Translate this page into:
Comparison of active release and post-isometric relaxation techniques on functional performance in patients with chronic lateral epicondylitis
*Corresponding author: Sana Hafeez, Department of Physical Therapy and Rehabilitation, University of Management and Technology, Lahore, Pakistan. Sana.hafeez@umt.edu.pk
-
Received: ,
Accepted: ,
How to cite this article: Hanif A, Hafeez S, Arif T, Habib S, Ejaz R. Comparison of active release and post-isometric relaxation techniques on functional performance in patients with chronic lateral epicondylitis. J Musculoskelet Surg Res. 2024;8:240-6. doi: 10.25259/JMSR_65_2024
Abstract
Objectives:
Lateral epicondylitis (LE) occurs as a result of repetitive strain near the place of origin of the extensor carpi radialis brevis tendon. This is due to eccentric overload and repetition, causing chronic degeneration of the forearm’s common extensor tendons, which are attached to the lateral epicondyle of the humerus. This study aimed to assess the comparative effects of post-isometric relaxation (PIR) and active release techniques (ARTs) on pain inhibition, grip strength, and functional ability among individuals suffering from chronic LE.
Methods:
A randomized clinical trial was conducted on 30 individuals suffering from chronic LE. All of the subjects were randomly assigned to one of two treatment groups: PIR method or active release approach. Both groups received 12 sessions over four weeks. The numerical pain rating scale (NPRS), handheld dynamometer, and patient-rated tennis elbow evaluation (PRTEE) were used to assess the impacts of therapy before and after treatment sessions.
Results:
The results showed that the NPRS pain score, strength of the grip, and functional performance all showed substantial differences between the two groups (P < 0.05) as well as within-group differences (P < 0.05).
Conclusion:
The study concluded that PIR techniques were more effective as compared to ARTs for pain reduction, improved strength of gripping, enhanced functionality, and showed better outcomes in terms of mean difference of NPRS, dynamometer, and PRTEE scoring across the groups.
Keywords
Active release
Extensor carpi radialis brevis
Lateral epicondylitis
Muscle energy technique
Post-isometric relaxation
INTRODUCTION
Lateral epicondylitis (LE) is the most prevalent reason for lateral elbow discomfort in older adults. It is also known as “tennis elbow.” It is an overuse injury at the point of beginning of the extensor carpi radialis brevis (ECRB) tendon caused by eccentric overload of the common extensors.[1] A new term, “tendinosis or tendinopathy,” has become popular and is now commonly used compared to the previous one, “tendinitis,” due to repetitive strain and chronic degeneration of the forearm’s common tendons of extension attached to the lateral epicondyle of the humerus.[2,3] Maffulli et al. were among the earliest researchers to advocate for a shift in medical terminology from tendinitis to tendinopathy. At present, tendinopathy is a recognized term that refers to a number of tissue diseases that develop in damaged tendons and represents non-rupture injury to the tendon or para-tendon that worsens under mechanical strain.[4] The terminology shift is being linked to new advancements in comprehension of tendon pathophysiology, indicating a greater clarity of the excessive use cycle and the subsequent structural as well as functional harm in tendons with chronic pain; more information regarding the mechanical stability disturbances that cause chronic tendon disease pathology; and an improved comprehension of the crucial role of both internal and external lifestyle factors.[5]
The ECRB muscle is more prone to injury when the tendon is stretched over the radial head, resulting in an increase in tensile load during repetitive wrist extension. It leads to further strain of the tendon during the forearm supination. This is due to the radial head’s anterior rotation against the ECRB muscle.[3] LE is one of the most commonly work-related disorders.[6] The prevalence of LE is more common among the middle-aged general population. In the general population, the prevalence of LE among males lies approximately between 1.0 and 1.3% and among females between 1.1 and 4.0% per year per 100 subjects.[6]
