Translate this page into:
Excellent outcome with modified thompson quadricepsplasty for knee extension contracture: Case report and review of the literature
Corresponding Author:
Sarmad Rashed K. Sulaiman
Department of Orthopaedic Surgery, Al Madina Al Munawara Hospital 60, Mahzur, Medina 42319, Almadinah Almunawwarah
Saudi Arabia
sar.ortsursrm@gmail.com
| How to cite this article: K. Sulaiman SR. Excellent outcome with modified thompson quadricepsplasty for knee extension contracture: Case report and review of the literature. J Musculoskelet Surg Res 2021;5:67-74 |
Abstract
The daily life routine activities require a good range of knee motion, losing that after femur fracture is a common problem that can be triggered by extension contracture, flexion contracture, or combined contractures. This case report is about a 19-year-old male with unremarkable medical history who suffered from extension contracture with no flexion following a wrongly applied plate for distal femur fracture, which was treated successfully surgically by modified Thompson's quadricepsplasty after 21 months from the initial injury. The final outcome was no extension lag and 120° active flection. The aim of reporting this case was to increase the awareness about the modified Thompson's quadricepsplasty, which is an excellent solution to the debilitating extension contracture complication and present a review of the literature of this procedure. The aim of the literature review is to evaluate the correlation and the influence of the patient's age, the interval to quadricepsplasty after the initial trauma, preoperative knee range of motion, surgical approach, and the postoperative care on the outcome of Thompson's quadricepsplasty and its modifications for the treatment of posttraumatic knee contractures besides that, to answer the question: Is Thompson's quadricepsplasty an excellent procedure to treat knee extension contracture?
Introduction
Extension contracture is a mischievous condition and is less frequent than flexion contracture.[1] Knee extension contracture remains to be a challenge to manage after distal femur fractures and can compromise the capability to carry out everyday activities.[2],[3],[4] The routine daily life activities require a good knee range of motion (ROM); for suitable walking, especially on slopes, <90° of knee flexion is necessary. At the same time, knee flexion of 90°–120° is needed for sitting comfortably on chairs and going upstairs, and for having a bath, nearly 135° of knee flexion is required. The literature suggests that 110° of flexion appears as an appropriate target for the rehabilitation of knee motion.[5],[6] For religious and social traditions, it is essential for daily life in many Asian countries to sit on the ground, losing that is considered a significant disability.[7],[8],[9],[10]
Extension contracture still occurs even with the development of surgical procedures and physical therapy.[11] This is because the fibrous scar proliferation in the knee joint predominantly facilitates adhesions and retraction of soft tissues,[2],[3],[4],[12],[13],[14],[15],[16],[17] which is associated with progressive limitation of knee ROM. Furthermore, fractures around the knee joint and malunion could worsen the knee ROM alongside the fibrosis and the loss of resilience of muscles, fascia, intermuscular septum, and aponeurosis that surround the knee joint. Depending on the description of the initial injury, intra-articular and extra-articular causes present in variable degrees.[15]
However, it would be critical to evaluate the causes properly before any operative intervention. If all causes are not handled correctly, failure is forthcoming. Quadriceps femoris muscle contracture was believed to be the main cause of extended knee stiffness where the muscle fails to lengthen enough to allow flexion and that could happen because of trauma, fracture fixation, or implant removal.[11] Quadricepsplasty is still the recommended technique for knee extension contracture treatment when there is a persistent decrease in knee ROM even with intensive physiotherapy.[1],[2],[3],[4],[8],[9],[10],[11],[16],[17],[18],[19],[20],[21],[22],[23],[24],[25],[26],[27],[28],[29],[30],[31],[32]
Many surgical procedures were used to treat knee extension contracture. Bennett[13] was the first to describe the lengthening of the quadriceps tendon in 1922, then Thompson[2] described his method in 1944, followed by Judet[14] in 1959. However, Thompson's quadricepsplasty and Judet's quadricepsplasty both raise concerns regarding the clinical outcomes and problems of wound healing like dehiscence, infection, skin necrosis, and failure of full extension associated with sizable exposures.[1],[2],[3],[14],[18],[19],[20],[24],[26],[29],[31] To avoid this, modifications of Thompson and Judet surgical techniques were described by many authors.[3],[4],[10],[18],[19],[20],[24],[27],[29],[31],[32]
The aim of reporting this case was to increase the awareness about the modified Thompson's quadricepsplasty, which is an excellent solution to the debilitating extension contracture complication. The literature review was to evaluate the correlation and the influence of the patient's age, interval to the quadricepsplasty after the initial trauma (IQ), preoperative knee ROM, surgical approach, and the postoperative care on the outcome of Thompson's quadricepsplasty and its modifications for the treatment of posttraumatic knee contractures besides that, to answer the question: Is Thompson's quadricepsplasty an excellent procedure to treat knee extension contracture?
