Translate this page into:
Ilioinguinal approach versus modified Stoppa approach and lateral window for management of high anterior column fracture
*Corresponding author: Abdelrahman Nabil Nada, Department of Orthopedics, Ain Shams University, Cairo, Egypt. abdelrahmanabil92@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sallam Masoud AM, Hassan E, Nada AN, Nagy AM, Moussa IS. Ilioinguinal approach versus modified Stoppa approach and lateral window for management of high anterior column fracture. J Musculoskelet Surg Res. 2024;8:359-67. doi: 10.25259/JMSR_225_2024
Abstract
Objectives:
The objective of this study was to compare the Ilioinguinal approach and the modified Stoppa approach regarding clinical and radiological outcomes.
Methods:
This prospective randomized controlled study involved 30 patients who were split into two groups.
Results:
There was no significant difference regarding the clinical and radiological outcomes and residual medial wall displacement. Blood loss during the operation was less in the modified Stoppa approach.
Conclusion:
When treating anterior column fractures, the modified Stoppa approach reduces blood loss and expedites surgery compared to the Ilioinguinal approach. The study’s original hypothesis has been validated, indicating that the modified Stoppa approach is a superior alternative for managing these fractures.
Keywords
Acetabular fracture
Anterior column
Ilioinguinal approach
Lateral window
Modified Stoppa approach
INTRODUCTION
The acetabular fractures are one of the hardest fractures in orthopedic surgery. There is a connection between reduction and treatment effectiveness.[1] To optimize the outcome of reduction and fixation, the best surgical technique should be used, one that emphasizes anatomical structures. When selecting a method, it is important to accurately determine the kind of fracture.[2] The chosen approach should enable anatomical reduction, allow for sufficient accessibility of the fracture, and allow for the reduction of the fracture. For many years, the ilioinguinal approaches have been utilized regularly. However, its effectiveness in treating anterior acetabular fractures has been demonstrated by numerous investigations (mostly anterior wall and column, anterior column with posterior hemitransverse fractures).[3] However, because the femoral nerve and external iliac arteries are so close to the operative plane, there is a risk to these vital neurovascular systems during this prolonged exposure.[4] Hirvensalo et al.[5] characterized the rectus abdominis muscle as the extraperitoneal (“Stoppa”) pathway as a substitute approach for treating acetabulum fractures in 1993. This approach keeps the fracture site completely isolated from the peritoneal sac, providing a single-window view of the operational field.[6] The purpose of this randomized controlled experiment is to evaluate the management of anterior acetabular fractures using the modified Stoppa and ilioinguinal approaches. Since there is currently a dearth of information on the care of these sorts of acetabular fractures, our research question is if the less invasive modified Stoppa approach and lateral window are as beneficial at a shorter follow-up duration as the extensile ilioinguinal approach regarding clinical and radiological outcomes.
In the present study, we treat high anterior column acetabular fractures by prospectively comparing radiological and clinical outcomes using the ilioinguinal approach versus the modified Stoppa approach and lateral window, encompassing the transverse anterior and posterior hemispheres as well as the related two-column fractures.
The main goal of this study was to compare the effect of the two approaches on clinical and radiological results; implant failure, residual medial wall displacement, and loss of reduction are the main goals. The secondary goals include post-operative problems, operating time, and blood loss.
MATERIALS AND METHODS
We conducted this investigation prospectively on 30 patients with high anterior column fracture (transverse acetabular fracture and both column fractures) after obtaining approval from the patients’ signed informed consent and the Hospital Research/Ethics Committee. To screen all patients for enrollment, we conducted a thorough clinical assessment of each patient’s medical history, a physical examination, and radiographic examinations – such as pelvic computed tomography scans and routine radiographs with anteroposterior and Judet views (obturator and iliac views).
The study’s inclusion criteria included acetabular fractures with high anterior column fractures, such as transverse acetabular fractures, both column fractures and age groups between 16 and 60 years old. The type of acetabular fractures (transverse or both column fractures) was not comparable between the patients included in our study.
The study excluded fractures presenting after three weeks of injury, pathological fractures, open fractures, low transverse acetabular fractures, associated urogenital or visceral injuries, and isolated posterior column fractures.
Statistical analysis
The Statistical Package for the Social Science (Rstudio) 2.3.2 version was utilized to input, code, and modify the data. The mean, standard deviations, and ranges were provided for the quantitative data with a parametric distribution; numbers and percentages were provided for the qualitative data; and the median with interquartile range was provided for the quantitative data with a non-parametric distribution. The Shapiro–Watson test was used to determine whether quantitative data were normal. With qualitative data, two groups were compared using the Chi-square test. Fisher’s exact test was used instead of the expected count in any cell, which was <5. When comparing two groups with quantitative data and a parametric distribution, the independent t-test was employed; when comparing two groups with quantitative data and a non-parametric distribution, the Wilcoxon Mann–Whitney test was utilized. A 95% confidence interval and a 5% allowable margin of error were established.
