Translate this page into:
Did COVID-19 restrictions affect post-operative rehabilitation of patients who underwent arthroscopic management of femoroacetabular impingement?
*Corresponding author: Mohamed A. Abdelsalam, Department of Orthopedic and Trauma Surgery, Assiut University Hospitals, Faculty of Medicine, Assiut University, Assiut, Egypt. mradi@aun.edu.eg
-
Received: ,
Accepted: ,
How to cite this article: Abdelsalam MA, Abdelmowla RA. Did COVID-19 restrictions affect post-operative rehabilitation of patients who underwent arthroscopic management of femoroacetabular impingement? J Musculoskelet Surg Res, 2023;7:278-87.
Abstract
Objectives:
This study aimed to evaluate the impact of a home-based exercise rehabilitation protocol for post-arthroscopy femoroacetabular impingement (FAI) patients compared to the routine physiotherapy protocol and investigate the effect of COVID-19 restrictions on patient rehabilitation and clinical outcomes.
Methods:
The study used a prospective cohort with a matched-pair comparison research design. The study group included 26 patients who underwent arthroscopic management of FAI through osteochondroplasty and suture anchor repair from July 2020 to June 2022. Thirty patients from the existing database who underwent arthroscopic management of FAI from June 2018 to June 2020 were included as a control group. Patient demographic and baseline data, the modified Harris Hip Score and the international Hip Outcome Tool-12 (iHOT-12) Score, the surgical satisfaction questionnaire, and the COVID-19 rehabilitation questionnaire were investigated for both groups. Patients in the study group received home-based exercise booklets.
Results:
The iHOT-12 score was significantly improved in the study group compared to the control group at 6 and 12 months (72 ± 22.33, 80.85 ± 13.46 vs. 58.03 ± 23.89, 62.1 ± 19.52, P = 0.029, P < 0. 001, respectively).
Conclusion:
Home-based exercise protocols successfully managed to achieve better outcomes in the study group assessed through the iHOT-12 Score at 1 year postoperatively. However, patients’ satisfaction was lower in the study group than in the control group.
Keywords
Arthroscopy
COVID-19
Femoroacetabular impingement
Post-operative pain
Rehabilitation
INTRODUCTION
Femoroacetabular impingement (FAI) is a clinical syndrome resulting from bone overgrowth that develops around the femoral head and along the acetabulum. Continuous or repetitive loading may cause abnormal contact on bony prominences, the labrum, and articular cartilage and may precipitate labral damage and cartilage degeneration.[1]
FAI is classified into three categories: Cam type, which results from bony growth at the femoral head-neck junction; pincer type, which is caused by extra bone growth at the acetabular side; and mixed type, which involves both types of FAI; the cam and pincer.[2]
The diagnosis of FAI is based on clinical and radiographic parameters, including patient history, physical examination findings, and radiological parameters. Plain radiographs are applied to assess bony morphologies, while magnetic resonance arthrography (MRA) diagnoses acetabular labral tears and articular cartilage pathology. Alpha angles are used to quantify the concavity of the femoral head-neck junction, where cam deformity is diagnosed when the alpha angle is >50°.[3]
In the past 30 years, the field of hip arthroscopy has changed tremendously. In a short time, it has progressed from adjunctive tools with clinical applications limited to diagnosis and pathology resection to safe, anatomic reconstructive procedures.[4] Hip arthroscopy for treating FAI associated with labral tear through osteochondroplasty and labral repair is the approach of choice because it is safe, minimally invasive, and requires a shorter recovery time than open surgery.[5]
Recently, many specific rehabilitation programs have been developed that usually divide the recovery of patients into different stages, focusing on restoring function, and improving the joint’s range of motion to facilitate a safe return to usual activity.[5-9] However, programs may vary significantly considering post-operative restrictions, rehabilitation activities, and the time points for the activities.[10] Therefore, comparative studies are needed to guide post-operative rehabilitation and conduct a standardized program after arthroscopic management of FAI.[5,6,8] As consequences of the COVID-19 pandemic, partial lockdown and associated strict social restrictions may have influenced the recovery of those patients due to restricted access to medical services, reduced or absent physiotherapy, exercises, support from relatives and friends, and face-to-face follow-up.
The primary aim of this study was to design and evaluate the impact of a home-based exercise rehabilitation protocol for patients who underwent arthroscopic management of FAI in comparison to the routine physiotherapy protocol. The secondary aim was to evaluate the impact of social restrictions imposed due to the COVID-19 pandemic on rehabilitation and outcomes as perceived by the patients and whether these affected their satisfaction rates.
The researchers hypothesized that patients following arthroscopy for FAI would have limited access to supervised post-operative rehabilitation with concerns that the COVID-19 restrictions would negatively affect recovery.
MATERIALS AND METHODS
Research design
This study was a prospective cohort with a matched-pair comparison research design.
Patients and setting
The present study was conducted in the arthroscopy unit and outpatient clinic in Assiut University Hospitals during the study period from July 2020 to June 2022 with a minimum 1-year follow-up. A prospective study group of 26 consecutive patients who underwent primary hip arthroscopy for FAI associated with a labral tear was included and treated through osteochondroplasty and suture anchor repair. Postoperative rehabilitation for those patients included home-based exercise protocol.
A matched control group of 30 patients from existing databases (from June 2018 to June 2020) with a 1-year follow-up was included in the study. Post-operative rehabilitation for those patients included routine hospital physiotherapy protocol.
