Translate this page into:
Educating the educators: Perspectives on surgical education
Corresponding Author:
Mohamed Khalid
Department of Orthopedics, College of Medicine, Taibah University, Universities Road, Almadinah Almunawwarah 41477
Kingdom of Saudi Arabia
movingbones1@gmail.com
| How to cite this article: Khalid M. Educating the educators: Perspectives on surgical education. J Musculoskelet Surg Res 2018;2:4-7 |
Abstract
These are challenging times for Surgical Educators. Limitations on working hours, resource constraints, rapidly evolving technological advances in the way, we communicate and interact, and increasing patient expectations are threatening the traditional and time-tested apprenticeship model of surgical training. It is imperative on the part of today's Surgical Educators to respond to these challenges in ways that enhance and promote the training of future surgeons. This has led to the birth of a new specialty of Surgical Education. Although generic Health Sciences/Medical Education programs are widely available and do serve a useful purpose, it may be argued that surgical trainees have unique needs that may not be adequately addressed by the generic programs. Thus, there is a need for focused Surgical Education programs. This review aims to identify these needs and to discuss the current Surgical Education programs available. It also aims to suggest additional issues that may need to be addressed to make these programs even more useful.“The goal of education is to enable individuals to continue their education.” ― John Dewey
Introduction
Surgical Education is undergoing a very significant change, and the editorial in this issue [1] succinctly highlights the reasons for the same and the direction in which the winds of change are blowing. The cornerstone of successful implementation of these changes is the education of surgical educators. This article will highlight the evolving role of surgical education as a subspecialty in its own right with a note on its relevance to the specialty of orthopedic surgery.
Historical Perspective
Apprenticeship is the natural and universal method of learning skills. We learnt basic skills of life such as eating, walking, and talking by observing and mimicking others. By a process of trial and error, in a supportive environment, we were initiated into the world of learning. This, we would learn later, was apprenticeship. Like other skills, surgery has traditionally been learnt by the apprentice mimicking the master surgeon or the mentor. The essential ingredients for the success of this traditional and time-tested model of learning were ample time (usually several years) and serendipity brewed in the crucible of a conducive environment that would define this special mentor-protégé relationship. As the wheel of time has moved on, this traditional relationship has come under a severe strain and is now more of a utopian dream than reality. This changing landscape presents surgical educators with challenges as well as opportunities. The challenges have been aptly described,[1] the opportunity needs elaboration. As the famous saying goes “Necessity is the mother of invention.” The necessity to adapt to the changing landscape in surgical education is providing a powerful impetus to look around and borrow well-established concepts from the field of education and training. Some notable examples are experiential education,[2] reflection-in-action and reflection-on-action,[3] situated learning [4] to name a few. It has also led to the adaptation of some relevant aspects of successful educational models from other walks of life such as the cognitive apprenticeship (CA) model,[5] which was originally developed to teach languages and mathematics. A brief description of these theories and the elements of CA are as follows.
According to Dewey,[2] who is widely regarded as the greatest educational philosopher of modern times, the only useful and long-lasting knowledge is the one derived from experience or in other words, experiential knowledge. However, he clarifies that “all experiences are not genuinely or equally educative.” The educative value is determined by the “Quality of the experience.” “Quality is defined by the palatability and the ability to promote future desirable experiences.” Palatability is the ability to derive the subject matter “within the scope of ordinary life experience” at the outset. This is then built up by the process of interaction with the external conditions. The role of the mentor is to steer the learner in the direction of positive growth and in shaping the external factors to facilitate this.
Schön [3] in his book, the Reflective Practitioner, the most quoted book on professional expertise in recent years,[6] built on Dewey's ideas and emphasized the importance of reflection. More importantly, he challenged the dominance of and highlighted the limitations of the epistemology of technical rationality. According to Schön “practice of a skill is characterized by uncertainty, uniqueness, instability, and value conflict and practitioners bound by a positivist epistemology find themselves caught in a dilemma. Their definition of rigorous professional knowledge excludes phenomena that they have come to see as central to their practice.” Sir William Osler, the father of modern medicine, alluded to this when he wrote “Medicine is a science of uncertainty and an art of probability.”[7]
Lave and Wenger [4] developed their theory of situated learning based on Vygotsky's concept [8] that “all learning is social.” They stated that learning is situated (e.g., in the operating theatre for surgeons) and that knowledge is intimately connected to participation in activities (such as assisting/performing an operation).