The pathophysiology of LE shows abnormal arrangements of collagen fibers, vascular disruption, and cellular disorganization at tendon fibers that lead to tendinosis. Musculoskeletal ultrasound examination reveals increased calcification, increase in heterogeneity, and thickening observed in common extensor tendons and marked irregularity of lateral epicondyle.[7,8] Subjects with LE are unable to perform normal functional tasks such as holding and gripping activities. LE patient presents with pain and local tenderness along and distal to the lateral epicondyle of the elbow joint and limited functional activities. The pain is observed due to repetitive wrist flexion and extension of the wrist and repetitive supination and pronation are associated with decreased grip strength. Some sleeping positions can be provocative and cause pain, such as the overhead arm position, mostly when lying on the side. The nightly overhead sleeping position presents with severe morning pain and delayed tendon healing at the initial acute lesion of the lateral epicondyle of the elbow, called the “pathological sleep position.”[9] The physical examination provides an early diagnosis of LE and helps to identify a differential diagnosis. On palpation, 1–2 cm distal to the lateral epicondyle, a spot of maximal pain, and tenderness is located. The special tests used to confirm the diagnosis of LE act as pain provocation tests. Three specific tests were used: Mill’s and Cozen’s test and Maudsley’s (3rd finger resisted extension).[10,11]
Post-isometric relaxation (PIR) is a type of muscle energy technique (MET) used to reduce muscle tone and lengthen and relax the shortened and hypertonic agonist muscles against the isometric contraction. This happens due to the activation of a naturally neurological protective mechanism through the stretch receptors “Golgi tendon organs,” located in the muscles’ tendon. About 75% of the maximal isometric contraction of a patient is maintained against a practitioner’s resistance for 5 s, followed by the release of resistance until a new range gain with another barrier is again met. The whole procedure should be repeated 3–5 times during each treatment session.[12]
Active release technique (ART) is a non-invasive, soft-tissue rehabilitation approach that removes and breaks adhesions and scar tissue formation, which can lead to pain, swelling, stiffness, and altered sensations due to mechanical dysfunctions within soft tissues. ART combines the exertion of deep tissue pressure on the tender region of concern with active patient engagement to shift tissue from a shorter to an extended posture to prevent the development of adhesions. It is also used to release nerve entrapment within muscles, tendons, and adjacent fascia. It contains four steps: (a) Tissue tension, (b) tissue texture, (c) tissue movement, and (d) tissue function.[13]
Therefore, this study aimed to assess the comparative effects of PIR and ART on pain inhibition, grip strength, and functional ability among individuals suffering from chronic LE. The results of this study will help provide prompt assistance in selecting the most beneficial approach for this targeted population. Thus, rapid improvements can be attained with fewer therapy sessions and patient visits.
MATERIALS AND METHODS
A randomized clinical pilot study was conducted from November 2019 to March 2020. The trial was registered in the World Health Organization Registry of Iranian registry of clinical trials (IRCT), having reference no # IRCT20200502047274N1. Data was collected from Sialkot Medical Complex and Sardar Begum Hospital Sialkot. In this study, the sample size was 24. A total of 30 LE subjects were assessed for eligibility. Participants who were clinically diagnosed and referred by their physician or orthopedician with chronic LE were recruited.
Four patients were unable to meet the inclusion criteria. The age of the two participants was above 45, and two patients had pain greater than six on the Numerical Pain Rating Scale (NPRS). Two patients declined to participate and were excluded from the study. Participants attended an outpatient physiotherapy clinic after at least six weeks of symptoms and were evaluated with screening clinical special tests for chronic LE. Hence, a total of 24 individuals were recruited based on the criteria for inclusion and picked by the chit-pick box technique of simple randomization.
In this simple randomized single-blinded clinical pilot study, the outcome assessor was blinded regarding patients’ baseline characteristics, treatment protocol, and study population. The age group of patients was between 25 and 45 years. For subjects with unilateral elbow involvement, pain intensity levels were between 3 and 6 on 0–10 points of the NPRS; subjects with positive “Cozen’s test” or “Mill’s test” were examined as LE, and subjects’ willingness to participate in this study. Before commencing the treatment regimen, participants were given written consent, and the procedure to be followed was explained to them.
