Translate this page into:
Effect of aquatic resistance, balance, and proprioception training on lower limb muscle performance in bilateral knee osteoarthritis
*Corresponding author: Sandeep Shinde, Department of Musculoskeletal Sciences, Krishna Vishwa Vidyapeeth, Karad, Maharashtra, India. drsandeepshinde24@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jain P, Shinde S. Effect of aquatic resistance, balance, and proprioception training on lower limb muscle performance in bilateral knee osteoarthritis. J Musculoskelet Surg Res. 2025;9:104-11. doi: 10.25259/JMSR_230_2024
Abstract
Objectives:
Knee osteoarthritis (KOA) leads to persistent pain, joint stiffness, and muscle weakness, significantly limiting physical activity. Treatment options include surgical interventions, non-invasive alternatives, and exercise-based therapies. Land-based training (LBE) strengthens muscles, reduces pain, and improves function. In contrast, aquatic exercise (AQE) offers comfort. The study aimed to investigate the impact of aquatic resistance, balance, and proprioception training on lower limb muscle performance in bilateral KOA patients.
Methods:
This randomized clinical trial included 290 participants assigned to Groups A (Control group) and B (Interventional group), with 145 participants in each group. Over eight weeks, participants engaged in both LBE and AQE. Visual analog scale (VAS), 1 repetition maximum (RM) leg press test, proprioception, timed up-and-go (TUG) test, 40-m fast-paced walk test (40 mFPWT), and Western Ontario and McMaster Universities Arthritis Index (WOMAC) were utilized to evaluate the results.
Results:
The results revealed highly significant improvements in both groups’ VAS and WOMAC scores (P = 0.0001). However, when compared to Group A, Group B demonstrated significantly better outcomes in the 1RM leg press test, proprioception, TUG test, and the 40 mFPWT (P = 0.0001).
Conclusion:
The study found that an eight-week aquatic training program helped alleviate pain and improved lower limb muscle performance in bilateral KOA patients.
Keywords
Aquatic training
Balance
Muscle function
Osteoarthritis
Proprioception
INTRODUCTION
Osteoarthritis (OA) is a common joint condition worldwide, especially among the geriatric population, and it is a major health concern in several societies. Furthermore, the financial cost of treating this disorder has been projected to be in the hundreds of billions of dollars, with governments having to deal with its serious side effects.[1] Approximately 250 million people globally are affected by OA. Knee OA (KOA) is the most prevalent type of degenerative joint condition, impacts both males and females and becomes more widespread with their ages.[2] KOA is a degenerative and progressive chronic disorder that accounts for 83% of all OA cases worldwide, with an incidence of 22–39% in India. The condition is distinguished by gradual cartilage deterioration and bone remodeling.[3]
Interestingly, recent studies suggest that proprioceptive deficits – problems with sensing joint position and movement may play a significant role in the onset and progression of KOA.[4] As KOA advances, proprioceptive function may decline further.[5] Diminished proprioception may contribute to an increased risk of falling in the KOA population. Pain in KOA affects proprioception and muscle strength.[6] Furthermore, given the importance of proprioception, targeted exercises are recommended for KOA patients. Proprioceptive training aims to improve joint awareness, balance, and dynamic stability. Engaging in proprioceptive exercises can enhance proprioceptive acuity, reduce discomfort, and improve mobility in individuals with OA.[5]
It appears that the quality and speed of walking will be negatively impacted in OA patients, who will have difficulty rising from their seats and climbing stairs. Several treatments are recommended for the therapy of individuals with KOA in an attempt to lessen the consequences. Surgical techniques, including arthroscopy, osteotomy, and joint replacements, are among them. In addition, there are non-surgical options, including using orthotic devices and lifestyle modifications, such as exercise-based interventions. Land-based training (LBE) is a highly recommended non-pharmacologic strategy for KOA.[7] Furthermore, a review published by Cochran noticed that LBE can provide temporary pain relief and enhance the quality of life for individuals with KOA for several months after treatment. While exercise is beneficial, excessive strain can worsen arthritis symptoms. According to statistical analysis, individuals with OA were over 50% less likely to be willing to engage in further exercise due to pain, and they also showed a decreased degree of exercise than the rest of the population. Regardless of whether they enroll in a regular exercise course, sustained commitment to exercise can be challenging. As a result, it is essential to investigate different treatment approaches for individuals with KOA.[7]
An effective substitute for the rehabilitation of KOA appears to be aquatic exercise (AQE). Physical characteristics like hydrostatic pressure of water help reduce muscle fatigue and spasms. It also enhances blood circulation, promoting overall relaxation. Water resistance provides a unique form of resistance training. Muscles must work against the water’s resistance, leading to improved strength and endurance. The buoyant nature of water supports body weight, reducing strain on bones, muscles, and joints. Patients can engage in weight-bearing activities without significant pain.[7] In addition, AQE offers a more pleasant and appropriate setting for participants with KOA who are hesitant to be physically active. As a result, AQE may help reduce pain associated with KOA. Engaging in AQE can positively impact overall well-being.[8] While AQE has advantages over LBE, determining which is better remains uncertain. Research studies have compared the efficacy of AQE and LBE, but the combined effects of strength, balance, and proprioception training are limited. Hence, this research intended to determine the “Effect of aquatic resistance, balance, and proprioception training on lower limb muscle performance in bilateral KOA patients.”
