Translate this page into:
Incidence and predictors of 30-day postoperative complications following musculoskeletal tumor surgery
2 College of Medicine, King Saud Bin Abdulaziz University for Health Sciences; King Abdullah International Medical Research Center, Riyadh, Saudi Arabia
3 King Abdullah International Medical Research Center; College of Medicine, Almareefa University, Riyadh, Saudi Arabia
4 King Abdullah International Medical Research Center, Riyadh; College of Medicine, King Faisal University, Al-Ahsa, Saudi Arabia
Corresponding Author:
Mutlaq Almutlaq
College of Medicine, King Saud Bin Abdulaziz University for Health Sciences,Riyadh; King Abdullah International Medical Research Center, Riyadh
Saudi Arabia
malmutlaq15@hotmail.com
| How to cite this article: Aljuhani W, Almutlaq M, Alomar A, Alanazi K, Al-Thani AS, Alqahtani T. Incidence and predictors of 30-day postoperative complications following musculoskeletal tumor surgery. J Musculoskelet Surg Res 2020;4:141-145 |
Abstract
Objectives: Surgical intervention remains one of the best curative approaches in musculoskeletal (MSK) tumors. However, postoperative complications remain an issue, especially within the first 30-day postoperatively. Hence, the main objective of this study is to estimate the incidence and to identify the predictive factors of 30-day complications following MSK tumor surgery (MTS). Methods: This is a retrospective, descriptive study of 85 patients who had undergone MTS between 2016 and 2019 in our institution. The included patients were those who had MTS caused by a malignant tumor or giant cell tumor. Results: Twenty-eight patients (33%) had a complication during the first 30 days following surgery. The most common complication was surgical site infection in 64% (n = 18 / 28) followed by venous thromboembolism in 11% (n = 3 / 28) and then death in 7% of the patients (n = 2 / 28). Complications were distributed equally among genders. The complication rate was 36% in bone tumor surgeries (n = 22 / 61) and 21% in soft tissue tumor surgeries (n = 4 / 24). Ewing's sarcoma patients had the highest complication rate among bone tumors (36%, n = 8 / 22). Lower extremities' surgeries had the highest complication rate (35%, n = 18 / 51). Furthermore, 80% of the patients with a cardiovascular condition other than hypertension developed a complication (n = 4 / 5, P = 0.0322). Conclusion: One-third of the patients who underwent MTS developed a complication within a 30-day duration. The diagnosis of Ewing's sarcoma, surgery of lower extremities, and preexisting cardiovascular conditions was linked to a higher complication rate.
Introduction
Musculoskeletal (MSK) tumors are a diverse group of lesions that can originate in the bones or soft tissues.[1] MSK tumors are not uncommon compared to other types of neoplasms. In Saudi Arabia, according to the tumor registry of King Faisal Specialist Hospital and Research Center, MSK neoplasms are one of the top ten cancers that affect the pediatric population.[2] In addition, these neoplasms are one of the top twenty malignant neoplasms in adults across Saudi Arabia.[3] Ranging from simple benign to very complex malignant, each type of tumor is unique. As such, meticulous planning is required to determine the treatment modalities for the best therapeutic outcomes. Despite the risk of developing complications, ranging from surgical site infections (SSIs) to death, surgery remains one of the best options for many types of MSK tumors.[4],[5] Identifying the predictive factors for developing a complication during the 30 days will lead to better patient-centered care. Hence, the early prediction of complications within the 1st postoperative month will significantly aid in preventing and monitoring these complications, and by that, it will help in decreasing the mortality and morbidity rates, associated costs, and hospital stays. Collectively, these factors will improve surgical/therapeutic outcomes and will help in establishing better guidelines for preoperative planning. Thus, the pertinent questions are can we predict which patients are at a higher risk for 30-day complications? and how can we prevent and/or monitor them accordingly? To date, studies in the literature that estimated and predicted early postoperative complications of MSK tumors surgery are scant. Nonetheless, the duration defining “early” differs between studies, with the majority ranging from 2 weeks up to 3 months. In this study, we focused on the complications occurring within the first 30 days following MSK tumor surgery (MTS). It is of importance to mention that this duration as a definition of early complications is not a novel one, and multiple studies in the literature have been built on the basis of studying 1st-month postoperative complications since it allows proper monitoring by being neither of short duration as in 2 weeks nor of long duration as in 3 months. The main objective of this study is to estimate the incidence and to identify the predictive factors that might lead to complications within 30 days following MSK tumor surgery.
