Translate this page into:
Effectiveness of dynamic over static foot abduction brace and evaluation of impact of parental socioeducational status in the maintenance phase of clubfoot correction
2 Department of Physiotherapy, Swami Vivekananda National Institute of Rehabilitation Training and Research, Cuttack, Odisha, India
Corresponding Author:
Pabitra K Sahoo
Department of Physical Medicine and Rehabilitation, Swami Vivekananda National Institute of Rehabilitation Training and Research, Olatpur, Cuttack - 753 014, Odisha
India
pabitra2406@gmail.com
| How to cite this article: Sahoo PK, Vijay M, Das SP, Sahu MM, Sanyal A. Effectiveness of dynamic over static foot abduction brace and evaluation of impact of parental socioeducational status in the maintenance phase of clubfoot correction. J Musculoskelet Surg Res 2021;5:109-115 |
Abstract
Objective: Foot abduction brace (FAB) plays an important role in the maintenance phase of Ponseti clubfoot management. Compliance with the bracing protocol is affected by different foot brace designs. The parents' education and socioeconomic status are major concerns in developing countries, thought to influence bracing adherence. The objectives of this study were to compare the effectiveness of dynamic and static FAB and the impact of the socioeducational status on compliance with the treatment protocol. Methods: A total of 54 children with clubfeet met the study criteria and were randomly allotted to static and dynamic FAB groups. The socioeducational status of the parents was recorded by the modified Kuppuswamy scale. Pirani score and brace wearing time were evaluated at the end of the 1st week and 1st, 2nd, and 3rd month. Results: The dynamic brace had better compliance than the static brace and differed significantly (P = 0.025) at 1-month follow-up. The brace wearing time increased in the dynamic FAB group at 2nd and 3rd month, but the result had no statistical significance difference (P = 0.13 and 0.16, respectively). The dynamic FAB group had a significantly lower Pirani score. However, there was a difference at the 2nd- and 3rd-month follow-ups, but it was not significant (P = 0.08 and 0.16). The modified Kuppuswamy score, when correlated with brace wearing time, in both the groups showed weak relation and were not statistically significant. Conclusion: Pirani score and compliance with the bracing protocol, when compared between static and dynamic brace groups, showed a significant difference at the end of the 1st-month follow-up. However, when compared further, both groups of FABs had no significant difference in compliance and foot correction.
Introduction
The Ponseti protocol of serial casting is widely accepted for clubfoot management, and actually, it is considered the gold standard nowadays. After removing the last cast, the use of a brace is the key to the maintenance of successful correction and prevention of deformity recurrence. This is achieved by the use of a foot abduction brace (FAB). Dennis Browne (DB) brace that was used universally following clubfoot correction by Kites method has been modified by several researchers keeping the fundamental principle intact. One such constant feature is keeping the distance between the heels of the shoes equal to the child's shoulder width. FAB keeps the foot in abduction and dorsiflexion and maintains correction by stretching posterior medial soft tissue achieved by the last cast. The child needs to wear the brace 23 h a day except during bathing and toileting for the first 3 months, followed by a night brace till 3–4 years of age.[1] This bracing protocol has been shown to be very effective, but the results vary with the wearing rate among the users. One of the important contributing factors for the successful outcome of the Ponseti method is the sincere adherence to the protocol by the parents.[2]
Lack of adherence has shown to be a leading cause of recurrence.[3],[4],[5],[6],[7] Studies estimated the noncompliance rate as 32%–61% for initial brace users.[4],[5] The reasons for noncompliance are mainly attributed to insufficient counseling and lower socioeconomic and educational status of the parents.[3],[5] Causes are many folded such as slippage of shoes, crying, skin rashes, and other factors including cultural and esthetic issues.[8] Moreover, studies have also shown higher compliance with the optimum result using new design dynamic braces compared to the traditional DB brace.[9] To improve brace tolerance by children, dynamic FABs that allow motion at the hip have been introduced.[10] Parent education about the necessity of brace and bracing protocol has a direct impact on compliance and affects the incidence of recurrence. This hypothesis holds true for most of the underdeveloped or developing countries like India. An extensive literature search of comparative studies on the effectiveness of a dynamic over static brace was done. However, there is a paucity of literature showing a correlation between parents' socioeducational level and compliance with the bracing protocol. Although most studies considered the first 3 months of the maintenance phase of Ponseti correction as the most crucial period, compliance with the bracing protocol really matters.