Case Report
A 19-year-old male with unremarkable medical history was hit by a car in April 2017 and sustained a right femur close supracondylar fracture. He was taken for surgery in another hospital the next day for fracture fixation with plate and screws. After surgery, a long leg cast was applied for 3 months; during that time, he had a superficial infection at the surgery site managed conservatively with antibiotics and frequent dressings.
After 3 months, the cast was removed, intensive knee physiotherapy was commenced for 3 months, but the knee ROM failed to improve. In October 2017, the plate and screws were removed, physiotherapy was resumed and lasted for another 3 months, but improvement in flexion was not achieved.
The patient was first seen in our orthopedic clinic in January 2019, complaining of the inability to bend his knee. His local examination showed a healed surgical scar with no wound complications, restricted knee ROM with no flexion, and nonmobile patella. Quadriceps muscle was atrophied; muscle power could not be assessed correctly because there was no knee ROM. However, no signs of chronic infection were there, and the distal neurovascular examination was normal. The inflammatory markers were within the normal range.
Radiographs [Figure - 1] before and after implant removal showed a united supracondylar femur fracture with the plate wrongly applied on the femur's anterior surface and a decrease in the patellofemoral joint space with irregular articular outlines denoting the loss of articular cartilage. The patient was admitted in January 2019 and prepared for surgery.
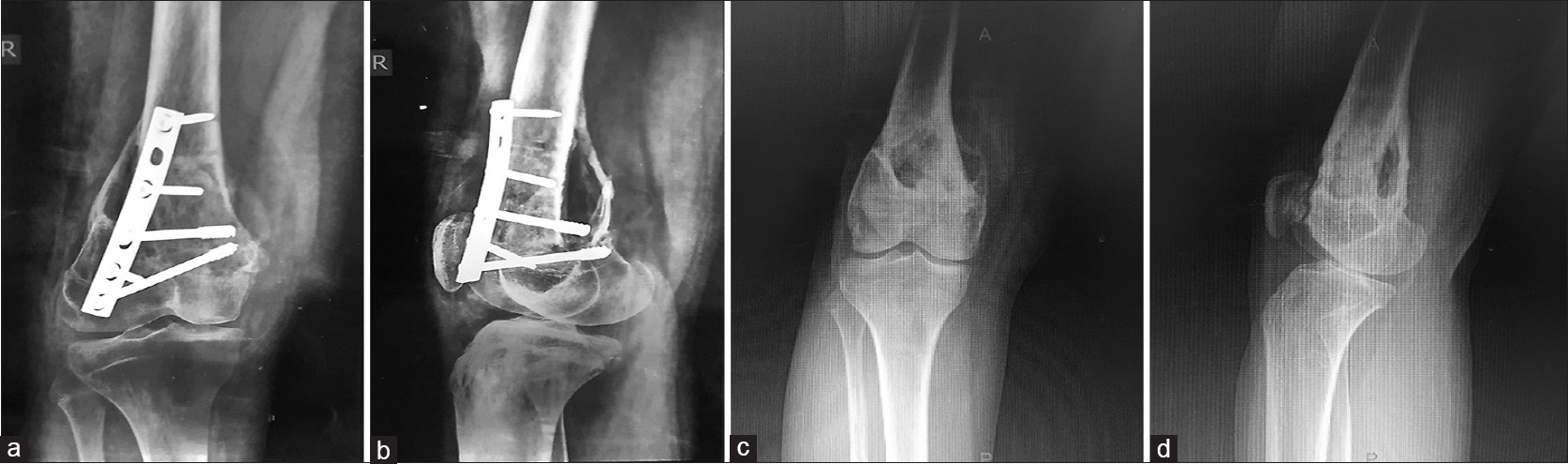 |
| Figure 1: (a and b) An anteroposterior and a lateral view showing the plate, which was fixed anteriorly abutting the patella and preventing it from appropriate gliding on its tract. (c and d) Postoperative radiograph after implant removal, lateral view showing abnormal articulation between patella and femur and a bony bridge posteriorly |
Surgical technique
With the patient in the supine position, the passive knee ROM was assessed under general anesthesia; the knee was fixed in extension with a total loss of flexion [Figure - 2]a. Tourniquet was not used, and an anterolateral incision on the previous scar extended from the distal third of the thigh to the tibial tuberosity distally.
