Translate this page into:
Correlation between body mass index and quadruple hamstring autograft size
2 Department of Orthopedics, Ministry of National Guard - Health Affairs; Department of Pediatrics, Ministry of National Guard - Health Affairs, Riyadh, KSA
3 Department of Medicine, King Abdulaziz Medical City, Riyadh, KSA
4 Department of Orthopedics, Ministry of National Guard - Health Affairs; King Abdullah International Medical Research Center, Riyadh, KSA
Corresponding Author:
Monerah M Annaim
Department of Orthopedics, King Abdulaziz Medical City, Riyadh 14611
KSA
monerahannaim@gmail.com
| How to cite this article: Aljuhani WS, Alamri SG, Alsharif SA, Annaim MM. Correlation between body mass index and quadruple hamstring autograft size. J Musculoskelet Surg Res 2019;3:200-203 |
Abstract
Objectives: Anterior cruciate ligament (ACL) tear is a common sports injury affecting the knee joint in the Middle East and worldwide. Providing an adequate graft is required to prevent revision surgery. This study aims to determine if the body mass index (BMI) can be used as a predictor of the hamstring autograft size. Methods: Data of 48 consecutive patients, who underwent ACL reconstruction using quadruple hamstring autograft technique in the same institute by the same surgeon, were retrospectively reviewed. Skeletally immature patients and those who underwent revision ACL surgeries were excluded. Patients' anthropometric measurements were collected. Quantitative data from the patients' charts were included in the descriptive statistics. Results: The mean age of our cohort was 30.3 ± 6.3 years, with a mean height of 1.7 ± 7.8 m and a mean weight of 81.3 ± 14.6 kg. Mean BMI was 27.8 ± 5, and mean graft size was 7.8 ± 0.5 mm. Results showed that the correlation between the BMI and the autograft size was statistically insignificant. Other variables have no association with the autograft size in the linear regression model. Conclusion: Our study showed no correlation between anthropometric measurements and the autograft size; therefore, these measurements were not able to determine the diameter of the autograft. Further studies looking into thigh diameter and ethnicity and radiological studies with a larger sample size are recommended.Introduction
Anterior cruciate ligament (ACL) injury is one of the common sports injuries in Saudi Arabia. Most of those injuries occur in young patients especially at the age of 20 years, with males more commonly affected than females.[1] The hamstring graft is usually taken from the semitendinosus tendon because it is the longest among hamstring tendons.[2] This type of graft can be either a double-striped semitendinosus or gracilis with semitendinosus, creating a four-striped (quadruple) graft that is stronger and more stable. The hamstring graft might not be as strong as the patellar tendon graft, but it is preferred in Islamic countries as it serves the religious needs, such as praying and kneeling, which is difficult with the patellar graft due to pain and difficulties in kneeling postoperatively.[3],[4],[5] According to the literature, the minimum diameter of a successful graft is equal to or more than 7 mm in diameter.[6] Knowing the graft diameter preoperatively might help the surgeons to predict the success and failure of the autograft that will be harvested.[6] Previous studies conducted have shown that height, thigh diameter, and possibly the body mass index (BMI) can be good predictors of the ACL graft size.[6],[7],[8],[9] This study aims to determine if the preoperative measurements such as the patient's height, weight, and BMI would have any correlation with the quadruple hamstring graft diameter in the Saudi population.
Materials and Methods
Ethical approval was received from our local medical research center, and no consent was needed as there was no direct involvement of the patients. A retrospective cohort study of 48 consecutive patients (47 males; 1 female) who underwent ACL reconstruction using quadruple hamstring autograft technique in the same institute by the same surgeon was carried out. Skeletally immature patients and those who underwent revision ACL surgeries were excluded from the study. Patients' characteristics consisting of gender, age, height, weight, and BMI were collected preoperatively.
Surgery
The standard anesthesia technique was implemented on all patients. An oblique incision was performed over the proximal tibia, where the distal attachments of both semitendinosus and gracilis tendons are present. The tendons were harvested separately, and then they were cleaned and doubled to form the standard quadruple graft. The graft's diameter was then measured using the graft measurement gauge. Afterward, the femoral and tibial tunnels were drilled as per the size that was obtained. The graft was placed and fixed using the EndoButton™ at the femoral side using interference screw at the tibial shaft and secured further with soft-tissue stables.
Statistical analysis
The data were analyzed using the Statistical Package for the Social Sciences software version 22 (IBM, New York, USA). Quantitative data from the patients' charts were included in descriptive statistics, such as mean, standard deviation, and frequencies. Inferential statistics were used to determine the outliers with P < 0.05. Regression analysis was utilized to examine if the variables were predictors of the hamstring graft size. Pearson's correlation coefficient was used to examine the correlation between the anthropometric measures and hamstring autograft size. The confidence interval of 95% was used to determine if the diameter of the graft is within the calculated mean.
