Translate this page into:
Debridement, antibiotics, and implant retention in a fracture-related infection with flexible forearm nail in situ: A case report of a successful outcome in an adolescent
*Corresponding author: Ganesh S. Dharmshaktu, MS. Department of Orthopaedics, Government Medical College, Haldwani, Uttarakhand, India. drganeshortho@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dharmshaktu GS. Debridement, antibiotics, and implant retention in a fracture-related infection with flexible forearm nail in situ: A case report of a successful outcome in an adolescent. J Musculoskelet Surg Res. doi: 10.25259/JMSR_466_2024
Abstract
Debridement, antibiotics, and implant retention (DAIR) is a well-described strategy for arthroplasty-related infections, resulting in good outcomes in selected cases. Fracture-related infection (FRI) poses a significant challenge to bone healing and the final outcome. FRI becomes a nagging problem for the treating physician and the patient alike. Various treatment modalities are described for the management of FRI, and one is selected based on the patient and disease characteristics. FRI in pediatric age is an uncommon entity. We hereby describe our case of an adolescent boy with FRI of the ulna bone in the setting of a well-fixed both-bone forearm fracture. FRI was successfully managed following the principle of DAIR with periodic debridement. Compliant follow-up and regular dressing can result in an uneventful healing of the FRI. DAIR can be a good option in an otherwise healthy pediatric case with implants in situ involving a segment of the forearm bone. A progressively encouraging result, following DAIR, should be checked before further continuation of the treatment. DAIR in selected cases, thus, is a viable option against FRI in pediatric forearm fractures.
Keywords
Complication
Debridement, antibiotics and implant retention
Flexible nailing
Forearm fractures
Infection
Open fracture
Pediatric
INTRODUCTION
Pediatric open forearm fractures are uncommon injuries and have the potential for later complications, including fracture-related infection (FRI), delayed healing, or non-union. Displaced pediatric forearm fractures are routinely managed with flexible nails and the procedure is largely safe and effective.[1] Usually, minor complications are noted with flexible nails and most of them are related to prominent nail ends.[2] Radius nailing is reported to have more complications than ulnar nailing, but most complications are minor, usually resolved with time, and do not require any unplanned surgery. Infection following flexible forearm nailing is reported in many studies as superficial soft-tissue infection around prominent nail ends, which finally heals by regular dressing, oral antibiotic, or hardware removal in recalcitrant cases.[2,3] Fulminant osteomyelitis or chronic bone infections are not widely reported after using flexible forearm nails. A low complication rate following elastic forearm nailing is reported in a large series of 201 cases (202 fractures).[4] Localized infection following a pre-existing open wound is a challenging complication, but there is no consensus on its management. The debridement, antibiotics, and implant retention (DAIR) method, widely utilized in infected scenarios such as that following major joint arthroplasties, has also been selectively utilized in FRI.[5] The successful use of the DAIR method in a pediatric case, having an infected segment of the ulna with a flexible nail in situ, is described here with relevant details. As the literature regarding, the use of DAIR in pediatric FRI cases is scant, and the following report aims to enrich the literature in this regard and improve future studies in this context.
CASE REPORT
A 14-year-old adolescent male presented to us with a history of injury following a fall from a moving vehicle into the road. There was immediate pain, deformity, and an open bleeding wound over the volar aspect of the mid-forearm region. He was rushed to us and provided first aid and cleaning of the wound. There was an approximately 3 × 2 cm open wound over the volar middle forearm [Figure 1a]. There was no visible bone, and the distal neurovascular status was intact. He could actively move his fingers and wrist. A radiograph of the forearm was done, and it revealed diaphyseal fractures in both bone forearms [Figure 1b]. On closer inspection, a radio-opaque foreign body was noted near the fracture site. The wound was cleaned in the emergency with copious lavage and visible dirt, and one small stone piece was removed. Following the cleaning and dressing of the wound, a protection slab was applied [Figure 1c]. The fracture was then planned to be fixed following an adequate debridement of the open wound. Thorough cleaning and debridement of the wound were done during the operation until it was healthier, and a small stone piece as the embedded foreign body was removed. After achieving a healthier wound, the forearm fracture was then managed by flexible titanium elastic nails for the radius and ulna [Figure 2a]. The ulna nail was easily introduced, and a mini-incision was used in the dorsal forearm region to assist with radius nailing. The wound was closed in layers and a protection plaster slab was applied.