Participants were excluded if they had a history of cervical radiculopathy, peripheral nerve involvement signs and symptoms, any previous surgery of the elbow, a history of previous physiotherapy treatment, and any steroid injection during the past six months.
All participants were allocated into two equal groups: Group A (ultrasound therapy with ART) and Group B (ultrasound therapy with PIR technique).
Each treatment protocol consisted of three sessions per week on alternate days. A total of 12 sessions per four weeks on alternate days were given. Assessment tools were the patient-rated tennis elbow evaluation (PRTEE) scale, NPRS scale, and handheld dynamometer used to collect before the first treatment session (pre-treatment) and the 12th treatment session (post-treatment). The evaluation form consists of general demographic data, duration of symptoms, detailed examination of the elbow joint, PRTEE scale to assess functional performance, NPRS scale for level of pain assessment, and handheld dynamometer for measuring the strength of gripping.
Interventions
Patients were asked to continue regular daily routines while excluding additional therapy protocols during the trial period. Other than the selected treatment protocol, patients were not allowed to administer other techniques such as steroids, tapings, and other electrotherapy modalities during interventional trials.
When the patient came to the first visit after referral
The physiotherapist conducted a thorough case assessment and physical evaluation of the chronic LE condition
The patient was asked to complete the NPRS, PRTEE, and grip strength measurements. The pre-treatment values were given to the assessor’s physiotherapist.
Conventional protocol
The conventional therapy was given in both A and B groups before applying a specific treatment technique. It includes therapeutic ultrasonics around the affected involved site at the teno-osseous junction distal to the lateral epicondyle of the humerus. Position of the patient was sitting with elbow flexed and forearm supported in pronation. Continuous mode application, frequency 1 MHz, pulse ratio of 1:4, intensity set at 1.5 W/cm2, with a duration of 5 min for each session, three sessions per week of the treatment protocol, and a total of 12 sessions for four weeks.
Group A (conventional therapy and ART)
In combination with conventional therapy, the ART was applied to the patient in a sitting position, with the elbow flexed at 90° supported on the treatment table, the forearm in a mid-prone position, and the wrist rest in neutral. The therapist focused on ECRB and longus tendons by exerting digital force at the teno-osseous junction below the attachment on the elbow. The patient started to flex the elbow and wrist in neutral while the therapist applied deep manual pressure with thumbs (deep friction massage position) on the teno-osseous junction. The patient extended the elbow with the forearm in pronation and the wrist in the flexion position. The therapist then applied deep tension in the proximal direction in an attempt to break the adhesion formation between the muscle fibers at the site of the humerus lateral epicondyle. A total number of 10 repetition/single treatment sessions was given for 10 min, three sessions each week for four weeks of duration. After four weeks of a post-therapy plan of care, hand gripping strength, pain, and functionality of the elbow joint were assessed with tools, handheld dynamometer, NPRS scale, and PRTEE scale, and evaluated pre- and post-treatment results by the outcome assessor.
Group B (conventional therapy and PIR technique)
In combination with ultrasound therapy and the PIR technique, the PIR was applied to the patient in a sitting position, with the elbow flexed at 90°, the patient’s forearm supported on the treatment table, and supinated. The therapist applied resistance manually and the patient pronated his forearm (approximately 75% of maximal isometric contraction) against the resistance of a 5-s hold, followed by supination of the forearm immediately until a new resistance was met. The whole process was repeated five times per single treatment session. The total treatment protocol of the PIR technique was given three sessions per week for four weeks. After four weeks of post-therapy plan of care, hand gripping strength, pain, and functionality of the elbow joint were assessed with tools, a handheld dynamometer, NPRS scale, and PRTEE scale, and evaluated pre- and post-treatment results by the outcome assessor.
