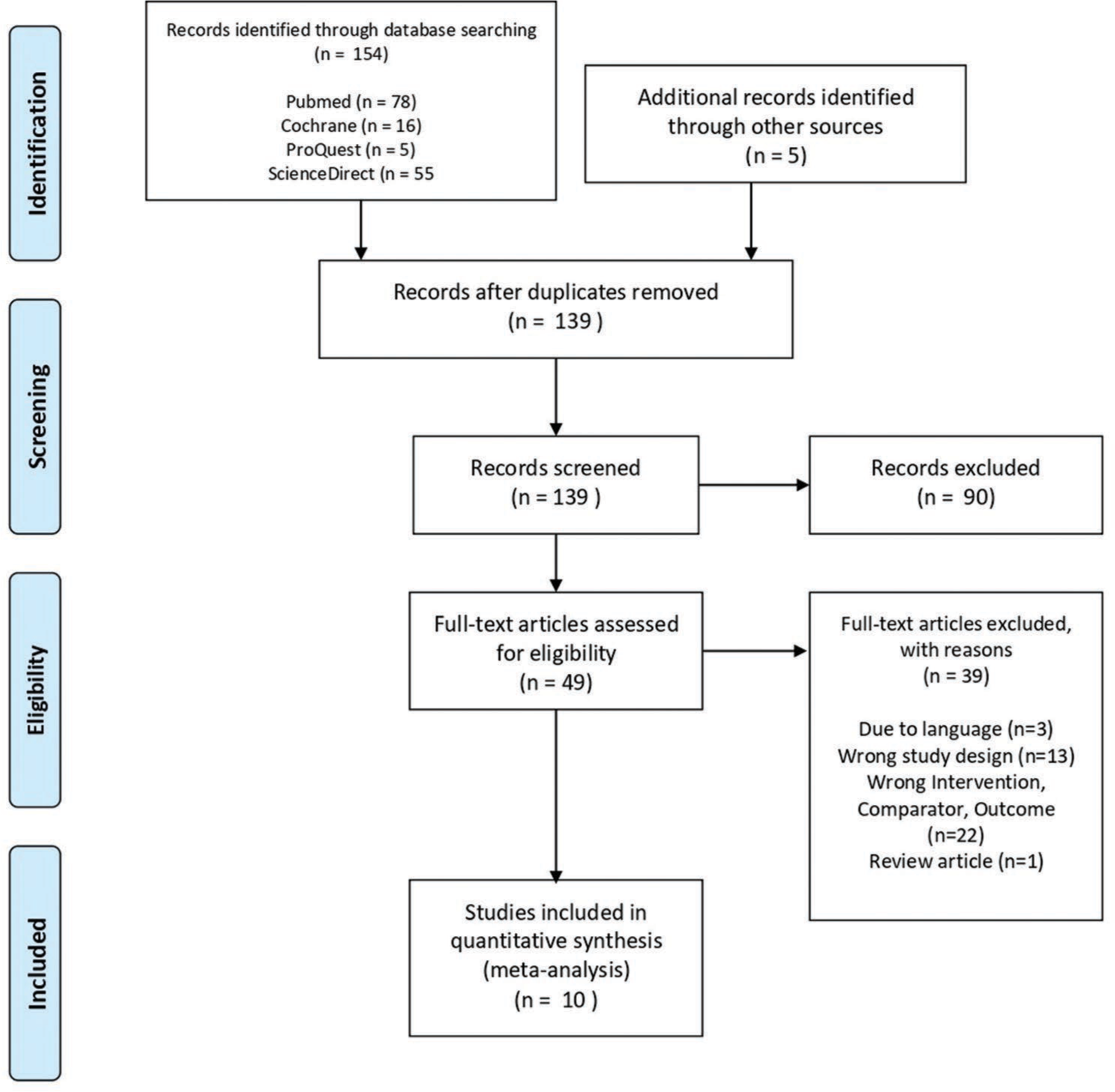
- Flowchart of search results, article inclusion, and exclusion.
Inclusion and exclusion criteria
Relevant articles, including prospective, randomized controlled trials (RCTs), or comparative observational studies, were manually screened using the Population, Intervention, Comparator, and Outcomes framework:
Population: Stable intertrochanteric fractures according to AO (AO type 31-A1)
Intervention: PFNA
Comparator: DHS
Outcomes: Functional outcome in HHS, major orthopedic complications (including implant failure, re-operation, infection, union problems, and other complications), or perioperative outcome (mean operation time and mean blood loss).
Studies were included in the analysis, with at least one of the clinical outcomes described above comparing the treatment of PFNA and DHS to stable intertrochanteric fracture (AO type 31-A1). Studies were excluded if they were as follows:
Included periprosthetic fractures
Included patients <18 years old
Included pathological fractures
Did not make a distinction between stable and unstable fractures
Used other fracture classification schemes (for example, EVANS or Jensen Classifications)
Review articles, biomechanical research, cadaver studies, animal trials, case reports, editorials, reviews, guidelines, and conference abstracts.
Data extraction
Data was extracted independently by authors according to the inclusion and exclusion criteria explained above. Any disagreements during this step were resolved by team consensus. The extracted primary data are summarized in Table 1. Some of the reported data presented in this study, which has several shortcomings, including standard deviation (SD) values that were not described sufficiently in the main articles. This happens to the SD values of the HHS in Sevinc et al.[14] and the SD values of mean operation time, mean blood loss, and HHS in Rathva et al. and Sharma et al.[15,16] To address this issue, corresponding authors were contacted through electronic mail (except for Sharma et al. due to missing address).[16] If this method was unsuccessful, missing SD values were imputed based on the pooled SD across all studies with no missing data.[17,18]
| Study (Publication date) | Study design | Inclusion period | Total population of stable fracture | PFNA | DHS | Mean age (years) | Follow-up (months) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of patient | % Male | % Female | Number of patient | % Male | % Female | ||||||
| Singh et al. 2019[19] | RCT | 2014–2016 | 49 | 24 | 30.00 | 70.00 | 25 | 53.33 | 46.67 | 71.0 | 12 |
| Zou et al. 2009[20] | RCT | 2006–2007 | 94 | 42 | 21.00a | 79.00a | 52 | 24.00a | 76.00a | 65.0a | 12 |
| Rathva et al. 2018[15] | RCT | 2015–2017 | 60 | 30 | ND | ND | 30 | N | ND | ND | 6 |
| Sharma et al. 2018[16] | Prospective Cohort | 2011–2014 | 60 | 31 | 60.67 | 39.33 | 29 | 65.51 | 34.49 | 61.70 | 12 |
| Yu et al. 2016[21] | Retrospective Cohort | 2005–2015 | 222 | 110 | 46.36 | 53.64 | 112 | 50.89 | 49.11 | 72.60 | 53 |
| van der Sijp et al. 2021[22] | Prospective Cohort | 2016–2018 | 126 | 94 | 24.20 | 75.80 | 32 | 28.10 | 71.90 | 81.20 | 9.8 |
| Cho and Lee, 2016[23] | Retrospective Cohort | 2004–2014 | 194 | 81 | 81.00 | 19.00 | 113 | 38.10 | 61.90 | 82.60 | 25.05 |
| Sevinc et al. 2020[14] | Prospective Cohort | ND | 64 | 16 | 48.21a | 51.79a | 48 | 59.10a | 40.90a | 78.00a | 12 |
| Tian and Wang, 2018[24] | Retrospective Cohort | 2013–2017 | 58 | 38 | 73.10 | 26.90 | 20 | 40.00 | 60.00 | 69.40 | 24 |
| Zeng et al. 2017[25] | Retrospective Cohort | 2007–2011 | 222 | 110 | 36.36 | 63.64 | 112 | 40.18 | 59.82 | 74.80 | 38 |
PFNA: Proximal femoral nail anti-rotation, RCT: Randomized controlled trials, DHS: Dynamic hip screw, ND: Not described. aValue for the total study population, including stable and unstable fracture
Quality assessment and risk of bias
Three authors independently assessed all studies for the risk of bias (EM, AP, and AF). This assessment was done according to the Cochrane Handbook for Systemic Intervention (v6.4). Cochrane Risk of Bias for Randomized Trials (ROB-2) is used for RCT assessment, while Cochrane Risk of Bias in Non-randomized Studies–of Interventions (ROBINS-I) was used for non-RCT studies.[17]
Each result from ROB-2 and ROBINS-I was inserted in the Robvis-Visualization tool to summarize the bias and risk of bias plot. Team consensus resolved any disagreements during this step.
Statistical analysis
All outcomes were statistically analyzed using Review Manager software version 5.4. Mean difference (MD) with 95% confidence intervals (CI) was used as effect sizes for functional HHS and perioperative data (mean operative time and mean blood loss). This continuous data outcome was pooled using an inverse variance weighting method. Meanwhile, risk ratio (RR) with 95% confidence intervals (CI) was used as effect size for major orthopedic complications, including implant failure, union problems, cut-out/protrusion rate, and infection. Cochran–Mantel– Haenszel statistic was used for this dichotomous data.
Forest plots were used to present all analyses. Subgroup analyses were independently applied to RCTs and observational studies. A fixed-effects model was used for meta-analysis if there was low heterogeneity among studies (P > 0.1 or I2 < 50%). A random-effects model was used instead if the results were the opposite. Statistical significance was assumed using P-value threshold of 0.05. To enhance the robustness, sensitivity analysis was performed by excluding one study at a time and the analysis was repeated without that particular study.
