Translate this page into:
Inserting the best knee: A short-term analysis of posterior stabilized versus cruciate substituting ultracongruent tibial inserts for total knee replacement
*Corresponding author: Pravin K. Vanchi, Department of Orthopedics, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India. pravinvanchi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rajguhan T, Vanchi P, Tarun Prashanth K, Ravi Veeraraghavan R, Murugesan M. Inserting the best knee: A short-term analysis of posterior stabilized versus cruciate substituting ultracongruent tibial inserts for total knee replacement. J Musculoskelet Surg Res, 2023;7:180-5.
Abstract
Objectives:
As the posterior cruciate ligament is a primary stabilizer of the knee, it is functionally replaced using posterior stabilized (PS) or anterior stabilized ultracongruent (UC) inserts in cases where it is attenuated or requires resection. This study compared PS and UC inserts in terms of functional and pain scores in patients undergoing total knee replacement (TKR).
Methods:
This prospective randomized study included 90 consecutive patients who underwent total TKR; PS and UC inserts were used in 47 and 43 patients, respectively. Outcomes were measured over 1 year. The duration of surgery was recorded, and the pain was assessed using the Visual Analog Scale score; functional outcomes were evaluated by assessment of the range of motion (ROM), Knee Society Score, and joint stability. All parameters and scores were assessed pre-operatively, immediately post-operative, 1 month, 3 months, and at 1-year follow-up.
Results:
The groups showed no significant differences and matched similarly in terms of body mass index, sex, or age. At a minimum of 1-year follow-up, TKR using either insert significantly improved the mean ROM and Knee Society and functional scores, which were comparable between the groups. Overall, 14 and 13 patients with UC and PS inserts, respectively, had excellent outcomes; 2 and 1 patients from the PS and UC groups, respectively, were lost to follow-up. Surgery was significantly shorter in the UC group. Although the Visual Analog Scale score had reduced significantly in both groups at the end of 3 months, one patient from the PS group had persistent knee pain with decreased ROM.
Conclusion:
The inserts showed no significant differences in terms of the ROM and Knee Society and functional scores. Surgery was notably shorter in the UC group (by 5 min). TKR using UC inserts is an effective alternative in patients with small bony geometry and may preserve intercondylar bone.
Keywords
Anterior stabilized knee
Posterior stabilized knee
Ultracongruent inserts
Posterior cruciate ligament substituting
Total knee replacement
INTRODUCTION
The decision on whether to retain or resect the posterior cruciate ligament (PCL) during total knee replacement (TKR) remains controversial. Although it was traditionally believed that cruciate-retaining designs could increase flexion and range of motion (ROM) by restoring normal knee biomechanics and anatomical femoral rollback,[1,2] studies suggest that there is a paradoxical anterior translation of the femur on the tibia during knee flexion.[3] The PCL is an important structure that aids femoral rollback and acts as a static stabilizer. It is responsible for absorbing a significant amount of force and has different types of receptors that detect joint position and motion.[4-6] However, PCL function can be affected or attenuated in degenerative joint diseases that cause severe varus, valgus, or fixed flexion deformities. As the PCL may require resection in such cases, it is essential to modify the implant design to retain its function.[6,7]
In ultracongruent (UC) inserts, the polyethylene is designed to create an elevated anterior rim and a more conformal articular surface. The elevated anterior rim helps in preventing anterior femoral translation during knee flexion and prevents dislocation.[8] Cruciate-substituting designs include either posterior stabilized (PS) or UC tibial inserts. The design of the PS knee incorporates a post and cam mechanism, where the polyethylene tibial post articulates with the femoral cam.