Outcome measures
The primary outcome measures were NPRS, hand grip strength with a handheld dynamometer, and PRTEE, which were taken before interventions as pre-treatment values and after four weeks as post-treatment values. The CONSORT flow diagram is shown in Figure 1.
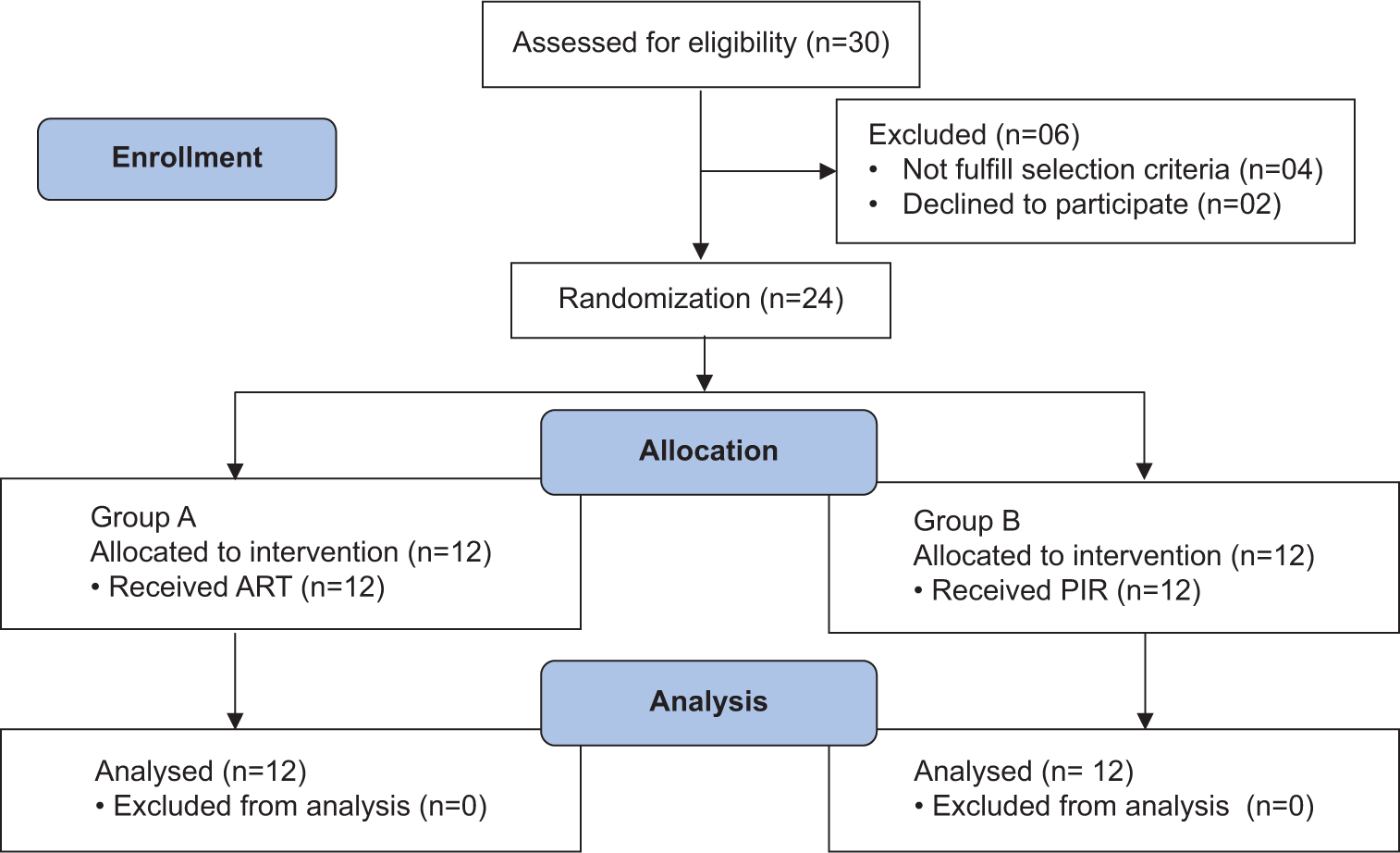
- Consolidated standards of reporting trials flow diagram. ART: Active release technique, PIR: Post isometric relaxation, n: total number of participants
Statistical analysis
The variables were analyzed using the Statistical Package for the Social Sciences version 21. The level of statistical significance had been set at P = 0.05. Frequency graphs, pie charts, and bar charts were utilized to present an overview of group measures taken over time. A parametric test, an independent sample t-test, was used to examine the intergroup difference. Intragroup before and after treatment data were examined using a parametric test and a paired sample t-test.