Materials and Methods
This is a retrospective, descriptive study of patients who had undergone MTS between 2016 and 2019. Patients who had undergone surgery due to a malignant MSK tumor or giant cell tumor (GCT) were enrolled in this study. The reason to include GCT is that it is a locally aggressive benign tumor, which is mimicking a low-grade malignant tumor.[6] A customized data collection procedure recorded relevant demographics such as age, gender, weight, height, smoking status, associated comorbidities, tumor type, tumor site, surgery type, duration of pre- and post-operational hospital stay, readmission within 30 days, complications within 30 days, type of complications, operational blood loss, and blood transfusion frequency. The American Society of Anesthesia Score was obtained from the patients' files.[7] All collected data were processed and analyzed. Data analysis was carried out by the Department of Bioinformatics and Biostatistics, King Abdullah International Medical Research Center (KAIMRC), using the SAS Systems (Copyright© 2002–2012 by SAS Institute Inc., Cary, NC, USA). Categorical variables such as gender and smoking status were described in frequency and proportions, while the quantitative variables such as age and weight were compared by analyzing means and standard deviations of corresponding data. Demographic and clinical characteristics were compared across the study groups using a t-test and Chi-square test for continuous and categorical variables, respectively. All data are represented in percentage and mean values and were used for comparative analyses, with a corresponding 95% confidence interval, and the statistical significance was considered at P ≤ 0.05.
Results
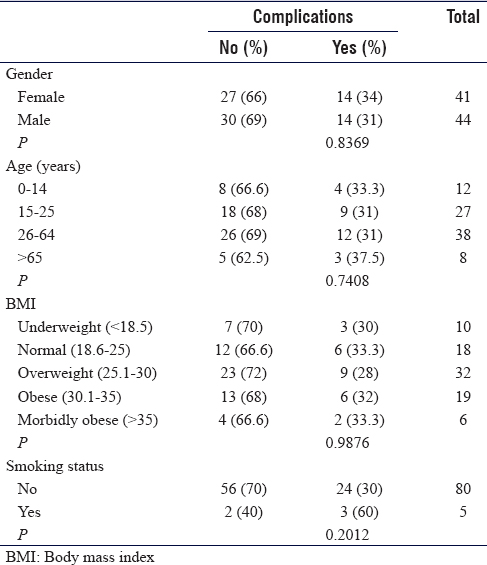
The study team reviewed 277 patients, 85 of which met our inclusion criteria, which is undergoing an MTS between 2016 and 2019. These cases were further subclassified according to the age (0–14, 15–25, 26–64, >64 years) and body mass index (BMI) (<18.5, 18.6–25, 25.1–30, 30.1–35, >35) [Table - 1]. Neither gender, age, BMI, nor smoking status was associated with having a higher rate of complications.