Patients’ ages ranged from 18 to 55 years old. All patients were practicing sports at the level of recreational activity. Osteochondroplasty and suture anchor repair were performed on all included patients. Patients with systemic immune diseases, degenerative arthritic hips, hip infections, hip deformities, and hip revision surgery were excluded from the study.
Data collection tools
Patients’ assessment sheet
This was used to assess demographic data, comorbidities, body mass index (BMI), and sports level.
Modified Harris hip score (mHHS)
It was developed by Byrd and Jones (2000) to assess patient-reported outcomes in hip arthroscopy surgery.[11] It is a valid and reliable tool demonstrating excellent test/retest reliability (intraclass correlation coefficient [ICC], 0.91) and construct validity.[9] It contains eight items that represent the different aspects of pain and function. The total score ranged from “0” = worst functional outcome and maximum pain level to “100” = best functional outcome and least pain level. The interpretation of the outcome is as follows: <70 = poor result, 70–79 = fair result, 80–89 = good result, and >90 = excellent result.
International hip outcome tool-12 (iHOT-12) score
This was developed by Griffin et al. (2012) to assess patient-reported measures of health-related quality of life in hip surgery. It is a valid and reliable tool demonstrating good test/ retest reliability with an ICC of 0.89. It contains 4-domains (12 items) representing symptoms and functional limitations, sports and recreational activities, job-related concerns, and social, emotional, and lifestyle concerns. It is scored on a visual analog scale from 0 to 100, with 100 indicating the best function and the fewest symptoms.[12]
Surgical satisfaction questionnaire
It is a valid and reliable 8-item questionnaire developed by Haff et al. (2011) to assess patient satisfaction following pelvic surgery. The internal consistency reliability by Cronbach’s alpha was 0.79. The response to the first six questions was graded using a 5-point Likert scale from 1 = very unsatisfied to 5 = very satisfied. The last two questions answers were 1 = never and 5 = yes.[13]
COVID-19 rehabilitation questionnaire
It is an 8-question questionnaire developed by MacDonald et al. (2021). It was modified by the researchers to be six questions to assess the responses of the study group toward the effect of COVID-19 restriction on their recovery. The researchers removed two questions that did not fulfill the criteria of our patients, as all patients underwent surgery and received home-based exercise. The response to each question was recorded as yes or no.[14]
Procedure
All patients diagnosed with FAI associated with labral tears scheduled for primary arthroscopy were recruited from the arthroscopy unit in Assiut University Hospitals. All eligible patients who agreed to participate in the study for 1 year (July 2020–June 2022) and were followed up for 1 year ending in June 2022 were included (study group). A matched-pair control group was collected from the registry system from June 2018 to June 2020, including 1-year data collection and 1-year follow-up. All patients’ diagnoses were confirmed by pelvic radiographs (anteroposterior/lateral) and MRA.
Patients of the study group with COVID-19 restrictions were educated and encouraged by the researchers to manage daily living activities, home-based exercises (teaching booklet), and mobilization. Patients were, then, reviewed at 2 weeks postoperatively in the outpatients’ clinic for removal of sutures and continuation of post-operative rehabilitation protocol. The researchers reinforced the importance of the commitment to the post-operative rehabilitation protocol and reviewed patients by phone and/or e-mail every month and in the outpatients’ clinic if patients’ conditions necessitated that. Patients were, then, followed up at 6 and 12 months postoperatively for clinical and radiological evaluation. Radiological evaluation was done with a pelvic radiograph.
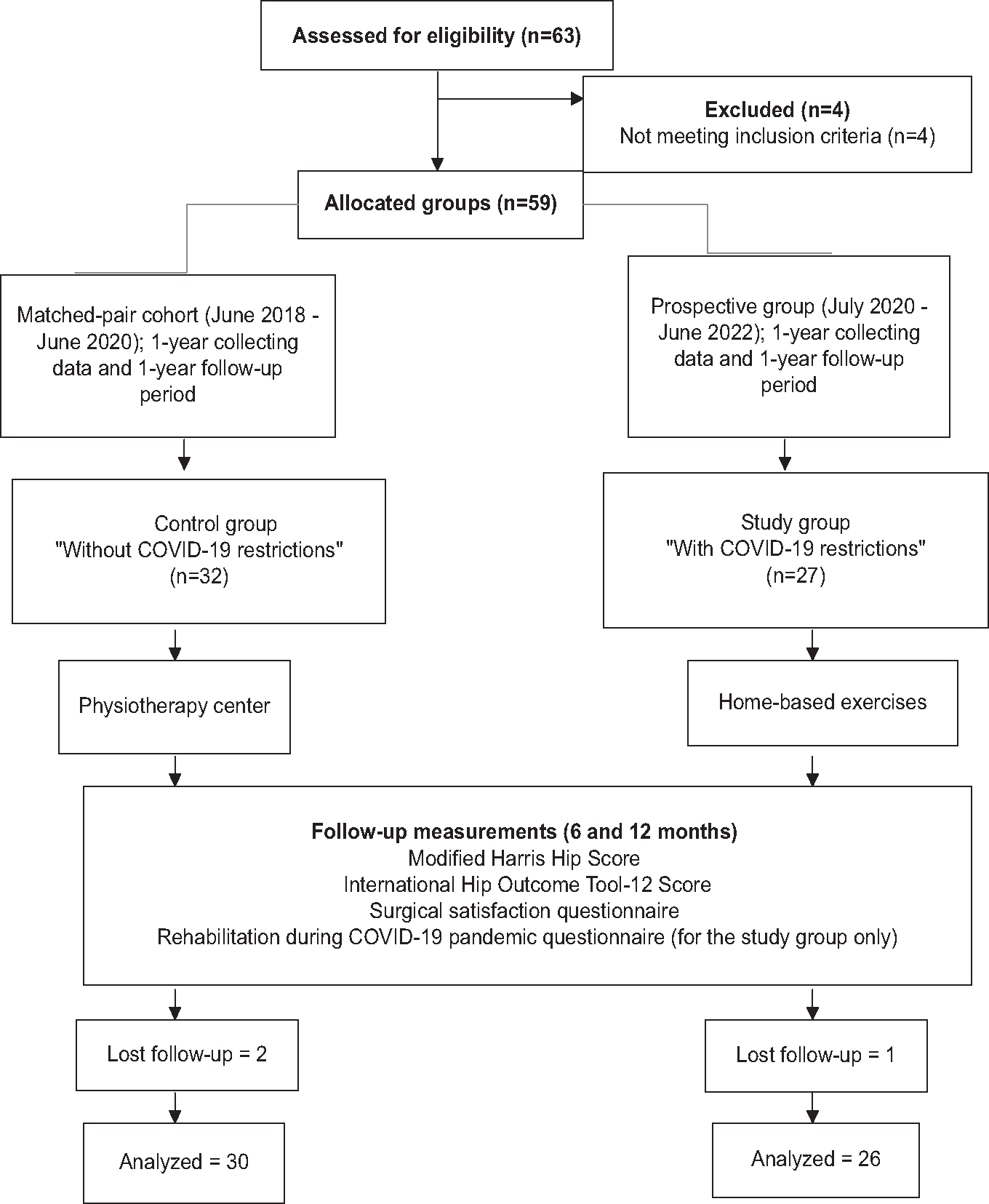
- Flow diagram of study sample recruitment