This study was prospectively conducted on 36 patients with high anterior column acetabular fractures that met our inclusion criteria. The independent doctor allocated the 36 cases to two groups: Group A (18 cases) fixed through the ilioinguinal approach and Group B (18 cases) fixed through the modified Stoppa approach. However, records were complete in 30 patients (83.3%) in the prospective analysis, of which six were lost at follow-up [Figure 1].

- Consolidated standards of reporting trails (CONSORT) flow diagram of the study groups.
Patients in our study were followed up for periods ranging from 12 to 24 months, and the mean length of follow-up was (18 ± 4) months. Patients were evaluated at two weeks, six weeks, three months, six months, and one year postoperatively. Matta radiological principles were used to assess radiological outcomes through plain radiographs showing both hips through anteroposterior Judet views after one year of follow-up. In addition, the clinical assessment was evaluated by a modified Merle d’Aubigné-Postel score at each follow-up visit, and the final clinical assessment was done after one year.
Surgical approach
Two surgeons with similar experience in pelvic surgery have performed all of the surgeries. Every procedure was carried out while the patient was supine decubitus, and they were catheterized to maintain an empty bladder to reduce the risk of infection and monitor the occurrence of hematuria.
Ilioinguinal approach
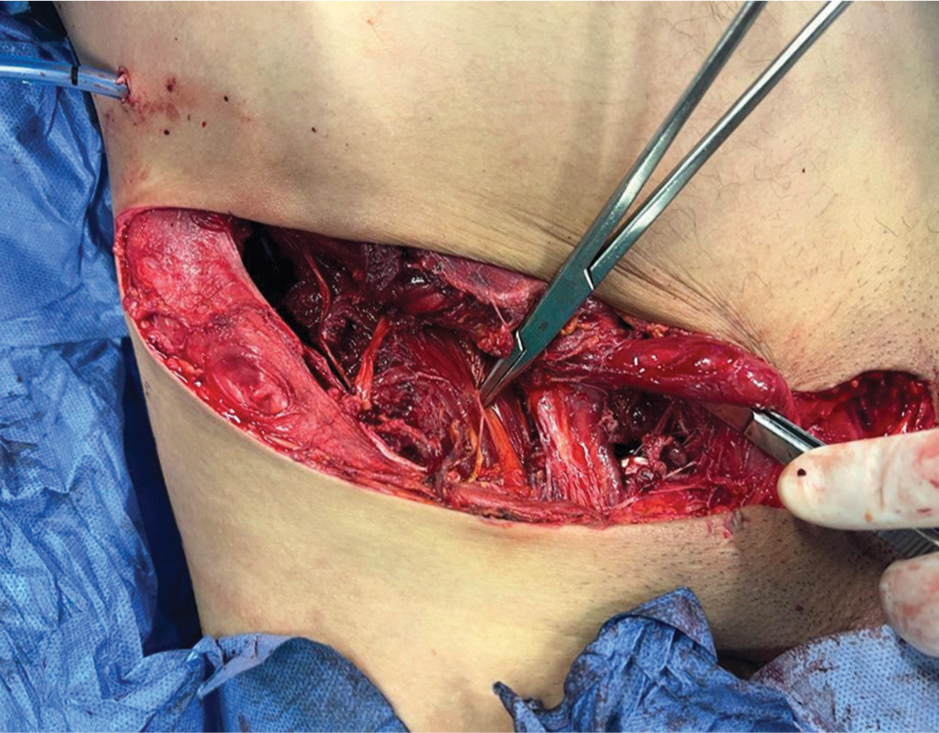
A significant amount of skin and soft-tissue exposure is part of the ilioinguinal approach. The skin incision reaches symphyses pubis from the posterior region of the iliac crest [Figure 2].

- The skin incision of the ilioinguinal approach from the posterior part of the iliac crest to the symphysis pubis anterior.
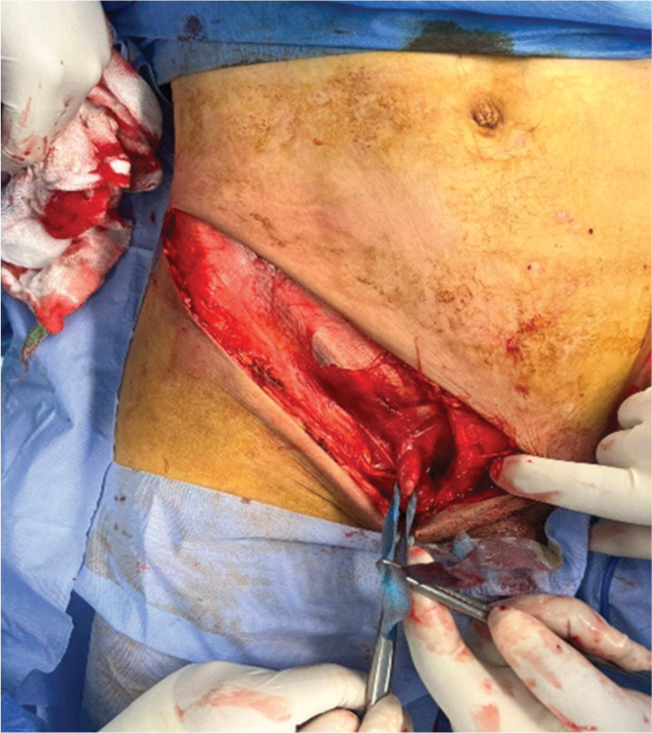
The inguinal ligament is severed when the oblique external muscle’s aponeurosis has been located. Three distinct windows can be identified on the deep plane. Located at the level of the iliac fossa, the lateral window provides a wide view of the fossa and is commonly used to reduce iliac displacement fractures. It must identify the specific lateral femoral cutaneous nerve [Figure 3].
