Translate this page into:
Distal femur locked plate for fixation of open distal femur fracture
*Corresponding author: Mohammed Hussein H. Almwuad’a, MD. Department of Orthopedic, Faculty of Medicine, Amran University, Amran, Yemen. almwuadah@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Almwuada M. Distal femur locked plate for fixation of open distal femur fracture. J Musculoskelet Surg Res. doi: 10.25259/JMSR_10_2025
Abstract
Objectives:
This study aimed to evaluate the functional outcomes and complications of open distal femur fractures treated with primary open reduction and internal fixation (ORIF) using a locking compression plate (LCP) after debridement and wound irrigation.
Methods:
This prospective study included 53 patients with open distal femur fractures from May 2018 to May 2023. Inclusion criteria were open fractures requiring surgery, excluding skeletally immature patients, those with gunshot wounds, or polytrauma. Patients were treated with open reduction and internal fixation (ORIF) using an LCP and Sanders’ Functional Evaluation Scale assessed outcomes.
Results:
The study consisted of 41 males (77.4%) and 12 females (22.6%) with an average age of 33.3 years. Most injuries (75.5%) were due to road traffic accidents, followed by falls (15%) and industry/farm-related injuries (9.4%). The Gustilo-Anderson classification revealed 54.7% type 1, 32.1% type 2, and 13.2% type 3A fractures. Bone union was achieved in 77.4% of patients, with an average union time of 5.6 months. The average knee flexion was 87.16 ± 20°, with a mean of 104.8°. Based on Sander’s score, functional outcomes were excellent in 35.8% of patients, good in 39.6%, fair in 13.2%, and poor in 11.3%. Complications included delayed union (9.4%), surgical site infections (13.2%), deep vein thrombosis (5.7%), and knee stiffness (3.8%).
Conclusion:
Primary ORIF with LCP for open distal femur fractures leads to satisfactory functional outcomes in most cases. Early mobilization and proper postoperative care help reduce complications.
Keywords
Distal femur
Functional outcomes
Locking compression plate