According to the registry, patients of the cohort control group before COVID-19 restrictions were referred to different physiotherapy centers to complete their post-operative rehabilitation period. They performed exercises under the supervision of physiotherapists. All follow-up appointments were conducted with the attendance of patients at the outpatients’ clinic 2 weeks, 6 weeks, 3 months, 6 months, and 12 months postoperatively. Clinical and radiological evaluations were recorded using the same study evaluation methods.
All patients were evaluated at 6 and 12 months postoperatively for their different aspects of pain and function using mHHS and for quality of life and abilities to return to an active lifestyle using the iHOT-12 score. Patients in both groups reported their satisfaction with their outcomes after 12 months postoperatively using a surgical satisfaction questionnaire to evaluate the impact of arthroscopic management and post-operative rehabilitation on their satisfaction level.
Patients in the study group were evaluated at 6 and 12 months postoperatively for their responses toward the effect of the COVID-19 pandemic and social restrictions on the care received, recovery, and mental health. Patients were asked if they felt that the COVID-19 pandemic limited their recovery after arthroscopic management of FAI associated with a labral tear and the reasons behind it. Furthermore, they were asked whether they received physiotherapy, had access to health-care services during recovery if diagnosed with COVID-19 after surgery, if any mental health deterioration occurred, and if they encountered anxiety and/or depression. This was addressed by the COVID-19 rehabilitation questionnaire.
Post-operative rehabilitation protocol
Home-based exercises (teaching booklet)
It was developed by the researchers after reviewing many national and international literature.[15-17] It was developed in our home language with illustrated photos to meet the needs of our patients. It was reviewed with five experts (three orthopedic staff and two medical-surgical nursing staff) to ensure the content’s clarity, comprehensiveness, and validity. Fewer modifications were performed based on experts’ opinions and patients’ needs. Emphasis was placed on reducing pain, swelling, and early restoration of hip function. Patients progressed to isometric quadriceps contractions (four sets of ten repetitions twice daily), flexion, extension and ankle circumduction (four sets of ten repetitions twice daily), hip flexion in supine trailing heel by stretcher (four sets of ten repetitions twice daily), passive hip circumduction (two series of 5 min daily), ambulation using “two” crutches without weight-bearing on the affected limb, a passive stretch of hip flexors, and keeping the hip in a neutral rotation position as soon as they were comfortable usually during the first 2 weeks. Passive hip circumduction (two series of 5 min daily), walking using a crutch, stationary biking with an elevated saddle without resistance for 15 min, and hip abductors (four sets of ten repetitions twice daily) commenced for 3–6 weeks. Progression to walking without crutches, static biking with an elevated saddle and without resistance for 25 min, lying in a prone position and extension of the hip with the knee in full extension, knee 45º flexion, and knee 90º flexion with resistance in the TheraBand rubber ankle of 1.5 m length and medium resistance (four sets of fifteen repetitions once daily), and sitting with full extension of the knee using TheraBand rubber ankle resistance of 1.5 m length and medium resistance (four sets of twenty repetitions once daily) commenced from 6 weeks to 6 months.
Routine hospital physiotherapy protocol
Patients of the control group underwent post-operative rehabilitation protocol in different physiotherapy centers. The post-operative rehabilitation protocol started as soon as possible during the first 2 weeks with a range of motion exercises for the hip. After 2 weeks to 6 months, postoperatively, patients progressed to abdominal core exercises and sacroiliac stabilization protocol in addition to electrical stimulation, infrared therapy, and therapeutic ultrasound. Patients progressed to gradual muscle strength; quadriceps strength began at four kilograms at 6 weeks. Patients were seen by physiotherapists in the rehabilitation center 3 times per week for 6 months to complete their postoperative rehabilitation period.