RESULTS
Study selection and baseline study characteristics
Initially, 159 articles were identified as potentially relevant. After removing duplicates, 139 articles remained, and the preliminary screening further excluded 90 irrelevant studies. After thoroughly examining the full text, 39 of 49 articles were further excluded, resulting in ten eligible studies published between 2009 and 2020, with an inclusion period from 2005 to 2018 for detailed evaluation. All studies comprised 1149 patients, with 203 patients from three RCT studies[19-21] and 946 patients from seven observational studies.[22-28] Patients were relatively equally distributed between the PFNA group (n = 576 patients) and the DHS group (n = 573 patients). The follow-up ranged from 6 to 53 months. A complete overview of the studies is shown in Table 1.
Risk of bias assessment
The risk of bias was assessed according to ROB-2 for RCTs and ROBINS-1 for observational studies [Figures 2 and 3]. For RCT, three studies scored moderately in measuring the outcomes. This happened because blinding participants who had the operation was almost impractical. Only one RCT study stated the allocation concealment method. For observational studies, almost all were judged to have a moderate risk of bias, with the exception of two studies, as they did not control the confounding and possible selection of participants.
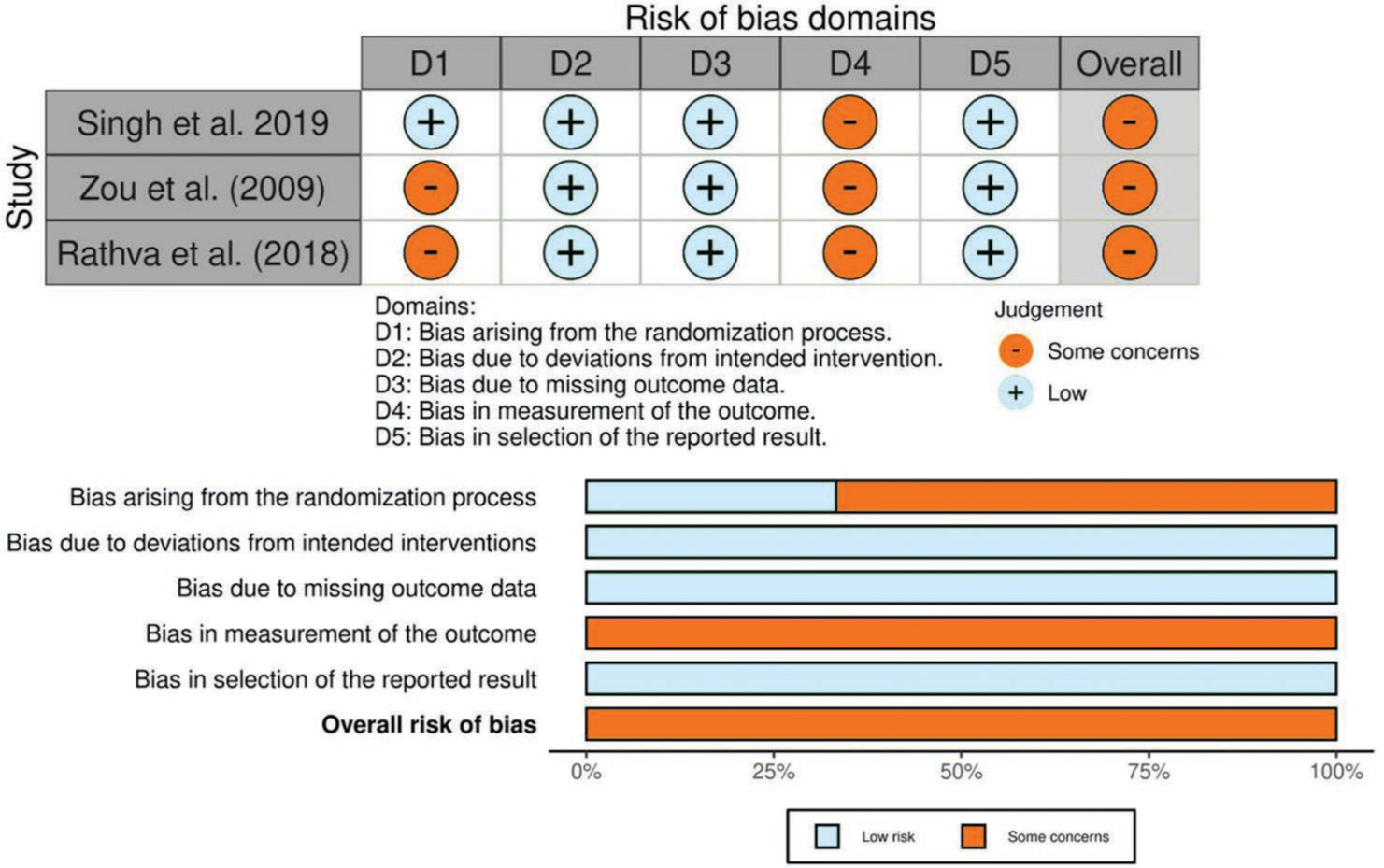
- Risk of bias assessment of RCT studies using ROB-2 Criteria. RCT: Randomized controlled trials, ROB-2: Risk of bias for randomized trials.
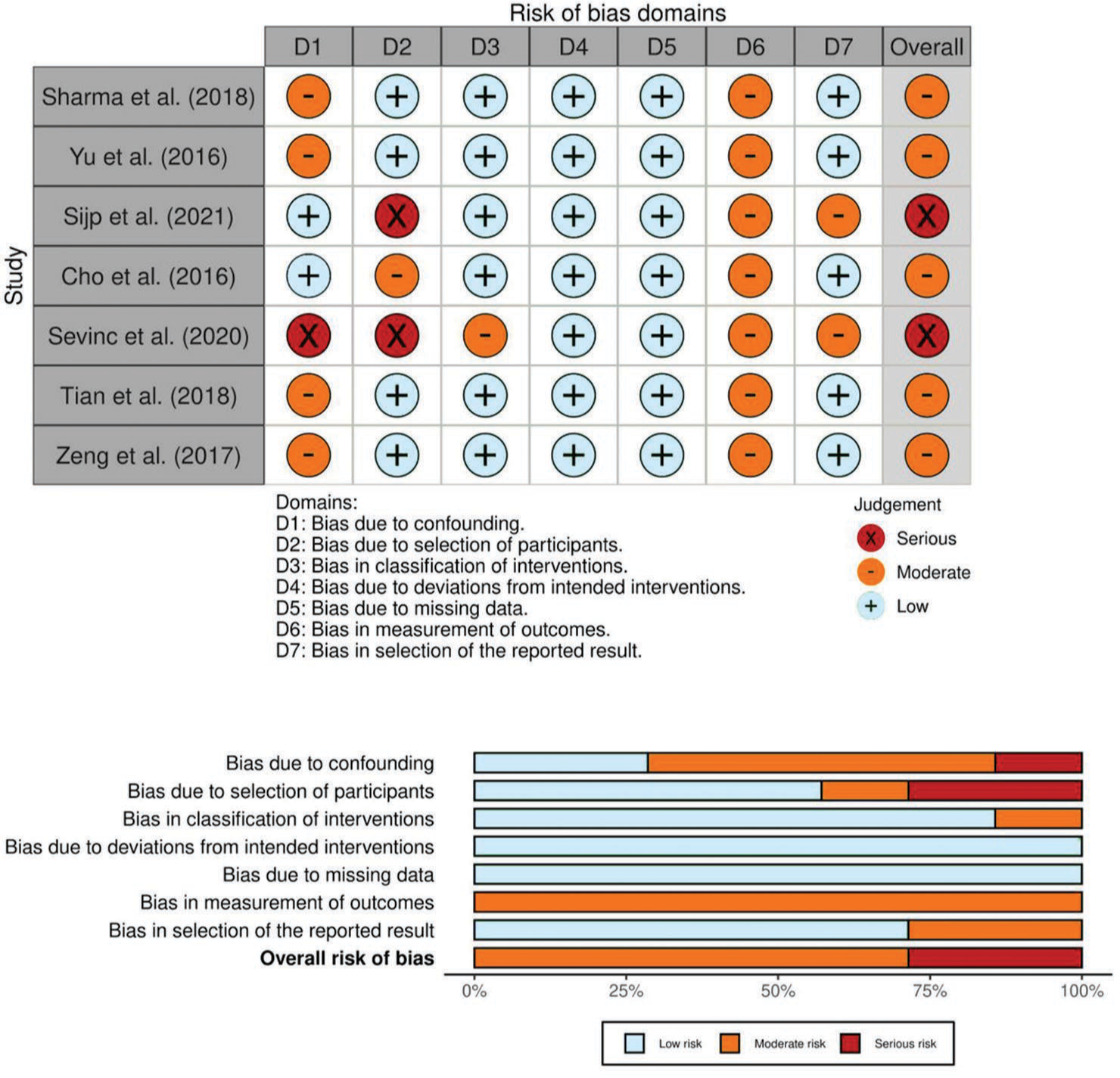
- Risk of bias assessment of observational studies using ROBIN-1 Criteria. ROBIN-1: Risk of bias in non-randomized studies–of interventions.
Primary outcome: Functional score
HHS in three months
HHS, in a three-month period, was reported in four studies (one RCT and three observational studies). A random-effects model was used due to the high level of heterogeneity (I2 = 97%, and P < 0.00001). The mean HHS for PFNA was 76.8 for 281 patients, and for DHS was 76.6 for 283 patients. Analysis of the forest plot showed no significant difference in the three months HHS between PFNA and DHS (MD 0.23, 95% CI [−2.85–3.31], P = 0.88) [Figure 4].