The objectives of the study were to compare the effectiveness of dynamic and static FABs and to study the impact of the socioeducational status on compliance with treatment protocol during the maintenance phase of the Ponseti method of treating idiopathic clubfeet.
Materials and Methods
We conducted a randomized comparative study at a tertiary rehabilitation center in India, running a dedicated clubfoot clinic. All the children who reported to this clinic and underwent Ponseti serial casting technique from December 2018 to April 2019 were considered for the study. With approval from the institutional review board, the study was conducted ar the department of physical medicine and rehabilitation. The study maintained the codes of the Declaration of Helsinki.
Inclusion criteria were children with idiopathic clubfoot and completed the treatment phase of Ponseti method, those having Pirani score of “0” at the end of the casting period, and those who gave authorized informed consent. Children more than 2 years of age, those having a neuromuscular disorder, arthrogryposis, genetic syndromes, and previous surgery for clubfoot, and those failing to complete the follow-up were excluded. The subjects were randomly allocated into two groups using a sealed envelope method.
According to Garg and Porter's prospective cohort study, the compliance in the dynamic and static braces was 81% and 47%, respectively.[9] With reference to these values, the minimum required sample size with 80% power of study and 5% level of significance is 27 for each study group. The experimental group was given a dynamic FAB and a conventional static brace was used by the control group.
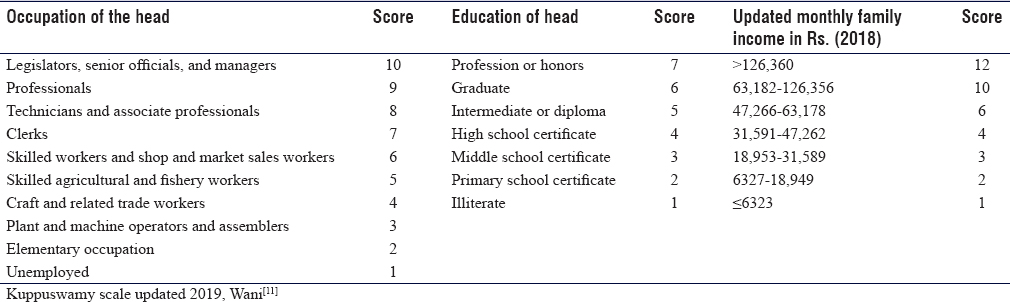
Demographic data were collected from all the participants before randomization. Socioeconomic status, including occupation, education level of parents or family head, and monthly income of the family was assessed using a modified Kuppuswamy scale, 2018 [Table - 1].[11] Pirani score was evaluated post-Ponseti serial cast deformity correction to ensure full correction. Children who have undergone the tendoachilles tenotomy procedure were also noted. A patient information sheet was provided to each parent or legal guardian, mentioning the study detail and their role during the study period. The subjects were reviewed four times within 3 months, along with weekly telecommunication regarding brace wearing time and the expected complications.
The static FAB used for the control group was the Steenbeek brace. It is a cost-effective brace developed by Steenbeek and David in Uganda.[12] It holds the affected foot in 70° of abduction and 15° dorsiflexion with a bar that keeps both feet separated. In unilateral involvement, the sound foot is kept at 40° of abduction and 15° dorsiflexion.[12] The brace does not allow independent unilateral movement of the lower limb at the hip and knee. The interventional group used a dynamic FAB called the Padmapada brace, without a sensor provided by Christian Medical College, Vellore, Tamil Nadu, for the study purpose [Figure - 1]. The principles for dynamic FAB are the same as static FAB except that the abduction bars are connected to the shoes through a four-bar linkage. This allows freedom of movement of the brace in the coronal plane and independent unilateral flexion–extension movement of hip and knees while maintaining the foot abduction, which can be possible [Figure - 2]. It helps for easy “rolling over” and crawling in babies. The angles maintained at the foot and ankle are the same as that of Steenbeek FAB. Both braces were provided free of cost by the institute.