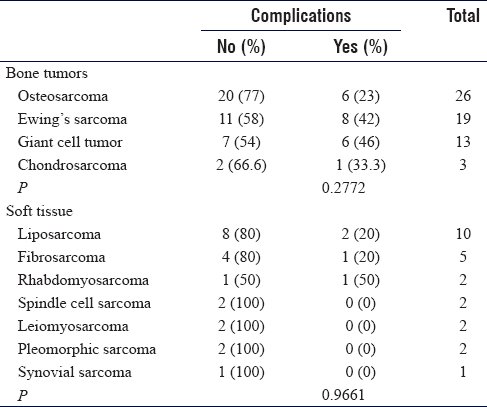
Among the selected 85 cases in our study, there were 61 cases of bone tumors (72%) and 24 cases of soft tissue tumors (28%). The prevalent bone tumors in our study were osteosarcoma (26 patients, 43% of bone tumors) and Ewing's sarcoma (19 patients; 31% of bone tumors). The most common soft tissue tumor was liposarcoma (10 patients, 42% of soft tissue tumors). The location of the tumors varied – 51, 27, and 7 patients had tumors in the lower extremities (60%), upper extremities (32%), and pelvis (8%), respectively. The rate of readmission within 30-day postsurgery was 20% (n = 17 / 85). In total, 25% (n = 21 / 85) of the patients were diagnosed with comorbid diseases such as diabetes or hypertension. The common comorbidities were hypertension (17%; n = 15 / 85), diabetes mellitus (14%; n = 12 / 85), respiratory illness (13%; n = 11 / 85), dyslipidemia (11%; n = 9 / 85), and cardiovascular diseases (6%; n = 5 / 85).
Postoperative complications within 30 days were observed in 28 patients (33% of those who underwent MTS) [Graph 1]. The most common complication was SSIs (64%; n = 18 / 28). Fourteen cases of SSIs were in the lower extremities, two in the upper extremities, and two in the pelvis. These infections primarily resulted from Pseudomonas aeruginosa, methicillin-resistant Staphylococcus aureus (MRSA), and Escherichia coli. Moreover, 15 cases of SSIs were located superficially (83%), and 3 cases were deeply located (17%). The second most observed complication in our study was venous thromboembolism (VTE, 11%; n = 3 / 28), two of which had MTS in the lower extremities and one in the upper extremities. Two patients with complications died within 30-day postsurgery (7%; n = 2 / 28).

Overall for bone tumors, 48 cases were Stage 2b (79%) and 13 were Stage 3 (21%). This staging is according to the Enneking's Staging System of Malignant Bone Tumors. For soft tissue tumors, 19 cases were Stage 3 (79%), 3 cases were Stage 3b (13%), and 2 cases were Stage 4 (8%). This staging is according to The American Joint Commission on Cancer. Furthermore, for the 18 patients who had an infection following the surgery, 15 of which were bone tumors: 11 had Stage 2b (61%) and four had Stage 3 (22%). Three were soft tissue tumors, and they were Stage 3 (17%). Furthermore, all three patients who had VTE following surgery were cases of bone tumors.
The complications were distributed equally between the males and the females. The complication rates of bone and soft tissue tumor surgeries were 36% (n = 22 / 61) and 17% (n = 4 / 24), respectively. The rate of complications in the patients with Ewing's sarcoma, osteosarcoma, and liposarcoma was 42% (8 of 19 bone tumors), 23% (6 of 26), and 20% (2 of 10 soft tissue tumors), respectively [Table - 2].
The highest rate of complications was observed among MSK tumor surgeries in the lower extremities (35%, n = 18 / 51), followed by the upper extremities (29%, n = 8 / 27) and pelvis (28%, n = 2 / 7). In total, 16 patients received blood transfusion. Among these recipients, six patients developed complications (38%). Among 69 patients who did not receive any blood transfusion, 20 patients developed complications (29%). Among 15 patients diagnosed with hypertension, only two developed complications (13%). In addition, 80% of the patients with a preexisting cardiovascular condition, other than hypertension, developed complications (n = 4 / 5) (P = 0.0322). The rest of the comorbidities (hypertension, diabetes mellitus, respiratory illness, and dyslipidemia) were not associated with any complications.
Discussion
MTS is challenging and potentially associated with a high complication rate. The identification of the complications within a short period of the surgical intervention would help healthcare providers to take caution in treating patients at a higher risk of developing a complication, resulting in better prognostic outcomes. Our results suggest that 33% of those who underwent MSK tumor surgery developed a postoperative complication within a month. The complications ranged from SSIs to death.