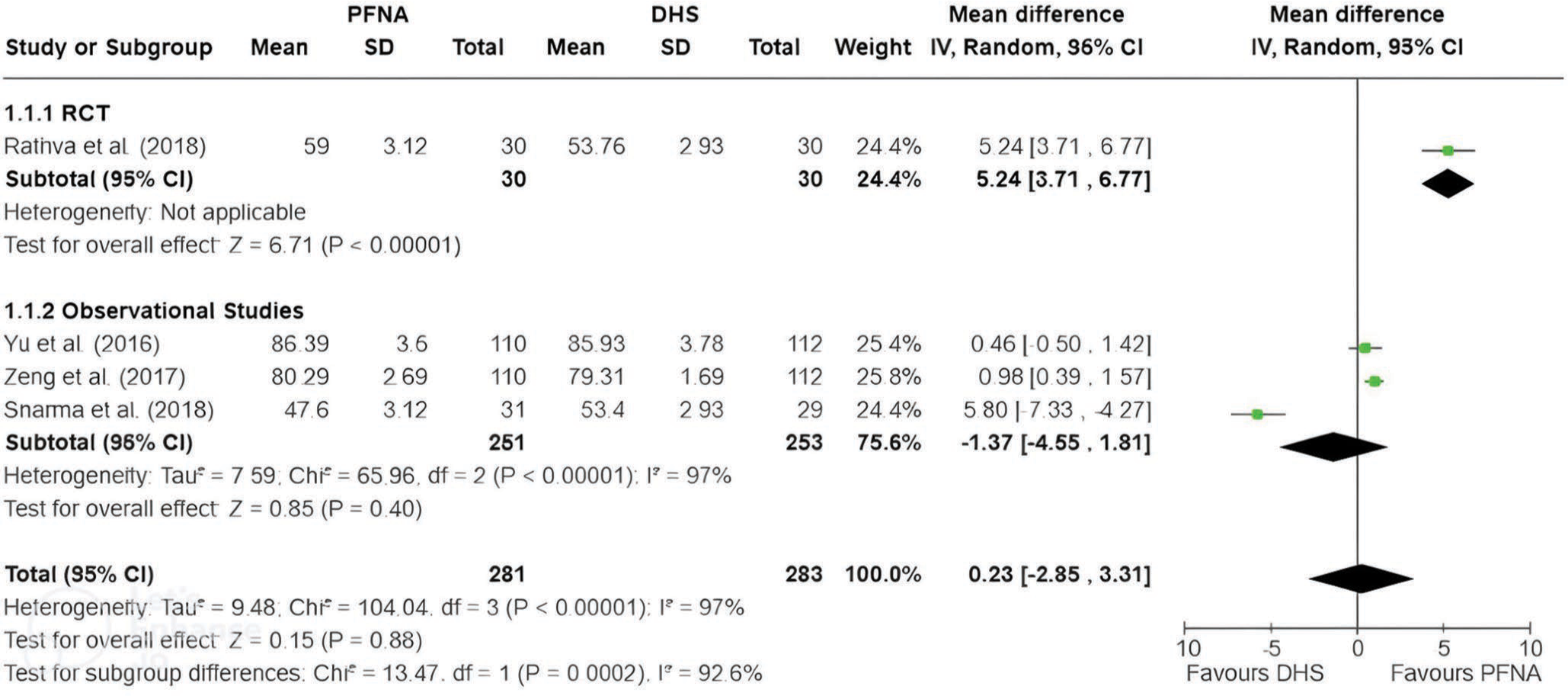
- Harris hip scores at three months showed no significant difference between PFNA and DHS. Bold values indicate statistically significant results with a P-value <0.05. PFNA: Proximal femoral nail anti-rotation, SD: Standard deviation, DHS: Dynamic hip screw, IV: Inverse variance, CI: Confidence interval, RCT: Randomized controlled trial, df: Degrees of freedom.
After conducting sensitivity analysis using the, we observed some shifts in the direction of the pooled effect size estimate by excluding specific studies. However, P-value remained insignificant in every study’s exclusion despite this change. The conclusion regarding the comparison between HHS in three months between the two treatments remained consistent, indicating that the studies included in the analysis were robust.
HHS in six months
The HHS in six months was reported in five studies (one RCT and four observational studies). A random-effects model was used due to high levels of heterogeneity (I2 = 96%, and P < 0.00001). The mean HHS for PFNA was 83.6 for 225 patients, and for DHS was 85.7 for 239 patients. Analysis of the forest plot showed no significant difference in the six months HHS between PFNA and DHS (MD −3.28, 95% CI [−7.66–1.09], P = 0.14) [Figure 5].
- Harris hip scores at six months showed no significant difference between PFNA and DHS. Bold values indicate statistically significant results with a P-value <0.05. PFNA: Proximal femoral nail anti-rotation, SD: Standard deviation, DHS: Dynamic hip screw, IV: Inverse variance, CI: Confidence interval, RCT: Randomized controlled trial, df: Degrees of freedom.
Sensitivity analysis showed that one RCT study (Rathva et al. 2018)[15] substantially influenced the statistical significance of the association between treatment and HHS in six months. While most sensitivity analyses maintained a non-significant P-value, excluding the RCT study resulted in a notable decrease in P-value (MD −5.11, 95% CI [−9.34–−0.88], P = 0.02), indicating a statistically significant result (P < 0.05) in favor of DHS treatment.
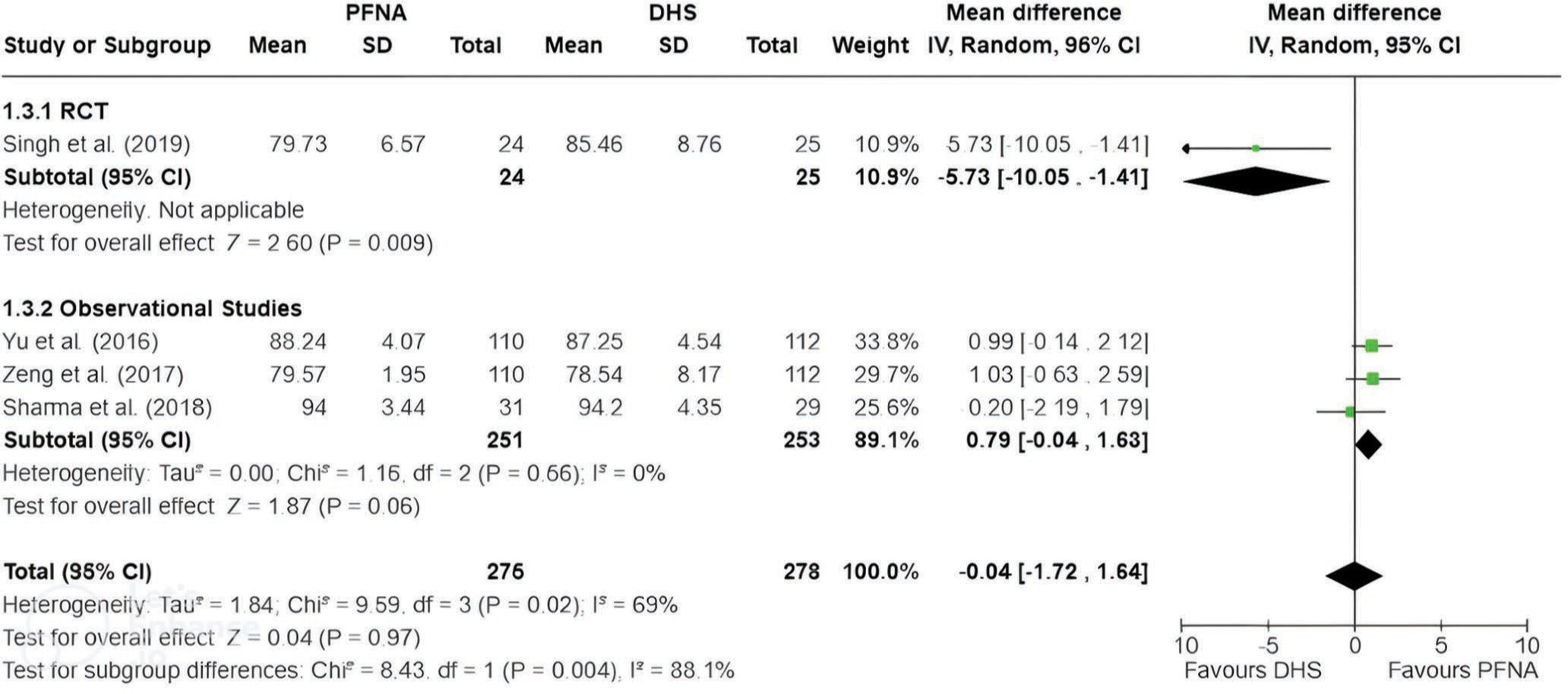
HHS in 12 months
HHS in 12 months was reported in four studies (one RCT and three Observational studies). A random-effects model was used due to a substantial level of heterogeneity (I2 = 69%, and P < 0.02). The mean HHS for PFNA was 84.7 for 275 patients, and for DHS was 84.3 for 278 patients. Analysis of the forest plot showed no significant difference in the 12 months HHS between PFNA and DHS (MD −0.04, 95% CI [−1.72–1.64], P = 0.97) [Figure 6].