 |
| Figure 1: Padmapada/dynamic foot abduction brace (above); Steenbeek/static foot abduction brace (below) |
 |
| Figure 2: Hip and knee movements in a child with dynamic brace |
Parents were given a printed sheet and instructed to mark the hours of brace use for each day in a week accurately. The brace wearing time data were arbitrarily divided into three categories, such as 23, 12–23, and <12 h/day. Using the brace for <23 h during the follow-up period is considered as a defaulter. Compliance was assessed by adherence to bracing protocol and reported brace wearing time during the study period. In the case of low compliance, the cause was ascertained by taking a detailed history from parents. Recurrence of the clubfoot deformity was noted at different follow-up intervals assessing the Pirani score.[13] Recurrence was defined as the reappearance of at least one of the four clubfoot components.[14] The Kuppuswamy score data were classified into five socioeconomic groups. A score of 26–29 is considered as an upper (I), 16–25 as the upper-middle (II), 11–15 as lower-middle (III), 5–10 as upper-lower (IV), and <5 as a lower class (V).[11]
Follow-up evaluations were done at the end of 1st week, 1st month, 2nd month, and 3rd month. On each visit, the Pirani score, the brace wearing time per day, and reasons for noncompliance were noted.
Statistical analysis
Clinical data were processed and analyzed using IBM SPSS Statistics, 24.0 software (IBM Corp., Bio-statistician). The mean and standard deviation for continuous variables and percentage (frequency) for categorical variables were measured. Quantitative variables were compared using the unpaired t-test and ANOVA for repetitive measures among the same group. Correlation of categorical variables was done by drawing Spearman's correlation coefficient. A P < 0.05 was considered statistically significant in each analysis.
Results
Biosocial parameters for both static and dynamic brace groups are depicted in [Table - 2]. The mean ages of both groups were comparable. Males were more in both groups. Bilateral clubfeet presentation was common in both groups, and in unilateral cases, the right-sided affection was more common (37%) in the static brace group. However, in the dynamic brace group, the left side was commonly involved (26%). Among the static FAB group, 44.5% belonged to the upper-lower class while lower-middle and upper-middle class comprised 26.5% each. In the dynamic FAB group, upper-lower, lower-middle, and upper-middle classes were 33.33% each [Figure - 3]. Percutaneous tendoachilles tenotomy as a part of the Ponseti treatment protocol was noted in 66.67% of the static brace and 63% of dynamic brace users.

 |
| Figure 3: Socioeconomic class distribution among study groups |
Brace wearing time for both groups reported at different time intervals is presented in [Table - 3]. Although average brace wearing time in children with static FAB decreased gradually in subsequent follow-ups, the difference was statistically insignificant (P = 0.08). The reasons for poor compliance reported by parents were crying of a child in five cases and slippage of the shoe in seven children. In the dynamic FAB group, one child died of pneumonia and the sample number was reduced to 26. Another child lost to follow-up from the 1st month onward. Statistically, no significant difference was observed among the average brace wearing durations in this group (P = 1.71). The decrease in compliance in the dynamic group was attributed to crying in three cases and slippage of shoes in seven cases.
The average Pirani score recorded in both groups at the end of 1st week, 1st month, 2nd month, and 3rd month showed alterations in the Pirani score, and the difference was statistically significant with a P = 0.04 and 0.039, respectively [Table - 3].

When the static FAB group compliance was compared with the dynamic FAB group, the later had less compliance during the 1st-week follow-up (P = 1.11). However, when evaluated at the end of 1st month, the dynamic FAB group had better compliance compared to the static one and the difference was significant (P = 0.025). During the 2nd and 3rd month, the average duration of brace wearing time increased in the dynamic FAB group. However, the difference was statistically insignificant (P = 0.13 and 0.16) [Table - 4].

Clinical comparison of Pirani score of both groups at the end of the 1st week showed a relatively lower score in the dynamic FAB group than the static group, but the difference was not statistically significant (P = 0.055). At 1st-month follow-up, the dynamic FAB group had a significantly lower Pirani score (P = 0.02). However, at 2nd- and 3rd-month follow-ups, though the Pirani score was clinically very low, the difference was insignificant (P = 0.08, P = 0.16 respectively) to draw any conclusion [Table - 4].
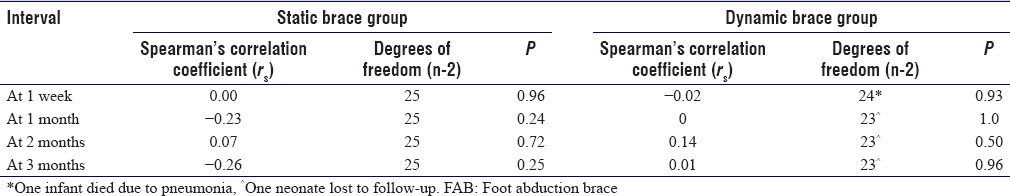
The modified Kuppuswamy score, when correlated with brace wearing time using Spearman's correlation coefficient, in both the static and dynamic groups, showed weak relation at different follow-up intervals and the results were statistically insignificant [Table - 5].
