Translate this page into:
Elastic stable intramedullary nailing as a treatment option for comminuted proximal humeral shaft fractures in adults: A report of two cases and a review of the literature
2 Department of Physical Medicine and Rehabilitation, King Fahad Medical City, Riyadh, Saudi Arabia
Corresponding Author:
Abdulmuhsen N Alshammari
Department of Orthopedics, King Fahad General Hospital, P.O. Box: 3892, Almadinah Almunawwarah,
Saudi Arabia
m_shamari@hotmail.com
| How to cite this article: Alshammari AN, Altayeb MA, Alnazer EM. Elastic stable intramedullary nailing as a treatment option for comminuted proximal humeral shaft fractures in adults: A report of two cases and a review of the literature. J Musculoskelet Surg Res 2019;3:221-227 |
Abstract
Despite the success of nonoperative treatment in the majority of adult-comminuted proximal third humeral shaft fractures, surgical intervention is preferable in selected cases in order to avoid specific potential disadvantages associated with nonoperative treatment, including shoulder and elbow stiffness, poor compliance, and nonunion. Elastic stable intramedullary nailing (ESIN) is commonly used in the treatment of children's long-bone fractures and is known to achieve a high union rate with minimal complications. The literature review of the use of percutaneous ESIN treatment of comminuted proximal third humeral shaft fractures reveals that while it is not a common procedure, it can still produce favorable results with limited complications. This paper evaluates the use of ESIN in two patients with comminuted proximal third humeral shaft fractures. The patients were aged 56 and 72 and both had experienced comminuted proximal third humeral shaft fractures. In this report, the management of these cases is presented, along with a review of other studies, which used ESIN in the treatment of humeral shaft fractures in adults.Introduction
Elastic stable intramedullary nailing (ESIN), also known as titanium elastic nailing or Nancy nailing, is a device that has low modular of elasticity, and the literature reveals that the resultant rotational stability is high with greater axial compression stiffness when used in pediatric femoral fractures, where it is the most common fracture-treated device.[1]
ESIN was first introduced in Nancy University, France in 1977 and was used in the treatment of a child with rickets. While it gained popularity in the management of pediatric long-bone fractures, the technique failed to achieve comparable acceptance in the treatment of adults due to the conviction that the basic biology of fractures differs in the bones of growing children. Specifically, it depends on the thick periosteum with its rich blood supply that gets less injured in comparison to the adult periosteum.[2]
The fixation biomechanical properties of this device depend on an intramedullary three-point fixation method, which is somewhat like the use of casting for fracture stabilization. This explains why some surgeons have described ESIN as an internal splint device.[1] In essence, it functions as a load sharing device, which gives it the advantage of limited cortical osteopenia compared to load-bearing devices.
Although the humerus is a nonweight-bearing bone, it does function to transmit load. This explains the diversity of management options, ranging from nonsurgical to surgical. Patients in the upper age demographic with humeral shaft fractures usually have multiple comorbidities, and they require inpatient management, which is associated with an increase in mortality.[3] Thus, choosing a treatment method associated with speedier recovery rates, earlier return to normal activity, and fewer complications is the goal.
On the other hand, Sarmiento popularized the nonoperative management with functional bracing for humeral shaft fractures.[4],[5] It has been reported that conservative management is associated with pain at the fracture site, some degree of loss of motion range in the shoulder and elbow joints, nonunion, and discomfort from the bracing in some patients.[6],[7],[8],[9] With medical advances, operative management has shown less nonunion and better functional outcome compared to conservative management.[8],[9] The usually used surgical options are external fixation, open reduction and plate fixation, and intramedullary locked nailing. With new reports showing a drawback from nailing to plating due to multi-factorial reasons including cost and higher surgical complications with intramedullary locked nailing.[10]
In an earlier study, Osman et al. reported that 22 out of 104 observed diaphyseal humeral fractures received fixation using multiple intramedullary wires through supracondylar approach. They consequently proposed the use of multiple intramedullary wires fixation for segmental humeral fractures or for diaphyseal fractures associated with fractures of the neck of the humerus.[11]
Insertion of ESIN for the treatment of humeral shaft fractures is usually done using the closed reduction internal fixation surgical technique under fluoroscopic guidance. This keeps the biology of bone healing intact without surgical dissection at the fracture site. In the humerus, ESIN can be inserted in a retrograde or antegrade fashion.