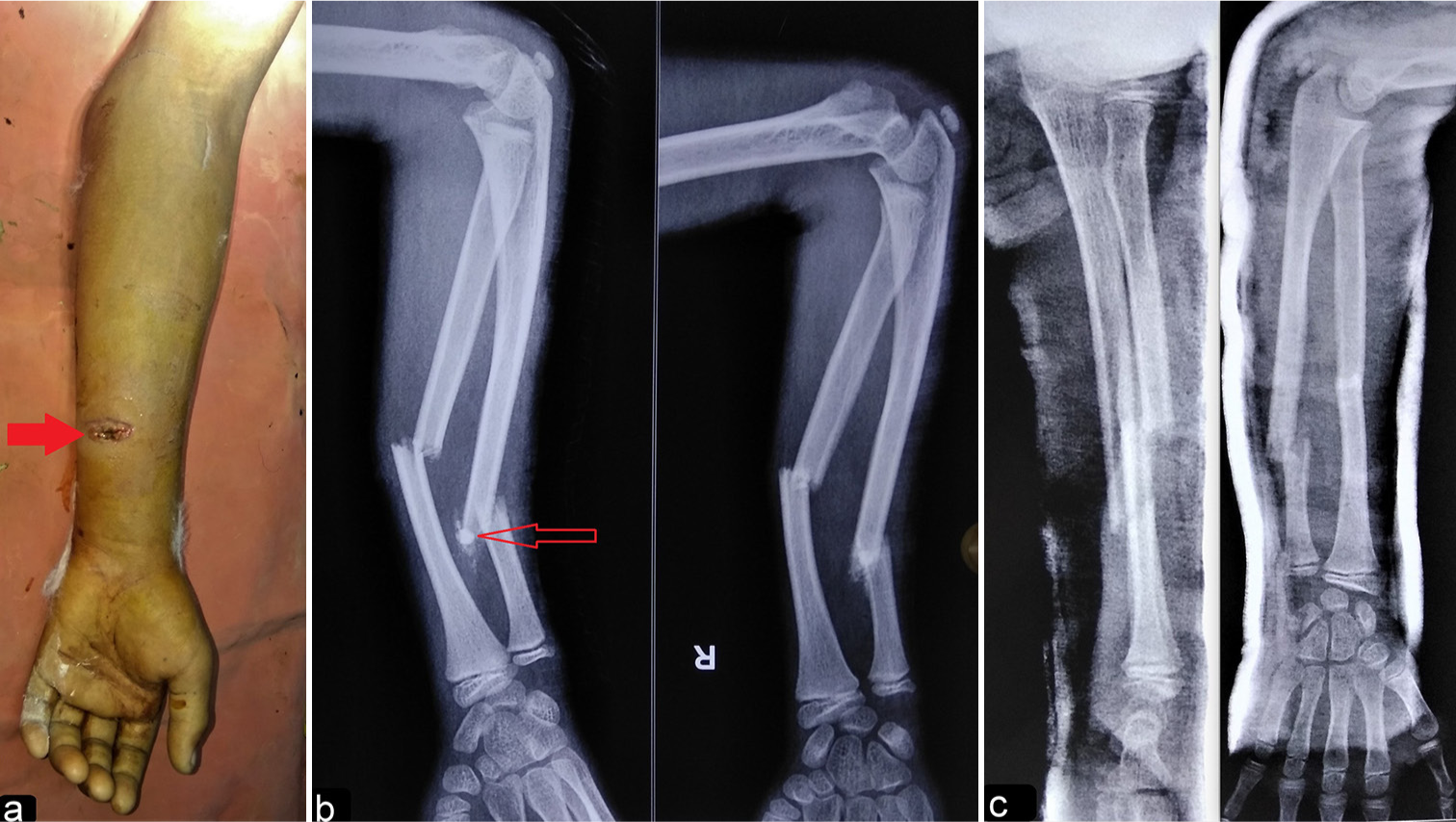
- (a and b) The clinical image shows the forearm injury with a wound over the volar aspect (red thick arrow), corresponding to the ulna region (red hollow arrow) in a both-bone forearm fracture. (c) The radiograph following the cleaning, debridement, removal of foreign body (stone), and plaster slab application.
Postoperatively, intravenous antibiotic ceftriaxone 1 g was given for 5 days, followed by oral cefuroxime 250 mg twice daily for the next 14 days. Ceftriaxone and amikacin are the standard antibiotics for routine use for Gram-positive and negative coverage, respectively, at our hospital based on institutional antibiograms. The perioperative period was uneventful, and the stitches were removed on the 12th day. The plaster slab was continued for 2 more weeks and removed after that, followed by the initiation of active range of motion exercises for the forearm. After 2 months of surgery, serous discharge was noted from the ulnar wound, and the radiographs revealed cortical irregularity noted over the corresponding ulnar region [Figure 2b]. The cell counts were not remarkable and there were no systemic features of infection. The wound underwent debridement in the operation theater under regional anesthesia and deep-tissue cultures were taken for Gram stain, acid–fast bacillus staining, and fungal culture. The presence of Staphylococcus aureus, sensitive to third-generation cephalosporins, was identified in the culture. Regular dressing and intravenous ceftriaxone were continued for 4 weeks, followed by 4 more weeks of oral therapy. The discharge became gradually scanty and serious over the course of treatment. The provisional diagnosis of localized FRI was made and regular dressing resulted in wound healing and discharge cessation. At the 4-month follow-up, no apparent infection or discharge was present, though the radiographs showed gradual cortical healing over the infected site [Figure 2c]. At the 13-month follow-up, the forearm wound was completely healed [Figure 3a], and the fractures showed sound union and healing of the infection with no radiological evidence of bony lysis, lucency, or sequestra [Figure 3b]. The patient had a full regain of elbow and forearm rotation movements and was painlessly performing activities of daily living while awaiting implant removal in the future [Figure 3c and d]. The patient, however, did not turn up for implant removal due to a change of address to a distant area. We were informed, when contacted telephonically, that he consulted a nearby hospital for the same.