MATERIALS AND METHODS
Study design
The present study was a randomized clinical trial with a pre/post-test experimental design.
Sample size
The associated study involved a sample size of 304 participants {n = ([Za+ Zb]2 × [s12+s22]/[m2–m1]2)} [Figure 1].
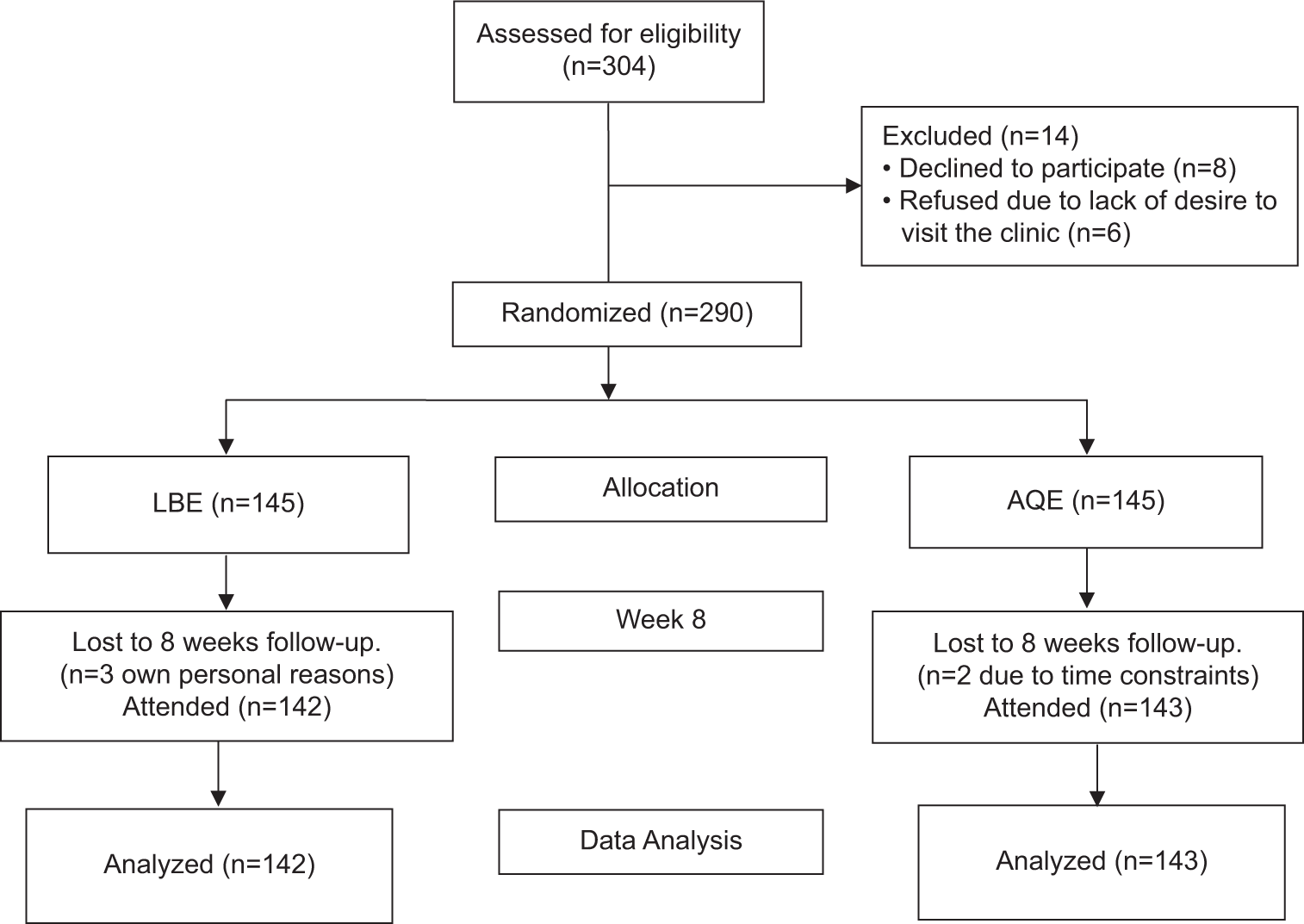
- Participants flow diagram. AQE: Aquatic exercise, LBE: Land-based exercise.