Statistical analysis
Categorical variables were described by count and percentages, whereas continuous variables were described by the mean and standard deviation (SD). The Chi-square test was used to compare categorical variables, while the t-test was used to compare continuous variables. A two-tailed P < 0.05 was considered statistically significant. All analyses were performed with the IBM SPSS 26.0 software.
RESULTS
The means of the age of the control and study groups were 37.13 ± 6.75 and 28.42 ± 7.72 years, respectively [Table 1]. Over three-quarters of the control and study groups were males (76.7% and 76.9%, respectively). Less than two-thirds of the control and study groups had a normal BMI (63.3% and 61.5%, respectively).
| Items | Control group (n=30) | Study group (n=26) | ||
|---|---|---|---|---|
| No. | % | No. | % | |
| Age | ||||
| <30 years | 5 | 16.6 | 18 | 69.2 |
| 30–40 years | 17 | 56.7 | 5 | 19.2 |
| More than 40 years | 8 | 26.7 | 3 | 11.5 |
| Sex | ||||
| Male | 23 | 76.7 | 20 | 76.9 |
| Female | 7 | 23.3 | 6 | 23.1 |
| Body mass index | ||||
| Normal weight (18.5–24.9 kg/m2) | 19 | 63.3 | 16 | 61.5 |
| Overweight (25–29.9 kg/m2) | 7 | 23.3 | 10 | 38.5 |
| Obese (30 or higher kg/m2) | 4 | 13.4 | 0 | 0.0 |
Control and study groups were matched and similar regarding the baseline assessment. All the studied patients in both groups were diagnosed with FAI with a labral tear in MRA [Table 2]. The right side was affected in 50% of the study group patients and 36.7% of the control group. Furthermore, 36.7% of control group patients and 19.2% in the study group had bilateral FAI. Cam-type was found in 40% of patients in the control group and 23.1% in the study group. Pincer type was found in 11.5% of patients in the study group. Sixty percentages of patients in the control group and 65.4% in the study group had both cam and pincer forms of FAI (mixed type). The mean duration of symptoms for patients in the control and study groups was 22.5 ± 19.36 and 16 ± 0 months, respectively. More than half (56.7%) of the patients in the control group and less than two-thirds (61.5%) of patients in the study group had positive flexion, abduction, and external rotation (FABER) test. Most patients (96.7%) in the control group and all patients (100%) in the study group had positive flexion, adduction, and internal rotation (FADDIR) test [Table 2].
| Items | Control group (n=30) | Study group (n=26) | Control group (n=30) | Study group (n=26) | ||
|---|---|---|---|---|---|---|
| No. | % | No. | % | Mean±SD | Mean±SD | |
| Type of FAI | ||||||
| Cam | 12 | 40.0 | 6 | 23.1 | - | - |
| Pincer | 0 | 0.0 | 3 | 11.5 | - | - |
| Mixed (cam and pincer) | 18 | 60.0 | 17 | 65.4 | - | - |
| Side | ||||||
| Right | 11 | 36.7 | 13 | 50.0 | - | - |
| Left | 8 | 26.6 | 8 | 30.8 | - | - |
| Bilateral | 11 | 36.7 | 5 | 19.2 | - | - |
| Duration of symptoms in months | - | - | - | - | 22.5±19.36 | 16±0 |
| Flexion-abduction-external rotation test | ||||||
| Positive | 17 | 56.7 | 16 | 61.5 | - | - |
| Negative | 12 | 43.3 | 10 | 38.5 | - | - |
| Flexion, adduction and internal rotation test | ||||||
| Positive | 29 | 96.7 | 26 | 100.0 | - | - |
| Negative | 1 | 3.3 | - | - | - | - |
| Labral tear in MRA | 30 | 100.0 | 26 | 100.0 | - | - |
| Pre-operative alpha angle | - | - | - | - | 63.18±9.06 | 61.58±6.19 |
| Post-operative alpha angle | - | - | - | - | 45.58±4.97 | 53±2.32 |
| Tönnis classification of arthritic changes | - | - | - | - | 1.17±2.98 | 2.31±4.06 |
| Treatment of labrum (Labral repair using anchors suturing) | 30 | 100.0 | 26 | 100.0 | - | - |
| Number of anchors | ||||||
| Two | 17 | 56.66 | 23 | 88.46 | - | - |
| Three | 11 | 36.67 | 3 | 11.54 | - | - |
| Four | 2 | 6.67 | - | - | - | - |
FAI: Femoroacetabular impingement, MRA: Magnetic resonance arthrography, SD: Standard deviation
Regarding pre-operative and post-operative alpha angles, the mean pre-operative alpha angles for patients in control and study groups were 63.18 ± 9.06 and 61.58 ± 6.19, respectively. The mean post-operative alpha angle for patients in control and study groups was 45.58 ± 4.97 and 53 ± 2.32, respectively. Regarding Tönnis classification of hip arthritic changes, the mean Tönnis classification of hip arthritic changes was 1.17 ± 2.98 for patients in the control group and 2.31 ± 4.06 for patients in the study group. All the studied patients (100%) in both groups were treated with arthroscopic management through osteochondroplasty (pincer resection, cam resection, or both according to the deformity type) and labral repair using anchor suturing. The majority of patients in the study group (88.46 %) and more than half of patients in the control group (56.66%) had two anchor sutures repair [Table 2].