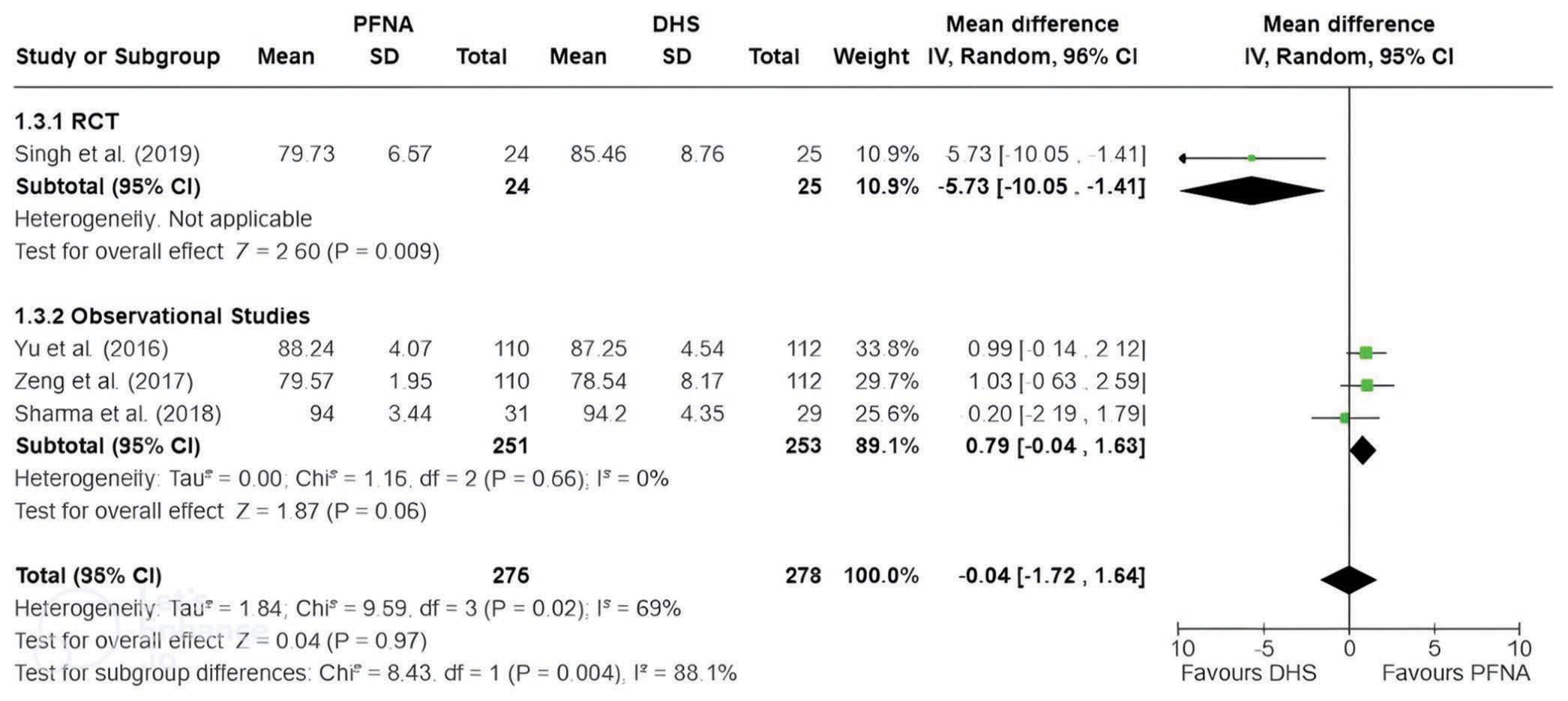
- Harris hip scores at 12 months showed no significant difference between PFNA and DHS. Bold values indicate statistically significant results with a P-value <0.05. PFNA: Proximal femoral nail anti-rotation, SD: Standard deviation, DHS: Dynamic hip screw, IV: Inverse variance, CI: Confidence interval, RCT: Randomized controlled trial, df: Degrees of freedom.
Sensitivity analysis also showed that another RCT study (Singh et al. 2019)[19] substantially influenced the statistical significance and heterogeneity of the association between treatment and HHS in 12 months. Excluding the RCT study resulted in a notable decrease in P-value to 0.06, approaching statistical significance favoring PFNA. The heterogeneity of the studies decreased from 69% to 0% while maintaining the pooled effect size direction at 0.79 (95% CI: −0.04–1.63). This meta-analysis also confirms the role of the RCT study in affecting the overall conclusions.
Secondary outcomes: Complications
Implant failure
Implant failure was reported in ten studies (three RCTs and seven observational studies). Implant failure occurred in nine out of 576 cases (1.6%) in PFNA treatment and 20 out of 573 cases (3.5%) in DHS treatment. A random-effects model was used due to a substantial level of heterogeneity (I2 = 59%, and P = 0.02). Analysis of the forest plot showed no significant difference in implant failure rate between PFNA and DHS (RR 0.60, 95% CI [0.14–2.55], P = 0.49) [Figure 7].
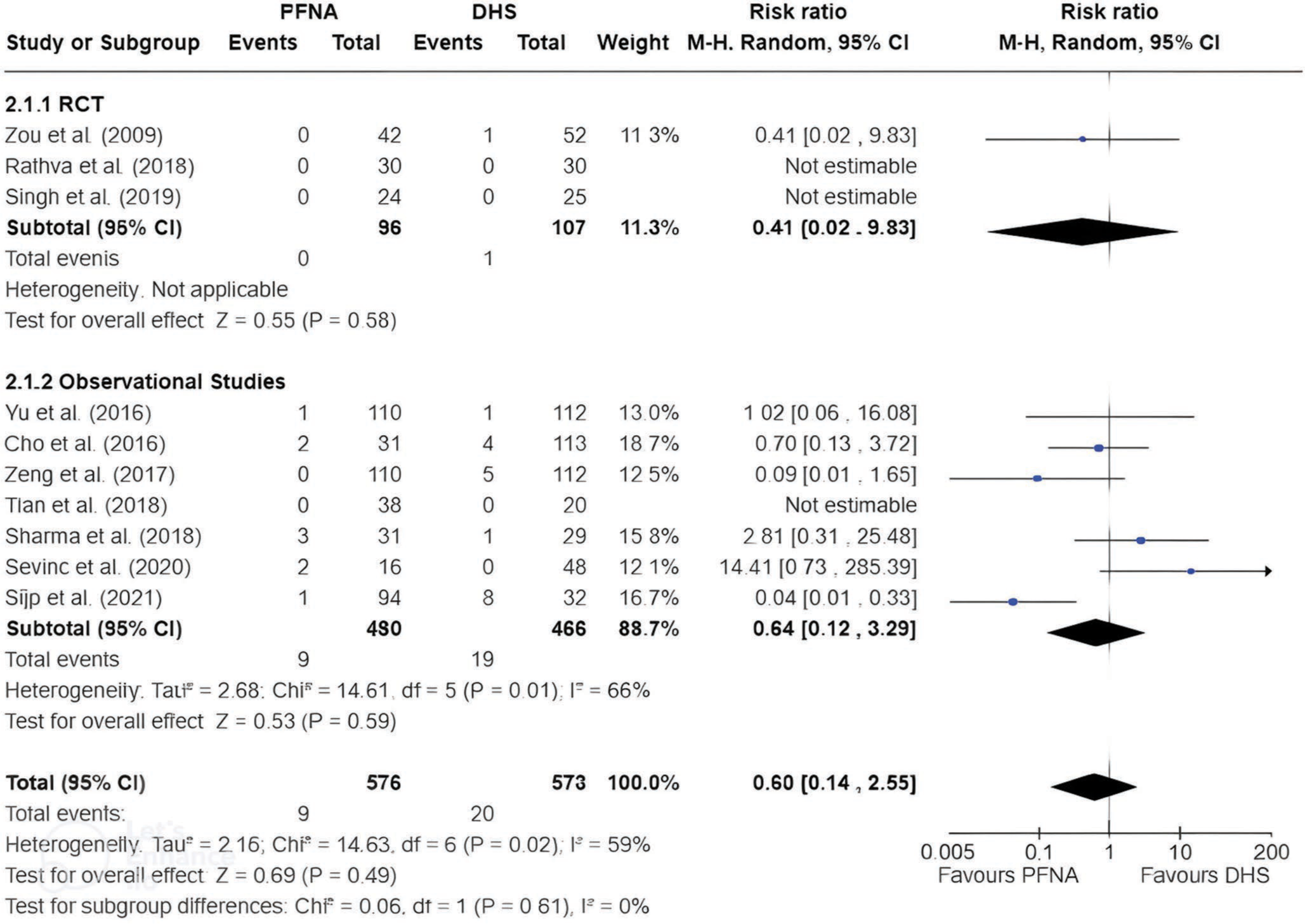
- Implant failure rates showed no significant difference between PFNA and DHS. Bold values indicate statistically significant results with a P-value <0.05. PFNA: Proximal femoral nail anti-rotation, SD: Standard deviation, DHS: Dynamic hip screw, CI: Confidence interval, RCT: Randomized controlled trial, df: Degrees of freedom, M-H: Mantel-Haenszel.
The sensitivity test showed that despite variations in effect size and heterogeneity on excluding individual studies, P-value remained insignificant in every exclusion of studies (P > 0.05 in every scenario). This consistency suggests that the meta-analysis results are robust to variations in study inclusion and not heavily influenced by any single study.