Study participants and sampling
Participants with KOA, aged between 45 and 65, were included with a body mass index (BMI) not exceeding 35 kg/m2. These participants had no valgus or varus deformities, limb length discrepancies, or underlying health issues hindering full participation in daily activities. In addition, they scored <7 on the visual analog scale (VAS) for activity. Exclusion criteria comprised individuals with open wounds, skin problems, recent fractures within the past six months, serious neurological conditions, uncontrolled severe hypertension, active cancer, severe asthma, visual impairments, recent intra-articular steroid injections, or fear of water.
A total of 290 participants were randomly assigned to two groups using a computer-generated random number generator. Each participant received a sealed envelope containing a group identification number (1 = land-based, 2 = hydrotherapy). The patient opened the sealed envelope when they were included in the study. The group assignment was concealed from the assessors who measured the patient’s variables. The duration of the study was one year in the physiotherapy outpatient department. The study design and reporting adhered to the CONSORT guidelines.
Procedure
Demographic data for the participants was collected, and the study’s objective was explained to them. In the pretest evaluation, primary measures like VAS, one-repetition maximum (1RM) leg press test, timed up-and-go (TUG) test, and Western Ontario and McMaster Universities Arthritis Index (WOMAC) scale whereas secondary measures such as 40-m fast-paced walk test (40 mFPWT) and proprioception assessment were utilized. Before treatment, all groups received interferential therapy, hot moist pack therapy, and ultrasonic therapy. Group A underwent LBE, while Group B received AQE.
Intervention programs
LBE program
Resistance, balance, and proprioception exercises were given in a gymnasium near the aquatic area where the AQE program was administered [Table 1].
| Type of exercises | Land exercises | Distance/repetitions/hold×Sets (week: 1→8)* | Aquatic exercises | Repetitions/Hold×Sets (week: 1→8)* |
|---|---|---|---|---|
| A. Warm-up (10 min) |
Cycling on a stationary bike | 5 min | Aquatic running with a belt | 8 m×2 → 16×3 m |
| Walking forward, backwards, and sidewalk | 15–75 steps×3 sets | Walking forward, backwards, and sidewalk with kickboard | 16 m×2 → 16×5 m | |
| B. Strength training (10 min) | 1. Hip flexion-extension | 10×3 → 10×7 m (Use of theraband-low, medium resistance) | Hip flexion-extension | 8 rpm×2 → 10×3 (Use of aquatic cuffs from week 4) |
| 2. Hip hyperextension | 10×3 → 10×7 m | Hip hyperextension | 8 rpm×2 → 10×3 | |
| 3. Hip abduction-adduction | 10×3 → 10×7 m | Hip abduction-adduction | 8 rpm×2 → 10×3 | |
| 4. Knee flexion-extension in sitting and standing | 10×3 → 10×7 m | Knee flexion-extension in sitting and standing | 8 rpm×2 → 10×3 | |
| 5. Kickback | 10×3 → 10×7 m | Kickback | 8 rpm×2 → 10×3 | |
| C. Balance and Proprioception training | 1. Marching on the spot | 15–75 steps×3 sets | Marching on the spot | 1→2 min |
| 2. Knee to chest | 8 rpm×2 → 10×3 | Knee to chest | 8rpm×2 → 10×3 | |
| 3. Cross-country skiing | 8 rpm×2 → 10×3 | Cross-country skiing | 8rpm×2 → 10×3 | |
| 4. Walking on the tip toes | 15–75 steps×3 sets | Walking on the tip toes | 1 min→2 min | |
| 5. Semi-Squats, lunges | 6 rpm×3 → 10×3 | Semi-Squats, lunges | 6 rpm×3 → 10×3 | |
| 6. Step up, down, forward and backward | 15–75 steps×3 sets | Step up, down, forward and backward | 8 rpm×2 → 25×2 | |
| 7. Multiple changes in direction drill (forward, backwards, sideways | 15–75 steps×3 sets (Progress to eyes closed at week 4) | Walking forward & backward holding aqua dumbbells | 16 m×2 → 16×5 m (Progress to eyes closed from week 4) | |