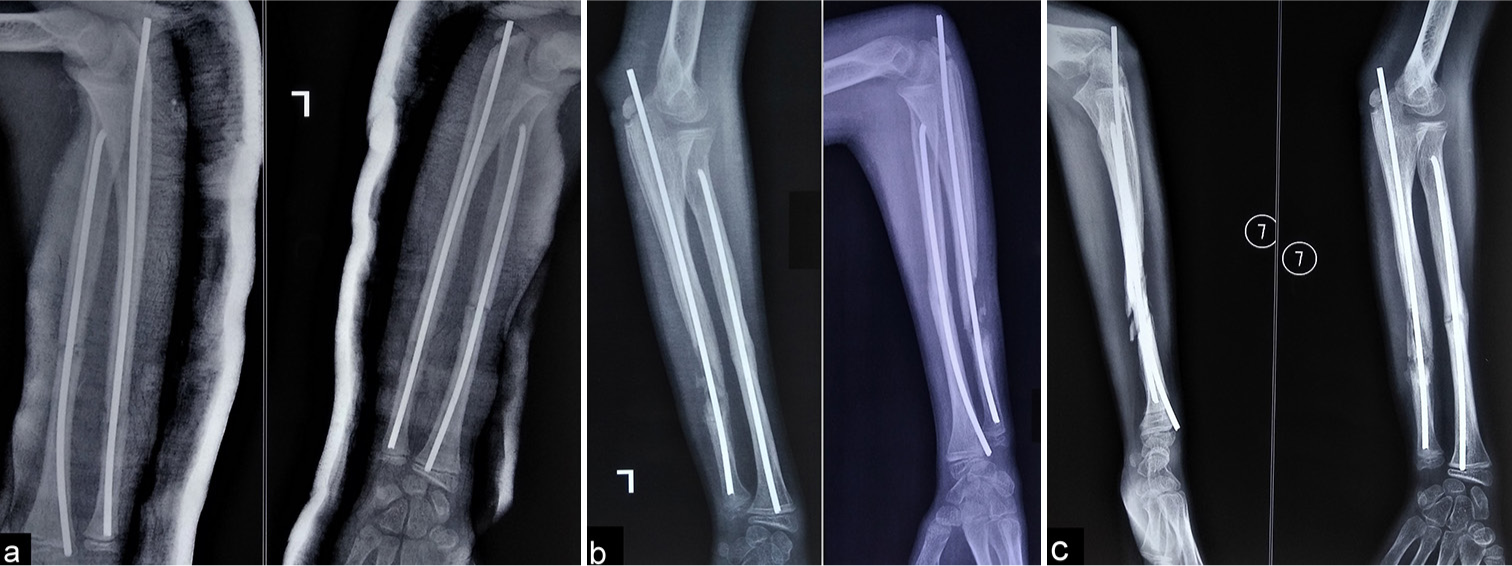
- (a) The radiograph shows well-reduced fracture fixation with flexible nails in the radius and ulna. (b) Cortical irregularity and localized infection were noted over the ulna. (c) The infection was managed with regular dressing and implant retention.

- (a and b) The final clinical image shows the healed wound, along with a completely united fracture. (c and d) The full regain of elbow and pronation-supination movement is noted in the final follow-up.
DISCUSSION
Flexible nails have reduced operative time and hospital stay, and when compared to plate fixation, the complication rates (refracture, infection, implant failure, and non-union) are comparable.[6,7] As low-grade superficial infection is seen in most cases, complicated bone infections are largely rare. Only one case of osteomyelitis was noted in a large series of 553 children treated with flexible forearm nailing.[7] Our case had a pre-existing open wound with an embedded foreign body, and infection occurred despite the best precautions. It was noted as an undesirable complication. Despite adequate debridement, a protracted course with serous discharge and localized osteomyelitis was noted.