Our findings are consistent with previously published literature that showed SSIs being frequently associated with MSK tumor surgery. A study published in 2013 reported a 7% incidence rate of postoperative complications, with SSIs as the most frequent complication (2.7%).[8] Another study in 2019 reported that 61% of the patients had complications, and the most reported complication was SSIs as well.[3] Furthermore, a study in 2017 reported that SSIs were the most common infection following limb-sparing surgeries (35.6%).[9] It is important to note that these studies were not specific in including only 30-day postoperative complications. The presence of organisms such as P. aeruginosa and MRSA indicates that the infections were either hospital-acquired or the patient was immunocompromised. A study on 79 patients at King Fahad Hospital, Al-Khobar, reported that the most common organism causing SSIs in orthopedic surgery was MRSA (23; 29.1%), followed by the Acinetobacter species (17; 21.5%) and the Pseudomonas species (15; 18.9%).[10] These data are in some concordance with our findings since SSIs reported in this study also resulted from the Staphylococcus and Pseudomonas species. Interestingly, we did not have SSIs resulting from the Acinetobacter species. Identification precedes the elimination of the causative infectious agents, and thus, proper identification of the infectious agents is paramount. Surgeries with reconstruction following resection, especially pelvic, have been shown to have 11% higher incidence rates of infection than surgeries without reconstruction. However, we were not able to study this factor unfortunately.[11] Blood transfusion is significantly associated with developing a postoperative infection, which includes infections of the surgical site, the respiratory tract, the urinary tract, endocarditis, and meningitis.[12] This is hypothesized to be driven by the blood transfusion-related immunomodulation. In our study, we observed a higher incidence rate of postoperative complications in patients who received blood transfusion (38%; n = 6 / 16) than in patients who did not receive any blood transfusion (29%; n = 20 / 69).
The second most common cause of complications in our study was VTE. A previous study showed that pelvis or lower limb surgeries could be associated with VTE.[13] We are not aware of any studies that showed VTE development following MTS. Therefore, it is clear that the prophylaxis of VTE is necessary for orthopedic procedures, including MSK tumor surgery. In terms of site, the highest rate of complications in our study was observed in the lower extremities. A study published in 2014 reported that pelvic involvement and pelvic surgeries have a significantly high rate of complications.[14]
Our study has several limitations. First, the study's sample is limited since it was conducted in a single tertiary-care hospital, which could have led to an underestimation or overestimation of some postoperative complications. To overcome this, future studies involving multicenters and a large cohort are required. Second, we were not able to identify a few important clinical parameters that could have affected the rates of postoperative complications, such as some laboratory results before and after the surgery and the exact amount of the blood transfusion.
Despite the above limitations, our study will be an essential cornerstone of researches in this field in Saudi Arabia. In addition, if there are similar studies, this study will still be addition with different findings for sure as the setting is different. Moreover, estimating the incidence and identifying the factors of early postoperative complications are of utmost importance, and no single study is sufficient to achieve that goal. Thus, our work is vital in paving the path for future studies and will help the orthopedic tumor society in investigating 30-day postoperative complications further.
Conclusion
Thirty-three percent of the patients who underwent MTS developed a complication within a month. The two most predominant complications were SSIs and VTE. The diagnosis of Ewing's sarcoma, surgeries in the lower extremities, and preexisting cardiovascular diseases is most likely associated with a higher complication rate. Future studies involving multicenters and a large cohort are required for further validations of our findings.
Recommendations
As the two most predominant complications were SSIs and VTE, emphasis should be on preventing these two. To help prevent SSIs, the usage of perioperative antibiotic prophylaxis, and to continue postoperative is paramount. To reduce the numbers of postoperative VTE, patients should be assessed for the risk of developing thromboembolism before the initiation of VTE prophylaxis. Then, the patient's individual risk of thromboembolism should determine whether to start VTE prophylaxis or not. The diagnosis of Ewing's sarcoma, surgeries in the lower extremities, and cardiovascular diseases was linked to a higher complication rate. Thus, those with these factors should be monitored as patients with a higher risk of developing complications.