| 8. Walking in a figure of 8 holding wand and then without wand |
15–75 steps×3 sets | Walking in a figure of 8 holding noodle and then without noodle | 16 m×2 → 16×5 m | |
| 9. Single leg stance by holding wand and then without wand | 10–20 s×3 | Single leg stance holding noodle and then without noodle | 10–20 s×3 | |
| 10. Double leg stance on hard surface | 10–20 s×3 | Double leg stance on kickboard | 10–20 s×3 | |
| 11. Single leg stance on hard surface | 10–20 s×3 | Single leg stance on kickboard | 10–20 s×3 | |
| 12. Single leg stance with leg swing on hard surface | 10–20 s×3 | Single leg stance with leg swing on noodle | 10–20 s×3 | |
| 13. Single leg stance on hard surface and throwing the ball. | 10–20 s×3 | Single leg stance on noodle and throwing the ball. | 10–20 s×3 | |
| 4. Cool down (10 min) |
1. Lying on the floor | 4–5 min | Supported cycling against wall | 4–5 min |
| 2. Stretches-Quadriceps, hamstrings, gastroc-soleus, pectoralis major, triceps, trunk lateral flexion | 30 s per leg×3 | Stretches-Quadricep, hamstrings, gastroc-soleus, pectoralis major, triceps, trunk lateral flexion | 30 s per leg×3 |
AQE program
The AQE sessions took place in the hydrotherapy pool at the Hospital’s Outpatient Physiotherapy Department. This program consisted of three weekly sessions over eight weeks, totaling 24 sessions, each lasting 40–50 min. The pool temperature was maintained at 36°C, and the water level typically reached the median sternum line. A licensed physiotherapist monitored the water workout regimen in the pool, prioritizing participant safety over accuracy during the training sessions. The same exercise protocol was given in water as given for Group A [Table 1].[9-12]
Outcome measurements
The VAS was used to assess pain levels in subjects, both at rest and during activity.[3] The TUG test was employed to measure dynamic balance, in which individuals were instructed to sit on a chair with a seat level of 46 cm. They are, then, asked to stand up, proceed to a designated spot where a 3 m cone is placed, walk back, turn around, and return to their chair.[10] Lower body strength was evaluated using the 1RM leg press test.[13] WOMAC is a specific self-assessment tool comprising 24 items categorized into three domains: Pain, function, and stiffness. On a scale based on Likert, the WOMAC value runs between zero and four. A greater value suggests severe pain, joint stiffness, and impaired functioning.[3]
Walking speed was assessed using the 40 mFPWT, in which participants were asked to walk along a 10-m pathway with a cone marking its end. This exercise is repeated until a 40-m walkway is covered in one continuous walk without any running.[14] In addition, the difference in joint position sense errors between pre- and post-intervention was measured by positioning the patient with their knees and hips bent at 90° on the edge of a couch. A Goniometer was used and 45° of flexion at the knee served as the reference. The patient was asked to maintain that position for 10–15 s while the therapist gently moved their leg to the reference locations. The patient was instructed to actively return their leg to the same angle.[15]
Statistical analysis
The data were entered into an Excel spreadsheet and analyzed using the Statistical Package for the Social Sciences Version 26.0. The following techniques were employed: unpaired t-tests to assess differences between groups and paired t-tests to identify variations within each group. The intent-to-treat (ITT) analysis included participants who dropped out during treatment sessions. To handle missing data, the final measurement carried forward approach was used to assess outcome measurements for the ITT population. For each variable, a significance threshold of P < 0.05 was applied.