Discussion
This study showed that compliance to brace use in the form of brace wearing time had shown significant improvement in successive follow-ups in dynamic FAB users. The maintenance of correction assessed with Pirani score showed better correction in the dynamic FAB group, which might be due to better compliance. Parent's socioeducational status had found to have weak relation with compliance for both the groups.
The Ponseti protocol's success lies not only in the correction of deformity but also in the prevention of recurrence. Education and encouragement of parents about the proper use of the corrective brace play a key role in maintaining the initial correction. Researchers have emphasized bracing management, compliance with the bracing protocol, and their influence on the final result. Noncompliance has been defined as a failure to use the brace for 23 h per day during the first 3 months.[15] Newer brace designs are evolving to reduce the rate of noncompliance to improve the effectiveness of brace treatment. On the contrary, some studies have also reported that the brace type and design do not influence adherence and compliance with the bracing protocol.[16]
Several factors influence family acceptance level of brace treatment. Parents' common complaint is that the bracing makes their child irritable and limits their limb movement.[17] As the child cries, parents remove the brace without analyzing whether the child is crying because of pain or annoyance. Excessive crying and slippage of the shoe were the major causes of low compliance in this study, and most of them showed recurrence of deformity. An under-corrected foot, when placed in a brace, leads to dislodgment of the foot. More pressure on the strap is required to keep the foot in place; this may lead to more crying and discomfort, which may further reduce the compliance and a vicious cycle is created.[16] The decrease in compliance in the current study was mainly due to child crying, slippage of shoes, and associated illness.
Compliance with a brace is a great challenge, especially in children belonging to the low socioeconomic group with a parents' low education level.[18] Dobbs et al. observed that the most common reason for noncompliance was an inconvenience to use orthosis for 23 h a day for the first 3 months.[3] They also found that the chance of recurrence increased 183 times if the family does not adhere to the bracing protocol. Further, parental education level has been considered as a risk factor for recurrence. The risk is increased tenfold when the parents have a high school education or less compared with parents with education beyond high school. However, no significant relation was observed between parental income and the risk of recurrence.[3] A study conducted by Jawadi et al. analyzed the correlation between the brace use and the family's demographic data such as monthly income, educational level of the parents, and the number of children in the family, but no significant correlation was observed.[19] Chong et al. have shown that parents' education level, the mean income of the family, patient-reported satisfaction, age of caregiver, and compliance were lower in the recurrence group, but the results were statistically insignificant.[20] In our study also, no significant correlation between parents' socioeconomic status and compliance to brace use has been observed in both groups.
Some researchers adopted other strategies that might improve compliance to brace treatment, including educating the parent, providing written patient information sheets, and making follow-up phone calls.[21] Building up a physician–family relationship may be considered as an important factor in adherence to bracing.[5],[16] The current study adopted the same strategy by providing a parent information sheet to all study participants, explaining the study in detail and the possible benefits of the sincere brace use. The physician–participant relationship was maintained by follow-up phone calls throughout the study period. A study by Morin et al. has shown that improving the communication skills of doctors with parents was directly related to the recurrence rate.[22] However, in our study, results in terms of adherence to brace wearing time did not show any significant changes in both groups.
Major causes of noncompliance reported by parents using static braces such as babies cried during the brace application and “fed up” with using the brace.[19] Garg and Porter reported improved compliance, fewer recurrences, and fewer skin complications with the use of a dynamic brace compared to a traditional static brace. There was an 81% compliance rate in the dynamic bracing group compared to 41% in the static bracing group.[9] Mang'oli et al., in their study, used a locally made static FAB that was easily affordable as well as well tolerated. They found better compliance with the new brace than the traditional DB brace, which was only marginally inferior to the newer ones, the child-friendly–expensive brace.[23] Kessler also observed improvement of compliance issues when children with rigid abduction brace were switched to a new flexible brace.[24] However, Lara et al. did not find any statistically significant difference between the two types of abduction brace in maintaining the deformity correction.[25] The noncompliance rate was much less as observed by Dobbs et al. during the first 3 months, where they had shown a significant correlation between parent educational level and noncompliance as well as noncompliance and relapse. In our study, no significant correlation was established between parents' socioeconomic status and compliance to brace wearing time for both the static and dynamic brace groups. However, the brace wearing time or compliance was higher in dynamic FAB compared to static FAB and was significant at 1st-month follow-up only. The outcomes are supported by the study of Chen et al., which reported noncompliance in dynamic orthosis being 7% as opposed to 41% in the traditional orthosis.[26]
This study had the following limitations: the objective measures of brace use, such as with sensors, were not available. The verbal report of brace wearing time was used as the primary data assessing compliance, which might have been over or underreported. Follow-up of 3 months period may be inadequate for proper evaluation of the compliance and recurrence rates.