- The ileo-psoas muscle with the femoral nerve.
The middle window is located after separating the psoas muscle and the adjacent femoral nerve. This portal allows access to the quadrilateral surface, part of the posterior column, and the real pelvis [Figure 4].
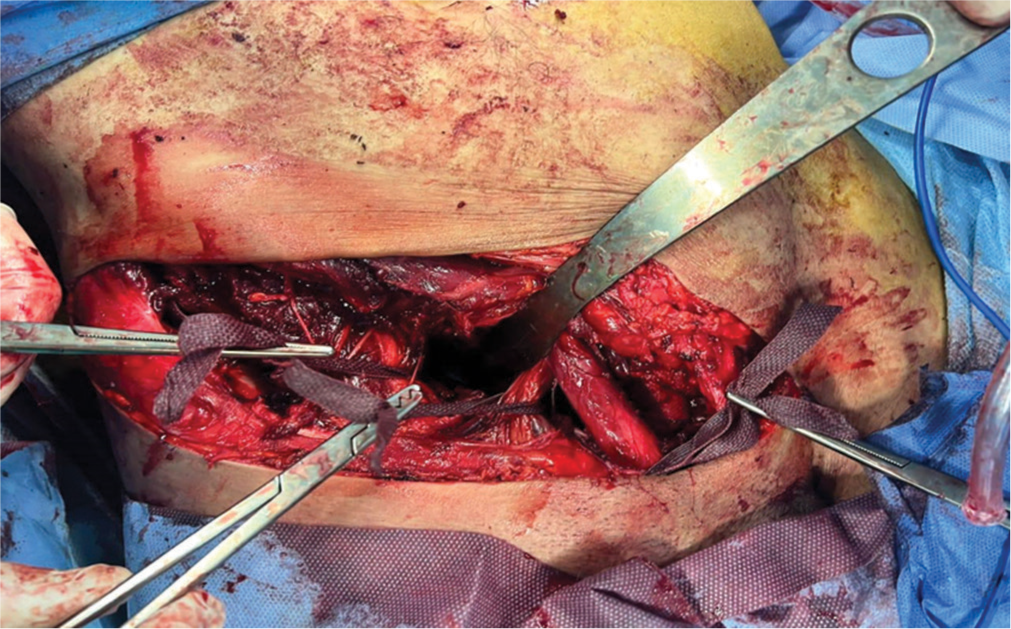
- The middle window between the ileo-psoas muscle, with the femoral nerve laterally and the external iliac vessels medially.
The pubic bones are accessible through the medial window, which develops between the external iliac arteries and the spermatic cord. In addition, it aids in plate medial side stabilization. It is also feasible to empty huge hematomas that often collect in this area and observe the bladder clearly through this incision [Figure 5].
- The spermatic cord identification.
Modified Stoppa approach
A Pfannenstiel-style horizontal incision is often the foundation of the modified Stoppa approach. The rectus abdominal muscles are seen during the superficial dissection. To get sufficient and prompt exposure of the bladder, true pelvis, and pubic ramus, it is important to make a vertical incision along the linea alba in the rectus fascia. For example, setting an infrapectineal plate requires the isolation of the obturator nerve to obtain a wide visualization of the quadrilateral plate. The corona mortis, which is situated 5–7 cm lateral to the pubic symphysis, must be promptly identified and ligated or cauterized. This is the most crucial phase in the surgery. This access does not allow the exposure of posterior column fractures. However, indirect reduction and fixation of posterior wall fracture can be obtained through this approach [Figure 6].