RESULTS
In the study, 304 individuals were initially evaluated for eligibility. Of these, 290 met the requirements [Figure 1]. It is shown in Table 2 that out of 290 participants, only 12.41% and 11.03% were men, whereas 89.43% and 90.20% were female in Groups A and B, respectively. The average age for Group A was 51.63 ± 9.47, and for Group B, it was 50.86 ± 8.20. The average BMI for Group A was 27.02 ± 3.506, whereas 26.13 ± 3.799 for Group B. In accordance with the Kellgren-Lawrence grade, 52.41% of individuals in Group A had grade I, compared to 53.10% in Group B, and 48.59% had grade II, compared to 46.89% in Group B.
| Variables | Group A (n=145) | Group B (n=145) | P-value |
|---|---|---|---|
| Age (years) | 55.41±10.272 | 54.32±11.35 | 0.3977 |
| Sex, n(%) | |||
| Male | 18 (12.41) | 16 (11.03) | |
| Female | 127 (89.43) | 129 (90.20) | |
| BMI (kg/m2) | 27.02±3.506 | 26.13±3.799 | 0.0428 |
| Kellgren-Lawrence Scale, n(%) | |||
| Grade I | 76 (52.41) | 77 (53.10) | 0.9068 |
| Grade II | 69 (48.59) | 68 (46.89) | |
BMI: Body mass index
The difference in the mean VAS values observed at rest and during exercise in individuals with bilateral KOA is described in Table 3. Group B experienced lower pain levels in both. Specifically, the mean difference in the right knee changed from 3.78 ± 1.022 to 1.55 ± 0.53 and from 6.34 ± 1.36 to 2.58 ± 1.002. Similarly, in the left knee, the mean difference shifted from 3.67 ± 1.29 to 1.76 ± 0.58 and from 7 ± 1.50 to 2.46 ± 1.080, which indicated statistical significance with a P-value <0.0001.
| VAS | Pre-test | Post-test | P-value | t-value |
|---|---|---|---|---|
| Right knee | ||||
| At rest | ||||
| Group A | 3.51±1.17 | 2.14±0.967 | <0.0001 | 11.034 |
| Group B | 3.78±1.022 | 1.55±0.53 | <0.0001 | 28.137 |
| Inference | 0.0396 | <0.0001 | ||
| On activity | ||||
| Group A | 6.07±0.51 | 2.51±0.97 | <0.0001 | 39.409 |
| Group B | 6.16±0.55 | 2.19±0.92 | <0.0001 | 40.273 |
| Inference | 0.1538 | 0.0049 | ||
| Left knee | ||||
| At rest | ||||
| Group A | 3.90±1.12 | 2.36±1.04 | <0.0001 | 12.351 |
| Group B | 3.67±1.29 | 1.76±0.58 | <0.0001 | 18.856 |
| Inference | 0.1112 | <0.0001 | ||
| On activity | ||||
| Group A | 6.31±0.59 | 2.71±1.19 | <0.0001 | 32.403 |
| Group B | 6.22±0.48 | 2.27±1.001 | <0.0001 | 40.991 |
| Inference | 0.1492 | 0.0009 | ||
The mean values of the 1RM leg press test for patients with bilateral KOA within the groups that were conducted are compared in Table 4. p-value indicated statistical significance, showing <0.0001 for Group B. In addition, the comparison between the groups also demonstrated a significant difference, with P < 0.0001. The average proprioception values among patients with bilateral KOA are analyzed in Table 4. The results indicated that in Group B, both the right and left knees showed P < 0.0001. However, in Group A, P-values were 0.0257 and 0.0281 for the right and left knees. Furthermore, the post-test average values across the groups for proprioception demonstrated significant differences, with P < 0.0001 both for the right and left knees.