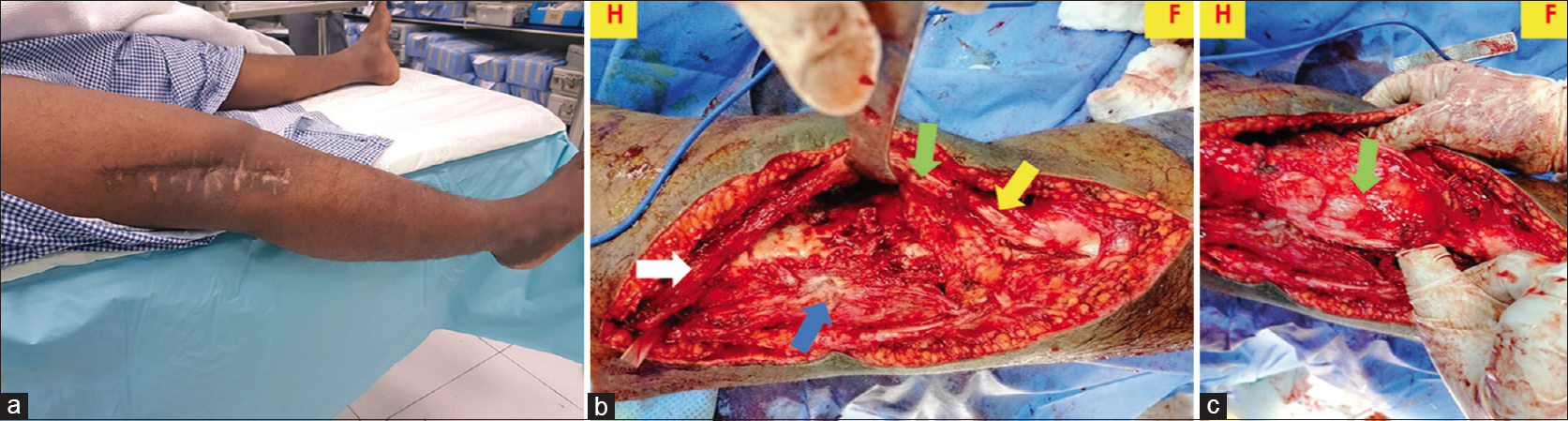 |
| Figure 2: (a) The knee was fixed in extension with the patient under general anesthesia. (b) After releasing vastus lateralis and its expansion, separation patella from the femur and releasing the patellar tendon. Screws holes appear on the anterior surface distal femur. (c) The picture showing that the anterolateral approach with a medial skin flap gave excellent exposure to medial retinaculum and vastus medialis. (H) Head side. (F) Foot side, white arrow rectus femoris, green arrow patella, yellow arrow patellar tendon, blue arrow vastus lateralis |
Dissection was carried out medially between the thigh fascia and the quadriceps to protect the skin's blood supply and minimizing skin necrosis. Medial skin flap above the quadriceps, the patella and the patellar tendon were retracted medially.
The patella was found adhered to the femur firmly. The vastus intermedius was fibrosed and anchored to the rectus femoris tendon. The suprapatellar pouch was obliterated and fibrosed, the vasti aponeurotic expansions were adhered to both sides of the femoral condyles, and the infrapatellar fat pad was fibrosed as well.
The junctions of vastus medialis and vastus lateralis with the rectus femoris were identified. Vastus lateralis was isolated from the rectus femoris. Medial and lateral retinacula were incised on each side of the patella, and the patellar tendon dawn to its attachment to the tibia were freed from the femoral condyles to regain the synovial recess medially and laterally.
The patella was separated from the femur by a thin osteotome; there was no cartilage on its articular surface, only a rough subchondral surface. The rough surfaces of the patella and the femur were smoothened with a fine bone rasp. The vastus intermedius was divided and excised. The patellar tendon was released from the fibrosed infrapatellar fat pad and proximal tibia [Figure - 2]b and [Figure - 2]c. The knee was manipulated at this stage; about 90° of flexion was obtained. Then, vastus medialis was isolated from the rectus femoris by blunt dissection, and 120° of flexion was obtained [Figure - 3]. The vasti were kept in place because it was impossible to suture them back and maintain the 120° flexion. The wound edges were sutured carefully above a closed suction drain.