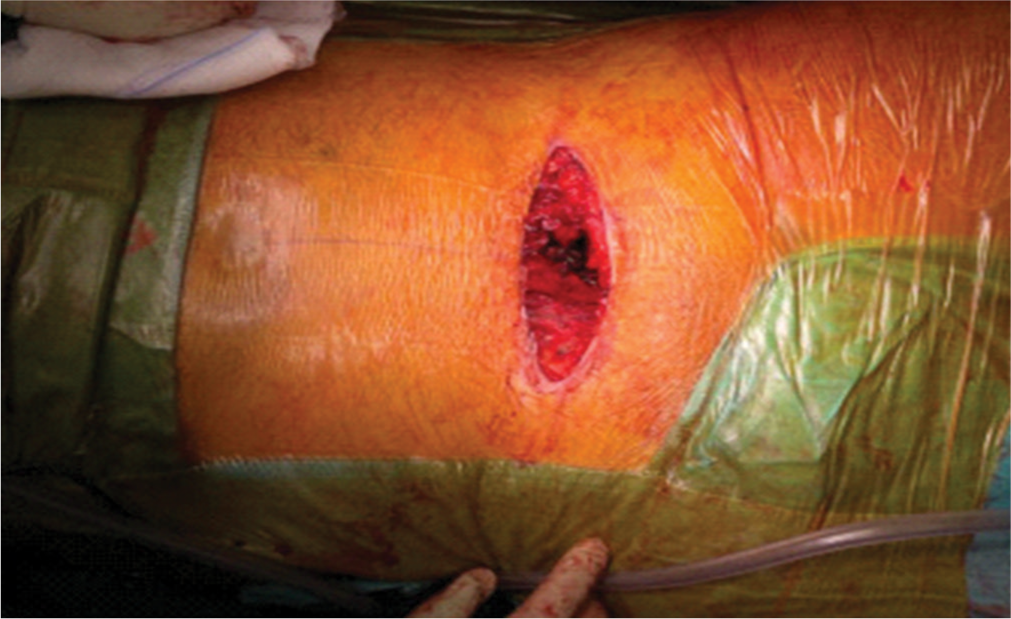
- The modified Stoppa approach.
RESULTS
The modified Merle d’Aubigné-Postel score has been used to evaluate clinical and functional outcomes. The following scores are found on the modified Merle d’Aubigné-Postel score: <7 points (poor), 11–14 points (acceptable), and 15–18 points (outstanding).
An orthopedic surgeon has evaluated the quality of reduction using Hammad[7] criteria while remaining blind to the procedure. These results were calculated after one year of follow-up. These measures evaluate the reduction in the residual displacement of the analyzed fragments:
0–1 mm is the anatomic reduction
Good reduction: residual displacement of 2–3 mm
Inadequate reduction: residual displacement <3 mm. Medical data from the time of admission till the follow-up have been examined for post-operative complications. We have thought about:
Nerve-related issues
Deep and superficial infectious problems
Vascular complications
One or more grave complications
As regards the demographic characters, the age ranged between (22 and 7) years with mean ± standard deviation (SD) (34.7 ± 9.4) years in Group A while ranged between (16 and 60) years with mean ± SD (35.2 ± 10.3) years in Group B with no statistically significant difference between two studied groups at (P = 0.898). The majority of patients were male (93.3%) in Group A and (66.7%) in Group B, with no statistically significant difference between males and females regarding the studied groups at (P = 0.169) [Table 1].
| Group A (n=15) | Group B (n=15) | P-value | |
|---|---|---|---|
| Age in years | |||
| Min.–Max. | 22–57 | 16–60 | 0.898 |
| Mean±SD | 34.7±9.4 | 35.2±10.3 | |
| Sex (%) | |||
| Female | 1 (6.7) | 5 (33.3) | 0.169 |
| Male | 14 (93.3) | 10 (66.7) |
SD: Standard deviation
Regarding the comparing clinical outcomes between two studied groups based on the modified Merle d’AubignéPostel score mentioned as follows:
Excellent: Group A has 4 participants (26.7%), while Group B has 3 participants (20.0%).
Fair: Group A has 5 participants (33.3%), while Group B has 2 participants (13.3%).
Good: Group A has 6 participants (40.0%), while Group B has 9 participants (60.0%).
Poor: Group A has 0 participants (0.0%), while Group B has 1 participant (6.7%).
There was no statistically significant difference in the clinical outcomes (modified Merle d’Aubigné-Postel score) between the two research groups (P = 0.494) [Table 2].
| Clinical outcomes modified Merle d’Aubigné-Postel score | Group A (n=15) (%) | Group B (n=15) (%) | P-value |
|---|---|---|---|
| Excellent | 4 (26.7) | 3 (20.0) | 0.494 |
| Fair | 5 (33.3) | 2 (13.3) | |
| Good | 6 (40.0) | 9 (60.0) | |
| Poor | 0 (0.0) | 1 (6.7) |
Regarding comparing the radiological outcome between the two groups based on the Matta radiological acetabular scoring system, as follows:
Excellent: Group A has 6 participants (40%), while Group B has 4 participants (26.7%).
Fair: Group A has 3 participants (20%), while Group B has 3 participants (20%).
Good: Group A has 6 participants (40.0%), while Group B has 8 participants (53.3%).
There was no statistically significant difference in radiological outcomes (Matta radiological acetabular scoring system) across the two groups at (P = 0.889) [Table 3].
| Radiological outcome Matta radiological acetabular scoring system | Group A (n=15) (%) | Group B (n=15) (%) | P-value |
|---|---|---|---|
| Excellent | 6 (40.0) | 4 (26.7) | 0.889 |
| Fair | 3 (20.0) | 3 (20.0) | |
| Good | 6 (40.0) | 8 (53.3) |
According to the comparison of the operative time, the time ranged between (1 and 3) h with a median of 2 h in Group A. However, the time ranged between (1 and 2) h, with a median of 1.5 h in Group A. Compared to Group A, there was a significant drop-in time in Group B at (P = 0.007) [Table 4].