Open fractures
Sanders’ functional evaluation scale
Surgical intervention
INTRODUCTION
Distal femur fractures are serious injuries that can result in varying degrees of long-term functional disability. With the growth of roadway networks and the increasing frequency of high-speed vehicle traffic, the incidence of severe trauma, including open femur fractures associated with polytrauma, has risen significantly. These traumatic events often result in a complex spectrum of both osseous and soft tissue damage.[1] Distal femur fractures constitute <1% of all fracture types, with approximately 5–10% classified as open fractures.[2,3]
Open distal femur fractures are particularly prone to complications such as infections, non-union, knee stiffness, and a reduction in range of motion (ROM).[4] Supracondylar femoral fractures typically exhibit a bimodal age distribution. Younger individuals often suffer high-energy injuries from events such as road traffic accidents, industrial accidents, or sports injuries, while the older age group, especially women, are more commonly affected by low-energy twisting injuries associated with osteoporosis.[5,6]
Distal femur fractures are classified based on the location and nature of the fracture, including extra-articular, intraarticular, unicondylar, intra-condylar, and bicondylar fractures, as well as the degree of fracture comminution.[7] The AO classification system is commonly used for these fractures [Figure 1].[7,8]
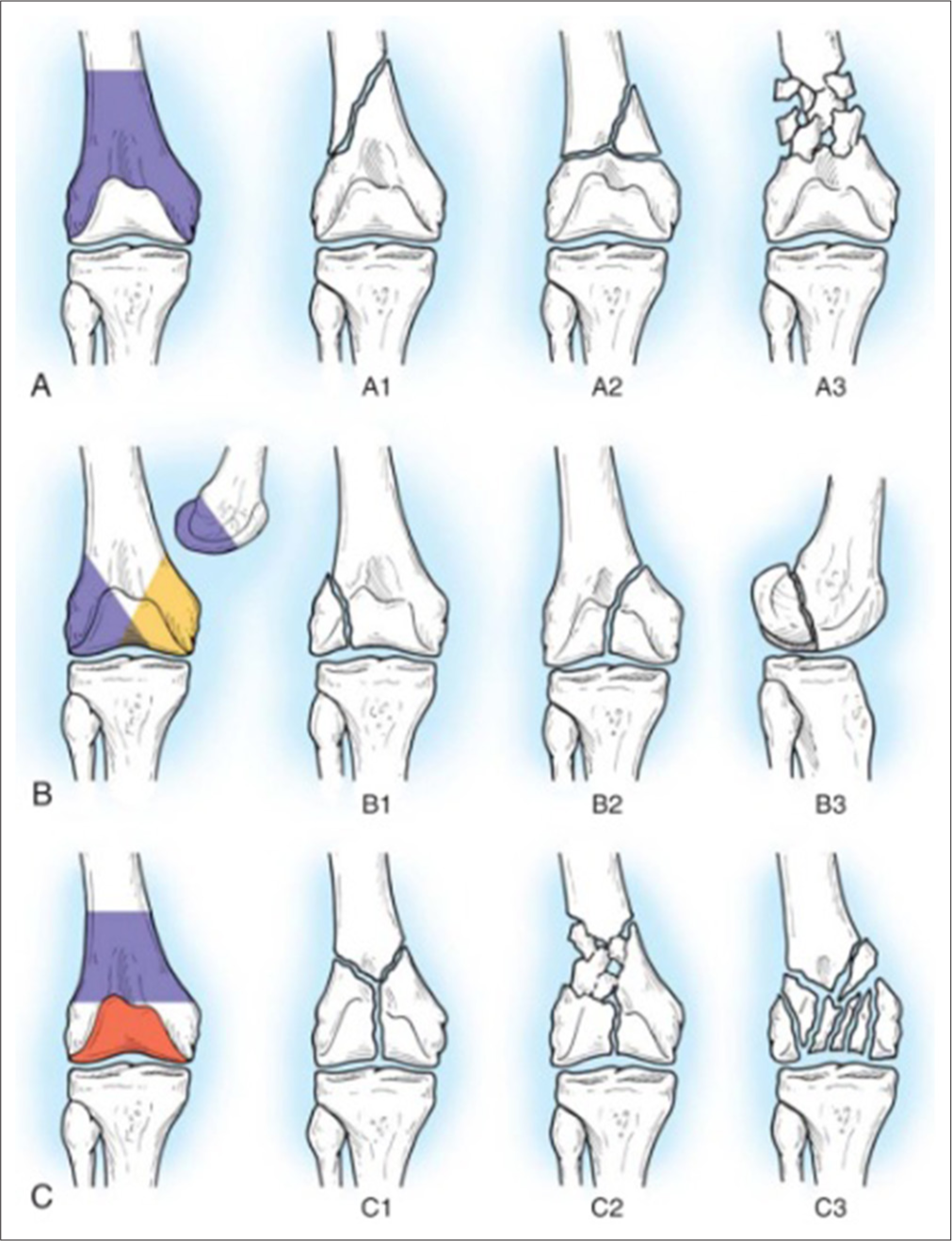
- Classification of fractures of distal femur described by Müller et al. Type A fractures involve the distal shaft only with (A1, A2, A3) varying degrees of comminution. Type B fractures are condylar fractures; type B1 is a sagittal split of the lateral condyle, type B2 is a sagittal split of the medial condyle, and type B3 is a coronal plane fracture. Type C fractures are T-condylar and Y-condylar fractures; type C1 fractures have no comminution, type C2 fractures have a comminuted shaft fracture with two principal articular fragments, and type C3 fractures have intra-articular comminution.