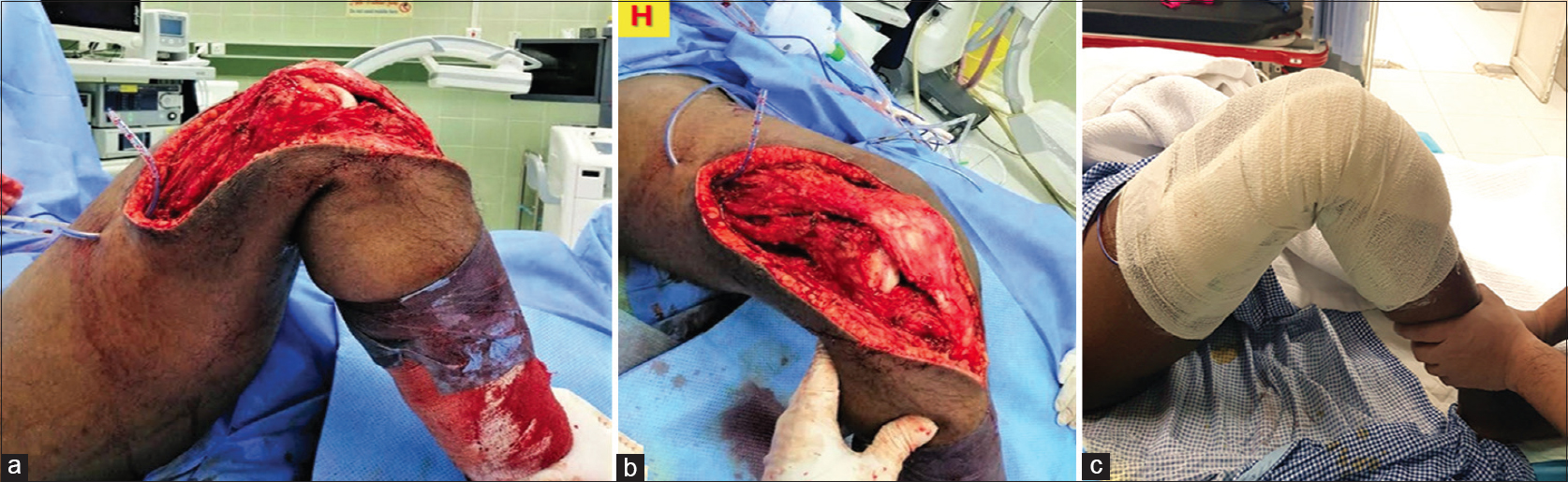 |
| Figure 3: (a and b) Showing flexion after release. (c) Degree of flexion in the recovery room. (H) head side |
Immediately postsurgery, a continuous passive motion (CPM) device was used [Figure - 4]a. The device was set up to give 0°–90° flexion increasing gradually. Siting with knee flexion and partial weight-bearing with support were encouraged [Figure - 4]b. After 7 days, the patient was discharged home on mild analgesia.
 |
| Figure 4: (a) Continuous passive motion for postoperative rehabilitation. (b) Five days after surgery, the patient could sit comfortably with the knee flexed 90° |
Sutures were removed after 14 days. The patient was trained to contract the quadriceps muscles and maintain it for seconds then relax it. He was advised to continue the knee flexion and extension exercises actively and passively until the knee extended against gravity. After that, a gradual increase of weights was added to the foot during exercises until the patient could achieve a full extension. After the rectus femoris muscle power improved, the patient walked with support and then allowed to bear weight gradually.
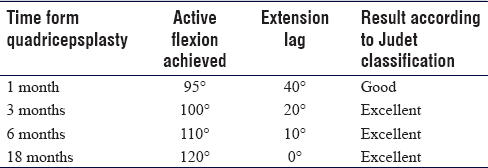
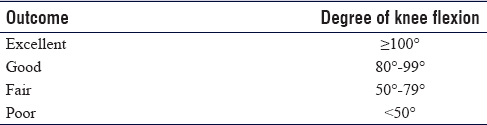
The postoperative follow-up results of the patient were summarized in [Table - 1]. The patient could sit cross-legged and pray on the ground after 10 months from quadricepsplasty [Figure - 5]a and [Figure - 5]b. Full knee ROM was regained after 18 months [Figure - 5]c and [Figure - 5]d. The Judet classification [Table - 2] was adopted for knee flexion assessment[8],[10],[14],[25] because it is relatively simple and practical. According to Judet criteria, the result, in this case, was excellent.
 |
| Figure 5: (a and b) Ten months after surgery, the patient sat with a cross-leg position and prayed on the ground. (c and d) Eighteen months after surgery, excellent knee flexion and no extension lag |
Discussion
In this reported case, the adhesions occurred because the plate was misplaced. Furthermore, leaving the cast for 3 months after surgery negatively affected the knee motion. The elements of the morbid anatomy that decrease the knee ROM can be inside or outside the knee joint.[3] These include adhesions, fibrosis and shortening of soft tissues such as the rectus femoris, the vasti, synovial recesses, aponeurotic expansions and the patellofemoral joint adhesions.[2],[3],[4],[12],[13],[14],[15],[16],[17] To get an appropriate outcome, it is crucial to tackle the morbid anatomy accurately.