| Operative time (hours) | Group A (n=15) | Group B (n=15) | P-value |
|---|---|---|---|
| Min.–Max. | 1–3 h | 1–2 h | 0.007 |
| Mean±SD | 2.1±0.5 | 1.6±0.4 | |
| Median | 2.0 (2.0–2.0) | 1.5 (1.5–2.0) |
SD: Standard deviation
As regards comparing the amount of blood loss during the operation in both studied groups, the blood loss volume ranged between (1000 and 3000) mL with mean ± SD (1966.7 ± 611.4) mL in Group A. However, in Group B, the blood loss volume ranged between (500 and 2000) mL with mean ± SD (1133.3 ± 441.9) mL. There was a significant decrease in blood loss volume in Group B compared to Group A at (P = 0.001) [Table 5].
| Blood loss (mL) | Group A (n=15) | Group B (n=15) | P-value |
|---|---|---|---|
| Min.–Max. | 1000–3000 mL | 500–2000 mL | 0.001 |
| Mean±SD | 1966.7±611.4 | 1133.3±441.9 | |
| Median | 2000 (1500–2250) | 1000 (1000–1250) |
SD: Standard deviation
Among 30 patients, 6 patients (40%) showed complicated symptoms in Group A, while 4 patients (26.7%) showed complicated symptoms in Group B with no difference between the two groups regarding complications diagnosed at (P = 0.699) [Table 6].
| Complication | Group A (n=15) (%) | Group B (n=15) (%) | P-value |
|---|---|---|---|
| Complicated | 6 (40.0) | 4 (26.7) | 0.699 |
| No complication | 9 (60.0) | 11 (73.3) |
Regarding the comparing residual medial wall displacement between the two studied groups, the following:
Anatomical: Group A has 6 participants (40.0%), while Group B has 4 participants (26.7%).
Good: Group A has 7 participants (46.7%), while Group B has 8 participants (53.3%).
Unsatisfactory: Group A has 2 participants (13.3%), while Group B has 3 participants (20.0%).
No statistically significant difference between the two groups regarding residual medial wall displacement is shown in Table 7 (P = 0.791).
| Residual medial wall displacement | Group A (n=15) (%) | Group (II) (n=15) (%) | P-value |
|---|---|---|---|
| Anatomical | 6 (40.0) | 4 (26.7) | 0.791 |
| Good | 7 (46.7) | 8 (53.3) | |
| Unsatisfactory | 2 (13.3) | 3 (20.0) |
DISCUSSION
Treatment for acetabular fractures is difficult due to the complex pelvic anatomy, accessibility issues, and the fractures near closeness to the hip joint. Returning to pre-injury functional activity is rare after these fractures due to a number of factors that are reported to affect the outcome.[8]
The majority of the fractures in both columns, as well as the anterior acetabular fractures, which comprise T-type fractures, anterior wall fractures, anterior column fractures, and anterior column with posterior hemi transverse fractures, were primarily fixed using the ilioinguinal approach.[3] Indirect reduction procedures are usually required depending on the view and assessment of the fracture.[9] Stoppa published a midline method for inguinal repair in 1989. Using this method, he observed a superb exposure of the real pelvis. The advantage of employing this method for acetabular fracture fixation was thus created.[6]