For open fractures, the Gustilo and Anderson classification is commonly used.[9] Historically, the management of open fractures has relied predominantly on prolonged hospitalization involving traction or external fixation. This approach is associated with numerous complications related to extended hospital stays, including loss of work hours and significant financial strain on the patient’s family. External fixators are linked to a considerable frequency of complications, including pin tract infections, malunion, late-onset angular deformities, joint stiffness, muscle wasting, extended recovery periods, higher reoperation rates, and patient compliance issues.[10,11,12] In contrast, surgical intervention can reduce hospitalization duration and facilitate recovery in a home setting. In addition, this method enables early rehabilitation, thereby mitigating the risks of joint stiffness and muscle atrophy.[13]
The goals of surgical treatment are anatomical reconstitution of the articular surface; reduction of the metaphyseal component of the fracture to the diaphysis and restoration of normal axial alignment, length, and rotation; stable internal fixation and early motion and functional rehabilitation of the limb.[14,15] Limited research has focused on the benefits of debridement and primary fixation for open fractures, and there is a lack of consensus on the optimal management strategies for these injuries.[16]
This study aimed to evaluate the functional outcomes and complications of open distal femur fractures treated with primary open reduction and internal fixation (ORIF) using a locking compression plate (LCP) after debridement and wound irrigation.
MATERIALS AND METHODS
This prospective study included 53 patients with open distal femur fractures admitted to Amran General Hospital between May 2018 and May 2023. The inclusion criteria consisted of patients with open distal femur fractures requiring surgical intervention, while skeletally immature patients, those who had gunshot wounds, vascular injuries, or polytrauma, were excluded [Figure 2a and b].
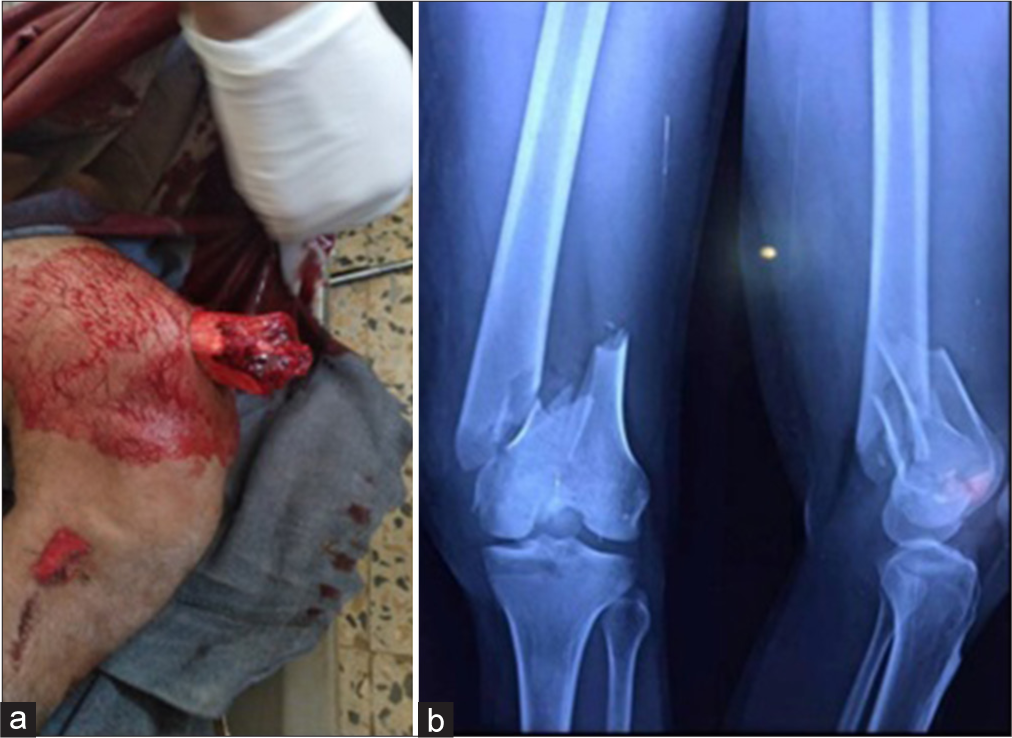
- (a) A 26-year-old patient with open distal femur fracture with bone exposed. (b) A radiograph of a patient shows a supracondylar femur with intra-articular extension.