RESULTS
The groups were similar according to their demographic variables, as shown in Table 1. In both groups (A and B), the mean age of participants was 35–38 years, and it is shown in Figure 2. An independent t-sample test was applied for across the group comparison. Results were statistically significant between the two groups for NPRS and PRTEE with P < 0.05, as shown in Table 2. The results were insignificant for grip strength, and P-value exceeded 0.05.
| Study groups | n | Mean | Standard Deviation | |
|---|---|---|---|---|
| Group A (active release technique) | Age | 12 | 38.6 | 3.98 |
| Group B (post- isometric relaxation) | 12 | 37.0 | 4.17 |
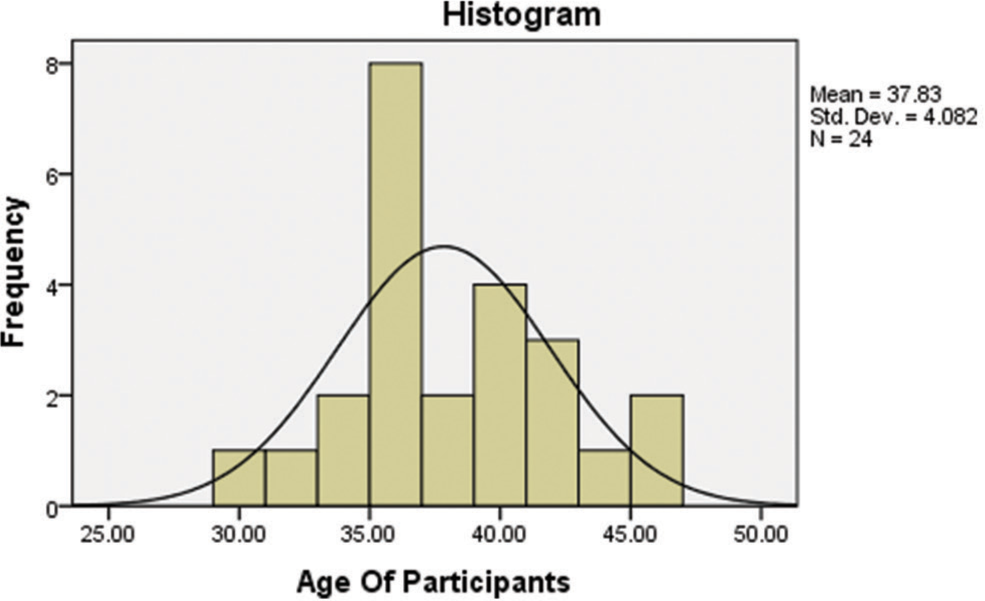
- Age of participants.
| Mean difference | P-value | |
|---|---|---|
| Pre-treatment NPRS | 3.27 | 0.41 |
| Post-treatment NPRS | 1.21 | 0.01 |
| Pre-treatment grip strength | 4.67 | 0.56 |
| Post-treatment grip strength | 2.76 | 0.12 |
| Pre-treatment PRTEE | 3.98 | 0.12 |
| Post-treatment PRTEE | 1.04 | 0.04 |
NPRS: Numeric pain rating scale, PRTEE: Patient-rated tennis elbow evaluation
The NPRS scale, grip strength, and PRTEE scale within each experimental group employing a paired-t-test are compared in Table 3. A statistically significant disparity was observed in both groups pre- and post-intervention.