Therefore, the question under review was whether the modified Stoppa approach ensures a lower rate of intra- and perioperative problems while still permitting an appropriate surgical gesture. Therefore, we conducted a prospective comparison between a group of patients (Group A), as a case in Figure 7, who underwent the ilioinguinal approach and a case–control group (Group B) , as a case in Figure 8, who received treatment using the modified Stoppa approach.
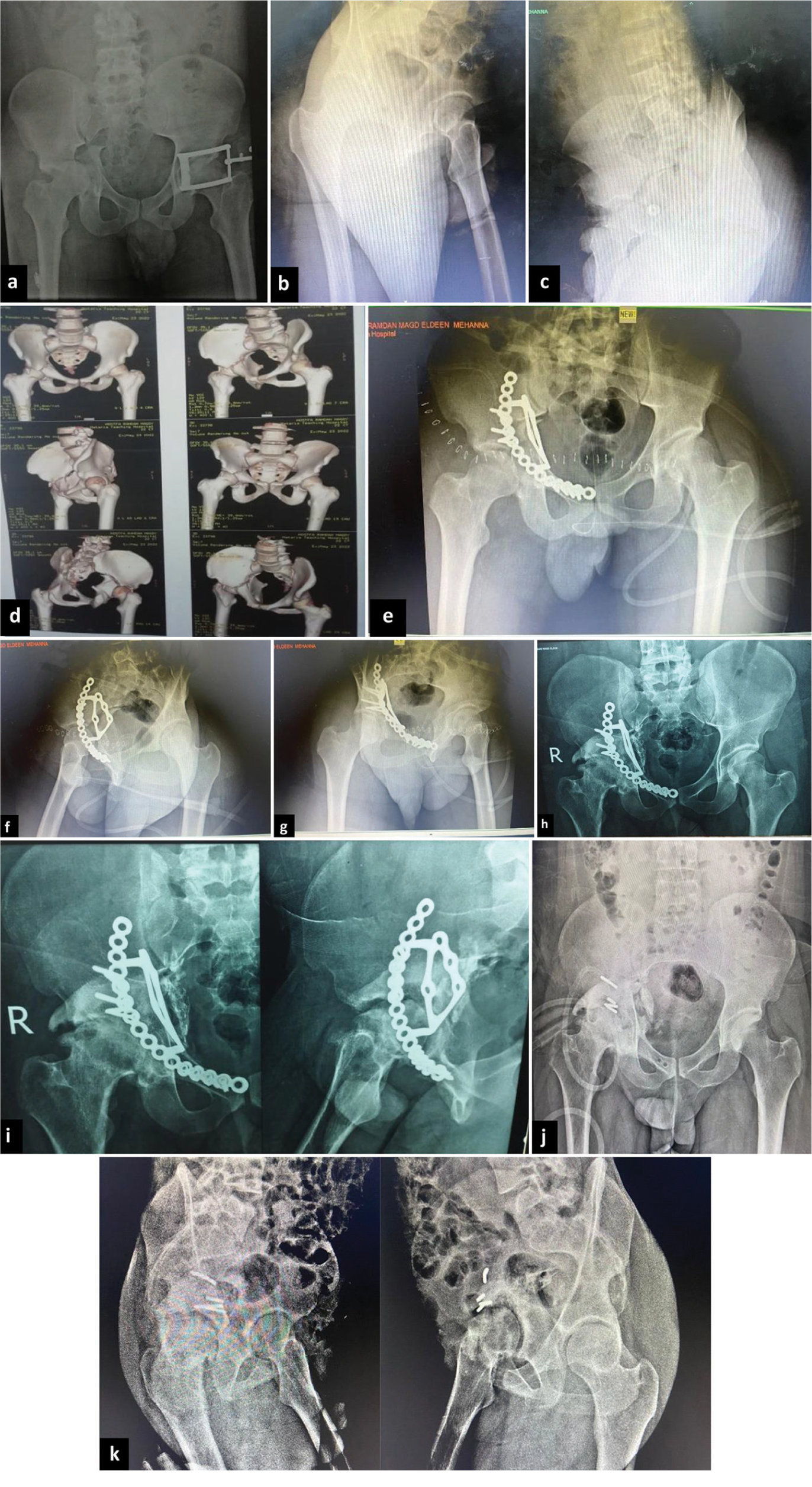
- A 22-year-old male patient, after road traffic accident, (a-d) computed tomography image and pre-operative radiographs demonstrating acetabular transverse fracture, (e-g) post-operative radiographs showing fixation through ilioinguinal approach, (h and i) radiographs 12 months postoperatively, and (j and k) radiographs after removal of plate 14 months postoperatively due to infection.
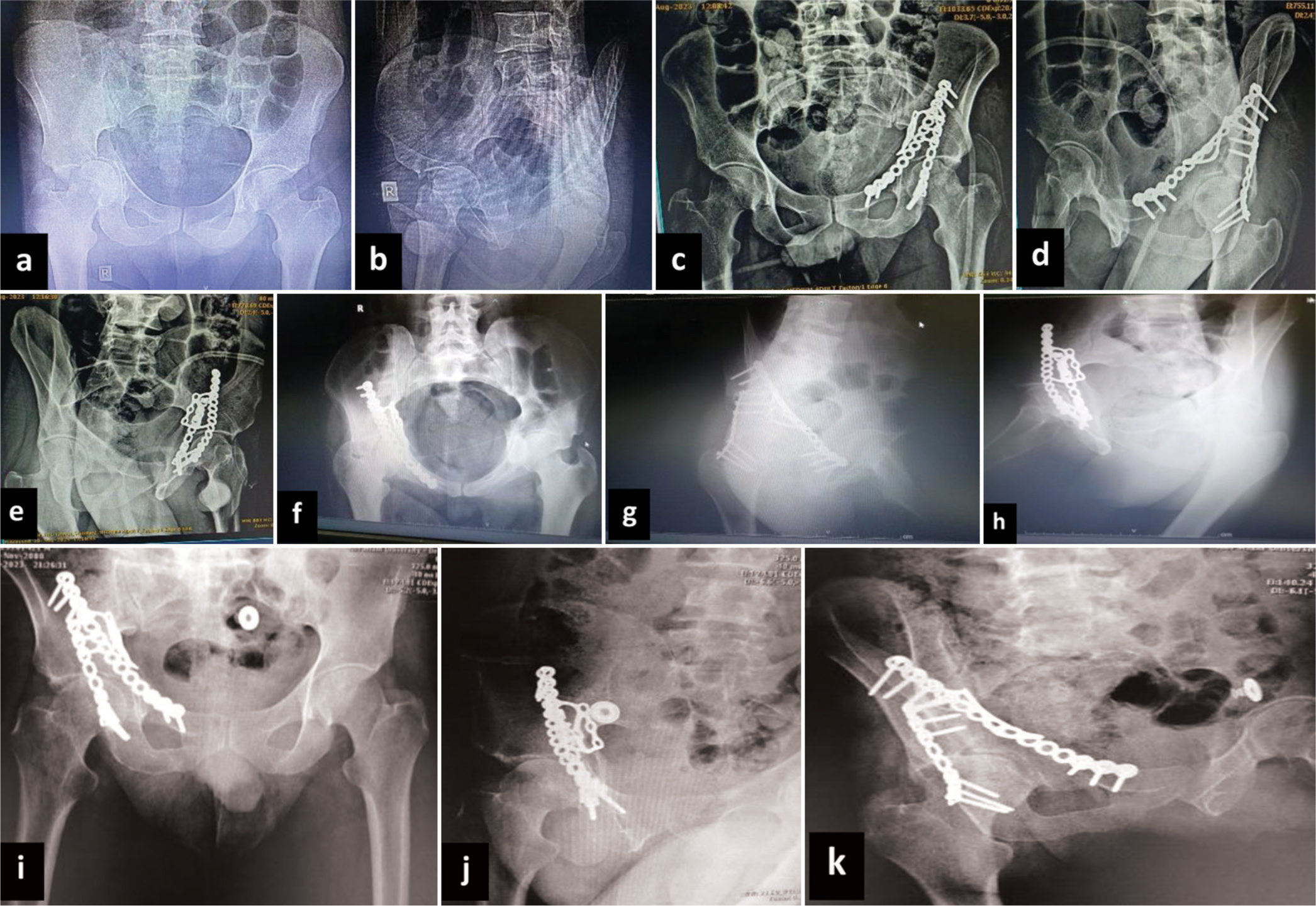
- A 35-year-old male patient, after road traffic accident, (a and b) pre-operative radiographs demonstrating acetabular transverse fracture, (c-e) post-operative radiographs showing fixation through modified Stoppa approach, (f-h) radiographs 6 months postoperatively, and (i-k) radiographs 12 months postoperatively.
Many factors were considered, such as the extent of fracture reduction, length of the treatment, bleeding, frequency of problems with the vascular and neurological systems, infection, both superficial and deep, and functional recovery as measured by assessment scales.
Numerous studies have looked into whether one surgical approach may be better than another in the literature. When Taller et al. examined these two methods in 2010,[10] they found that the modified Stoppa approach was less intrusive and guaranteed to result in a reduced incidence of peripheral neuropathy. Having proven a greater incidence of fracture reduction and a decreased likelihood of complications, Fan et al. in 2012[11] corroborated these findings. According to Matta,[12] the ilioinguinal approach improves fracture reduction and is associated with a decreased incidence of heterotopic ossification as well as a quicker rate of muscle recovery. In a 2014 Injury article, Rocca et al.[13] reported that the modified Stoppa approach access improved clinical outcomes with fewer intra- and perioperative problems. However, in 2013, Kunlong Ma, Fujun Luan et. al.[14] reported findings that were entirely consistent between the two approaches.