Union problems
Union problems, including malunion and non-union, were reported in eight studies (three RCTs and five observational studies). Union problems occurred in eight out of 466 cases (1,7%) in PFNA treatment and ten cases out of 493 (2.0%) in DHS treatment. A fixed-effects model was used due to the low level of heterogeneity (I2 = 0% and P = 0.41). Analysis of the forest plot showed no significant difference in union problems rate between PFNA and DHS (RR 0.87, 95% CI [0.35–2.12], P = 0.76) [Figure 8].
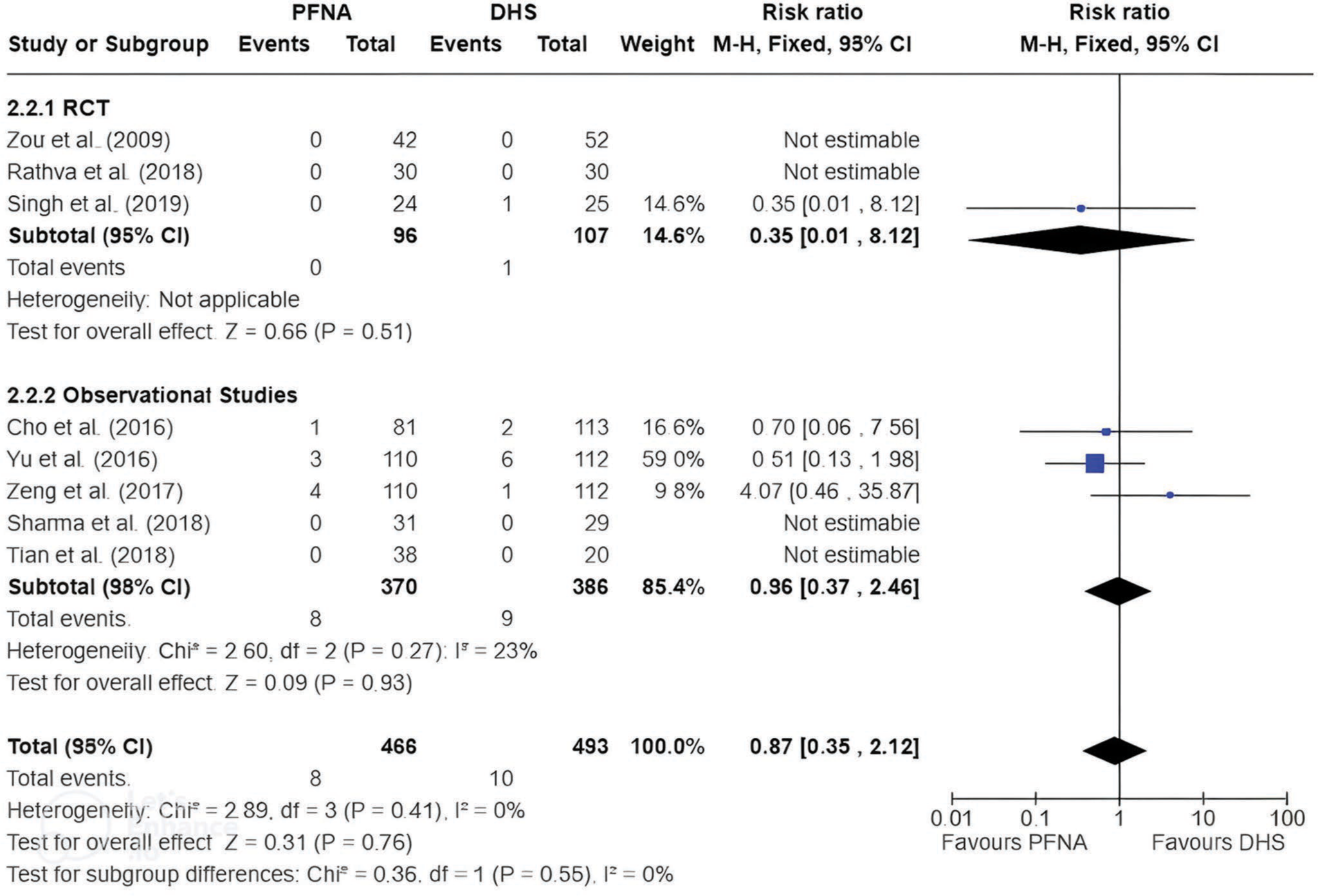
- Union problem rates (malunion and non-union) showed no significant difference between PFNA and DHS. Bold values indicate statistically significant results with a P-value <0.05. PFNA: Proximal femoral nail anti-rotation, SD: Standard deviation, DHS: Dynamic hip screw, CI: Confidence interval, RCT: Randomized controlled trial, df: Degrees of freedom, M-H: Mantel-Haenszel.
The sensitivity test showed that despite variations in effect size and heterogeneity on excluding individual studies, p-value remained insignificant in every exclusion of studies (P > 0.05 in every scenario). This consistency suggests that the meta-analysis results are robust to variations in study inclusion and not heavily influenced by any single study.
Cut-out/protrusion rate
The cut-out rate was reported in six studies (two RCTs and four observational studies). Cut-out rate occurred in three out of 405 cases (0.7%) in PFNA treatment and eight out of 434 cases (1.8%) in DHS treatment. A fixed-effects model was used due to the low level of heterogeneity (I2 = 0% and P = 0.52). Analysis of the forest plot showed no significant difference in cut-out rate between PFNA and DHS (RR 0.42, 95% CI [0.13–1.40], P = 0.16) [Figure 9].
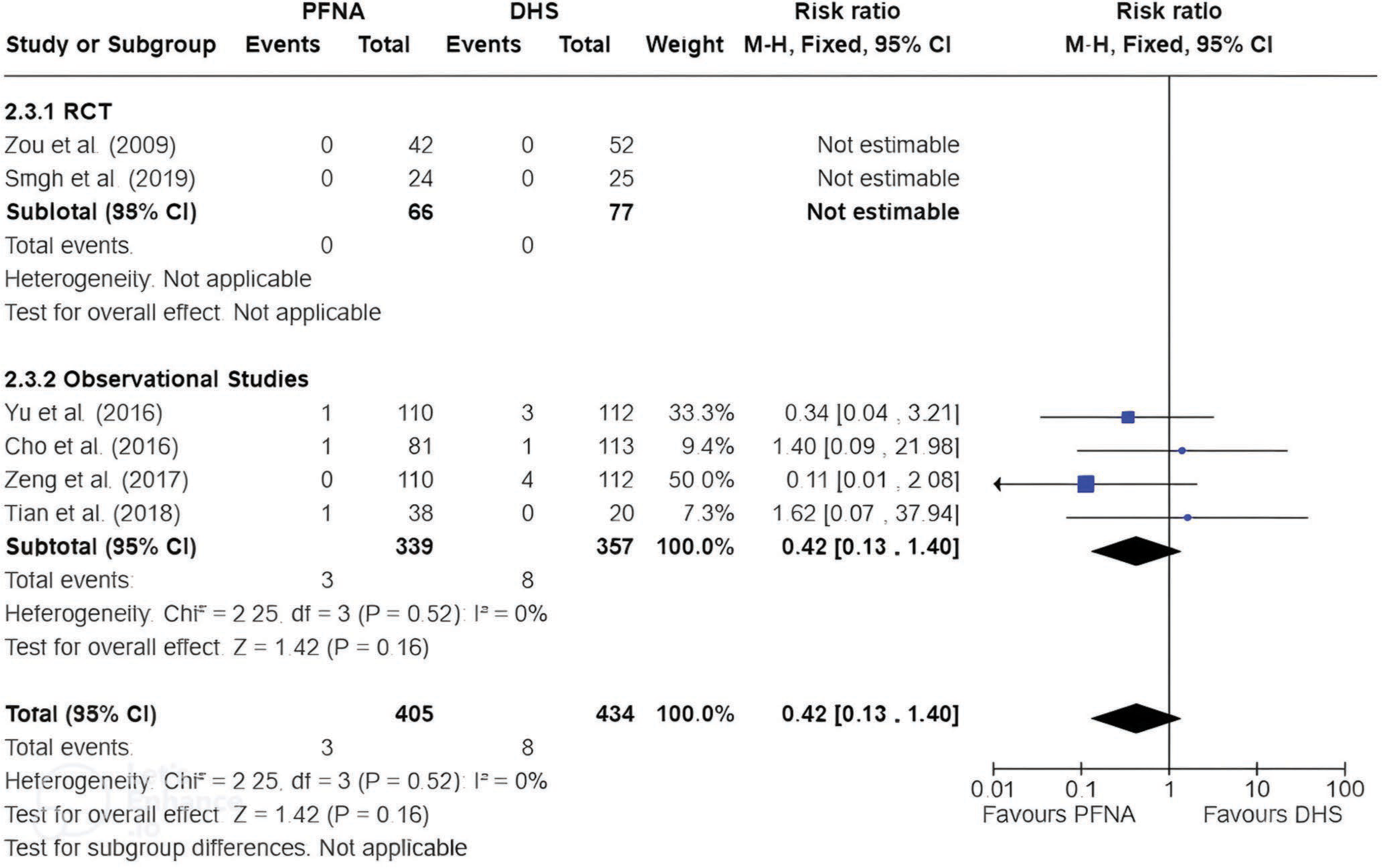
- Cut-out/protrusion rates showed no significant difference between PFNA and DHS. Bold values indicate statistically significant results with a P-value <0.05. PFNA: Proximal femoral nail anti-rotation, SD: Standard deviation, DHS: Dynamic hip screw, CI: Confidence interval, RCT: Randomized controlled trial, df: Degrees of freedom, M-H: Mantel-Haenszel.