No statistically significant difference (P = 0.059) was found between the control and study groups in pre-operative mHHS. Improvement in mHHS throughout the rehabilitation periods (6 and 12 months postoperatively) was observed in control (85.5 ± 17.04, 93.95 ± 5.78) and study (93.32 ± 12.41, 96.63 ± 4.71) groups. However, no statistically significant difference was observed in mHHS at 6 and 12 months postoperatively (P = 0.058, P = 0.064, respectively).
A statistically insignificant difference (P = 0.051) was found between the control (34.83 ± 20.94) and study (46.7 ± 23.13) groups in pre-operative iHOT 12 scores. A statistically significant improvement was observed (6 and 12 months postoperatively) through iHOT 12 score in control (58.03 ± 23.89, 62.1 ± 19.52) and study (72 ± 22.33, 80.85 ± 13.46) groups (P = 0.029, P < 0. 001, respectively).
A high statistically significant difference was found between the control (31.33 ± 0.48) and study (29.54 ± 1.98) groups through surgical satisfaction questionnaire score (P < 0.001) [Figure 1]. Both groups were satisfied with their outcomes, but the control group showed a higher satisfaction score than the study group.
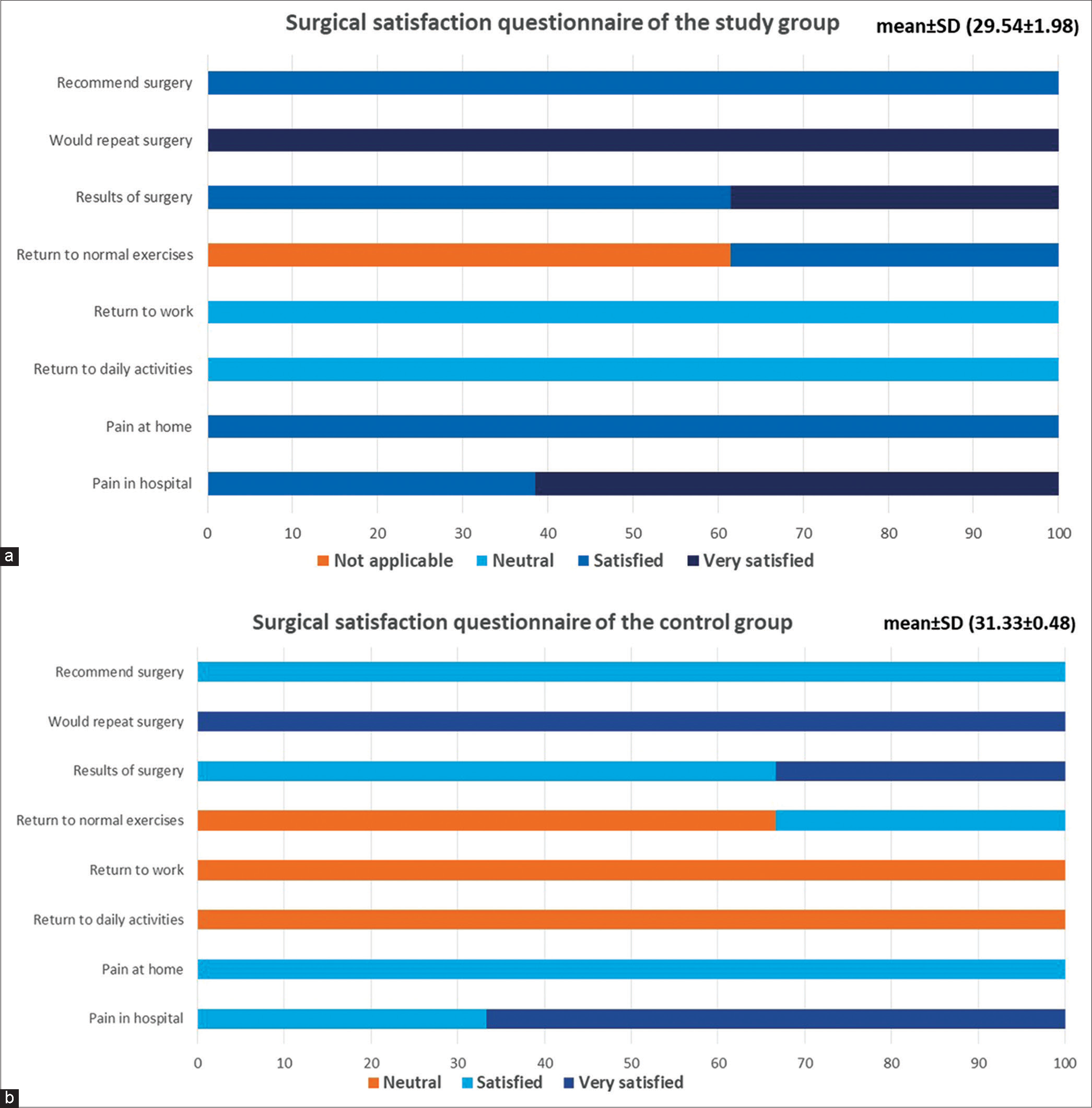
- (a) Surgical satisfaction questionnaire for patients of the study group and (b) surgical satisfaction questionnaire for patients of the control group.
In the study group, all patients were very satisfied with the questions concerning whether, looking back, they would repeat surgery, were satisfied with pain control at home after surgery, and recommended the surgery to someone else. All patients reported neutral responses regarding the time to return to daily activities and work. Sixty-two percentages of patients were very satisfied with pain control at the hospital after surgery and were satisfied with the results of surgery and rehabilitation. Non-applicable responses were reported in 61.5% of patients to concerns about time to return to normal exercises after surgery due to COVID-19 restrictions [Figure 1a].