As far as the authors are aware, only a limited number of studies have specifically described the employment of this device in patients aged over 55 years with rare comminuted proximal third humeral shaft fractures classified as 12.C3i (proximal diaphyseal-metaphyseal) based on the new AO/Orthopaedic Trauma Association classification.[12]
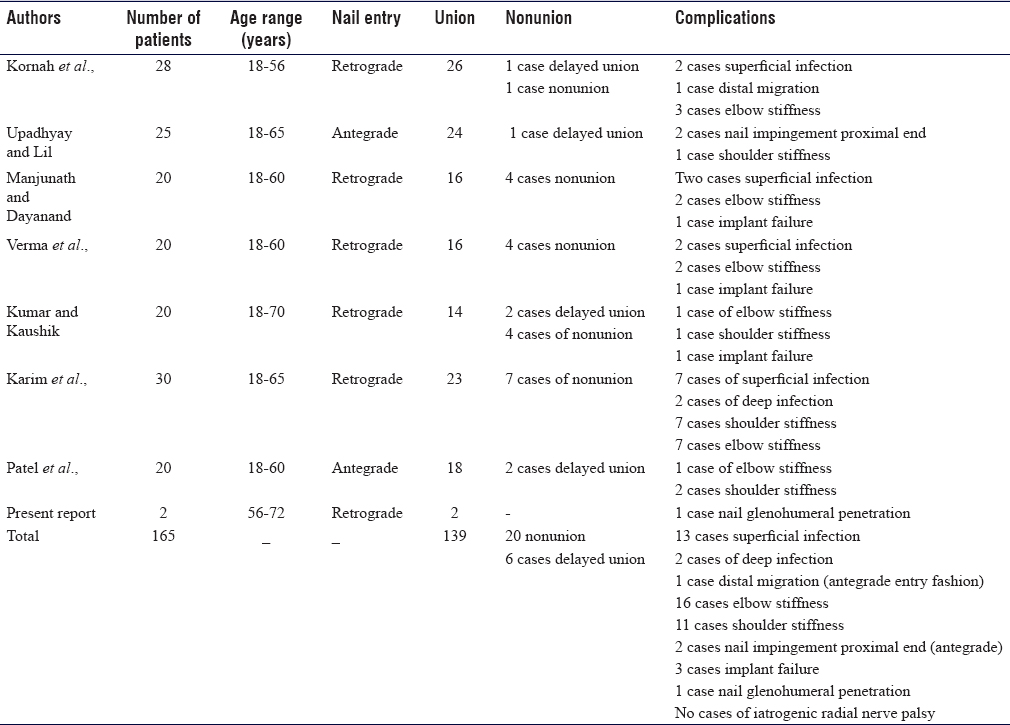
The intention of this report is to evaluate the use of retrograde ESIN in comminuted proximal third humeral shaft fractures in two individual cases. We also have reviewed the English language literature published within the past 10 years related to the use of this method in humeral shaft fractures [Table - 1].
Case Reports
The two cases reported here are those of a 72-year-old male and a 56-year-old female with comminuted proximal third humeral shaft fractures, managed by closed reduction and ESIN retrograde fixation at King Fahad General Hospital, Al-Madinah, Al-Munawwarah, Saudi Arabia. Both cases were followed up for approximately 18 months. The clinical course and management of these patients are discussed.