Upon arrival at the emergency room, the team treated patients according to the advanced trauma life support protocol. A detailed examination of the neurovascular status was conducted, along with a full systemic evaluation for any additional injuries. A complete medical history and physical examination were performed to assess any underlying health issues, and laboratory tests were ordered to evaluate the patient’s surgical risk. Any bleeding was controlled using direct pressure and gauze bandages. If the patient was in shock, intravenous fluids and blood transfusions were administered. Photos of the wound were taken, and the first dose of antibiotics (2 g of cefazolin and 80 mg of gentamicin) was given, along with 1000 mg of intravenous paracetamol for pain relief. A splint was applied to immobilize the leg, and the patient was prepared for surgery.
The average time from injury to surgery was 8 h, ranging from 4 to 16 h. Surgery is usually performed under spinal or general anesthesia, with the patient positioned supine on a radiolucent table under C-arm guidance. A sandbag was placed under the buttock on the affected side. The wound was thoroughly examined, followed by copious irrigation with 6 liters of normal saline and extensive wound debridement. ORIF was performed through a lateral incision (usually different from a traumatic wound), starting at the lateral femoral condyle and extending proximally to ensure proper plate placement. At least four screws were placed above the most proximal fracture line. If needed, the incision was extended for a parapatellar approach. After performing a closed or open reduction for intra-articular and metaphyseal fractures, temporary stabilization was achieved using K-wires. Depending on the fracture’s geometry, stabilization was carried out using compression, bridging, or a combination. An anatomically pre-contoured LCP was inserted through a submuscular tunnel and laid flat against the femoral condyle. To secure the plate, a 4.5 mm bicortical screw was inserted into the proximal portion, followed by 6.5 mm screws for the metaphyseal and intra-articular fragments and locking bolts for the proximal and distal fragments [Figure 3] single lateral plate used in all cases. A drain was placed, and the wound was closed in layers.

- (a) Fracture fixation with distal femur locking plate pre-operative radiograph. (b) Fracture fixation with distal femur locking plate postoperative radiograph. (c) Fracture fixation with distal femur locking plate six months post-operative.
Post-surgery, patients are closely monitored and start moving early, usually within one day, to prevent complications like deep vein thrombosis (DVT) and help in faster recovery. The drain is removed 24 h later. Antibiotics are given intravenously for 3 days, then switched to oral for another 7 days. Sutures are removed on the 13th day after surgery, and most patients are discharged within 4 days. Post-operative physiotherapy is started early to promote joint mobility, strengthen muscles, and improve functional outcomes.
Demographic details (age and sex), fracture classification (Gustilo-Anderson and AO classification), and postoperative outcomes were recorded. Patients were followed up at 2 weeks, 1 month, and monthly intervals for up to 6 months to 3 years, with an average follow-up of 10 months. Once callus formation was observed at the fracture site, patients were allowed partial weight-bearing, and full weight-bearing was permitted after the clinical and radiological union was confirmed. Functional outcomes were primarily assessed based on bone union, infection rate, and knee ROM. The final evaluation was done 6 months after surgery using Sanders’ Functional Evaluation Scale [Table 1].[17]
| Function | Result | Points |
|---|---|---|
| Range of motion | ||
| Flexion | ||
| >125 | Excellent | 6 |
| 100-124 | Good | 4 |
| 90-99 | Fair | 2 |
| <90 | Poor | 0 |
| Extension | ||
| 0 | Excellent | 3 |
| ≤5 | Good | 2 |
| 6-10 | Fair | 1 |
| >10 | Poor | 0 |
| Deformation | ||
| Angulation | ||
| 0 | Excellent | 3 |
| <10 | Good | 2 |
| 10-15 | Fair | 1 |
| >15 | Poor | 0 |
| Shortening (cm) | ||
| 0 | Excellent | 3 |
| <1.5 | Good | 2 |
| 1.5-2.5 | Fair | 1 |
| >2.5 | Poor | 0 |
| Pain | ||
| None | Excellent | 10 |
| Occasional or with Changes in Weather or both | Good | 7 |
| With fatigue | Fair | 5 |
| Constant | Poor | 0 |
| Walking Ability | ||
| Walking | ||
| Unrestricted | Excellent | 6 |
| >30 minutes to <60 minutes | Good | 4 |
| <30 minutes | Fair | 2 |
| Walks at home, is confined to a wheelchair or is bedridden | Poor | 0 |
| Stair climbing | ||
| No limitation | Excellent | 3 |
| Holds rail | Good | 2 |
| One stair at a time | Fair | 1 |
| Elevator only | Poor | 0 |
| Return to work (A or B) | ||
| A. Employed before injury | ||
| Returned to preinjury job | Excellent | 6 |
| Returned to preinjury job with Difficulty | Good | 4 |
| Altered full-time job | Fair | 2 |
| Part-time job or unemployed | Poor | 0 |
| B. Retired before injury | ||
| Returned to preinjury lifestyle | Excellent | 6 |
| Needs occasional help | Good | 4 |
| Needs assistance at home with activities of daily living | Fair | 2 |
| Moved in with family or nursing home | Poor | 0 |
Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences version 24 software, and results were presented in frequencies, tables, and percentages.