Conclusion
Pirani score and compliance with the bracing protocol, when compared between static and dynamic brace user groups in the maintenance phase of clubfoot management, in dynamic FAB users, showed good correction and better compliance at the end of 1st-month follow-up. Intolerance to brace use in the early stage was minimized by allowing for hip and knee movements with the dynamic FAB. However, when compared further, both the FABs had no significant difference in compliance and foot correction. Both of them had a weak correlation with the education and socioeconomic level of parents. Assessment of parents' socioeconomic status may portend the surgeon indirectly about the recurrence of deformity and the need for resources such as educational material and phone counseling in higher-risk cases to limit the recurrences.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms from parents. In the form the patients' parents have given their consent the images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Ethical consideration
The study had its ethical clearance from the Institutional Review Board vide No DA1A01/AC/EC dated February 11, 2019.
Acknowledgment
We would like to thank Christian Medical College, Vellore, Tamil Nadu, India, for providing us with the dynamic FAB named Padmapada brace free of cost.
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Authors' contribution
PKS conceived and designed the study as the principal investigator, supervised the study, and interpreted the results of the study. MV collected the data, statistically analyzed the data and prepared the initial draft of the manuscript. SPD provided intellectual inputs to preparation of the manuscript. MMS helped in drafting and correcting the initial version of the manuscript. AS revised the manuscript critically by providing important intellectual inputs. All authors have critically reviewed and approved the final draft and are responsible for the manuscript's content and similarity index.
| 1. | Morgenstein A, Davis R, Talwalkar V, Iwinski H Jr, Walker J, Milbrandt TA. A randomized clinical trial comparing reported and measured wear rates in clubfoot bracing using a novel pressure sensor. J Pediatr Orthop 2015;35:185-91. [Google Scholar] |
| 2. | Sangiorgio SN, Ho NC, Morgan RD, Ebramzadeh E, Zionts LE. The objective measurement of brace-use adherence in the treatment of idiopathic clubfoot. J Bone Joint Surg Am 2016;98:1598-605. [Google Scholar] |
| 3. | Dobbs MB, Rudzki JR, Purcell DB, Walton T, Porter KR, Gurnett CA. Factors predictive of outcome after use of the Ponseti method for the treatment of idiopathic clubfeet. J Bone Joint Surg Am 2004;86:22-7. [Google Scholar] |
| 4. | Ramírez N, Flynn JM, Fernández S, Seda W, Macchiavelli RE. Orthosis noncompliance after the Ponseti method for the treatment of idiopathic clubfeet: A relevant problem that needs reevaluation. J Pediatr Orthop 2011;31:710-5. [Google Scholar] |
| 5. | Zionts LE, Dietz FR. Bracing following correction of idiopathic clubfoot using the Ponseti method. J Am Acad Orthop Surg 2010;18:486-93. [Google Scholar] |
| 6. | Göksan B, Fuat B, İlker E, Bursalı A3, Eylem K. Factors affecting adherence with foot abduction orthosis following Ponseti method. Acta Orthop Traumatol Turc 2015;49:620-6. Available from: http://www.aott.org.tr/en/factors-affecting-adherence-with-foot-abduction-orthosis-following-ponseti-method-133796. [Last accessed on 2020 Sep 13]. [Google Scholar] |
| 7. | Janicki JA, Wright JG, Weir S, Narayanan UG. A comparison of ankle foot orthoses with foot abduction orthoses to prevent recurrence following correction of idiopathic clubfoot by the Ponseti method. J Bone Joint Surg Br 2011;93:700-4. [Google Scholar] |