The sensitivity test showed minimal variations in effect size and heterogeneity with consistent p-values (insignificant in every scenario). This consistency also suggests the result’s robustness.
Infection rate
Infection, both superficial and deep, was reported in eight studies (three RCTs and five observational studies). Infection occurred in six out of 466 cases (1.3%) in PFNA treatment and 15 out of 493 cases (3.0%) in DHS treatment. A fixed-effects model was used due to the low level of heterogeneity (I2 = 0% and P = 0.85). Analysis of the forest plot showed no significant difference in infection rate between PFNA and DHS (RR 0.49, 95% CI [0.22–1.10], P = 0.08) [Figure 10].
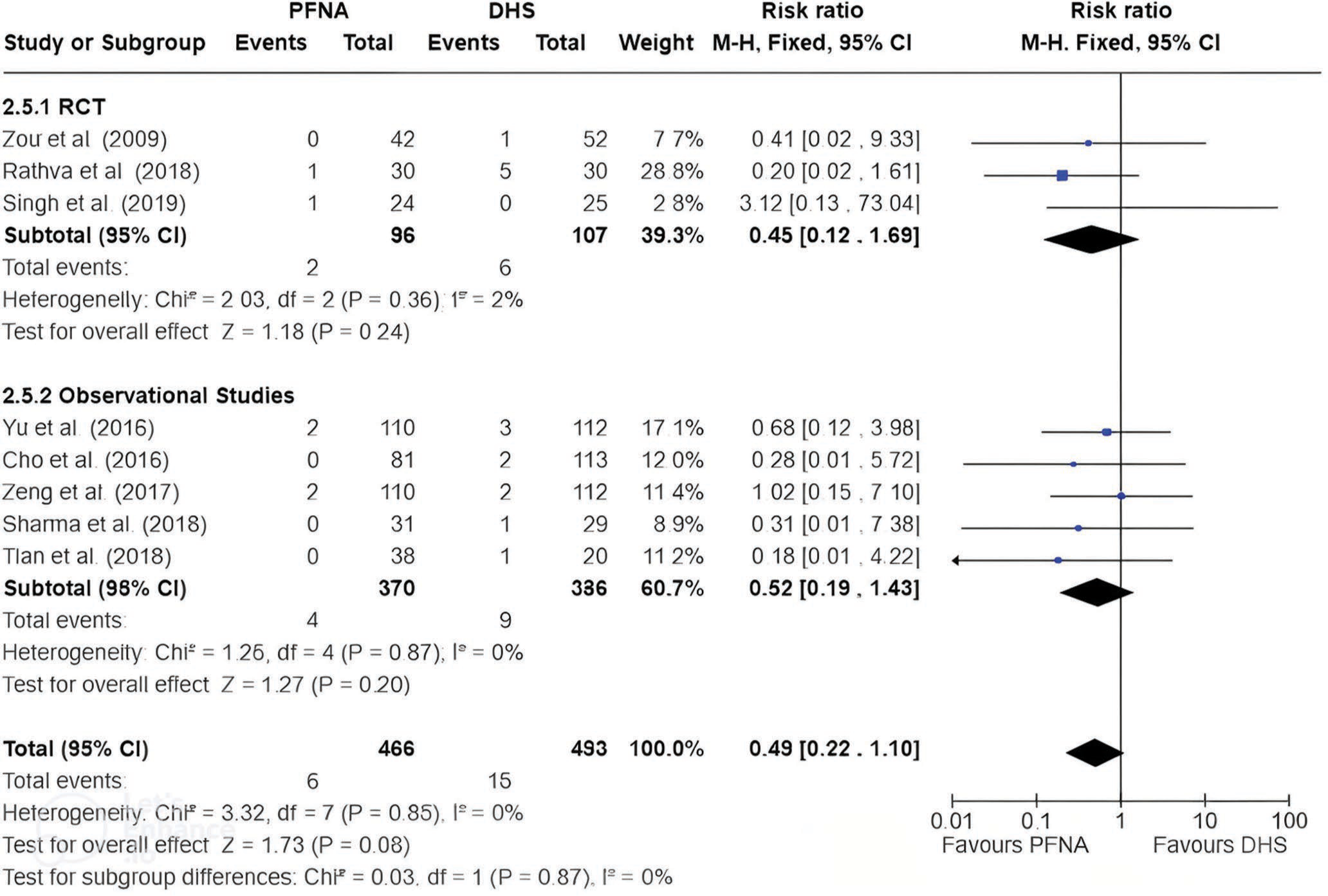
- Infection rates showed no significant difference between PFNA and DHS. Bold values indicate statistically significant results with a P-value <0.05. PFNA: Proximal femoral nail anti-rotation, SD: Standard deviation, DHS: Dynamic hip screw, CI: Confidence interval, RCT: Randomized controlled trial, df: Degrees of freedom, M-H: Mantel-Haenszel.
The sensitivity test showed minimal variations in effect size and heterogeneity on excluding individual studies with consistent p-values (insignificant in every scenario). This consistency also suggests the result’s robustness.
Secondary outcome: Perioperative outcomes
Mean operation time
Mean operation time was reported in six studies (two RCTs and four observational studies). A random-effects model was used due to high levels of heterogeneity (I2 = 87%, and P < 0.00001). PFNA had a significantly shorter operation time, with a mean of 51.9 min in 298 patients, compared to DHS, with a mean of 77.3 min in 249 patients (MD −18.63, 95% CI [−27.92–−9.34], P < 0.0001) [Figure 11].
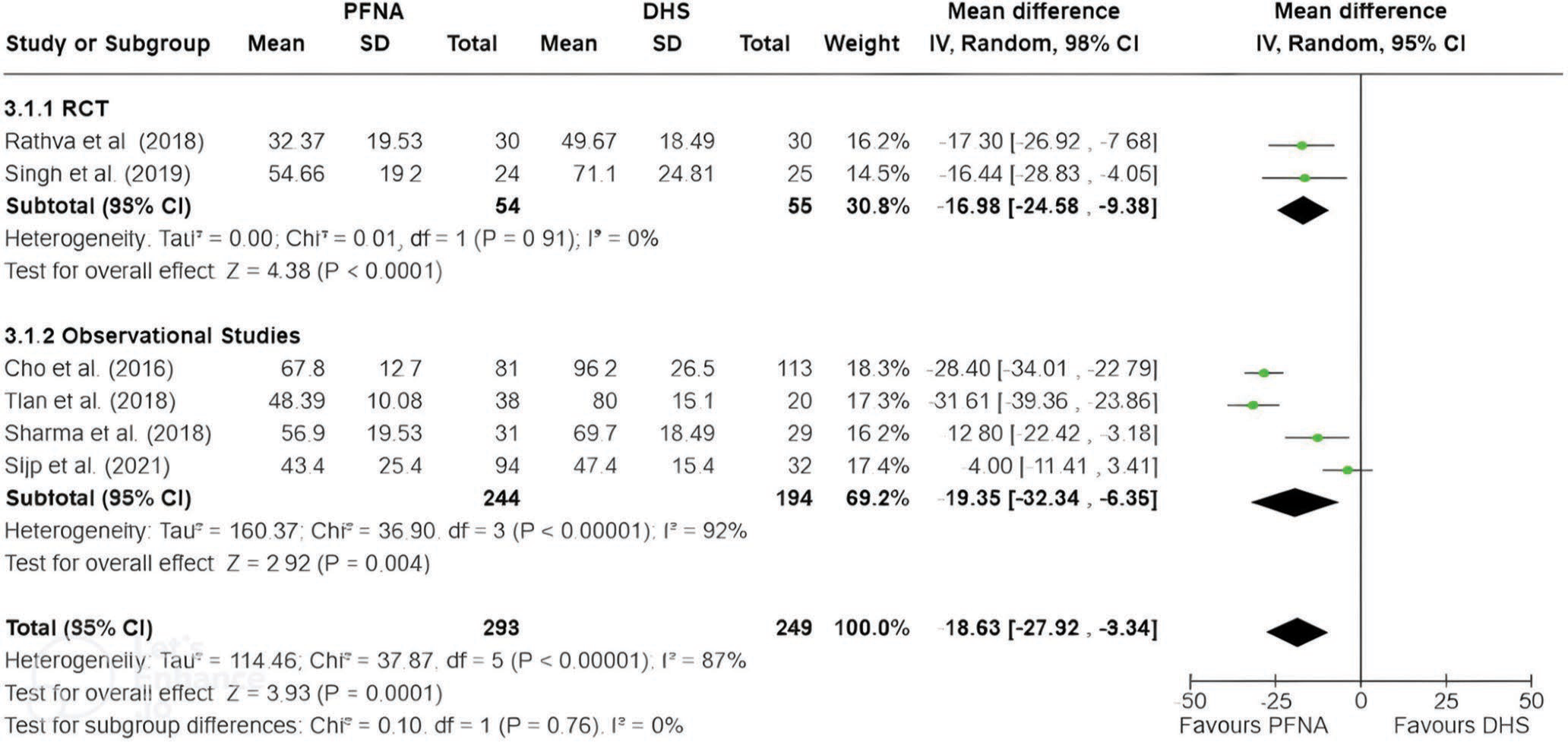
- Mean operation time was significantly shorter for PFNA compared to DHS. Bold values indicate statistically significant results with a P-value <0.05. PFNA: Proximal femoral nail anti-rotation, SD: Standard deviation, DHS: Dynamic hip screw, IV: Inverse variance, CI: Confidence interval, RCT: Randomized controlled trial, df: Degrees of freedom.