RESULTS
Out of the 53 patients in the study, 41 (77.4%) were males, and 12 (22.6%) were females. The age distribution showed that 20 patients were over 40, while 33 were between 18 and 40. Most of the injuries (75.5%; 40 patients) were caused by road traffic accidents, 15% (8 patients) were due to falls, and 9.4% (5 patients) were related to industrial or farming accidents. Fracture classifications showed that 29 patients (54.72%) had Gustilo-Anderson type 1 fracture, 17 (32.1%) had type 2, and 7 (13.2%) had type 3A. There were no patients with 3B or 3C. According to the AO classification, 14 (26.4%) patients were categorized as A1, 5 (9.4%) as A2, 22 (41.5%) as C1, and 12 (22.6%) as C3 [Table 2].
| No of patients | Percentage | |
|---|---|---|
| Age | ||
| 18–40 years | 33 | 62.3 |
| >40 years | 20 | 37.7 |
| Sex | ||
| Male | 41 | 77.4 |
| Female | 12 | 22.6 |
| Mechanism of injury | ||
| Road traffic accidents | 40 | 75.5 |
| Fall down | 8 | 15 |
| Industry and farm-related injury | 5 | 9.4 |
| Gustilo type of fracture | ||
| Type 1 | 29 | 54.7 |
| Type 2 | 17 | 32.1 |
| Type 3A | 7 | 13.2 |
| AO classification | ||
| A1 | 14 | 26.4 |
| A2 | 5 | 9.4 |
| C1 | 22 | 41.5 |
| C3 | 12 | 22.6 |
| Result (Sanders’ score) | ||
| Excellent | 19 | 35.8 |
| Good | 21 | 39.6 |
| Fair | 7 | 13.2 |
| Poor | 6 | 11.3 |
| Complications | ||
| Delayed union | 5 | 9.4 |
| Surgical site infections | 7 | 13.2 |
| Deep vein thrombosis | 3 | 5.7 |
| Knee stiffness | 2 | 3.8 |
Forty-one patients (77.4%) achieved good bone healing, with an average healing time of 5.6 months. The average knee flexion was 87.16 ± 20°, with a mean of 104.8°. Functional outcomes, assessed using Sanders’ Functional Evaluation Scale, were rated as excellent in 35.8% of cases, good in 39.6%, fair in 13.2%, and poor in 11.3% [Table 2].
Five patients (9.4%) experienced delayed bone healing and required bone grafting. Four of them had type C3 fractures, and one had a type A2 fracture [Figure 4]. Seven patients (13.2%) developed surgical site infections (four had Gustilo type IIIA, two had type II, and one had type I). Five of them improved with antibiotics, along with dressing changes, without the need for debridement or irrigation, while 2 required wound cleaning and debridement, but without removing the hardware. Antibiotics were given based on culture and sensitivity for 4 weeks. In addition, 3 patients developed DVT, and 2 had knee stiffness [Table 2].