| Group A (n=12) | Group B (n=12) | |||
|---|---|---|---|---|
| Mean difference±SD | P-value | Mean difference±SD | P-value | |
| Pre-post NPRS | 2.43±0.84 | 0.001 | 3.10±0.72 | 0.001 |
| Pre-post grip strength | 9.41±2.31 | 0.001 | 15.83±2.91 | 0.001 |
| Pre-post PRTEE | 22.08±4.29 | 0.001 | 31.833±4.87 | 0.001 |
NPRS: Numeric pain rating scale, PRTEE: Patient-rated tennis elbow evaluation
DISCUSSION
The findings of a recent study showed that both the ART (Group A) and PIR technique (Group B) showed significant improvements in hand gripping strength and functional performance and reduced pain associated with chronic LE following four weeks of treatment sessions. The reported effectiveness of the PIR technique compared to other interventional techniques is supported by published previous literature.[14] Females are more affected by chronic LE than males.[15] Dominant arms of right-sided patients are more commonly affected by LE as compared to left-sided. The number of patients lies within 40–45 years of age.[16]
The present study revealed that males were more affected by LE in both groups. Dominant right-sided were more affected, but left-sided patients were also affected almost similarly. The mean age of patients was in the middle age group of 35–38 years.
The present study found statistically noteworthy outcomes across ART and PIR procedure groups regarding NPRS, strength, and PRTEE scales using paired sample t-tests. However, the mean change in values of the PIR group improved more than that of the other treatment group. This result is similar to a previous study, which shows the difference in improvement in the PIR group as compared to the ART group based on pain threshold (NPRS), grip strength, and functional performance duration by the PRTEE scale.[15]
In most of the previous literature, VAS was used as an outcome measuring tool for evaluating the pain threshold level by applying METs and, compared to other related techniques such as MWM follow-up of 3 weeks.[3] The recent study revealed that the NPRS scale was used to assess pain using ART and PIR techniques as a measuring tool, followed by four weeks of interventions. Regarding inter-group comparison, pain-free grip strength improved significantly with the ART after the application of 12 sessions over four weeks (P < 0.05). [3] The present study showed that grip strength measured by handheld dynamometer showed that both groups had similar results (P > 0.05) followed by 12 sessions of four weeks. There was a significant decrease in mean from 4.50 to 2.66 (P < 0.05) on the NPRS scale in both group analyses.[17] The results are similar to the present study, decreasing from 3.10 to 0.37 (P < 0.05) on the NPRS scale in both group analyses. The consequences of the present study showed that ART and PIR techniques have statistically significant differences in the post-treatment value of NPRS score between group analyses (P < 0.05) and for both group analyses (P < 0.001).
The PRTEE scores improved significantly by ART after the application of 12 sessions of four weeks (P < 0.05).[18] The present study showed that PRTEE scores, although improved by ART, but more significantly improved by PIR (P < 0.05) as compared to the ART (P > 0.05), followed by 12 sessions of four weeks. Kaux et al. recommended that PRTEE is the best scale for evaluating pain, functional performance in LE-affected patients, and improvement in ADLS following post-intervention programs.[19] This evidence supported the present study that the PRTEE scale evaluated and significantly improved after applying ART and PIR techniques.
This study speculates that both interventions can be effective in a clinical setup with or without conventional treatment protocol for long-term and better improvements. However, the PIR technique is more effective because it directly corrects muscle imbalance than ART.
Limitations
The study consists of a small number of patients. Due to limited time, long-term follow-up could not be done.
CONCLUSION
Both the ART and PIR methods were effective, but the PIR techniques, along with conventional therapy, were found to be much better than the ART group for reducing pain on a NPRS, improving grip strength by a handheld dynamometer and patient-rated LE evaluation questionnaire with a marked increase in functional performance of normal ADLS after 12 treatment sessions. The results were statistically significant for Group B in terms of mentioned outcome measures based on mean differences.