Thompson shared his very satisfactory result and described his principles of the technique of quadricepsplasty. The core principle was excision of the scarred tissue and isolation of the normal muscle from the surrounding scar tissue in the thigh's extensor mechanism, and then with the physical therapy, the rectus femoris is strengthened to the degree that it takes the action of knee extension.[2]
In the standard Thompson's quadricepsplasty technique, the rectus femoris is separated entirely from the vasti surgically. To the best of my knowledge, the procedure was never described for the knee extension contractures caused by a wrongly applied plate on the distal femur. In the current case, a modified surgical technique to the original Thompson's quadricepsplasty was performed.[2],[3],[19] Instead of an anterior midline incision as in the original technique and some modifications to the technique,[9],[10],[27],[32] an anterolateral incision through the previous scar was used to reduce the wound healing problems. This approach gave good access to the lateral and medial sides. There was no need for a separate incision for medial retinaculum release, as reported in some modified techniques.[18],[32] Good flexion was achieved without dividing the tensor fascia lata or Z-lengthening of the rectus femoris that has been reported to improve intraoperative flexion.[20],[32] In addition, the arthroscopic release could not be performed, as reported in the literature.[7],[24] Open release was opted to separate the patella as it was completely adherent to the femur with dense fibrous tissue.
One of the challenges, in this case, was that there was no cartilage left on the patella articular surface to restore the smooth gliding movement, which raised concerns regarding patellofemoral pain, impingement, and re-stiffness. The outcome of follow-up showed excellent adaptation of the patella leading to painless and acceptable knee flexion.
Another challenge was that the patient was operated 21 months post the traumatic surgery. In earlier studies, it was mentioned that the critical factor affecting knee ROM improvement is the time interval between the surgical release and the beginning of the inflammatory contracture process.[7],[34],[35] Three to nine months was the preferred time. Less successful results were encountered when the surgical release was performed one year or more after the start of the process.[7],[10],[13],[34],[35] On the other hand, the extension lag varied from 8°–52°, and that was attributed to the weakness of the rectus femoris after separation from the vasti. Extension lag was reduced and had gradual improvement of extension power with quadriceps physical therapy.[3],[4],[18],[19],[22],[23],[26],[31]