| 8. | Morcuende JA, Dolan LA, Dietz FR, Ponseti IV. Radical reduction in the rate of extensive corrective surgery for clubfoot using the Ponseti method. Pediatrics 2004;113:376-80. [Google Scholar] |
| 9. | Garg S, Porter K. Improved bracing compliance in children with clubfeet using a dynamic orthosis. J Child Orthop 2009;3:271-6. [Google Scholar] |
| 10. | Desai L, Oprescu F, DiMeo A, Morcuende JA. Bracing in the treatment of children with clubfoot: Past, present, and future. Iowa Orthop J 2010;30:15-23. [Google Scholar] |
| 11. | Wani RT. Socioeconomic status scales-modified Kuppuswamy and Udai Pareekh's scale updated for 2019. J Family Med Prim Care 2019;8:1846-9. [Google Scholar] |
| 12. | Alves C. Bracing in clubfoot: Do we know enough? J Child Orthop 2019;13:258-64. [Google Scholar] |
| 13. | Khan MA, Chinoy MA, Moosa R, Ahmed SK. Significance of Pirani score at bracing-implications for recognizing a corrected clubfoot. Iowa Orthop J 2017;37:151-6. [Google Scholar] |
| 14. | Zhao D, Liu J, Zhao L, Wu Z. Relapse of clubfoot after treatment with the Ponseti method and the function of the foot abduction orthosis. Clin Orthop Surg 2014;6:245-52. [Google Scholar] |
| 15. | Jawadi AH. Clubfoot management by the Ponseti technique in Saudi patients. Saudi Med J 2010;31:49-52. [Google Scholar] |
| 16. | Hemo Y, Segev E, Yavor A, Ovadia D, Wientroub S, Hayek S. The influence of brace type on the success rate of the Ponseti treatment protocol for idiopathic clubfoot. J Child Orthop 2011;5:115-9. [Google Scholar] |
| 17. | Vitale MG, Choe JC, Vitale MA, Lee FY, Hyman JE, Roye DP Jr. Patient-based outcomes following clubfoot surgery: A 16-year follow-up study. J Pediatr Orthop 2005;25:533-8. [Google Scholar] |
| 18. | Porecha MM, Parmar DS, Chavda HR. Mid-term results of Ponseti method for the treatment of congenital idiopathic clubfoot--(A study of 67 clubfeet with mean five year follow-up). J Orthop Surg Res 2011;6:3. [Google Scholar] |
| 19. | Jawadi AH, Al-Abbasi EM, Tamim HA. Factors predicting brace noncompliance among idiopathic clubfoot patients treated with the Ponseti method. J Taibah Univ Med Sci 2015;10:444-8. [Google Scholar] |
| 20. | Chong DY, Finberg NS, Conklin MJ, Doyle JS, Khoury JG, Gilbert SR. Prospective evaluation of the use of Mitchell shoes and dynamic abduction brace for idiopathic clubfeet. J Pediatr Orthop B 2014;23:501-4. [Google Scholar] |
| 21. | Paulsen-Miller M, Dolan LA, Stineman A, Morcuende JA. Understanding the educational needs for parents of children with clubfoot. Orthop Nurs 2011;30:273-8. [Google Scholar] |
| 22. | Morin ML, Hoopes DM, Szalay EA. Positive communication paradigm decreases early recurrence in clubfoot treatment. J Pediatr Orthop 2014;34:219-22. [Google Scholar] |
| 23. | Mang'oli P, Theuri J, Kollmann T, MacDonald NE. Ponseti clubfoot management: Experience with the Steenbeek foot abduction brace. Paediatr Child Health 2014;19:513-4. [Google Scholar] |
| 24. | Kessler JI. A new flexible brace used in the Ponseti treatment of talipes equinovarus. J Pediatr Orthop B 2008;17:247-50. [Google Scholar] |
| 25. | Lara LC, Gil BL, Torres LC Filho, Dos Santos TP. Comparison between two types of abduction orthotics in treating congenital clubfoot. Acta Ortop Bras 2017;25:125-8. [Google Scholar] |
| 26. | Chen RC, Gordon JE, Luhmann SJ, Schoenecker PL, Dobbs MB. A new dynamic foot abduction orthosis for clubfoot treatment. J Pediatr Orthop 2007;27:522-8. [Google Scholar] |
Fulltext Views
5,124
PDF downloads
1,787