| Pre-test | Post-test | P-value | t-value | |
|---|---|---|---|---|
| 1 RM leg press test | ||||
| Group A | 58.34±10.614 | 59.04±9.301 | 0.0230 | 2.298 |
| Group B | 57.79±9.031 | 66.39±11.23 | <0.0001 | 35.626 |
| Inference | 0.6391 | <0.0001 | ||
| Proprioception | ||||
| Right Knee | ||||
| Group A | 13.11±2.61 | 12.48±1.54 | 0.0257 | 2.255 |
| Group B | 12.73±2.18 | 10.09±1.37 | <0.0001 | 19.152 |
| Inference | 0.1856 | <0.0001 | ||
| Left Knee | ||||
| Group A | 12.92±2.50 | 12.61±1.44 | 0.0231 | 2.219 |
| Group B | 13.14±2.22 | 10.48±1.12 | <0.0001 | 17.224 |
| Inference | 0.4390 | <0.0001 | ||
1 RM: 1 Repetition maximum
The mean results of the TUG, 40 mFPWT, and WOMAC scale for participants having bilateral KOA within the groups conducted are compared in Table 5. P-value of TUG indicated statistical significance, showing <0.0001 for Group B. In addition, the comparison between the groups also demonstrated a significant difference, with P < 0.0001. Furthermore, for 40 mFPWT, Group B, the duration decreased significantly, with a mean difference shifting from 31.19 ± 4.21 to 27.06 ± 2.573, which indicated statistical significance with a P-value <0.0001. The analysis of the average WOMAC scale results for subjects with bilateral KOA, among and across both groups, was obtained to be statistically significant (P < 0.0001).
| Pre-test | Post-test | P-value | t-value | |
|---|---|---|---|---|
| TUG test in seconds | ||||
| Group A | 12.48±2.54 | 11.76±2.50 | 0.0163 | 2.431 |
| Group B | 12.65±2.72 | 10.01±2.57 | <0.0001 | 10.789 |
| Inference | 0.5834 | <0.0001 | ||
| 40 mFPWT | ||||
| Group A | 30.97±4.18 | 29.90±2.67 | 0.0178 | 2.397 |
| Group B | 31.19±4.21 | 27.06±2.573 | <0.0001 | 8.088 |
| Inference | 0.6528 | <0.0001 | ||
| WOMAC | ||||
| Group A | 58.50±8.40 | 53.79±7.45 | <0.0001 | 5.056 |
| Group B | 60.37±7.22 | 49.42±6.52 | <0.0001 | 13.399 |
| Inference | 0.0456 | <0.0001 | ||
TUG: Timed up-and-go, 40mFPWT: 40-m fast paced walk test, WOMAC: Western Ontario and Mcmaster universities arthritis index
DISCUSSION
The current research demonstrated that AQE indeed plays a crucial role in enhancing lower limb performance and managing pain in individuals with KOA. Fisken et al. compared AQE to patient education in KOA patients. After 12 weeks of aquarobic therapy, participants experienced a significantly greater decrease in pain than those who received patient education. This highlights the effectiveness of AQE in managing pain and improving overall well-being. In addition, the systematic review explored various interventions for OA patients, including water-based exercises, aerobics, and strength training. These interventions collectively demonstrated effective pain reduction, emphasizing the importance of tailored exercise programs for OA management.[16] In the present study, the experimental group experienced reductions in VAS scores at rest: 1.55 for the right knee and 1.76 for the left knee. In comparison, the control group had greater reductions: 2.14 for the right knee and 2.36 for the left knee. The statistical significance (P < 0.0001) indicates that these differences are unlikely due to chance. Both the control and experimental groups showed significant reductions in VAS scores during activity. P < 0.0001 emphasizes the extreme significance of these changes. Water immersion induces circulatory changes and hydrostatic force. These factors compress tissues, reduce edema, and enhance joint mobility. Consequently, pain is alleviated by lowering joint and soft-tissue stiffness.[17]
Hinman et al. highlighted that gradual training during hydrotherapy can enhance leg muscle strength.[17] Zamanian et al. investigated how water-based training affected fall risk and quadriceps strength in women with chronic KOA.[18]
Both intervention groups significantly improved in outcomes. However, the experimental group demonstrated remarkable gains in quadriceps strength.[18] In the present study, the control group exhibited a statistically significant improvement in the mean 1 RM leg press test (0.64 kg, P = 0.0230). Remarkably, the experimental group achieved even greater gains, with a mean improvement of 8.6 kg (P < 0.0001). Notably, both groups experienced improved lower body strength.