The literature was reviewed to answer the question: Is Thompson's quadricepsplasty an excellent technique to treat knee extension contracture? and for that, the PubMed search was conducted using the keywords: Extension contracture, knee contracture, knee stiffness, which were subsequently matched with search terms: Quadricepsplasty, Thompson's quadricepsplasty, modified Thompson's quadricepsplasty. The review inclusion criteria included: (1) Published articles, which were written only in English for all available years, (2) Randomized-controlled trials, longitudinal cohort and retrospective studies, (3) Assessment of surgical results of Thompson's quadricepsplasty in patients with posttraumatic knee contractures. Exclusion criteria included: (1) Results of other techniques of quadricepsplasty, (2) Study population with the majority being pediatric patients. The search result was 147 articles. The articles were scanned by the titles and the public abstracts to exclude the nonrelevant articles; the result was 39 articles. After the exclusion of the duplicated articles, the search ended with 16 studies, with a total of 332 patients. The relevant data was summarized in [Table - 3] and [Table - 4].
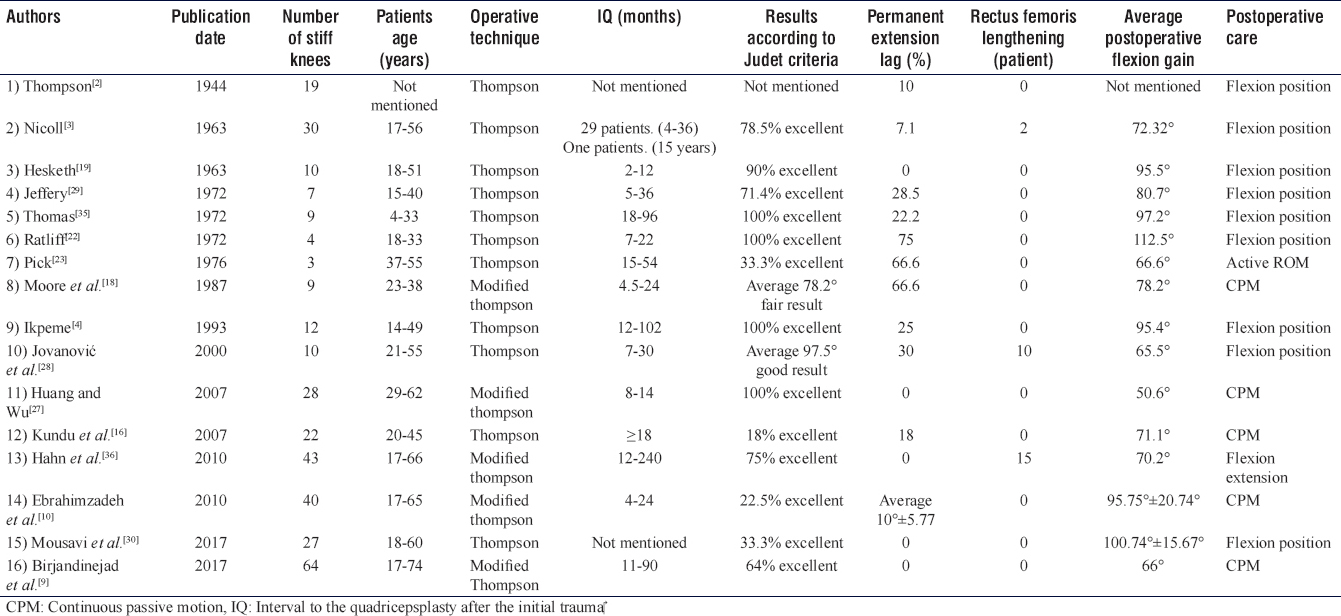
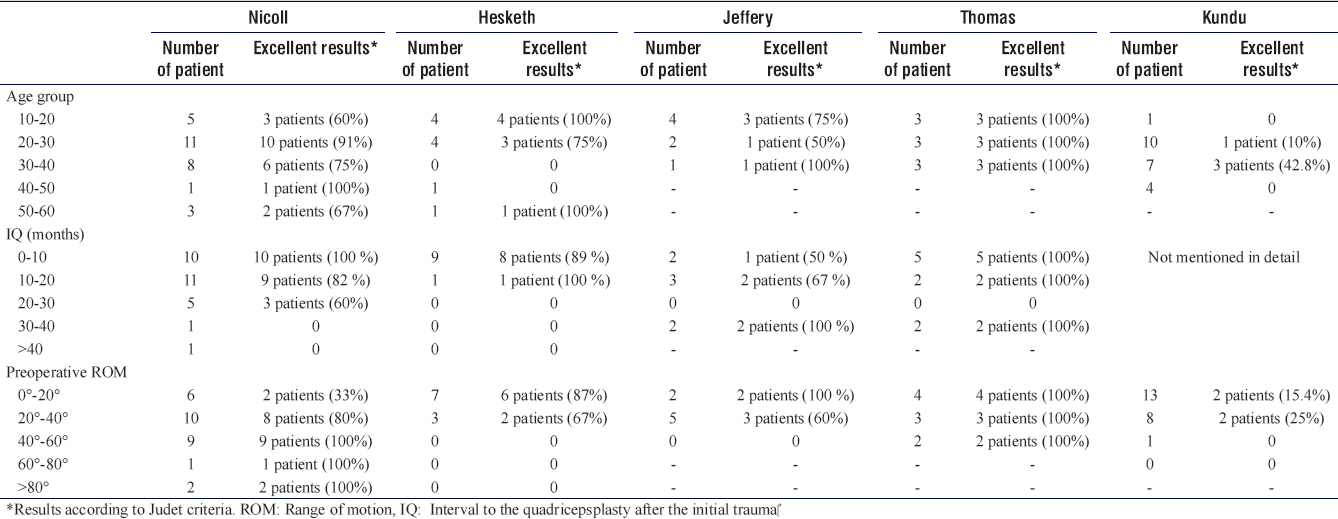
When reviewing the data from the papers, the author noticed that the age of the patients did not correlate to the result,[3],[4],[9],[10],[19],[22],[23],[27],[29],[33],[36] while there was a reverse association between the final flexion gain and the preoperative ROM.[3],[9],[10],[19],[29],[33],[36] Some of the results revealed that intraoperative ROM could be the vital defining element for the final improvement of the flexion.[10],[36] In addition, the IQ was found to play an influential role in the results,[4],[9],[10],[19],[22],[23],[27],[29],[36] and a better flexion was achieved when quadricepsplasty was performed in the the first six to ten months after the last surgery.[3],[9],[10] As a factor may correlate to this result, recently, immediate postoperative CPM was preferred over the knee immobilization in flexion position, and it was used in the current case.[9],[10],[16],[18],[27]
On the other hand, in other studies, the effect of the patient's age, IQ, and preoperative ROM on the clinical outcome in some papers was not clear because the patients' data were not individualized in the study and the final ROM for every patient was not documented.[16],[18],[28],[30]
Birjandinejad et al.[9] had the largest number of patients in their study, which allowed them to evaluate other variables not tackled in the studies before them, such as BMI, gender, and the surgical approach. They noticed that the final flexion was considerably higher in the patient with normal BMI in comparison with overweight patients, and the gender and the surgical approach (midline vs. anterolateral) had not significantly influenced the results.