Recommendations
Further research is advocated to check the long-term effectiveness of interventions by proceeding with follow-up sessions
Interventions should be applied to a larger population, targeting the other groups of muscles to see favorable outcomes.
ACKNOWLEDGMENT
We want to express our gratitude to all who volunteered to get involved in the study.
AUTHORS’ CONTRIBUTIONS
AH contributed to conception and design, AH and SH contributed to data collection, TA contributed to data analysis, and SH contributed to article drafting, and contributed to critical article analysis and proofreading. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The study was approved by “Riphah International University, Lahore Campus” Research and Ethics Committee (ref no: RCRS-RE-MS-OMPT/Sp19/006) on November 30, 2019.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Lateral epicondylitis and physical exposure at work? A review of prospective studies and meta-analysis. Arthritis Care Res. 2016;68:1681-7.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of active release technique and myofascial release technique on pain, grip strength and functional performance in patients with chronic lateral epicondylitis. Int J Physiother Res. 2014;2:488-94.
- [Google Scholar]
- Overuse tendon conditions: Time to change a confusing terminology. Arthroscopy. 1998;14:840-3.
- [CrossRef] [PubMed] [Google Scholar]
- Tendinopathy: Update on pathophysiology. J Orthop Sports Phys Ther. 2015;45:833-41.
- [CrossRef] [PubMed] [Google Scholar]
- Lateral and medial epicondylitis: Role of occupational factors. Best Pract Res Clin Rheumatol. 2011;25:43-57.
- [CrossRef] [PubMed] [Google Scholar]
- Lateral elbow tendinopathy: Development of a pathophysiology-based treatment algorithm. Orthop J Sports Med. 2016;4:2325967116670635.
- [CrossRef] [PubMed] [Google Scholar]
- Tennis elbow (lateral epicondylitis) In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2019.
- [Google Scholar]
- Evaluation of sleep position for possible nightly aggravation and delay of healing in tennis elbow. JAAOS Glob Res Rev. 2019;3:e082.
- [CrossRef] [PubMed] [Google Scholar]
- Lateral epicondylitis of the elbow. Rev Bras Ortop. 2012;47:414-20.
- [CrossRef] [PubMed] [Google Scholar]
- A study to compare the effect of muscle energy technique and positional release technique on pain and cervical rom in patients with chronic upper trapezitis. Int J Sci Res. 2019;8
- [Google Scholar]
- Effectiveness of active release technique and muscle energy technique in adhesive capsulitis. Int J Res Pharm Sci. 2017;8:693-8.
- [Google Scholar]
- Mets and oscillating energy manual therapy in chronic lateral epicondylosis: A comparative study. Int J Res Pharm Sci. 2019;10:1914-9.
- [CrossRef] [Google Scholar]
- Efficacy of active release technique in tennis elbow-a randomized control trial. Indian J Physiother Occup Ther. 2012;6:132.
- [Google Scholar]
- Comparison of effects of leukocyte-rich and leukocyte-poor platelet-rich plasma on pain and functionality in patients with lateral epicondylitis. Arch Rheumatol. 2018;33:73-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic release of resistant tennis elbow. Egypt J Hosp Med. 2019;76:3595-9.
- [CrossRef] [Google Scholar]
- A comparative study of muscle energy technique versus cyriax technique in lateral epicondylitis among professional Indian cooks 2019 In: Corpus ID: 197860728.
- [Google Scholar]
- Efficacy of muscle energy technique with plyometric exercises in chronic lateral epicondylitis. Int J Health Sci Res. 2019;9:108-14.
- [Google Scholar]
- Cross-cultural adaptation and validation of the patient-rated tennis elbow evaluation questionnaire on lateral elbow tendinopathy for French-speaking patients. J Hand Ther. 2016;29:496-504.
- [CrossRef] [PubMed] [Google Scholar]