The sensitivity test showed consistent effect size and heterogeneity with slight variation on excluding individual studies. p-value remained significant in every exclusion of studies (P < 0.05 in every scenario) favoring PFNA treatment. This consistency suggests that the meta-analysis results are robust to variations in the study inclusion and not heavily influenced by any single study.
Mean blood loss
Mean blood loss was reported in six studies (two RCTs and four observational studies). A random-effects model was used due to high levels of heterogeneity (I2 = 93%, and P < 0.00001). There was a significantly lower blood loss for PFNA, with a mean of 145.5 ml in 298 patients, compared to DHS, with a mean of 261.8 ml in 249 patients (MD −88.84, 95% CI [−158.03–−19.65], P = 0.01) [Figure 12].
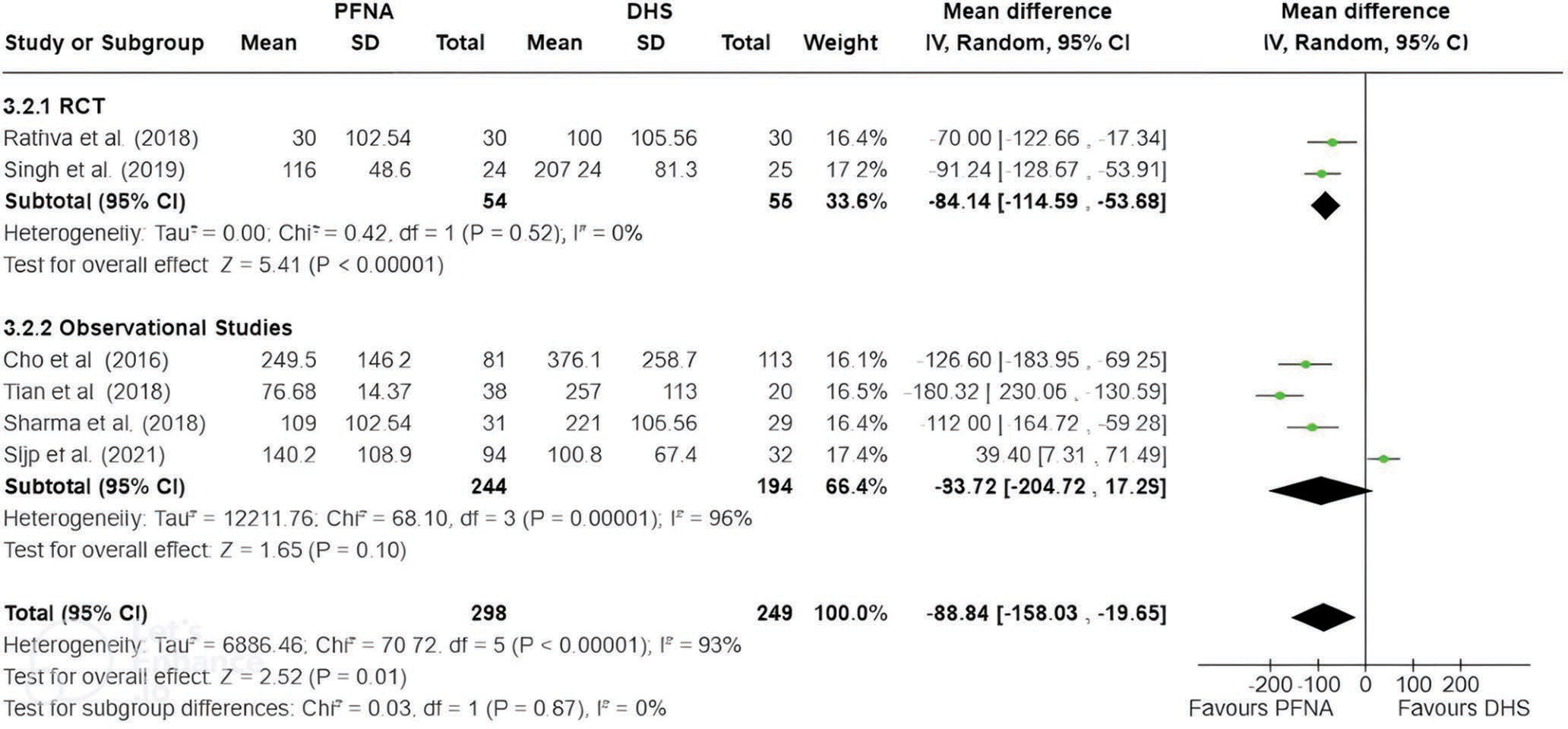
- Mean blood loss was significantly less for PFNA compared to DHS. Bold values indicate statistically significant results with a P-value <0.05. PFNA: Proximal femoral nail anti-rotation, SD: Standard deviation, DHS: Dynamic hip screw, IV: Inverse variance, CI: Confidence interval, RCT: Randomized controlled trial, df: Degrees of freedom.
The sensitivity test showed two findings in this study:
There were minimal variations in effect size and heterogeneity on excluding most of the individual studies, except one observational study (Sijp et al. 2020).[22] This study showed a substantial decrease in heterogeneity (93–64%). The exclusion of this study strengthens the conclusion that PFNA has less blood loss than DHS (P = 0.05 to P < 0.00001).
Exploring more of this study’s sensitivity, one RCT (Singh et al. 2019)[19] substantially influenced the statistical significance of the association between treatment and mean blood loss. P-value increased to 0.05. Therefore, the recalculated P-value suggests a borderline result. This is due to the importance of the RCTs in conducting a meta-analysis, as explained before, to balance the potential outlier of the van der Sijp et al.[22] study.
Overall, the result suggests a potential study (Singh et al. 2019)[19] as the outlier of this study. However, the outlier does not change the conclusion of this study.
DISCUSSION
This meta-analysis compared PFNA and DHS devices for treating stable intertrochanteric femoral fractures according to the newest AO classification (AO 31-A1). The important thing to note is that there is a difference between the old and the new classification of intertrochanteric fracture. However, eight out of the ten studies included in this meta-analysis specifically addressed 31-A1 fractures, ensuring consistency regardless of whether the original or modified AO classification was used. The studies by Singh et al. and Sharma et al. were the only two that included 31-A2.1 fractures, as defined by the older classification.[16-19] However, due to the limited number of studies available, these studies were included in the meta-analysis.
The PFNA and DHS are the most common internal fixation devices for treating stable fractures. However, which one is better remains a topic of ongoing debate. This study included 1149 patients, including three RCTs and seven observational studies. This enabled us to compare the functional score as the primary outcome and the complications and perioperative outcomes as the secondary outcome.
This study compared the functional scores from several studies using HHS as the assessment tool. It consists of a questionnaire that assesses some parameters of hip function, which include pain, mobility, activities of daily living, and physical function.[28-30] The higher the score, the better the hip function and overall outcome. In this study, we analyzed HHS in three different follow-up periods (3 months, 6 months, and 12 months). This is the first meta-analysis noted to compare the recovery progression of PFNA compared to DHS in different periods. This study found no differences in the HHS between PFNA and DHS treatment. This is true for different follow-up periods that we analyzed (3–12 months).
The 12-month follow-up represented a long-term follow-up period, allowing for a comprehensive evaluation of the surgical intervention. In this period, we found no differences again between PFNA and DHS treatment. The effectiveness of post-operative rehabilitation and physical therapy may play a crucial role in regaining abductor strength and minimizing the differences between these two treatments. A meta-analysis by Zhang et al.[3] compared the clinical outcome of PFNA to DHS in unstable fractures. Their study found that PFNA is superior to DHS for unstable fractures in terms of HHS. This result contradicts what our study yielded after one year of follow-up. This difference is related to the nature of the fracture itself. For unstable fractures, axial flexion, extension stability, and rotational stability provided by internal fixation after fracture reduction are critical.[31,32] Conversely, stable trochanteric fractures typically involve minimal displacement and good alignment of fracture fragments. Both of these devices treat the fracture by compression force and maintain a stable alignment. This phenomenon leads to the same outcome between these two devices.
Moreover, since stable trochanteric fractures generally have a favorable prognosis, long-term functional outcomes may be similar after treatment with PFNA or DHS. The anti-rotation properties by PFNA may be unnecessary and excessive for stabilizing this type of fracture. Sensitivity analysis in our study for 12-month follow-up showed a significant change in terms of heterogeneity following the exclusion of one RCT study. However, the core conclusion of the study is still consistent.
The post-operative complications discussed in this study included implant failure, union problems, cutout/protrusion, and infection. Overall, treating stable intertrochanteric femoral fractures with either PFNA or DHS resulted in similar risks.[33,34]
Mean operative time and mean blood loss were found to be statistically different between the two groups, which was in favor of PFNA fixation. Other studies have reported similar findings. The shorter operative time of PFNA is related to the size of the incision and the soft-tissue dissection. Smaller incisions and limited soft-tissue dissection lead to shorter time required for wound closure. Similar to surgery time, PFNA was also reported to have less blood loss than DHS. The extensive surgical area needed for DHS as an extramedullary surgical method leads to greater blood vessel disruption, leading to more blood loss.[22]
These perioperative outcomes are particularly relevant for specific populations that are susceptible to long surgical duration and excessive blood loss. However, these results should be interpreted with care. Mean operative time and mean blood loss reported in this study have high levels of heterogeneity (I2 = 87% for mean operative time and I2 = 93% for mean blood loss). The high heterogeneity level may be attributed to differences in surgery protocols, device used, surgeons’ experience, and the perioperative parameters’ standard measurement protocols. However, sensitivity tests in this study suggest that this conclusion is robust and not heavily influenced by any single study.