Results
Demographic characteristics
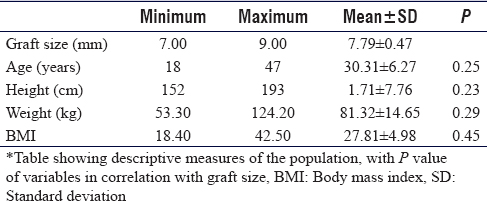
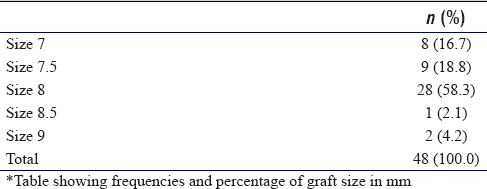
The mean of demographic characteristics and anthropometric measures of the patients is presented in [Table - 1]. The mean age was 30.3 ± 6.3 years, with a mean height of 1.7 ± 7.8 m and a mean weight of 81.3 ± 14.6 kg. Mean BMI was 27.1 ± 5, and mean graft size was 7.8 ± 0.5 mm [Table - 1]. The frequencies of graft size are shown in [Table - 2]. Majority of the patients (n = 28 [58.3%]) had a graft size of 8 mm intraoperatively [Table - 2].
Correlation
The correlation between graft size and age, height, weight, and BMI was studied. The correlation between graft size and BMI was r = 0.018, P = 0.451, that of graft size and age was r = −0.100, P = 0.250, that of graft size and height was r = 0.123, P = 0.203, and that of graft size and weight was r = 0.082, P = 0.291. No significant correlation between graft size and other variables was found.
Discussion
This study has shown no significant correlation between hamstring autograft diameter and BMI. Other measurements such as age, height, and weight also showed no correlation with all of the variables (P > 0.05). In contrast to our study, some anthropometric measurements, such as BMI, height, and thigh diameter, had shown a positive correlation with autograft size in other studies in different regions around the world. Stergios et al. in a study reviewing 61 patients in Greece reported that graft diameter had a moderate correlation with height, weight, and BMI.[6] Khashayar et al., in Iran, reported a positive correlation with height, weight, and BMI.[10] Height has shown to be a good predictor due to its correlation with graft diameter, which is in accordance with both Challa and Satyaprasad. and Pereira et al.[11],[12] Tuman et al. reviewed 106 patients and found a good correlation with some of the anthropometric data, and they also found that patients with short stature of 147 cm or below tend to have an insufficient graft diameter of <7 mm.[7] Other predictors have been included in a study by Treme et al. where they found a good correlation with lower-limb length and thigh circumference.[13] In a study of correlation with physical activity and fitness level by Treme et al. and Pichler et al., the authors found correlation neither with the length nor with the diameter of the flexor tendons.[13],[14] According to the literature review, the minimum diameter of a successful graft is to be equal or more than 7 mm, and the failure rate rises with smaller graft, as a graft size of 8.5 mm has shown higher success rate.[6],[9],[15] The hypothesis of predicting the graft size with BMI in order to prevent having a nonsuccessful graft cannot be supported by our study. We found that the majority of patients had a graft size diameter of 8 mm, and they accounted for 58.3% of the study population. Outliers in graft diameter of size 9 mm and 7 mm were appreciated. All the population had a graft size of 7 mm and above that is believed to be the cut point to a successful graft size. The graft diameter and length have been the focus in the surgical techniques used in the reconstructive surgeries. However, the contractility element and whether that plays a role in the success and failure of the grafts has not been studied well. Hamner et al. studied the biomechanical properties of the ACL tendon and found that those properties are highly affected by the diameter.[16] New surgical techniques have been currently used to increase the graft size through increasing the tendon strands. Moreover, by using the two cortical fixations, the use of folded grafts is not a difficulty anymore.[17],[18],[19],[20] In addition, those developed techniques help the surgeon to preserve the gracilis tendon for possible revision surgeries.[16] The study was conducted on fixed variables by the same surgeon, and it is the first study to be conducted in the region. Therefore, the results might reflect the anatomical variation in our region in comparison to other international studies. However, our study was based on one center, which makes it insufficient to prove such a hypothesis. Another limitation of our study is the limited time frame, which is the reason for the inadequate number of patients to have a proper correlation. Gender is not a useful variable for comparison because the study had an inadequate number of females. The entire population in this study had sufficient size according to the literature; graft size of 7 mm or more. The requirement of prediction in the population of the Middle East and the conversion into the new technique in order to increase the diameter might not be required.
Conclusion
In the literature, while the correlation between anthropometric measurements and graft diameter has been studied, there is a dearth of regional studies reflecting the Middle East population. We strived to achieve the same. Our study showed no correlation between anthropometric measurements and the autograft size; therefore, these measurements were not able to determine the diameter of the autograft.
Recommendation
As our study was based in one center with a limited number of patients, further large-scale studies looking into thigh diameter and ethnicity and radiological studies with a larger sample size are recommended.
Ethical approval
Ethical approval was obtained from King Abdullah International Medical Research Center's (KAIMRC) RIYADH, SA.
Financial support
This study was financially supported by King Abdullah International Medical Research Center.
Conflicts of interest
There are no conflicts of interest.