Case 1
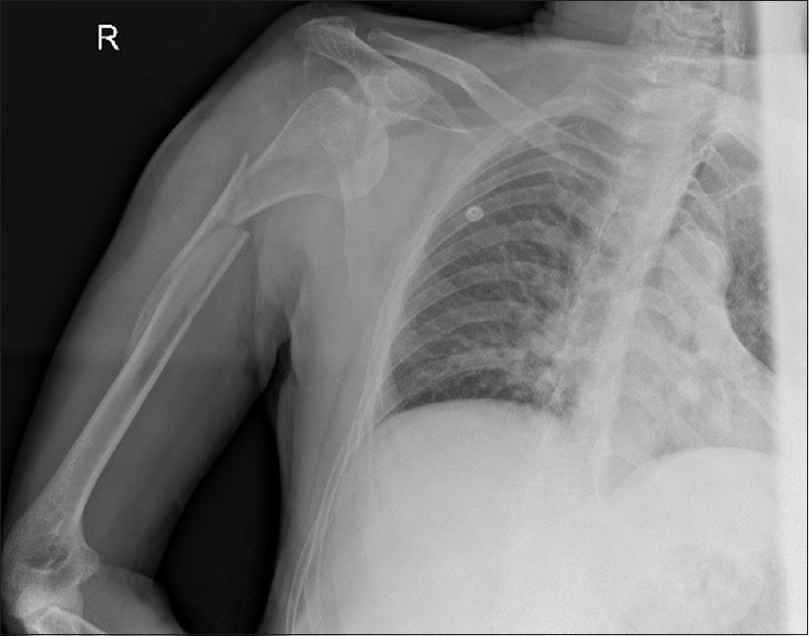
A 56-year-old right-handed obese female with hypothyroidism presented to our emergency department following involvement in a motor vehicle accident that day. She complained of pain and swelling of the right arm. On examination, she had normal vital signs. While the right arm was swollen and tender, the remainder of her examination was normal. There was no distal neurovascular deficit. Radiographs of the right humerus revealed a comminuted proximal third humeral shaft fracture [Figure - 1]. The arm was temporarily immobilized in a U-shaped slab applied in the emergency department. She was operated on the following day under general anesthesia, involving intraoperative fluoroscopy guidance in a supine position with the operated right upper limb placed over a flat radiolucent side table. In addition, intravenous prophylactic antibiotics were administered. Surgical treatment was performed by closed reduction and internal fixation using retrograde-inserted ESIN [Figure - 2].
 |
| Figure 1: Initial posttraumatic anteroposterior radiograph of the right humerus (Case 1) |
 |
| Figure 2: Immediate postoperative radiograph of the right humerus (Case 1) |
Postoperatively, the limb was initially immobilized in a broad-arm sling. Early functional physiotherapeutic training of the shoulder and elbow was commenced on the ensuing postoperative day. The patient was discharged in good general condition with a total inpatient stay of 3 days. After discharge, she continued to receive physiotherapy in the form of both muscle strengthening and shoulder pendulum exercises. She was followed up 2-week postoperatively to check for loss of reduction. Subsequent 4-, 8-, and 12-week postoperative checks were utilized to evaluate healing. These then continued at 3-month intervals until the 18-month postoperative point was reached. Plain radiographs taken at 4-month postoperatively indicated fracture healing with no hardware complications. At this stage, she was pain-free and satisfied with her function [Figure - 3]. At the 8-month follow-up check, the patient was able to perform all her daily activities with no difficulty. At the 18-month follow-up check, the patient's shoulder was painless and she regained a full range of motion. It was anticipated that the nails would be removed 3 months thence.
 |
| Figure 3: Anteroposterior radiograph 18-month postoperatively demonstrating complete fracture healing (Case 1) |
Case 2
A 72-year-old right-handed gentleman slipped on the floor and fell onto his right side. He presented to the emergency department with pain and swelling over the right shoulder and arm. His only recorded medical problem was hypertension, for which he was on antihypertensive medications. On arrival, he had a visible deformity of his arm and loss of the normal contour of the shoulder with no neurovascular deficits. Radiographs showed an anterior dislocation of the shoulder with a comminuted fracture of the proximal humeral shaft on the same side [Figure - 4]. Closed reduction under sedation was attempted in the emergency department but failed. The arm was temporarily immobilized in a U-shaped slab. After both his blood pressure and medical condition were stabilized, the surgery was performed early on the next day. The surgery took the form of a glenohumeral-closed reduction, followed by a fracture closed reduction and ESIN retrograde fixation of the humeral fracture under regional anesthesia and intraoperative fluoroscopy guidance. The entrance point for both nails was the lateral column of the distal humerus, 2 cm above the lateral epicondyle [Figure - 5].