The model of Enhanced apprenticeship was developed by Collins et al.[5] It is a model based on situated learning through guided experience. It consists of three stages core, intermediate, and advanced as summarized in [Table - 1].
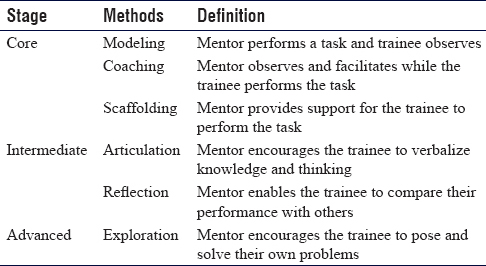
The core elements of modeling, coaching, and scaffolding are well known and practiced in a traditional apprenticeship. Articulation, on the other hand, needs to be examined more closely. Conventionally, a lot of emphases is placed on the ability of a trainee to articulate or verbalize the steps of a procedure. Indeed, whether a trainee gets to do a procedure often depends on his/her ability to describe the steps in advance. In his book, the Reflective Practitioner Schön [3] writes that “we learn to execute such complex performances as crawling, walking, juggling, or riding a bicycle without being able to give a verbal description even roughly adequate to our actual performance. Indeed, if we are asked to say how we do such things, we tend to give wrong answers, which if we were to act according to them would get us into trouble.” Reflection, on the other hand, is an under-utilized albeit vital element. As Confucius said, “Learning without reflection is a waste, Reflection without leaning is dangerous.” The advanced stage of exploration is reserved for the rare occasion when the trainee is of exceptional talent/skill. Here, the mentor may use his own experience to enable the trainee to go beyond what he himself may have gone. This obviously is rare and is mainly seen in a mentor/protégé type of relationship.
The traditional master surgeon seldom had or felt the need to have any formal training in educational methods. On the other hand, time and resource constraints, increasing complexity of surgical procedures propelled by technological advances, and rising patient expectations, partly due to improved access to information have created unique challenges to the contemporary surgical educator. He/She is forced to adapt and seek smarter ways of training the future of generations of surgical trainees. Thus, there is a compelling need for formal training in surgical education.
Generic Health Sciences/Medical Education or Surgical Education?
While surgical education shares several common attributes with generic health sciences education or medical education, the context and emphasis are different. [Table - 2] lists the major differences between surgical Education and generic Health Sciences Education.
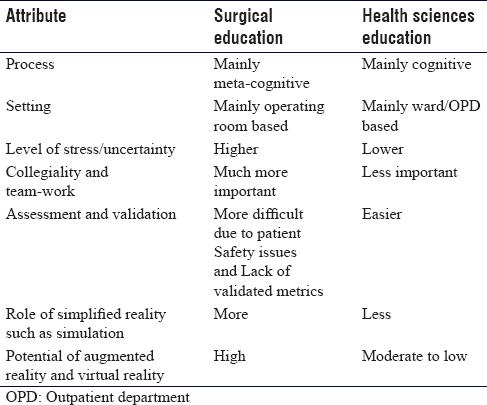
While rooted in the cognitive domain, skills acquisition is largely a metacognitive phenomenon. While cognitive skills involve content-knowledge acquisition and retention, learning of surgical skills involves the mind's ability to reflect on how effectively it is handling the learning process as it is doing so. This is reflected in the Fitts and Posner [9] model of skills acquisition in which the first stage is the cognitive stage where the trainee intellectualizes the process and becomes familiar with the tools, the second stage is the associative stage in which he/she develops appropriate motor behavior, and finally, the autonomous stage where repeated practice leads to expert performance. Surgical trainees are often required to learn skills while under considerable stress. It can be emotional or cognitive or physical stress or a combination thereof. The correlation between stress and performance is so ubiquitous that it has come to be accepted as a law in psychology – the Yerkes-Dodson (Y-D) law.[10] The law takes the form of an inverted U-shaped relationship between performance and stress. Performance on any task is Optimal at moderate level of stress, falling off as stress becomes too low or too high.