All patients in the control group were very satisfied with the question concerning whether, looking back, they would repeat surgery, were satisfied with pain control at home after surgery, and would recommend surgery to someone else. Two-thirds of patients (66.7%) were very satisfied with pain control at the hospital after surgery and the results of surgery and rehabilitation. They had a neutral response to the question concerning the time to return to normal exercises after surgery. All patients reported neutral responses regarding the amount of time to return to daily activities and return to work [Figure 1b].
As illustrated in [Figure 2], all patients in the study group reported limited recovery due to the COVID-19 pandemic. All of them reported that they had limited recovery due to limited access to care or rehabilitation centers and restrictions of partial lockdown. All patients reported having access to health-care services about concerns while recovering. Twenty-one (80.8%) were diagnosed with COVID-19 after surgery and felt anxious. All patients in the study group did not have mental health deterioration or depression during the partial lockdown.
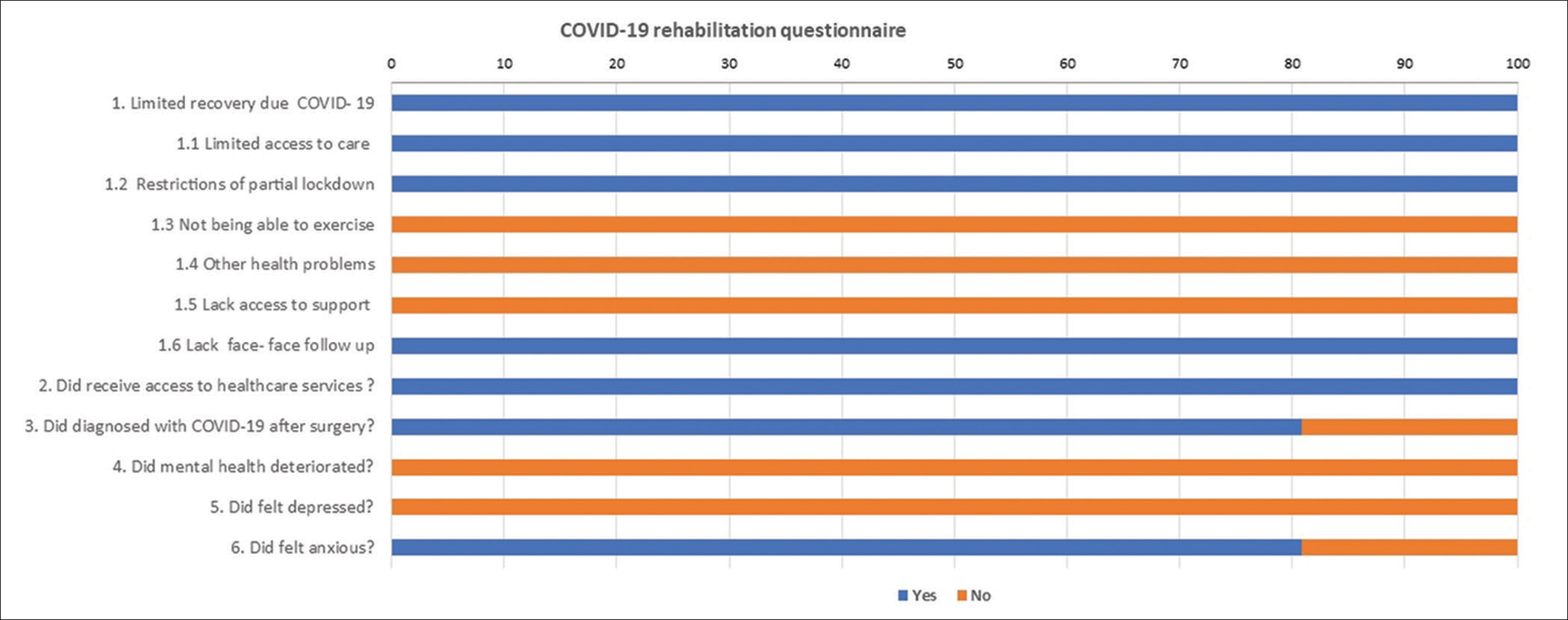
- Responses of the study group patients for COVID-19 rehabilitation questionnaire.
A statistically significant improvement was found between non-COVID-19 patients and COVID-19-affected patients of the study group by the iHOT 12 scores (P = 0.028). The mean (±SD) iHOT 12 score for patients diagnosed with COVID-19 after surgery was 78.48 (±13.47) versus 90.8 (±8.43) for patients not diagnosed with COVID-19 after surgery. The same significant improvement was found regarding mHHS (P = 0.038). The mean (±SD) mHHS for patients diagnosed with COVID-19 after surgery was 96.03 (±5.0) versus 99.14 (±1.9) for patients not diagnosed with COVID-19 after surgery.
DISCUSSION
This study demonstrated that the designed home-based exercise rehabilitation protocol showed improvement at 6 and 12 months postoperatively, with more obvious improvement after 12 months as regards the functional outcomes, health-related quality of life, and pain for patients in the study group. Patients in both the study and control groups were satisfied with the outcome of the arthroscopic management of FAI. However, patients in the study group still felt that their recovery had been affected by the restrictions imposed by the partial COVID-19 lockdown.