 |
| Figure 4: Anteroposterior radiograph of the right humerus showing comminuted proximal third humeral shaft fractures associated with glenohumeral dislocation (Case 2) |
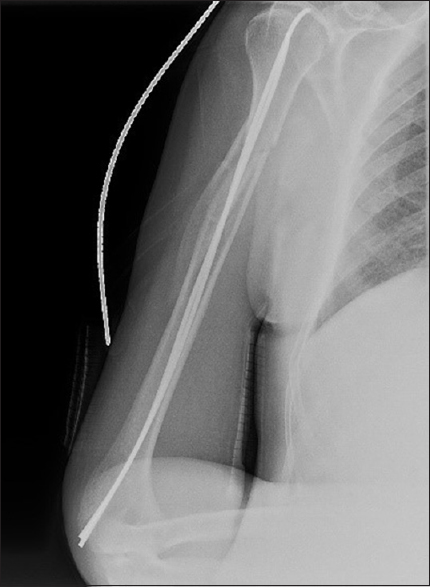 |
| Figure 5: Postoperative anteroposterior radiograph showing reduced glenohumeral joint dislocation and right humerus fixed by elastic stable intramedullary nailing (Case 2) |
Postoperatively, the right shoulder was immobilized in a Velpeau sling. Three-week postoperatively, the patient was encouraged to start a passive range of motion and shoulder muscle strengthening exercises. At around 3-month postoperatively, mild pain and restriction of shoulder abduction over 90° were demonstrated due to penetration of the tip of the nail out from the head of the humerus into the glenohumeral joint [Figure - 6]. At that time, there were clinical and radiological signs fracture healing. Consequently, after 1 week from that visit, both nails were removed, and complete fracture healing was recognized intraoperatively at the time of the nails removal, after which the pain was drastically reduced. At the 6-month follow-up assessment, the patient demonstrated a considerably improved range of motion. At the 18-month follow-up assessment, the patient's shoulder was painless with a satisfactory range of functional motion. No evidence of recurrence of dislocation or instability was observed.
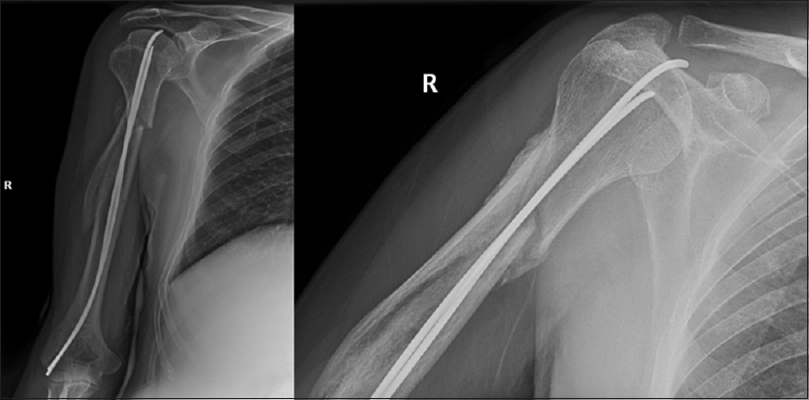 |
| Figure 6: Anteroposterior view of the right shoulder showing fractures healed in good position and nail tip penetration to the shoulder joint through the humeral head (Case 2) |
Discussion
Humeral shaft fractures account for 1%–3% of all fractures. This paper focuses on patients with a comminuted proximal third fracture of the humeral shaft, which is a relatively uncommon fracture location, in turn, representing only around 15% of all humeral shaft fractures as reported by Sarmiento and Verma et al.[4],[13] Comminuted humeral shaft fracture constituted an uncommon pattern among the 249 cases of unilateral humeral shaft fractures in Tytherleigh-Strong et al.'s research, they comprised a mere 10% of the cases described as complex Type-C fractures.[14] Although humeral shaft fractures are usually managed nonoperatively, Rutgers and Ring have shown that fractures located at the proximal third of the humerus have higher nonunion rates, specifically approximately 29%, when managed conservatively compared to middle 4% and none in the distal third humeral shaft fractures.[7]
The usual cause of humeral shaft fractures in the younger population is high energy trauma,[15],[16],[17] while in older age groups, humeral shaft fractures are usually a result of a fall or to a lesser commonly from pathology in the bony segment. As a result of osteoporosis, even minor trauma, such as a simple fall involving the arm, can cause a complex fracture pattern, which can ultimately result in permanent disability.[18] On the other hand, humeral shaft fractures are frequently accompanied by concomitant injuries and the incidence of associated injuries increases with age. In our report, the mechanism of injury in the second case was a trivial fall, which resulted in a comminuted proximal third shaft fracture associated with the anterior glenohumeral joint dislocation.[19]
Indications for operative management of humeral shaft fractures include, but are not limited to, open fractures, fractures associated with brachial artery injury, segmental fractures, floating elbow injuries, pathologic fractures, and patients with polytrauma and associated injuries, including lower extremity trauma, which require weight bearing through the upper extremity for crutch and/or walker use.[20] The number of indications of surgical management of humeral shaft fractures is expanding and the list of indications is being constantly amended as a consequence.