Postgraduate Programs in Surgical Education
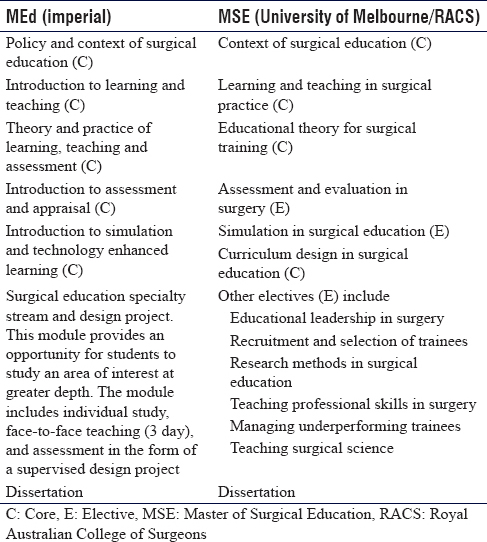
Currently, there are two Universities offering training in Surgical Education. The Master in Education (MEd) offered by Imperial College, London, and the Master of Surgical Education (MSE) offered by the University of Melbourne and co-badged with the Royal Australian College of Surgeons RACS).
The MEd qualification consists of eight modules (Modules 1–8), completed in full or part-time study mode. Full-time study mode is demanding and only suitable for students taking a year away from full-time employment (e.g., overseas students). The PG Diploma consists of modules 1–7, is available in part-time study mode only and is delivered over a 10-month period.
The program comprises five core modules each consisting of 1-week intensive contact teaching time with further private study required to complete module preparation, coursework, and assessment.
The MSE program is designed to be completed over 3 years and consists of eight modules. Most candidates take 1–2 modules per se mester depending on work, family, and other personal commitments. Each module consists of 12.5 credit points. The master level is 150 points. It is usually possible to complete 50 credit points per year. Perhaps the sentinel part of the course is a workshop (1 day/subject) conducted at RACS, Melbourne. Usually, this has preparatory assignments. The workshop focuses on important aspects of the subject and consists of interactive lectures and activity sessions. The activity sessions intrigued me when I first experienced them. They were carefully designed to provide a unique learning opportunity. Later, I understood the way they worked when I read John Dewey's book “Education and Experience” in which he wrote, “Give the pupils something to do, not something to learn; and the doing is of such a nature as to demand thinking; learning naturally results.” During the semester, the candidates are expected to read key articles that shed light on the various aspects of the subject and write an essay (sometimes two) to demonstrate the understanding of the subject. The topics could be selected from a list that is provided during the workshop or a new topic could be chosen with the approval of the faculty. All assignments are designed to draw on or have application to the surgical education practices of each student. Some of the essays involve reflective writing. I found this type of writing a very useful learning tool. As John Dewey wrote, “We do not learn from experience. We learn from reflecting on experience.” There is a webinar as well during which the Program Director and a group of 4–6 students log in, and each students presents a topic (chosen from a list or new as in case of the essay). Others in the group ask questions, the student is assessed based on their performance.
Both programs have similarities as shown in [Table - 3].
Perceived Gaps and Suggestions for Improvement
While both the programs are very popular and appropriate, there are certain aspects that might need consideration. These can be summarized as follows:
- Considering that surgical learning often takes place under stressful conditions, and it is now widely accepted that while a certain level of stress improves Performance, excessive stress can hamper skills acquisition, more emphasis should be placed on learning about stress and strategies to handle it. Perhaps, this should be taught as a core subject
- Considering that most of the surgical learning takes place in the OR, a dedicated module on OR teaching may be useful
- With recent advances in augmented reality (AR) and virtual reality (VR) technology, it is quite likely that these will be increasingly used in surgical education. Perhaps, an elective on AR and VR would be useful.