Ethical considerations
The data were collected after obtaining Institutional Review Board approval from KAIMRC (RSS19 / 026/R). Access for the data was only available to the research members. The confidentiality of all patients was preserved, and neither names nor medical record numbers were used or collected.
Acknowledgments
We acknowledge Ms. Bayan AlBaddah, from KAIMRC, for doing the statistical analysis.
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Authors' contribution
WSA conceived and designed the study. MSA, AOA, KAA, ASA, and TMA acquired and interpreted data and prepared the initial draft. WSA, MSA, and AOA wrote the final draft of the article. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | American Academy of Orthopaedic Surgeons; 2020. Available from: https://orthoinfo.org/en/diseases--conditions/?topic=Tumors [Last accessed on 2020 Jan 20]. [Google Scholar] |
| 2. | Nhic.gov.sa; 2019. Available from: https://nhic.gov.sa/eServices/Documents/2014.pdf. [Last accessed on 2019 Jul 03]. [Google Scholar] |
| 3. | Kfshrc.edu.sa; 2019. Available from: https://www.kfshrc.edu.sa/store/media/8ek.pdf. [Last accessed on 2019 Jul 03]. [Google Scholar] |
| 4. | Benatto M, Hussein A, Gava N, Maranho D, Engel E. Complications and cost analysis of hemopelvectomy for the treatment of pelvic tumors. Acta Ortopédica Brasileira 2019;27:104-7. [Google Scholar] |
| 5. | Gutowski CJ, Basu-Mallick A, Abraham JA. Management of bone sarcoma. Surg Clin North Am 2016;96:1077-106. [Google Scholar] |
| 6. | Hogendoorn CW, de Andrea C. Bones and joints cancer: Pathology and genetics. In: Boffetta P, Hainaut P, editors. Encyclopedia of Cancer. 3rd ed. Oxford, UK: Elsevier; 2019. p. 164-5. [Google Scholar] |
| 7. | American Society of Anesthesiologists; 2019. Available from: https://www.asahq.org/standards-and-guidelines/asa-physical-statusclassification-system. [Last accessed on 2020 Jan 20]. [Google Scholar] |
| 8. | Ogura K, Yasunaga H, Horiguchi H, Ohe K, Shinoda Y, Tanaka S, et al. Impact of hospital volume on postoperative complications and in-hospital mortality after musculoskeletal tumor surgery. J Bone Joint Surg 2013;95:1684-91. [Google Scholar] |
| 9. | Severyns M, Briand S, Waast D, Touchais S, Hamel A, Gouin F. Postoperative infections after limb-sparing surgery for primary bone tumors of the pelvis: Incidence, characterization and functional impact. Surg Oncol 2017;26:171-7. [Google Scholar] |
| 10. | Al-Mulhim FA, Baragbah MA, Sadat-Ali M, Alomran AS, Azam MQ. Prevalence of surgical site infection in orthopedic surgery: A 5-year analysis. Int Surg 2014;99:264-8. [Google Scholar] |
| 11. | Angelini A, Drago G, Trovarelli G, Calabrò T, Ruggieri P. Infection after surgical resection for pelvic bone tumors: An analysis of 270 patients from one institution. Clin Orthop Relat Res 2014;472:349-59. [Google Scholar] |
| 12. | Fisahn C, Schmidt C, Schroeder JE, Vialle E, Lieberman IH, Dettori JR, et al. Blood transfusion and postoperative infection in spine surgery: A systematic review. Global Spine J 2018;8:198-207. [Google Scholar] |
| 13. | Tuy B, Bhate C, Beebe K, Patterson F, Benevenia J. IVC filters may prevent fatal pulmonary embolism in musculoskeletal tumor surgery. Clin Orthop Relat Res 2009;467:239-45. [Google Scholar] |
| 14. | Schaser KD, Melcher I, Märdian S, Perka C, Locher R, Schwabe P. Management of complications following resection and defect reconstruction of tumors near the hip joint. Orthopade 2014;43:92-102. [Google Scholar] |
Fulltext Views
1,781
PDF downloads
434