Matta[12] assessed how fracture displacement prep affected the outcome and discovered that a 21 mm gap created an extraordinary result, with an 18 mm fracture gap producing a good result, a 17 mm gap producing a fair result, and a 23 mm gap producing a terrible result. In our investigation, the fracture gap’s impact on the final result was statistically insignificant (P = 0.889). Muscles and neurovascular structures surround the pelvis and acetabulum well. A high-impact injury is indicated by a wide fracture gap or displacement; in these cases, the protecting muscle layers are compromised, and reduction is also challenging. This study appears to have made an important discovery on the impact of fracture displacement on the final result. Prior research has been published in the literature regarding the impact of related injuries on the functional outcome.
Restoration of articular congruity with stable fixation is the most significant predictor of post-traumatic osteoarthritis in acetabular fractures. A few authors have already classified the reduction quality according to the gap or step size.[15] We found that the reduction quality had a major effect on the outcome. A poor prognosis is definitely connected with a poor-quality reduction in the weight-bearing dome of the acetabulum, even though anatomical reduction is not always linked to a favorable outcome. The accompanying cartilage damage, muscle injury, surgical morbidity, and factors outside the surgeon’s control play a major role in predicting the prognosis. A large hole or gap persists in the metaphyseal region when articular congruency is restored in comminuted or impacted marginal fractures by pulling up the impacted components. This metaphyseal malreduction is acceptable; however, the pieces bordering the articular surface must be fastened tightly due to the high fracture risk during postoperative therapy.[6,16]
According to the study, there was no statistically significant difference in clinical outcomes (modified Merle d’AubignePostel score) between the two groups that were the subject of the investigation at each follow-up visit (P = 0.494).
Pre- and post-operative serialized controls showed more blood loss in patients treated with the ilioinguinal approach, according to the study of the two groups. The mean blood loss using the modified Stoppa approach was reported to be 1133 mL (range, 500–2000 mL) compared to 1900 mL (range, 1000–3000 mL) in the ilioinguinal approach. A study by Fan et al. that comprised fractures of the pelvis and acetabulum found a mean blood loss of 320 mL (range, 100–1200 mL) using the modified Stoppa approach. Blood loss differs significantly between the modified Stoppa and ilioinguinal approach in the current investigation (P = 0.001).[11]
This study observed a statistically significant reduction in operating time (an average saving of almost half an hour) among patients with high anterior column fractures treated with the modified Stoppa approach. The average length of the procedure was 1.5 h.