Author's contributions
WSA and MMA conceived and designed the study, conducted research, provided research materials, and collected and organized data. SGA and SAA analyzed and interpreted data. MMA wrote the initial and final draft of the article and provided logistic support. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Sadat-Ali M, Sankaran-Kutty M. Sports injuries in Saudi Arabia. Br J Sports Med 1985;19:28-9. [Google Scholar] |
| 2. | Makihara Y, Nishino A, Fukubayashi T, Kanamori A. Decrease of knee flexion torque in patients with ACL reconstruction: Combined analysis of the architecture and function of the knee flexor muscles. Knee Surg Sports Traumatol Arthrosc 2006;14:310-7. [Google Scholar] |
| 3. | Sachs RA, Daniel DM, Stone ML, Garfein RF. Patellofemoral problems after anterior cruciate ligament reconstruction. Am J Sports Med 1989;17:760-5. [Google Scholar] |
| 4. | Shaieb MD, Kan DM, Chang SK, Marumoto JM, Richardson AB. A prospective randomized comparison of patellar tendon versus semitendinosus and gracilis tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med 2002;30:214-20. [Google Scholar] |
| 5. | Feller JA, Webster KE. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med 2003;31:564-73. [Google Scholar] |
| 6. | Stergios PG, Konstantinidis G, Konstantinos N, Efthymia P, Nikolaos K, Papadopoulos G. Alexandros adequacy of semitendinosus tendon alone for anterior cruciate ligament reconstruction graft and prediction of hamstring graft size by evaluating simple anthropometric parameters. Anat Res Int 2012;2012;8. [Google Scholar] |
| 7. | Tuman JM, Diduch DR, Rubino LJ, Baumfeld JA, Nguyen HS, Hart JM, et al. Predictors for hamstring graft diameter in anterior cruciate ligament reconstruction. Am J Sports Med 2007;35:1945-9. [Google Scholar] |
| 8. | Thomas S, Bhattacharya R, Saltikov JB, Kramer DJ. Influence of anthropometric features on graft diameter in ACL reconstruction. Arch Orthop Trauma Surg 2013;133:215-8. [Google Scholar] |
| 9. | Çeliktaş M, Gölpinar A, Köse Ö, Sütoluk Z, Çelebi K, Sarpel Y, et al. Prediction of the quadruple hamstring autograft thickness in ACL reconstruction using anthropometric measures. Acta Orthop Traumatol Turc 2013;47:14-8. [Google Scholar] |
| 10. | Mardani-Kivi M, Karimi-Mobarakeh M, Mirbolook A, Keyhani S, Saheb-Ekhtiari K, Hashemi-Motlagh K, et al. Predicting the hamstring tendon diameter using anthropometric parameters. Arch Bone Jt Surg 2016;4:314-7. [Google Scholar] |
| 11. | Challa S, Satyaprasad J. Hamstring graft size and anthropometry in South Indian population. J Clin Orthop Trauma 2013;4:135-8. [Google Scholar] |
| 12. | Pereira RN, Karam FC, Schwanke RL, Millman R, Foletto ZM, Schwanke CH, et al. Correlation between anthropometric data and length and thickness of the tendons of the semitendinosus and gracilis muscles used for grafts in reconstruction of the anterior cruciate ligament. Rev Bras Ortop 2016;51:175-80. [Google Scholar] |
| 13. | Treme G, Diduch DR, Billante MJ, Miller MD, Hart JM. Hamstring graft size prediction: A prospective clinical evaluation. Am J Sports Med 2008;36:2204-9. [Google Scholar] |
| 14. | Pichler W, Tesch NP, Schwantzer G, Fronhöfer G, Boldin C, Hausleitner L, et al. Differences in length and cross-section of semitendinosus and gracilis tendons and their effect on anterior cruciate ligament reconstruction: A cadaver study. J Bone Joint Surg Br 2008;90:516-9. [Google Scholar] |
| 15. | Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE, et al. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy 2012;28:526-31. [Google Scholar] |
| 16. | Hamner DL, Brown CH Jr., Steiner ME, Hecker AT, Hayes WC. Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: Biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am 1999;81:549-57. [Google Scholar] |
| 17. | Calvo R, Figueroa D, Figueroa F, Vaisman A, Schmidt-Hebbel A, Morales N, et al. Five-strand hamstring autograft versus quadruple hamstring autograft with graft diameters 8.0 millimeters or more in anterior cruciate ligament reconstruction: Clinical outcomes with a minimum 2-year follow-up. Arthroscopy 2017;33:1007-13. [Google Scholar] |
| 18. | Lavery KP, Rasmussen JF, Dhawan A. Five-strand hamstring autograft for anterior cruciate ligament reconstruction. Arthrosc Tech 2014;3:e423-6. [Google Scholar] |
| 19. | Lee RJ, Ganley TJ. The 5-strand hamstring graft in anterior cruciate ligament reconstruction. Arthrosc Tech 2014;3:e627-31. [Google Scholar] |
| 20. | Sasaki S, Tsuda E, Hiraga Y, Yamamoto Y, Maeda S, Sasaki E, et al. Prospective randomized study of objective and subjective clinical results between double-bundle and single-bundle anterior cruciate ligament reconstruction. Am J Sports Med 2016;44:855-64. [Google Scholar] |
Fulltext Views
1,545
PDF downloads
409