Kirthika et al. demonstrated that combining proprioceptive exercises with traditional physiotherapy is more effective than physiotherapy alone for individuals with KOA.[19] Hajouj et al. investigated the impact of innovative aquatic proprioceptive training in male athletes after anterior cruciate ligament reconstruction and showed significant improvements in joint position sense errors.[11] In the present investigation, the control group exhibited minor reductions in proprioception deficits (mean values of 0.0257 and 0.0231) for both right and left knees. Remarkably, the interventional group demonstrated substantial improvements in proprioception efficiency, as evidenced by reduced deficits in average proprioception (2.64 and 2.66) of the right and left knee with P < 0.0001.
Taglietti et al. compared AQE alone with patient education during an eight-week intervention. They showed statistically significant differences in TUG scores between the orientation and the aquatic training groups.[12] In the current research, the interventional group demonstrated a significant improvement in mean TUG values (reduction of 2.64 s, P < 0.0001). Interestingly, even the conventional group showed improvement, with an average TUG value increase of 0.72 s (P = 0.0163).
Hinman et al. investigated the effects of water workouts in individuals with hip and KOA. After treatment, the exercise group showed lower WOMAC discomfort, stiffness, and improved physical performance.[17] Another study evaluated AQE in older adults with lower extremity OA. WOMAC discomfort levels decreased, and physical function improved significantly with AQE.[20] In the current research, the experimental group demonstrated substantial improvements in WOMAC scores (10.95 points). The control group also improved (4.73 points), but the experimental group showed more significant gains (P < 0.0001).
People with KOA often adjust their walking pace to minimize the impact on their knee joint during heel strikes. Shoepe et al. highlighted the positive effects of AQE, especially for older adults. The AQE enhances muscle strength and water’s buoyancy, challenges balance and proprioception, promoting stability and reducing fall risk. Water allows for larger movements without excessive joint stress, facilitating functional gains. The water’s viscosity encourages slower, controlled movements, giving older adults more time to respond during training sessions.[21] In the current research, the interventional group significantly increased their walking speed by 4.13 (P < 0.0001). The conventional group also improved, although to a lesser extent (1.07, P = 0.0178).
In the present study, aquatic training was found to be more effective than land exercise in improving lower-limb muscle performance in bilateral KOA patients. These results can help physiotherapists create patient-centered, more efficient rehabilitation programs that address the functional and physical deficits linked to bilateral KOA.
Strengths
The eight-week follow-up period and AQE program demonstrate a commitment to consistency and gradual progression. In addition, the motivation and tolerance of participants with grade I and II KOA are positive indicators.
Limitations
The small sample size and focus on a single geographical area can impact the generalizability of the findings. Longer training periods and more intense interventions could enhance the evaluation of peri-articular muscle improvement in patients with bilateral KOA.
CONCLUSION
The study found that an eight-week aquatic training program helped alleviate pain and improved lower limb muscle performance in bilateral KOA patients.
Recommendations
Future research endeavors could focus on maintaining long-term fitness regimens post-intervention. It would be valuable to investigate the effects of intense aquatic resistance exercise on individuals with chronic hip OA issues, and those with OA who have additional comorbidities.
ACKNOWLEDGMENT
We acknowledge the guidance from Dr. G. Varadharajulu and Dr. Kakade for statistical help.
AUTHORS’ CONTRIBUTIONS
PJ and SS contributed to study conception and design, data acquisition, data analysis, manuscript preparation, and editing. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The study was approved by the Institutional Review Board at Institutional Human Ethics Committee of Krishna Institute of Medical Sciences, Deemed to be University, Karad, number 579/2022/2023, dated May 19, 2023.
DECLARATION OF PATIENT CONSENT
The authors certify they obtained all appropriate patient consent forms from study participants. In the consent form, patients have permitted clinical information to be reported in the journal. Patients understand that their names and initials will not be published, and efforts will be made to conceal their identity. However, complete anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of AI technology to assist in writing or editing the manuscript, and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Effect of spinal and lower limb re-alignment protocol on bilateral medial compartment osteoarthritis of knee in postmenopausal women. Int J Disabil Sports Health Sci. 2024;7:527-40.