Relevance of Surgical Education Courses to Orthopedic Surgeons
Orthopedic surgery has expanded enormously in recent years. Compared to their peers from other specialties, orthopedic surgical trainees often face unique challenges, for example, the range of surgical procedures that they need to learn is far more than in many other branches of surgery. Technological advances take place at a much faster rate in orthopedics compared to many other surgical fields. Technical errors are much easier to detect and therefore, the need to accurately perform the operation is much more compared to some other surgical specialties. In the context of orthopedic training in Saudi Arabia, it has been mentioned that “in many centers, the true needs of the trainees are not met and the teaching strategies used do not result in the intended outcome.[11] It is, therefore, imperative that effective surgical education techniques should be learnt and practiced by those involved in training the residents. There is a need for more programs offering training in surgical education.
In conclusion, it is important to consider these developments in the context of the current trend to formalizing the education and supervisory expertise of surgeons. The Royal College of Surgeons of Edinburgh has defined competencies for surgical trainees and has a Faculty of Surgical Trainers.[12] RACS has also introduced an Academy of Surgical Educators.[13] The move toward improving the way we educate future surgeons by learning relevant aspects of the educational theory and practice is a positive development. Being able to train future generations of surgeons is indeed a privilege and with it should come responsibility. Improving our ability to teach should be a part of this new paradigm. As the old Chinese proverb says, “A teacher affects eternity – one can never know when his influence stops….”
Acknowledgements
The author wishes to acknowledge the help and guidance received in the preparation of this manuscript from Professor Debra Nestel, Professor of Surgical Education, University of Melbourne, Australia and Professor Khalid I. Khoshhal, Professor of Pediatric Orthopedic Surgery, Taibah University, Almadinah Almunawwarah, KSA.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors contributions
MK testifies that criteria for authorship are fully met and that the article has been checked for plagiarism. MK conceived, designed, and wrote the initial and final draft. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Guraya SY. The changing landscape of surgical education and training. J Musculoskelet Surg Res 2018;2:1-3. [Google Scholar] |
| 2. | Dewey J. Experience and education. Indianapolis, USA: Kappa Delta Pi; 1997. [Google Scholar] |
| 3. | Schön DA. Educating the Reflective Practitioner: Toward a New Design for Teaching and Learning in the Professions. San Francisco: Jossey-Bass Publishers; 1987. [Google Scholar] |
| 4. | Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. Cambridge, UK: Cambridge University Press; 1991. [Google Scholar] |
| 5. | Collins A, Brown JS, Newman SE. Cognitive apprenticeship: Teaching the crafts of reading, writing, and mathematics. Knowing, Learning, and Instruction: Essays in Honor of Robert Glaser. Vol. 18. Hillsdale, New Jersey; Lawrence Erlbaum associates; 1989. p. 32-42. [Google Scholar] |
| 6. | Gilroy P. Reflections on Schön: An epistemological critique and a practical alternative. J Educ Teach 1993;19:125-42. [Google Scholar] |
| 7. | Bean WB. Sir William Osler: Aphorisms from his Bedside Teachings and Writings. Henry Schumann, Inc. New York; 1954. [Google Scholar] |
| 8. | Vygotsky LS, Hanfmann E, Vakar G. Thought and Language. Cambridge, Massachusetts, USA: MIT Press; 2012. [Google Scholar] |
| 9. | Fitts PM, Posner MI. Human Performance. Belmont, CA: Brooks/Cole; 1967. [Google Scholar] |
| 10. | Yerkes RM, Dodson JD. The relation of strength of stimulus to rapidity of habit-information. J Comp Neurol Psychol 1908;18:459-82. [Google Scholar] |
| 11. | Taha WS. The changing landscape of surgical education and training. J Taibah Univ Med Sci 2015;10:109-15. [Google Scholar] |
| 12. | Available from: https://www.rcsed.ac.uk/faculties/faculty-of-surgical-trainers. [Last accessed 2018 Jan 29]. [Google Scholar] |
| 13. | Available from: https://www.surgeons.org/for-health-professionals/academy-ofsurgical-educators/. [Last accessed 2018 Jan 29]. [Google Scholar] |
Fulltext Views
2,902
PDF downloads
766