Post-operative rehabilitation was significantly affected during the COVID-19 pandemic as the clustering risk was higher in outpatients than in inpatient rehabilitation due to uncontrolled exposure.[18] Therefore, the health education of patients undergoing arthroscopic management of FAI is an important issue, which was the reason for designing a home-based exercise rehabilitation protocol.[19,20]
In the present study, a comparison of patients’ demographic and baseline characteristics, including pre-operative data, clinical and radiological findings, and operative data, showed that both groups were similar. It demonstrated that FAI associated with labral tears occurs in young adults, mostly males, with positive FABER and FADDIR tests and some arthritic changes. All types, cam, pincer, or mixed, were treated with arthroscopic intervention. This result is similar to that of Müller-Torrente et al. (2021), who conducted a study on 90 patients who underwent hip arthroscopy (45 in the control group and 45 in the experimental group) and stated that the demographic and baseline data of the patients were similar.[21] They reported that FAI occurs in young adults, mostly males with positive FABER and FADDIR tests and all patients were treated with hip arthroscopy.
In the pre-operative measurement, the mean scores obtained from the mHHS in the control and study groups were close, indicating poor pre-operative conditions, and there was a statistically non-significant difference between them. This result demonstrated that both groups had similar scores and characteristics. Both groups had improvement in mHHS from preoperatively to 6 and 12 months postoperatively after rehabilitation, with significant improvement in the study group. This result is similar to that of Müller-Torrente et al. (2021). They stated that the baseline pre-surgery mHHS was poor in both the experimental and control groups.[21]
In the pre-operative measurement, the mean scores obtained from the iHOT 12 score in the control and study groups were close, indicating poor pre-operative status, and there was a statistically insignificant difference between them. This result clarified that both groups had similar scores and characteristics. Both groups had improvement in iHOT 12 scores from preoperatively to 6 and 12 months postoperatively after rehabilitation, with significant improvement in the study group. This is similar to the result of Horton et al. (2021), who conducted a study on 51 patients divided into three groups (17 patients in each group) who underwent hip arthroscopy and reported no statistical difference in the mean score of pre-operative iHOT 12.[19] Postoperatively, after rehabilitation, all groups significantly improved their iHOT-12 scores from pre-operative to 3-month post-operative evaluations.
From the researchers’ point of view, the better improvement in outcomes of patients in the study group regarding mHHS and iHOT 12 scores could be due to the effect of the home-based rehabilitation protocol, continuous follow-up by the researchers through phone and e-mail communication, and outpatient clinic visits when patients’ conditions necessitated that.
In the present study, both groups were satisfied with their post-operative outcomes after rehabilitation, with statistically significant differences. Patients in the study group demonstrated less satisfaction with their outcomes due to their inability to return to normal exercise routines, which responded to this question as not applicable due to COVID-19 restrictions. A statistically significant relationship was found between patients’ satisfaction and the mHHS and iHOT-12 scores in both groups. This result is in agreement with MacDonald et al. (2021), who conducted a study on 48 patients who underwent primary total hip arthroplasty and 57 patients who underwent total knee arthroplasty to evaluate the effect of social restrictions of COVID-19 on their outcomes and satisfaction. They reported that social restrictions due the COVID-19 pandemic limited recovery, with worse outcome measure scores and lower patient satisfaction rates.[14]
The present study demonstrated that all patients in the study group reported limited recovery due to the COVID-19 pandemic. They reported that they had limited recovery due to limited access to care or rehabilitation centers and the restrictions of partial lockdown. They all reported having access to health-care services when concerns arose while recovering. Most of them were diagnosed with COVID-19 after surgery.
Before and after surgery, patients should access sufficient information and support from the arthroscopy staff as well as their friends and families. Post-operative recovery and rehabilitation plans should start before surgery to keep patients alert about their recovery phases and reduce their anxiety levels.[22,23] However, the COVID-19 pandemic may have diminished access to support services during postoperative rehabilitation and recovery. Due to the restrictions of partial lockdown, patients felt unable to connect with the health team and have a face-to-face follow-up. This is supported by reasons given by the patients in the study group who felt that recovery and rehabilitation were limited as a result of the restrictions of the COVID-19 pandemic.
Despite the perceived limitations on the recovery and rehabilitation of patients in the study group during the partial lockdown, the mHHS and iHOT-12 scores were significant compared to patients in the control group. Patients in this group showed better outcomes regarding the mHHS and iHOT-12 scores than patients in the control group.
According to the COVID-19 rehabilitation questionnaire, all patients in the study group received support from friends and family and did not have mental health deterioration or depression during the partial lockdown, in contrast to MacDonald et al. (2021), who stated that the COVID-19 pandemic resulted in a lack of support from friends and family during the post-operative rehabilitation and recovery period. Despite the same improvement in function and satisfaction levels, it profoundly affected patients’ mental health and perception of recovery during the follow-up period following arthroplasty. Patients felt the social restrictions enjoined by the COVID-19 pandemic limited recovery and rehabilitation and were associated with worse Oxford hip scores, Oxford knee scores, quality of life scores, and a lower satisfaction rate. However, compared to the control cohort group, no difference was found in outcomes, such as the Oxford hip score, the Oxford knee score, or the satisfaction rate after total hip or knee arthroplasty.[14]
Strengths and limitations
To the best of our knowledge, this is the first prospective study with matched-pair control that evaluated the effect of COVID-19 restrictions on FAI patients who underwent hip arthroscopic osteochondroplasty and labral repair. Furthermore, the selection of one hip pathology made a point of strength that unifies the patient stratification. However, the study had limitations, including few patients, short-term follow-up, and lack of randomization.