Jansen and Rasmussen have noted in their study that the nonoperative treatment of humeral shaft fractures in overweight patients is unsatisfactory.[21] Occasionally, it gets difficult to maintain the reduction of humeral shaft fracture in a satisfactory position in very obese patients and in women with very large breasts; in these cases, an internal fixation is indicated. Our first case was a morbidly obese female, and it was difficult to apply a proper U-shaped slab and maintain it as a definitive management option.
Age, osteoporosis, or the presence of multiple medical issues are not absolute indications for operative management. However, all these factors play a major role in causing patients to be incompatible with the brace and regular follow-up approach, and thus these variables are considered to be reasonable indications for surgical management.[20] To forestall the disadvantages of nonoperative management in the second patient and in consideration of his desire to regain good function with minimal intervention, ESIN was proposed along with the closed reduction of the glenohumeral dislocation.
Verma et al.'s study of 20 cases of diaphyseal humeral fractures managed with ESIN in a 19–57-year-old age group revealed a union rate of 80%, with the majority of fractures united in 10–16 weeks. The study encompassed all fracture morphology types with 60% being transverse. These had a nonunion rate of 20%, and all involved spiral and oblique fractures.[13]
A similar study by Manjunath and Dayanand observed 20 cases of humeral shaft fractures treated by ESIN retrograde closed reduction fixation. The ages of patients ranged from 18 to 60 years. The average time for union was 7.2 weeks and the overall union rate was 80%. There were no cases of iatrogenic nerve injury and two cases of superficial infection but no deep infection. None of the cases required blood transfusions. There were four nonunion cases and one case of implant failure. Two cases reported limited elbow range of motion due to nail prominence.[22]
Kumar andKaushik conducted a retrospective study of 20 cases, in which the majority of patients were in the middle age range, the average age being 40 years. Most of these patients had middle-third humeral shaft fractures and transverse fracture patterns. The study reported two cases with delayed union and four cases (20%) of nonunion. Nineteen cases (95%) achieved a full range of motion of the shoulder and elbow joint and 70% had healed within 18 weeks. There was one instance of the implant breaking at the fracture site.[23]
A study by Kornah et al. reported 28 humeral shaft fractures with different levels of humerus stabilized by ESINs. Union was achieved in 26 patients (92.8%) at a mean time of 13.1 weeks. One case was reported of distal nail migration. This required rehammering and trimming to avoid skin irritation. Superficial infection developed in two patients and was managed by daily dressing and antibiotics. The average time of inpatient stay was 2–5 days. None of the patients experienced implant failure.[24]
The recent prospective study by Patel et al. and the retrospective study by Upadhyay andLil both used an antegrade approach and exclude unstable fracture geometry. Only two cases out of the 25 in Upadhyay andLil study revealed nail impingement at the proximal end. The same complication was reported in two out of the 20 cases analyzed by Patel et al., in which the same insertion method has been employed. Furthermore, shoulder stiffness was recorded in these two cases due to impingement of the nail, although the patients subsequently regained favorable functional outcome following nail removal and physiotherapy. In our second case, shoulder range of motion was limited due to nail penetration to the shoulder joint through the humeral head, and once the nail was extracted, the patient regained acceptable shoulder function. In both methods of insertion (antegrade and retrograde), nail penetration can be managed if proper healing was documented by removal followed by physiotherapy, which reveals good functional outcomes.