Each design possesses distinct strengths and weaknesses. Although the PS implant design offers the advantages of femoral rollback and stability, it is associated with certain disadvantages, including distal femur fractures, damage or dislocation of the post, and patellar clunk syndrome. The main limitation lies in the need for box-cut resection of the distal femur, which decreases the bone stock in this region. This reduction in bone stock makes future revision challenging. It increases the likelihood of condylar fractures in Indian female patients with small femoral geometry, as it is already common in primary TKR.[9] In addition, reports from a few cases suggest that the tibial post may undergo plastic deformation and suffer damage.[10]
UC inserts allow the bone stock to be preserved, decrease surgical duration, and expedite post-operative recovery. UC designs also allow for substituting the PCL with ease, without the need for additional bone resection. In this context, the cruciate-retaining component confers the disadvantage of abnormal anteroposterior translation and an increase in peak pressures in the patellofemoral region; this may cause increased wear of the component.[11,12]
PCL is a primary stabilizer of the knee, and it is functionally replaced using PS or anterior stabilized UC inserts in cases where it is attenuated or requires resection. This study aimed to compare PS and UC inserts in terms of pain and functional scores in patients undergoing TKR.
MATERIALS AND METHODS
This prospective study included 90 consecutive patients who underwent TKR during the period of October 2020– December 2021 and had consented to participate in the study. The inserts were selected pre-operatively using simple randomization. The patients were asked to pick a lot, and that determined the group that they were assigned to. This aided in eliminating bias and ensuring that the groups were comparable. After randomization, 47 and 43 patients were included in the PS and UC groups, respectively. The two groups were followed up between October 2020 and December 2022. All parameters and scores were assessed preoperatively, immediately post-operative, 1 month, 3 months, and at 1-year follow-up. Informed consent was obtained from all the patients before inclusion. The height and weight were recorded in all cases and the body mass index (BMI) was calculated. The ROM and deformities of the knee were documented pre-operatively, in addition to thorough history-taking and physical examination. Radiographs of the knee were obtained pre-operatively in the standing position and anteroposterior and lateral views were obtained. Patients with a BMI exceeding 40, having collateral ligament laxity, and those receiving high doses of steroids were excluded from the study. All surgeries were performed by the same experienced arthroplasty surgeon using the Smith and Nephew Genesis II knee system.
All patients underwent surgery using the same surgical protocol. A midline skin incision was placed, and the joint was accessed through the medial parapatellar approach. Following initial soft-tissue dissection, arthrotomy, and patellar subluxation, tibial resection was performed perpendicular to the mechanical axis of the tibia using an extramedullary guide with an anatomic slope. The PCL was resected in all knees, and the intramedullary jig was used to perform the distal femoral cut. The ideal femoral size and cutting block were selected using the anterior referencing system; appropriate anterior, posterior, distal femur, and chamfer cuts were then placed. All the above steps were common to both groups. In PS-TKR, the cut on the intercondylar notch was placed in the distal femoral region. Out of the options provided by the manufacturer in the PS design (high-flex and regular), we used the regular design in all our cases. The UC and PS used the cruciate-retaining and PS femoral components, respectively. The post-operative rehabilitation protocols were similar in both groups. Patients were mobilized on post-operative day 2 and were assessed at 1 month, 3 months, and 1 year after surgery. Radiographs were obtained at all follow-up visits and a thorough clinical examination was performed to assess all the parameters. The surgical duration was compared between the groups; the Knee Society Score (KSS), functional score, ROM, joint stability in both sagittal and coronal planes, and pain (in terms of visual analog scale scores) were compared between the two groups at all post-operative follow-up visits. The SPSS for Windows Inc. software package (version 23.0; IBM Corporation, Armonk, NY, USA) was used for statistical analysis.
RESULTS
Female and male patients predominated in the UC and PS groups, respectively. The UC and PS groups had 27 and 20 female patients, respectively; 7 and 6 patients in the UC and PS groups, respectively, had rheumatoid arthritis. The UC group had a mean BMI of 32, as opposed to a mean value of 32.8 in the PS group. The UC and PS groups had a mean age of 60.8 and 61.9 years, respectively. The age for requirement of TKR ranged between 48 years (in a female patient) and 81 years (in a male patient). The mean pre-operative KSS in the UC and PS groups was 41.95 and 43.5, respectively. At the end of 3 months, the mean KSS in the UC and PS groups was 72.4 and 70.9, respectively (P-value was not statistically significant).