- [CrossRef] [Google Scholar]
- To study the effect of agility and perturbation exercises versus dynamic resistance exercises to improve knee function in knee osteoarthritis-a comparative study. Int J Physiother. 2015;2:834-9.
- [CrossRef] [Google Scholar]
- Effect of multi-component exercises program on pain-related gait adaptations among individuals with osteoarthritis of the knee joint. J Educ Health Promot. 2023;12:138.
- [CrossRef] [PubMed] [Google Scholar]
- Objective assessment of knee proprioception and sensorimotor function in patients with primary gonarthrosis before and after knee replacement. Ortop Traumatol Rehabil. 2017;19:403-14.
- [CrossRef] [PubMed] [Google Scholar]
- Proprioceptive training for knee osteoarthritis: A systematic review and meta-analysis of randomized controlled trials. Front Med (Lausanne). 2021;8:699921.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of pain reduction on postural sway, proprioception, and quadriceps strength in subjects with knee osteoarthritis. Ann Rheum Dis. 2002;61:422-8.
- [CrossRef] [Google Scholar]
- Is aquatic exercise more effective than land-based exercise for knee osteoarthritis? Medicine (Baltimore). 2018;97:e13823.
- [CrossRef] [PubMed] [Google Scholar]
- Aquatic exercise for the treatment of knee and hip osteoarthritis. Cochrane Database Syst Rev. 2016;3:CD005523.
- [CrossRef] [PubMed] [Google Scholar]
- The PICO project: Aquatic exercise for knee osteoarthritis in overweight and obese individuals. BMC Musculoskelet Disord. 2013;14:320.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison between aquatic and thera-band exercises on pain intensity and endurance among obese individuals with knee osteoarthritis. Int J Hum Mov Sports Sci. 2022;10:1-9.
- [CrossRef] [Google Scholar]
- Effects of innovative aquatic proprioceptive training on knee proprioception in athletes with anterior cruciate ligament reconstruction: A randomized controlled trial. Arch Bone Jt Surg. 2021;9:519-26.
- [CrossRef] [Google Scholar]
- Effectiveness of aquatic exercises compared to patient-education on health status in individuals with knee osteoarthritis: A randomized controlled trial. Clin Rehabil. 2018;32:766-76.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of pre-participation aquatic training program on running performance in marathon runners. Int J Disabil Sports Health Sci. 2024;7:94-102.
- [CrossRef] [Google Scholar]
- Reliability and measurement error of the Osteoarthritis Research Society International (OARSI) recommended performance-based tests of physical function in people with hip and knee osteoarthritis. Osteoarthritis Cartilage. 2017;25:1792-6.
- [CrossRef] [PubMed] [Google Scholar]
- Quantitative effects of proprioceptive exercises and Mulligan's MWM in subjects with osteoarthritis of knee-a randomized clinical trial. Physiotherapy. 2015;101:e555-6.
- [CrossRef] [Google Scholar]
- Comparative effects of 2 aqua exercise programs on physical function, balance, and perceived quality of life in older adults with osteoarthritis. J Geriatr Phys Ther. 2015;38:17-27.
- [CrossRef] [PubMed] [Google Scholar]
- Aquatic physical therapy for hip and knee osteoarthritis: Results of a single-blind randomized controlled trial. Phys Ther. 2007;87:32-43.
- [CrossRef] [PubMed] [Google Scholar]
- The role of aquatic exercise on strength of quadriceps muscle and falling risk in elderly people. Res J Sport Sci. 2013;1:26-34.
- [Google Scholar]
- Efficacy of combined proprioceptive exercises and conventional physiotherapy in patients with osteoarthritis knee joint: A double-blinded two-group pretest-posttest design. J Ortho Traumatol Rehabil. 2018;10:94-7.
- [CrossRef] [Google Scholar]
- Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis. Health Technol Assess. 2005;9:iii-iv, ix-xi, 1-114
- [CrossRef] [PubMed] [Google Scholar]
- Elastic band prediction equations for combined free-weight and elastic band bench presses and squats. J Strength Cond Res. 2010;24:195-200.
- [CrossRef] [PubMed] [Google Scholar]