- (a) Pre-operative radiograph shows intraarticular comminuted distal femur fracture. (b) Postoperative radiograph shows delayed fracture union. (c) Three months after bone graft with good bone healing.
DISCUSSION
In our study of 53 patients, 77.4% were males, which is consistent with other studies, such as Jambukeswaran et al. (66.7% males)[18] and Maley et al. (66.7% males).[19] Jambukeswaran et al. noted that the average age of their patients was between 36 and 45 years, highlighting that middle-aged individuals are more likely to experience open distal femur fractures,[18] which is somewhat similar to our findings where many patients were between 18 and 40. Kalande’s study, with 85.1% male participants and a mean age of 31 years, illustrates a younger demographic but also emphasizes male predominance, supporting the trend seen across multiple studies.[13]
Gustilo-Anderson classification revealed 54.7% type 1 fracture, 32.1% type 2, and 13.2% type 3A. In contrast, Maley et al. reported that Gustilo-Anderson type IIIB fractures were the most common.[18] Kalande’s study also indicated that a significant percentage (76.31%) of fractures were grade IIIA and above.[13]
Our findings indicated that 77.4% of patients achieved good bone union with an average healing time of 5.6 months. This aligns with Maley et al., who reported a similar mean time to bony union of 5.6 months.[19] In Jose’s and Krishnan’s study, the average time for union was 20.5 weeks.[20] In Mahajan et al.’s study, the union was seen around 5 months in 55% of the cases. The mean time for the radiological union was 15 weeks.[21]
In our study, the average knee flexion was 87.16 ± 20°, with a mean of 104.8°. Knee flexion can be influenced by factors such as the type of fracture, the method of fracture fixation, the healing process, and postoperative rehabilitation. In the study by Jose and Krishnan, knee flexion was <70° in 2 cases (10%), between 71° and 100° in 10 cases (50%), and over 100° in 8 cases (40%).[20] In Mahajan et al.’s study, the average knee flexion at 1.5 months follow-up was 75.75 ± 13.50°. This improved to 85.75 ± 12.28° at the 3-month follow-up, and by 6 months, the average flexion was 106.6 ± 15.80°.[21] In Gyanendra et al.’s study, the average flexion of the knee achieved by the participants was 103.5° (range is 60°–120°).[22] Our study evaluated functional outcomes using Sanders’ Functional Evaluation Scale. We found that 35.8% (19 patients) had excellent results, 39.6% (21 patients) had good results, 13.2% (7 patients) had fair results, and 11.3% (6 patients) had poor results. In the study by Jose and Krishnan, among 20 surgically treated patients, 5% had excellent outcomes, 65% had good outcomes, 25% had fair outcomes, and 5% had poor outcomes.[20] In Mahajan et al.’s study, 33% of cases (10 patients) achieved excellent scores, 52% (16 patients) had satisfactory scores, 11% (3 patients) had unsatisfactory scores, and only one patient had a poor score.[21] In Gyanendra et al.’s study, out of 30 patients, 16 had outstanding outcomes, 11 had good outcomes, two had acceptable outcomes, and one had a failed outcome.[22] In our study, 13.2% of patients developed surgical site infections, most of which (5 patients; 9.4%) were treated successfully with antibiotics and regular dressing changes and 2 patients (3.8%) were treated by debridement, antibiotics, and implant retention. In comparison, Maley et al. reported complications such as knee stiffness and deep infections in 10% of their cases.[19]
Study limitations
The study was conducted at a single hospital, so we cannot generalize the findings to other settings or patient populations. The sample size may not be large enough to draw definitive conclusions about rare complications or long-term outcomes. Most of the study patients were low-grade in the Gustilo-Anderson classification and had no type 3B and C. One of the study’s limitations is the lack of a control group with staged internal fixation of fractures.
CONCLUSION
This study illustrates that open distal femur fractures, types I through III-A, can be effectively treated through primary definitive internal fixation in conjunction with wound debridement and irrigation, yielding favorable outcomes in most cases.