[25],[26] On the other hand, in cases when healing did not occur, pulling off the nail with trimming can be used. The study by Nectoux et al. reported that the use of end caps provided improved stability over the alignment of length-unstable fractures and may address the problem of fracture telescoping in the poor quality bone and comminuted fractures.[27] In a biomechanical study, Chen et al. demonstrated that prebending ESIN in a double C-shaped manner with degree equal to the intramedullary canal diameter and combined with end caps play a major role in improving the stability and offer a good solution for treating comminuted diaphyseal long-bone fractures.[28]
No cases of deep infection were recorded as a complication in either in the present study or in the above-mentioned studies. This contrasts with Karim et al.'s study of 30 cases of humeral shaft fractures fixed by ESINs. Two reported cases of deep infection were treated with intravenous antibiotics, removal of nails, and the use of a temporary external fixator, followed by a fracture brace. In addition, seven cases developed superficial infections and were treated with a short course of oral antibiotics. The majority of patients in Karim et al.'s series had transverse fracture patterns, and the age range was 18–65 years.[29]
It has been demonstrated that the use of ESIN in humeral shaft fractures is an acceptable surgical option providing satisfactory results. One of the most commonly encountered device complications is shoulder stiffness due to impingement from a prominent device when the antegrade technique is employed. The device has only limited significant complications. None of the aforementioned studies reported iatrogenic radial nerve injury (a known complication of plating) and only one study reported having a deep infection. In addition, this device is renowned for its short operative time and reduced hospital stays. We have also used it in a fracture dislocation case, in which it presented a favorable functional outcome.
When considering nonunion or delayed union, it is suggested that this is caused by motion at the fracture site secondary to poor rotational control when the canal is not filled with the nails as recommended by Rosenbaum and Uhl.[30] It has already been noted that mechanical distraction can contribute to nonunion.[31] In fact, the use of ESINs in comminuted humeral shaft fractures facilitates alignment of the fractures with relative stability, and subsequent secondary bone healing typically occurs at the fracture site. In an experimental surgical study conducted in animals, it was revealed that fracture healing with ESIN is mainly by periosteal callus (external callus). Furthermore, it was proved that two intramedullary nails do not completely fill the medullary canal and thus endosteal callus formation is not inhibited.[32] Another factor related to nonunion is metallosis and titanium-alloy wear particles; Kang and Stern reported one case of metallosis associated with humeral hypertrophic nonunion after ESIN fixation.[33] In our cases, both cases did not have metallosis nor nonunion.
Conclusion
The review of the literature and our two cases support the proposition that the closed reduction and ESIN fixation of comminuted proximal humeral shaft fractures technique offers limited complications and improved patients' satisfaction. However, further studies are required with larger sample sizes to confirm these findings.