Several authors noticed that a mild extension lag might persist for several weeks postoperatively, but can usually be improved with physical therapy and it takes up to a year to regain full active extension of the knee. They were reluctant to lengthen the rectus femoris tendon because it always leads to permanent loss of active extension.[18],[19],[29],[36]
Many modifications to Thompson's quadricepsplasty were reported.[9],[10],[18],[27],[33] Single medial or combined medial and lateral parapatellar incisions were described.[18],[33] A number of authors utilized an anterior longitudinal incision with a longitudinal division of the quadriceps tendon.[9],[10],[27] This approach was also used for implant removal and the release in the patients who suffered from knee contracture after patella fracture fixation.[27] Division of tensor fascia lata transversely in the distal thigh with preservation of the vastus medialis insertion to the patella was also reported; it could prevent permanent extension lag even with the high percentage of the rectus femoris tendon lengthening.[33] It was reported that vastus intermedius never excised, even when it was found scarred and fibrosed because the excision could increase the likelihood of further adhesions.[9],[10]
In the current case, some modifications of Thompson's quadricepsplasty were utilized, an anterolateral incision was used through the scar of previous surgery. The vastus intermedius was excised, the tensor fascia lata was kept intact, and lengthening the rectus femoris was not performed.
Conclusion
Modified Thompson's quadricepsplasty is an effective procedure with satisfactory results and a high success rate in severe extension contracture with few complications. The definitive flexion gain did not correlate with the patient's age, gender, or the approach (midline vs. anterolateral); it was inversely related to the interval between the initial injury and the quadricepsplasty, the preoperative ROM and patient body mass index. The postoperative physiotherapy is an essential part of the management not only in achieving maximum flexion but also in resuming active extension. The preoperative extension lag is less likely to improve substantially. The postoperative extension lag, which is not a result of tendon lengthening, eventually improves with vigorous regular exercises and often takes one year. Rectus femoris lengthening should be avoided when possible because it leads to permanent extension lag.
Declaration of patient consent
The author certifies that he has obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published, and outstanding efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
| 1. | Warner JJ. The Judet quadricepsplasty for management of severe posttraumatic extension contracture of the knee. A report of a bilateral case and review of the literature. Clin Orthop Relat Res 1990;256:169-73. [Google Scholar] |
| 2. | Thompson TC. Quadricepsplasty to improve knee function. J Bone Joint Surg 1944;26:366-79. [Google Scholar] |
| 3. | Nicoll EA. Quadricepsplasty. J Bone Joint Surg Br 1963;45:483-90. [Google Scholar] |
| 4. | Ikpeme JO. Quadricepsplasty following femoral shaft fractures. Injury 1993;24:104-8. [Google Scholar] |
| 5. | Rowe PJ, Myles CM, Walker C, Nutton R. Knee joint kinematics in gait and other functional activities measured using flexible electrogoniometry: How much knee motion is sufficient for normal daily life? Gait Posture 2000;12:143-55. [Google Scholar] |
| 6. | Kettelkamp DB, Johnson RJ, Smidt GL, Chao EY, Walker M. An electrogoniometric study of knee motion in normal gait. J Bone Joint Surg Am 1970;52:775-90. [Google Scholar] |
| 7. | Dhillon MS, Panday AK, Aggarwal S, Nagi ON. Extra articular arthroscopic release in post-traumatic stiff knees: A prospective study of endoscopic quadriceps and patellar release. Acta Orthop Belg 2005;71:197-203. [Google Scholar] |
| 8. | Ali AM, Villafuerte J, Hashmi M, Saleh M. Judet's quadricepsplasty, surgical technique, and results in limb reconstruction. Clin Orthop Relat Res 2003;415:214-20. [Google Scholar] |
| 9. | Birjandinejad A, Mohammad H. Ebrahimzadeh MH, Sayyed-Hosseinian SH, Tabesh S, Ghanbarifard M. Prognostic factors affecting the results of modified thompson quadricepsplasty for the treatment of extension contracture of the knee. Arch Bone J Surg 2017;5:109-13. [Google Scholar] |