Acknowledgment:
We sincerely thank our university and hospital administration for providing the facilities to complete this research.
Ethical approval:
The research was approved by the Research Ethics Committee of Amran General Hospital , reference number 3/2018, dated January 13, 2018.
Declaration of patient consent:
The author certifies that he has obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Conflicts of interest:
There are no conflicting relationships or activities.
Financial support and sponsorship: This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Reconstruction of traumatic, open supracondylar femoral fractures by autologous fibular strut grafting and cortico-cancellous bone grafting-a single-centre, observational study. J Orthop Trauma. 2018;32:75-81.
- [CrossRef] [PubMed] [Google Scholar]
- The epidemiology of fractures of the distal femur. Injury. 2000;31:C62-3.
- [CrossRef] [PubMed] [Google Scholar]
- Distal femur fractures In: Court-Brown CM, Heckman JD, McQueen MM, eds. Rockwood and Green's fractures in adults. Philadelphia, PA: Wolters Kluwer Health; 2015. p. :2230.
- [Google Scholar]
- The epidemiology of open long bone fractures. Injury. 1998;29:529-34.
- [CrossRef] [PubMed] [Google Scholar]
- Mortality after distal femur fractures in elderly patients. Clin Orthop Relat Res. 2011;469:1188-96.
- [CrossRef] [PubMed] [Google Scholar]
- Fracture and Dislocation Classification Compendium-2018. J Orthop Trauma. 2018;32:S1-S170.
- [CrossRef] [PubMed] [Google Scholar]
- The comprehensive classification of fractures of long bones Berlin: Springer-Verlag; 1990.
- [CrossRef] [Google Scholar]
- Handbook of fractures (3rd ed). Philadelphia: Lippincott Williams and Wilkins; 2006.
- [Google Scholar]
- External fixation of open femoral shaft fractures. J Trauma. 1995;38:648-52.
- [CrossRef] [PubMed] [Google Scholar]
- Fractures of the femoral shaft treated by external fixation with the Wagner device. J Bone Joint Surg Am. 1984;66:360-4.
- [CrossRef] [PubMed] [Google Scholar]
- A review of the management of open fractures of the tibia and femur. J Bone Joint Surg Br. 2006;88:281-9.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment outcomes of open femoral fractures at a county hospital in Nakuru, Kenya. East Afr Orthop J. 2018;12:52-7.
- [Google Scholar]
- Surgical treatment of displaced, comminuted fractures of the distal end of the femur. J Bone Joint Surg Am. 1982;64:871-9.
- [CrossRef] [PubMed] [Google Scholar]
- Distal femoral fractures: Current treatment, results and problems. Injury. 2001;32:SC3-13.
- [CrossRef] [PubMed] [Google Scholar]
- Open distal femur fractures treated with lateral locked implants: Union, secondary bone grafting, and predictive parameters. Orthopedics. 2012;35:e843-6.
- [CrossRef] [Google Scholar]
- Functional outcome of supracondylar femur fracture managed retrograde intramedullary nailing at a tertiary care centre. Nat Volatiles Essent Oils. 2021;8:1250-4.
- [Google Scholar]
- Functional outcome analysis of staged management of compound distal femur fracture. Int J Acad Med Pharm. 2023;5:283-86.
- [Google Scholar]
- Evaluation of results of open distal femur fractures with primary fixation and antibiotic impregnated collagen. Chin Med J. 2019;132:2564-9.
- [Google Scholar]
- Study of functional outcome of distal femur fractures treated by open reduction and internal fixation with locking compression plate. J Evol Med Dent Sci. 2016;5:1984-91.
- [CrossRef] [Google Scholar]
- Assessment of functional outcome of distal femur intra-articular fractures treated with locking compression plate. Int J Res Orthop. 2020;6:145-50.
- [CrossRef] [Google Scholar]
- Outcome of supracondylar femur fracture in adults managed by distal femur locking compression plate. Biomed J Sci Tech Res. 2018;3:1-7.
- [CrossRef] [Google Scholar]