Clinical message
In the elderly, comminuted humeral shaft fractures are not always amenable to standard treatments. To address predictable conditions, such as those requiring restricted operative time, minimal blood loss, and soft-tissue damage, and in order to minimize the length of hospital stay, the usage of ESIN presents as a viable alternative.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors contributions
ANA and MAA conceived and designed the study. ANA and EMA collected and organized data while ANA and MAA wrote initial and final draft of the article and provided critical input. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Fricka KB, Mahar AT, Lee SS, Newton PO. Biomechanical analysis of antegrade and retrograde flexible intramedullary nail fixation of pediatric femoral fractures using a synthetic bone model. J Pediatr Orthop 2004;24:167-71. [Google Scholar] |
| 2. | Hunter JB. The principles of elastic stable intramedullary nailing in children. Injury 2005;36 Suppl 1:A20-4. [Google Scholar] |
| 3. | Somersalo A, Paloneva J, Kautiainen H, Lönnroos E, Heinänen M, Kiviranta I, et al. Increased mortality after upper extremity fracture requiring inpatient care. Acta Orthop 2015;86:533-57. [Google Scholar] |
| 4. | Sarmiento A, Zagorski JB, Zych GA, Latta LL, Capps CA. Functional bracing for the treatment of fractures of the humeral diaphysis. J Bone Joint Surg Am 2000;82:478-86. [Google Scholar] |
| 5. | Sarmiento A, Kinman PB, Galvin EG, Schmitt RH, Phillips JG. Functional bracing of fractures of the shaft of the humerus. J Bone Joint Surg Am 1977;59:596-601. [Google Scholar] |
| 6. | Fjalestad T, Strømsøe K, Salvesen P, Rostad B. Functional results of braced humeral diaphyseal fractures: Why do 38% lose external rotation of the shoulder? Arch Orthop Trauma Surg 2000;120:281-5. [Google Scholar] |
| 7. | Rutgers M, Ring D. Treatment of diaphyseal fractures of the humerus using a functional brace. J Orthop Trauma 2006;20:597-601. [Google Scholar] |
| 8. | Denard A Jr., Richards JE, Obremskey WT, Tucker MC, Floyd M, Herzog GA, et al. Outcome of nonoperative vs operative treatment of humeral shaft fractures: A retrospective study of 213 patients. Orthopedics 2010;33:552. [Google Scholar] |
| 9. | Matsunaga FT, Tamaoki MJ, Matsumoto MH, Netto NA, Faloppa F, Belloti JC, et al. Minimally invasive osteosynthesis with a bridge plate versus a functional brace for humeral shaft fractures: A randomized controlled trial. J Bone Joint Surg Am 2017;99:583-92. [Google Scholar] |
| 10. | Gottschalk MB, Carpenter W, Hiza E, Reisman W, Roberson J. Humeral shaft fracture fixation: Incidence rates and complications as reported by American board of orthopaedic surgery part II candidates. J Bone Joint Surg Am 2016;98:e71. [Google Scholar] |
| 11. | Osman N, Touam C, Masmejean E, Asfazadourian H, Alnot JY. Results of non-operative and operative treatment of humeral shaft fractures. A series of 104 cases. Chir Main 1998;17:195-206. [Google Scholar] |
| 12. | Kellam JF, Meinberg EG, Agel J, Karam MD, Roberts CS. Introduction: Fracture and dislocation classification compendium-2018: International comprehensive classification of fractures and dislocations committee. J Orthop Trauma 2018;32 Suppl 1:S1-10. [Google Scholar] |
| 13. | Verma A, Kushwaha SS, Khan YA, Mohammed F, Shekhar S, Goyal A, et al. Clinical outcome of treatment of diaphyseal fractures of humerus treated by titanium elastic nails in adult age group. J Clin Diagn Res 2017;11:RC01-RC04. [Google Scholar] |
| 14. | Tytherleigh-Strong G, Walls N, McQueen MM. The epidemiology of humeral shaft fractures. J Bone Joint Surg Br 1998;80:249-53. [Google Scholar] |