DAIR has been practiced and advocated in post-arthroplasty infections or prosthetic joint infections as a viable treatment option.[8] DAIR has also been described as a viable option in FRI.[9] Our case met the confirmatory criteria of FRI as per the description by Metsemakers et al., with the presence of a sinus over the ulna, discharge of pus, and S. aureus isolated from the deep culture during the course of treatment.[10] Our case was delayed FRI as per the criteria used in a previous publication that classifies FRI into three types – early (<2 weeks), delayed (2–10 weeks), and late (>10 weeks).[10,11] The success of our treatment may have been positively affected by the proper use of DAIR. Early initiation of DAIR following FRI has been reported to yield better outcomes, and if it is started within 10 weeks of FRI, it may be even more effective.[12]
The recent FRI prevention strategy is a multidisciplinary care approach. It includes well-coordinated brainstorming between the consultant, hospital infection control, and primary team members (including the anesthesia and nursing team).[13]
A multidisciplinary team approach is recommended to manage FRI comprehensively.[14] In many centers of developing nations, such elaborate teams are not widely available, and thus, dependence on personal or eminence-based evidence determines the course of management.
DAIR is among three common treatment options for FRI, with removal (or exchange of implant) or removal.[9,15] The selection of one treatment is based on various factors, such as the organism, host, and environment (bone and soft-tissue status).
DAIR approach is suitable option in the setting of a short duration of ongoing symptoms, well-reduced and fixed fracture with stable implants and presence of good soft tissue envelope. Multistage implant exchange is reserved for compromised local and systemic host characteristics, recalcitrant pathogens, intramedullary implants, or those cases with long-standing biofilm, reinfections, or failed DAIR attempts.[15] A short overview of the three common treatment strategies, based on various literature cited in the article, is presented here for general readership [Table 1].
| Treatment method | Basic prerequisite | Pros | Cons |
|---|---|---|---|
| Implant removal | Well-united fracture |
|
|
| Implant retention | Well-perused soft-tissue envelope. Good debridement necessary |
Retention may help the union |
|
| Implant revision | Patient literacy for prognosis and outcome | Good for impending infected non-union |
|
CONCLUSION
Judicious use of DAIR in FRI of pediatric forearm bones may be a viable option for FRI. Early use of DAIR may help in infection control along with the fracture union in selected cases.
ETHICAL APPROVAL
Institutional Review Board approval is not required.
DECLARATION OF PATIENT CONSENT
The author certifies that he has obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published, and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY STATEMENT
The author confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Stable elastic intramedullary nailing for fractures of the femur in children. J Bone Joint Surg Br. 2004;86:954-7.
- [CrossRef] [PubMed] [Google Scholar]
- Complications of elastic stable intramedullary nailing for treating paediatric long bone fractures. J Orthop. 2013;10:17-24.
- [CrossRef] [PubMed] [Google Scholar]
- Delayed healing of forearm shaft fractures in children after intramedullary nailing. J Pediatr Orthop. 2008;28:303-6.
- [CrossRef] [PubMed] [Google Scholar]
- Low complication rate of elastic stable intramedullary nailing (ESIN) of pediatric forearm fractures: A retrospective study of 202 cases. Medicine (Baltimore). 2017;96:e6669.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome and risk factors for recurrence of early onset fracture-related infections treated with debridement, antibiotics and implant retention: Results of a large retrospective multicentre cohort study. Injury. 2022;53:3930-7.
- [CrossRef] [PubMed] [Google Scholar]
- Pearls and pitfalls of forearm nailing. J Pediatr Orthop Soc North Am. 2021;3:218.
- [CrossRef] [Google Scholar]
- Failures and complications in intramedullary nailing of children's forearm fractures. J Child Orthop. 2010;4:159-67.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2013;56:e1-25.
- [CrossRef] [Google Scholar]
- The surgical management of fracture-related infection. Surgical strategy selection and the need for early surgical intervention. J Orthop. 2024;50:36-41.
- [CrossRef] [PubMed] [Google Scholar]
- Fracture-related infection: A consensus on definition from an international expert group. Injury. 2018;49:505-10.
- [CrossRef] [PubMed] [Google Scholar]
- Current concepts of fracture-related infection. Int J Clin Pract. 2023;2023:4839701.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of duration of infection on outcome of debridement and implant retention in fracture-related infection. Bone Joint J. 2021;103B:213-21.
- [CrossRef] [PubMed] [Google Scholar]
- General treatment principles for fracture-related infection: Recommendations from an international expert group. Arch Orthop Trauma Surg. 2020;140:1013-27.
- [CrossRef] [PubMed] [Google Scholar]
- Prevention of fracture-related infection: A multidisciplinary care package. Int Orthop. 2017;41:2457-69.
- [CrossRef] [PubMed] [Google Scholar]
- The DAIR-procedure in fracture-related infection-When and how. Injury. 2024;55(Suppl 6):111977.
- [CrossRef] [PubMed] [Google Scholar]