The mean functional score had improved significantly at the end of 1-year follow-up, with values of 82.50 and 83.50 in the UC and PS groups, respectively (P = 0.60; statistically insignificant). The pre-operative mean ROM in the UC and PS groups was 90° and 87°, respectively; at the end of 1 year, these values improved to 102.75° in the UC group and 103.75° in the PS group (P = 0.59; statistically insignificant). There were no cases of sagittal plane and coronal plane instability in both groups.
The mean duration of surgery lasted 113.72 and 118.9 min in the UC and PS groups, respectively. The surgical time in the UC group was 4.35% faster than in the PS group. A notable disparity with a statistically significant difference of 5.18 min was observed between the groups (P = 0.049) [Figure 1]. A considerable reduction in pain was observed in both groups at the end of the 3-month follow-up; no instances of instability were seen in either group at the end-of-study follow-up.

- Duration of surgery in the two groups.
At 1-year follow-up, 14, 27, and 1 patients in the UC group demonstrated excellent, good, and poor outcomes (in terms of the KSS), respectively. The patient with poor outcomes had multiple comorbidities. In the PS group, 13 and 31 patients had excellent and good outcomes, respectively. One patient experienced an unfavorable outcome characterized by persistent pain and a reduced ROM in the knee. This patient was obese, with a BMI of 37 [Table 1].
| Pre-operative variables | Group | Mean | Standard deviation | Standard error of the mean | P-value |
|---|---|---|---|---|---|
| Range of motion | |||||
| UC inserts | 102.7500 | 7.84056 | 1.23970 | 0.59 | |
| PS | 103.7500 | 8.96932 | 1.41817 | ||
| KSS | |||||
| UC inserts | 79.7250 | 6.15604 | 0.97335 | 0.48 | |
| PS | 80.6500 | 5.55416 | 0.87819 | ||
| Functional score | |||||
| UC inserts | 82.5000 | 9.54074 | 1.50852 | 0.60 | |
| PS | 83.5000 | 7.35544 | 1.16300 | ||
| Total KSS | |||||
| UC inserts | 81.1125 | 6.87944 | 1.08774 | 0.49 | |
| PS | 82.0750 | 5.59939 | 0.88534 | ||
| Surgical duration | |||||
| UC inserts | 113.7250 | 12.53096 | 1.98132 | 0.049 | |
| PS | 118.9000 | 10.53152 | 1.66518 |
PCL: Posterior cruciate ligament, PS: Posterior stabilized, UC: Ultracongruent, KSS: Knee society score
DISCUSSION
In our study, no statistically significant difference was observed between the UC and PS groups in terms of functional outcomes; this was observed irrespective of the higher pre-operative KSS in the PS group. Among PS and UC inserts, the former is commonly used in primary TKR.[13] The sacrifice of the PCL is the major consideration during the analysis of outcomes in these patient groups. In this context, decision-making depends entirely on surgeon preferences and experience.[14] UC inserts have been available for clinical use in recent years and are being commonly used. This is mainly responsible for the relative lack of clinical studies that have analyzed and compared UC inserts with other inserts such as PS, cruciate-retaining, and rotating platforms. In this context, it is an established fact that the pre-operative functional status determines postoperative outcomes.[15]
In their meta-analysis, Akti et al. analyzed and compared clinical and isokinetic performance outcomes between patients receiving PS and UC inserts.[16] The end-of-study ROM in the UC and PS groups was 128.7° and 133.9°, respectively. The outcome differences were not statistically significant and agreed with our study’s findings. The demographic characteristics of their cohort were also comparable to our study. In addition, their analysis showed no statistically significant differences in terms of the KSS; the authors, therefore, concluded that there are no significant functional differences between these two inserts. In another study, Machhindra et al. found the mean ROM to be higher in the PS group than in the UC group; the difference was statistically significant.[17] Notably, the end-of-study ROM in our cohort’s UC and PS groups was 102.75° and 103.75°, respectively.
Certain studies question the functionality of knees with UC inserts owing to various factors; these include anteroposterior translation and instability, which are observed postoperatively.[18] The findings of our study suggest the absence of any statistically significant differences in post-operative function and, therefore, contradict this assumption.