| 15. | Ekholm R, Adami J, Tidermark J, Hansson K, Törnkvist H, Ponzer S, et al. Fractures of the shaft of the humerus. An epidemiological study of 401 fractures. J Bone Joint Surg Br 2006;88:1469-73. [Google Scholar] |
| 16. | Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury 2006;37:691-7. [Google Scholar] |
| 17. | Walker M, Palumbo B, Badman B, Brooks J, Van Gelderen J, Mighell M, et al. Humeral shaft fractures: A review. J Shoulder Elbow Surg 2011;20:833-44. [Google Scholar] |
| 18. | Mahabier KC, Van Lieshout EM, Bolhuis HW, Bos PK, Bronkhorst MW, Bruijninckx MM, et al. HUMeral shaft fractures: Measuring recovery after operative versus non-operative treatment (HUMMER): A multicenter comparative observational study. BMC Musculoskelet Disord 2014;15:39. [Google Scholar] |
| 19. | Schneider KN, Schliemann B, Manz SM, Buddhdev PK, Ahlbäumeri G. Bilateral anterior shoulder dislocation in the elderly – A case report and review of the literature. J Orthop Case Rep 2017;7:42-9. [Google Scholar] |
| 20. | Attum B, Obremskey W. Treatment of humeral shaft fractures: A critical analysis review. JBJS Rev 2015;3. pii: 01874474-201509000-00001. [Google Scholar] |
| 21. | Jensen AT, Rasmussen S. Being overweight and multiple fractures are indications for operative treatment of humeral shaft fractures. Injury 1995;26:263-4. [Google Scholar] |
| 22. | Manjunath, Dayanand. Outcome of Fracture Shaft Humerus Treated with TENS. Int J Orthop Rehabil 2018;4:20-3. [Google Scholar] |
| 23. | Kumar M, Kaushik YS. Functional outcome of humerus shaft fractures in adults treated by flexible nails using retrograde technique. Int J Orthop Sci 2017;3:176-8. [Google Scholar] |
| 24. | Kornah BA, Soltan AA, Abdel-Aal MA. Elastic stable intramedullary nailing for closed diaphyseal fractures of humerus in adults. A case series of 28 patients. J Trauma Treat 2017;6:400. [Google Scholar] |
| 25. | Upadhyay AS, Lil NA. Use of titanium elastic nails in the adult diaphyseal humerus fractures. Malays Orthop J 2017;11:53-9. [Google Scholar] |
| 26. | Patel I, Modi DR, Patel M. Functional outcome of humeral shaft fractures in adults treated with titanium elastic nailing. Int J Res Orthop 2018;4:582. [Google Scholar] |
| 27. | Nectoux E, Giacomelli MC, Karger C, Gicquel P, Clavert JM. Use of end caps in elastic stable intramedullary nailing of femoral and tibial unstable fractures in children: Preliminary results in 11 fractures. J Child Orthop 2008;2:309-14. [Google Scholar] |
| 28. | Chen YN, Lee PY, Chang CW, Ho YH, Peng YT, Chang CH, et al. Biomechanical investigation of titanium elastic nail prebending for treating diaphyseal long bone fractures. Australas Phys Eng Sci Med 2017;40:115-26. [Google Scholar] |
| 29. | Karim A, Ahmed MA, Haq A. Titanium elastic nailing in adult humerus diaphyseal fracture. Med Forum 2018;29:32-5. [Google Scholar] |
| 30. | Rosenbaum A, Uhl R. Nonunion of humeral shaft fractures following flexible nailing fixation. Orthopedics 2012;35:512-5. [Google Scholar] |
| 31. | Cheng HR, Lin J. Prospective randomized comparative study of antegrade and retrograde locked nailing for middle humeral shaft fracture. J Trauma 2008;65:94-102. [Google Scholar] |
| 32. | Vining NC, Goldberg MJ. Pierre lascombes: Flexible intramedullary nailing in children: The Nancy University manual. J Child Orthop 2010;4:477-8. [Google Scholar] |
| 33. | Kang R, Stern PJ. Humeral nonunion associated with metallosis secondary to use of a titanium flexible humeral intramedullary nail: A case report. J Bone Joint Surg Am 2002;84-A: 2266-9. [Google Scholar] |
Fulltext Views
6,263
PDF downloads
2,151