After an acetabulum fracture, post-traumatic osteoarthritis is the latest consequence. According to Matta,[12] 28.8% of patients had secondary osteoarthritis. Post-traumatic arthritis was identified after more than a decade of patient follow-up for 38% of the patients. They concluded that during long-term follow-up, a growing number of patients may develop osteoarthritis despite the initial complete reduction of fracture risk. According to Matta’s analysis, the infection rate was approximately 5.01%, but the two groups’ differences in complications were not statistically significant (P = 0.699).
CONCLUSION
Compared to the ilioinguinal Approach, the modified Stoppa approach reduces blood loss and shortens surgical timeframes for treating anterior column acetabulum fractures. Positive outcomes can be achieved by utilizing the Stoppa approach in the anterior acetabulum and posterior surgery. There are no discernible changes in terms of morbidity or fracture prevention following surgery with the Stoppa approach, despite the fact that very little scarring remains.
The study’s original hypothesis has been validated, indicating that the modified Stoppa approach is a more effective treatment option for these fractures at a short follow-up in terms of shorter operation time and less blood loss.
RECOMMENDATIONS
To confirm this finding, more research with a bigger patient population and a longer follow-up focusing on the development of secondary osteoarthritis is necessary.
ACKNOWLEDGMENT
The authors would like special thank to Dr. Andrew Magdy, and I am extremely grateful and indebted to him for his expert, sincere and valuable guidance in every stage of this research paper.
AUTHORS’ CONTRIBUTIONS
AN and IM designed the study, wrote the protocol, analyzed data, reviewed the manuscript critically, and approved the final version to be published; ZH and AM analyzed the data, and reviewed the manuscript critically; AN collected data and wrote the manuscript. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The research/study approved by the Institutional Review Board at Ain Shams University, number FMASU R78/2024, dated April 7, 2023.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- The Stoppa approach versus the ilioinguinal approach for anterior acetabular fractures: A case control study assessing blood loss complications and function outcomes. Orthop Traumatol Surg Res. 2014;100:675-80.
- [CrossRef] [Google Scholar]
- Modified Stoppa approach versus ilioinguinal approach for pelvic and/or acetabular fractures: A meta-analysis. Chinese J Tissue Eng Res. 2017;21:3108-16.
- [Google Scholar]
- The treatment of acetabular fractures through the ilioinguinal approach. Clin Orthop Relat Res. 1993;292:62-76.
- [CrossRef] [Google Scholar]
- A comparison between ilioinguinal and modified Stoppa approach in anterior column acetabular fractures. Injury. 2024;55:111166.
- [CrossRef] [Google Scholar]
- Modified and new approaches for pelvic and acetabular surgery. Injury. 2007;38:431-41.
- [CrossRef] [Google Scholar]
- Modified Stoppa approach versus ilioinguinal approach for anterior acetabular fractures; a systematic review and meta-analysis. Bull Emerg Trauma. 2017;5:6-12.
- [Google Scholar]
- Accuracy of reduction and early clinical outcome un acetabular fractures treated by the standard ilio-inguinal versus the Stoppa approach. Injury. 2015;46:320-6.
- [CrossRef] [Google Scholar]
- Single modified ilioinguinal approach for the treatment of acetabular fractures involving both columns. J Orthop Trauma. 2018;32:E428-34.
- [CrossRef] [Google Scholar]
- Treatment of anterior column posterior hemitransverse fracture with supra-ilioinguinal approach. J Int Med Res. 2021;49:300060520982824.
- [CrossRef] [Google Scholar]
- Surgical treatment of pelvic ring and acetabular fractures using the Stoppa approach. Acta Orthop Cech. 2010;77:93-8.
- [CrossRef] [Google Scholar]
- Modified Stoppa approach in treatment of pelvis and acetabular fracture. Zhongguo Gu Shang. 2012;25:810-2.
- [Google Scholar]
- Operative treatment of acetabular fractures through the ilioinguinal approach: A 10-year perspective. J Orthop Trauma. 2006;20(1 Suppl):S20-9.
- [CrossRef] [Google Scholar]
- Anterior combined Endopelvic (ACE) approach for the treatment of acetabular and pelvic ring fractures: A new proposal. Injury. 2014;45(Suppl 6):S9-15.
- [CrossRef] [Google Scholar]
- Randomized, controlled trial of the modified Stoppa versus the ilioinguinal approach for acetabular fractures. Orthopedics. 2013;36:e1307-15.
- [CrossRef] [Google Scholar]
- Modified Stoppa approach for acetabular fractures with anterior and posterior column displacement: Quantification of radiographic reduction and analysis of interobserver variability. J Orthop Trauma. 2010;24:271-8.
- [CrossRef] [Google Scholar]
- The Stoppa combined with iliac fossa approach for the treatment of both-column acetabular fractures. J Orthop Surg Res. 2020;15:588.
- [CrossRef] [Google Scholar]