CONCLUSION
The rehabilitation protocol following arthroscopic management of FAI proposed to patients in the study group achieved better benefits than the usual hospital physiotherapy rehabilitation protocol in terms of better functional outcomes, health-related quality of life, and pain reduction (mHHS, iHOT-12).
Recommendations
The results of this study proposed a model that can be considered for updating the usual hospital rehabilitation protocol aiming to improve the patients’ recovery following arthroscopic management of FAI.
AUTHORS’ CONTRIBUTIONS
MAA and RAA shared the study conception, study design, material preparation, data collection, data analysis, and the first draft of the manuscript. MAA performed the surgical operations for both groups of patients. All authors carefully reviewed and approved the final draft of the manuscript and were responsible for the content.
ETHICAL APPROVAL
The research design was reviewed and approved by the Ethics Review Board Committee at the Faculty of Nursing, Assiut University, Assiut, Egypt, with registration number 4210031 on 28-5-2020. Informed consent from patients was taken and all data were kept confidential.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patients consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Femoroacetabular impingement and osteoarthritis of the hip. Can Fam Physician. 2015;61:1055-60.
- [Google Scholar]
- Hip arthroscopy for femoracetabular impingement in China: A review and meta-analysis. Orthop Surg. 2021;13:1721-9.
- [CrossRef] [PubMed] [Google Scholar]
- Advances in FAI imaging: A focused review. Curr Rev Musculoskelet Med. 2020;13:622-40.
- [CrossRef] [PubMed] [Google Scholar]
- Hip arthroscopy-state of the art in 2018. Sports Med Arthrosc Rev. 2018;26:185-9.
- [CrossRef] [PubMed] [Google Scholar]
- Postoperative rehabilitation after hip arthroscopy: A search for the evidence. J Sport Rehabil. 2015;24:413-8.
- [CrossRef] [PubMed] [Google Scholar]
- Variability and comprehensiveness of North American online available physical therapy protocols following hip arthroscopy for femoroacetabular impingement and labral repair. Arthroscopy. 2017;33:1998-2005.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of a physiotherapy rehabilitation program for individuals undergoing arthroscopic management of femoroacetabular impingement-the FAIR trial: A randomised controlled trial protocol. BMC Musculoskelet Disord. 2014;15:58.
- [CrossRef] [PubMed] [Google Scholar]
- Rehabilitation following hip arthroscopy-a systematic review. Front Surg. 2015;2:21.
- [CrossRef] [PubMed] [Google Scholar]
- Rehabilitation following hip arthroscopy: An evolving process. Int J Sports Phys Ther. 2014;9:765-73.
- [Google Scholar]
- A four-phase physical therapy regimen for returning athletes to sport following hip arthroscopy for femoroacetabular impingement with routine capsular closure. Int J Sports Phys Ther. 2017;12:683-96.
- [Google Scholar]
- Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16:578-87.
- [CrossRef] [PubMed] [Google Scholar]
- A short version of the International Hip Outcome Tool (iHOT-12) for use in routine clinical practice. Arthroscopy. 2012;28:611-6.
- [CrossRef] [PubMed] [Google Scholar]
- The surgical satisfaction questionnaire (SSQ-8): A validated tool for assessment of patient satisfaction following surgery to correct prolapse and/or incontinence. J Minim Invasive Gynecol. 2011;18:S49-50.
- [CrossRef] [Google Scholar]
- The effect of COVID-19 restrictions on rehabilitation and functional outcome following total hip and knee arthroplasty during the first wave of the pandemic. Bone Jt Open. 2021;2:380-7.
- [CrossRef] [PubMed] [Google Scholar]
- The physiotherapy for femoroacetabular impingement rehabilitation STudy (physioFIRST): A pilot randomized controlled trial. J Orthop Sports Phys Ther. 2018;48:307-15.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic surgery versus physiotherapy for femoroacetabular impingement: A meta-analysis study. Eur J Orthop Surg Traumatol. 2020;30:1151-62.
- [CrossRef] [PubMed] [Google Scholar]
- Physiotherapy as an initial treatment option for femoroacetabular impingement: A systematic review of the literature and meta-analysis of 5 randomized controlled trials. Am J Sports Med. 2020;48:2042-50.
- [CrossRef] [PubMed] [Google Scholar]
- The role of physical and rehabilitation medicine in the COVID-19 pandemic: The clinician's view. Ann Phys Rehabil Med. 2020;63:554-6.
- [CrossRef] [PubMed] [Google Scholar]
- Transition to telehealth physical therapy after hip arthroscopy for femoroacetabular impingement: A pilot study with retrospective matched-cohort analysis. Orthop J Sports Med. 2021;9:2325967121997469.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of the coronavirus (COVID-19) pandemic on surgical practice-Part 2 (surgical prioritisation) Int J Surg. 2020;79:233-48.
- [CrossRef] [Google Scholar]
- Benefits of a specific and supervised rehabilitation program in femoroacetabular impingement patients undergoing hip arthroscopy: A randomized control trial. J Clin Med. 2021;10:3125.
- [CrossRef] [PubMed] [Google Scholar]
- Factors influencing day surgery patients' quality of postoperative recovery and satisfaction with recovery: A narrative review. Perioper Med (Lond). 2019;8:3.
- [CrossRef] [PubMed] [Google Scholar]
- Holding it together-patients' perspectives on postoperative recovery when using an e-assessed follow-up: Qualitative study. JMIR Mhealth Uhealth. 2018;6:e10387.
- [CrossRef] [PubMed] [Google Scholar]