Based on the explanation provided, it is tempting to conclude that surgeons utilize either type of fixation. More surgeons have favored the newer PFNA devices over managing stable fractures in recent years.[12] From our perspective, this is too excessive due to the lack of superiority of this device. Another aspect, including implant cost, should be considered. The DHS implant is likely the most cost-effective option, considering that PFNA, being an intramedullary device, can exceed DHS by over $1000 in cost. Other costs associated with acute hospitalization and subsequent rehabilitation were assumed to be equal between the treatment groups. Although these costs are high, the literature has not shown a significant difference in length of stay, post-operative function, transfusion requirements or operating room utilization between implant types, provided that the fracture healed successfully.[35] Our evolving understanding of how implant choices are affected by clinical outcomes and socioeconomic aspects will likely play an important role in the near future.
Some limitations should be considered when interpreting the result of this study. Some of the analyzed studies included significant heterogeneity, especially for functional outcomes and perioperative complications. In functional outcomes, we found that RCT studies may have contributed to their disproportionate influence on the overall meta-analysis results. This occurred due to the different nature of the study, which offers rigorous experimental control through randomization. However, observational studies play a crucial role in elucidating real-world associations and outcomes. The incorporation of diverse study designs enriches the depth of the analysis but also introduces complexities in synthesizing heterogeneous data, especially in the limitation of a small number of the included studies.
Further, well-designed studies, especially RCTs, carefully considering patient characteristics and standardized outcome measures, are warranted to elucidate the optimal treatment approach in this clinical context. Another limitation of this study is that all studies included were assessed to have a moderate or higher overall risk of bias, which elevates the risk of reporting and measurement biases. Finally, this study is limited to clinical parameters without considering broader aspects of implant choice decisions.
CONCLUSION
Both PFNA and DHS demonstrate favorable outcomes, and there are no meaningful differences in long-term functional outcomes and complications between these two. Due to its minimally invasive nature, PFNA may be more beneficial in the perioperative aspect, including shorter surgical duration and lesser blood loss. Since the overall outcomes are similar, considering socioeconomic aspects becomes crucial. The DHS is more cost-effective, which can significantly reduce the financial burden on patients and health-care systems. With the limitation of the current literature, future research should prioritize well-designed trials and explore broader aspects beyond clinical outcomes when making decisions about implant choices.
AUTHORS’ CONTRIBUTIONS
EM: Conceptualization, supervision, validation. APA: Writing – review and editing, supervision, validation. AF: Writing – original draft preparation, data curation, visualization, methodology. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The Institutional Review Board approval is not required.
DECLARATION OF PATIENT CONSENT
Patient’s consent not required as there are no patients in this study.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Intertrochanteric femur fracture In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493161/ [Last accessed on 2024 Mar 21]
- [Google Scholar]
- Are intertrochanteric fractures evolving? Trends in the Elderly population over a 10-year period. Clin Orthop Surg. 2022;14:13-20.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of clinical outcomes with proximal femoral nail anti-rotation versus dynamic hip screw for unstable intertrochanteric femoral fractures: A meta-analysis. Medicine (Baltimore). 2023;102:e32920.
- [CrossRef] [PubMed] [Google Scholar]
- A review of tip apex distance in dynamic hip screw fixation of osteoporotic hip fractures. Niger Med J. 2012;53:184-91.
- [CrossRef] [PubMed] [Google Scholar]
- Intertrochanteric femur fractures: A current concepts review. SA Orthop J. 2023;22:41-7.
- [CrossRef] [Google Scholar]
- Clinical evaluation of the Asian proximal femur intramedullary nail antirotation system (PFNA-II) for treatment of intertrochanteric fractures. J Orthop Surg Res. 2014;9:112.
- [CrossRef] [PubMed] [Google Scholar]
- Management of hip fractures in older adults evidence-based clinical practice guideline. United States: American Academy of Orthopaedic Surgeons 2021:e1297-301.
- [CrossRef] [PubMed] [Google Scholar]
- AAOS clinical practice guideline summary: Management of hip fractures in older adults. JAAOS J Am Acad Orthop Surg. 2022;30:e1291-6.
- [CrossRef] [Google Scholar]
- Comparative prospective study of proximal femoral nail and dynamic hip screw in treatment of intertrochanteric fracture femur. J Clin Orthop Trauma. 2012;3:28-36.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of the clinical effectiveness of PFNA, PFLCP, and DHS in treatment of unstable intertrochanteric femoral fracture. Am J Ther. 2017;24:e659-66.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of PFNA and DHS for the treatment of elderly unstable intertrochanteric fractures of femur. Chin J Orthop Traumatol. 2019;32:824-9.
- [Google Scholar]
- Changing trends in the management of intertrochanteric hip fractures-a single centre experience. Injury. 2016;47:1525-9.
- [CrossRef] [PubMed] [Google Scholar]
- The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of functional outcomes in patients fixed with dynamic hip screw and proximal femur nail-anti-rotation in A1 and A2 type intertrochanteric femur fractures. Turk J Trauma Emerg Surg. 2020;26:811-7.
- [CrossRef] [PubMed] [Google Scholar]
- Choice of implant in stable intertrochanteric fracture femur: PFNA vs DHS. Int J Orthop. 2018;4:9-15.
- [CrossRef] [Google Scholar]
- Treatment of stable intertrochanteric fractures of the femur with proximal femoral nail versus dynamic hip screw: A comparative study. Rev Brasil Ortop. 2018;53:477-81.
- [CrossRef] [Google Scholar]
- Cochrane handbook for systematic reviews of interventions, version 6.4 Hoboken, NJ: Cochrane; 2023. Available from: https://www.training.cochrane.org/handbook [Last accessed on 2024 Apr 26]
- [Google Scholar]
- Imputing missing standard deviations in meta-analyses can provide accurate results. J Clin Epidemiol. 2006;59:7-10.
- [CrossRef] [PubMed] [Google Scholar]
- Is PFNA-II a better implant for stable intertrochanteric fractures in elderly population? A prospective randomized study. J Clin Orthop Trauma. 2019;10:S71-6.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of proximal femoral nail antirotation and dynamic hip screw devices in trochanteric fractures. J Int Med Res. 2009;37:1057-64.
- [CrossRef] [PubMed] [Google Scholar]
- Proximal femoral nails anti-rotation versus dynamic hip screws for treatment of stable intertrochanteric femur fractures: An outcome analyses with a minimum 4 years of follow-up. BMC Musculoskelet Disord. 2016;17:222.
- [CrossRef] [Google Scholar]
- High risks of failure observed for A1 trochanteric femoral fractures treated with a DHS compared to the PFNA in a prospective observational cohort study. Arch Orthop Trauma Surg. 2021;142:1459-67.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and functional outcomes of treatment for type A1 intertrochanteric femoral fracture in elderly patients: Comparison of dynamic hip screw and proximal femoral nail antirotation. Hip Pelvis. 2016;28:232-42.
- [CrossRef] [PubMed] [Google Scholar]
- Short-term follow-up of dynamic hip screw versus proximal femoral nail anti-rotation for type AO/OTA A1 intertrochanteric femoral fracture in older adults. Chin J Tissue Eng Res. 2018;23:1834.
- [Google Scholar]
- Proximal femoral nail antirotation versus dynamic hip screw fixation for treatment of osteoporotic type 31-A1 intertrochanteric femoral fractures in elderly patients. J Int Med Res. 2017;45:1109-23.
- [CrossRef] [PubMed] [Google Scholar]
- Is the Harris hip score system useful to study the outcome of total hip replacement? Clin Orthop Relat Res. 2001;384:189-97.
- [CrossRef] [PubMed] [Google Scholar]
- Clinically important improvement thresholds for Harris Hip Score and its ability to predict revision risk after primary total hip arthroplasty. BMC Musculoskelet Disord. 2016;17:1-8.
- [CrossRef] [PubMed] [Google Scholar]
- Antirotation proximal femoral nail versus dynamic hip screw for intertrochanteric fractures: A meta-analysis of randomized controlled studies. Orthop Traumatol Surg Res. 2013;99:377-83.
- [CrossRef] [PubMed] [Google Scholar]
- Femoral shortening after surgical treatment of trochanteric fractures in nongeriatric patients. J Trauma Acute Care Surg. 2008;64:982-9.
- [CrossRef] [PubMed] [Google Scholar]
- A prospective comparative study of outcome of management of unstable intertrochanteric fracture of femur with dynamic hip screw and proximal femoral nail anti rotation. Int J Contemp Med Res. 2018;5:4-7.
- [CrossRef] [Google Scholar]
- Evaluation of risk for secondary fracture after removal of a new femoral neck plate for intracapsular hip fractures. J Orthop Trauma. 2011;25:721-5.
- [CrossRef] [PubMed] [Google Scholar]
- Complications following implant removal in patients with proximal femur fractures-an observational study over 16 years. Orthop Traumatol Surg Res. 2015;101:785-9.
- [CrossRef] [PubMed] [Google Scholar]
- Femoral neck fractures after removal of hardware in healed trochanteric fractures. Injury. 2017;48:2619-24.
- [CrossRef] [PubMed] [Google Scholar]
- Cost-effectiveness analysis of fixation options for intertrochanteric hip fractures. JBJS. 2014;96:1612-20.
- [CrossRef] [PubMed] [Google Scholar]