| 10. | Ebrahimzadeh MH, Birjandi-Nejad A, Ghorbani S, Khorasani MR. A modified Thompson quadricepsplasty for extension contracture resulting from femoral and periarticular knee fractures. J Trauma 2010;68:1471-5. [Google Scholar] |
| 11. | Mira AJ, Markley K, Greer RB 3rd. A critical analysis of quadriceps function after femoral shaft fracture in adults. J Bone Joint Surg Am 1980;62:61-7. [Google Scholar] |
| 12. | Mariani PP, Santori N, Rovere P, Della Rocca C, Adriani E. Histological and structural study of the adhesive tissue in knee fiE. Histologi: A clinical-pathological correlation. Arthroscopy 1997;13:313-8. [Google Scholar] |
| 13. | Bennett GE, George E. Lengthening of the quadriceps tendon. J Bone Joint Surg 1922;4:279-316. [Google Scholar] |
| 14. | Judet R. Mobilisation of the stiff knee. J Bone Joint Surg 1959;41-B: 856-7. [Google Scholar] |
| 15. | Shelbourne KD, Patel DV, Martini DJ. Classification and management of arthrofibrosis of the knee after anterior cruciate ligament reconstruction. Am J Sports Med 1996;24:857-62. [Google Scholar] |
| 16. | Kundu Z, Sangwan S, Guliani G, Siwach R, Kamboj P, Singh R. Thompson's quadricepsplasty for stiff knee. Indian J Orthop 2007;41:390-4. [Google Scholar] |
| 17. | Pujol N, Boisrenoult P, Beaufils P. Post-traumatic knee stiffness: Surgical techniques. Orthop Traumatol Surg Res 2015;101 Suppl 1:S179-86. [Google Scholar] |
| 18. | Moore TJ, Harwin C, Green SA, Garland DE, Chandler RW. The results of quadricepsplasty on knee motion following femoral fractures. J Trauma 1987;27:49-51. [Google Scholar] |
| 19. | Hesketh KT. Experience with the Thompson quadricepsplasty. J Bone Joint Surg 1963;45-B: 491-5. [Google Scholar] |
| 20. | Hosalkar HS, Jones S, Chowdhury M, Hartley J, Hill RA. Quadricepsplasty for knee stiffness after femoral lengthening in congenital short femur. J Bone Joint Surg Br 2003;85:261-4. [Google Scholar] |
| 21. | Oliveira VG, D'Elia LF, Tirico LE, Gobbi RG, Pecora JR, Camanho GL, et al. Judet quadricepsplasty in the treatment of post-traumatic knee rigidity: Long-term outcomes of 45 cases. J Trauma Acute Care Surg 2012;72:E77-80. [Google Scholar] |
| 22. | Ratliff AH. Quadricepsplasty. Injury 1972;4:126-30. [Google Scholar] |
| 23. | Pick RY. Quadricepsplasty: A review, case presentations, and discussion. Clin Orthop Relat Res 1976;120:138-42. [Google Scholar] |
| 24. | Wang JH, Zhao JZ, He YH. A new treatment strategy for severe arthrofibrosis of the knee. A review of twenty-two cases. J Bone Joint Surg Am 2006;88:1245-50. [Google Scholar] |
| 25. | Whang KS, Park KC, Kim KS. Results of Judet quadricepsplasty in knee stiffness. J Korean Fracture Soc 2000;13:96-102. [Google Scholar] |
| 26. | Merchan EC, Myong C. Quadricepsplasty: The Judet technique and results of 21 post-traumatic cases. Orthopaedics 1992;9:1081-5. [Google Scholar] |
| 27. | Huang YC, Wu CC. Modified Thompson quadricepsplasty to treat extension contracture of the knee after surgical treatment of patellar fractures. Chang Gung Med J 2007;30:263-9. [Google Scholar] |
| 28. | Jovanović S, Orlić D, Wertheimer B, Zelić Z, Has B. Quadricepsplasty after war fractures. Mil Med 2000;165:263-7. [Google Scholar] |
| 29. | Jeffery CC. Quadricepsplasty. Injury 1972;4:131-6. [Google Scholar] |
| 30. | Mousavi H, Mir B, Safaei A. Evaluation of Thompson's quadricepsplasty results in patients with knee stiffness resulted from femoral fracture. J Res Med Sci 2017;22:50. [Google Scholar] |
| 31. | Ebraheim NA, DeTroye RJ, Saddemi SR. Results of Judet quadricepsplasty. J Orthop Trauma 1993;7:327-30. [Google Scholar] |
| 32. | Hahn SB, Lee WS, Han DY. A modified Thompson quadricepsplasty for the stiff knee. J Bone Joint Surg Br 2000;82:992-5. [Google Scholar] |
| 33. | Lindenfeld TN, Wojtys EM, Husain A. Operative treatment of arthrofibrosis of the knee. Inst Course Lecture 2000;49:211-21. [Google Scholar] |
| 34. | Lindenfeld TN, Bach BR Jr., Wojtys EM. Reflex sympathetic dystrophy and pain dysfunction in the lower extremity. Instr Course Lect 1997;46:261-8. [Google Scholar] |
| 35. | Thomas FB. Quadricepsplasty. Injury 1972;4:137. [Google Scholar] |
| 36. | Hahn SB, Choi YR, Kang HJ, Lee SH. Prognostic factors and long-term outcomes following a modified Thompson's quadricepsplasty for severely stiff knees. J Bone Joint Surg Br 2010;92:217-21. [Google Scholar] |
Fulltext Views
4,956
PDF downloads
2,060