The cohort studied by Lützner et al.[19] had a similar age group and a predominance of female patients. However, the patients had a higher BMI compared to our study. The authors included 127 patients in their study. The mean functional score at the end of 1-year follow-up was 86.1 in both the UC and PS groups; the corresponding scores in our cohort were 82.50 and 83.50, respectively. Both studies showed good functional results with no statistically significant differences between the inserts. [Figure 2] shows a comparison of KSS scores observed in the cohorts included by Laskin et al., Lützner et al., Han and Kang, and our study.[8,19,20]
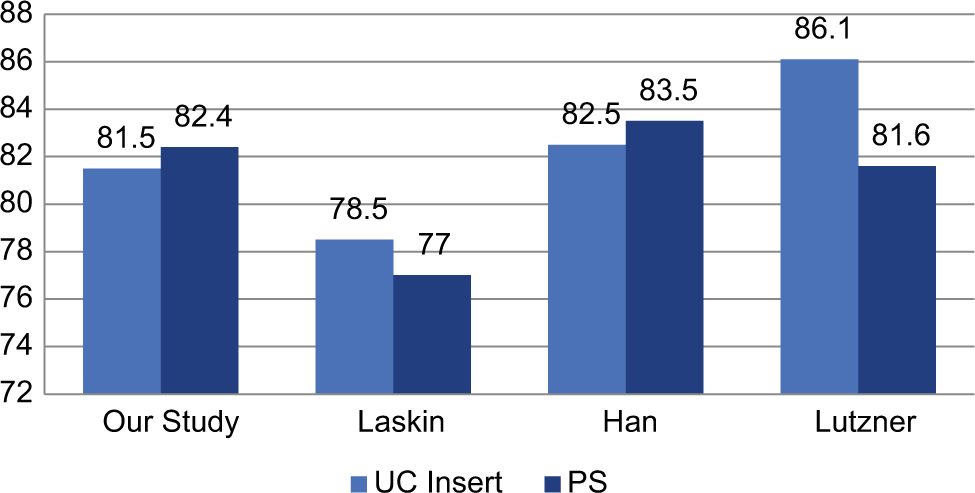
- Comparison of knee society score between various studies.
Our study revealed a significantly longer duration of surgery in the PS group (by 5 min) than in the UC group. This may be due to the fewer surgical steps needed for UC insert placement (the box cut required for femoral preparation in the PS group was not required in the UC group). No varus, valgus, or anteroposterior instability was observed in any patient in either group. None of the cases in our study demonstrated tibial post-breakage, intercondylar fractures of the femur, or cam dislocation at the end of 1-year follow-up. In this context, tibial post-breakage and cam dislocation are possible in cases of TKR using PS inserts. Surgical variables, including excessive flexion of the femoral component, the anterior position of the tibial tray, posteriorly inclined tibial slope, and joint line alteration by 8 mm, may predispose to post-impingement and failures.[21] Longer follow-up is therefore needed for identifying the development of tibial post-breakage.
UC inserts that were used in cruciate-substituting TKR offered a lower ROM, KSS, and functional scores compared to TKR using PS inserts. However, the difference was not statistically significant [Figure 3]. Notably, the UC inserts offered the advantages of shorter surgical duration and preservation of bone stock; however, no statistically significant differences in clinical outcomes were found compared to PS inserts.

- Comparison of knee society score between the two groups.
The small sample size and short follow-up were a major limitation of our study. Further data from long-term studies in larger cohorts are needed to improve understanding of the preferable inserts for optimal knee outcomes. Although patients with various grades of osteoarthritis were included in our study, most patients had two particular grades.
CONCLUSION
TKR using UC inserts is a reliable alternative procedure that can reduce dependence on PS designs in cases where the PCL needs to be sacrificed. On short-term follow-up, it provided comparable results in terms of functionality and reduction of pain. However, UC inserts offered no clear advantages over PS inserts other than a reduced surgical duration. The UC group had reduced end-of-study ROM (102.75) compared to the PS group (103.75). However, the difference was not statistically significant.
ETHICAL APPROVAL
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Sri Ramachandra Institute of Higher Education and Research on 15.10.2020 with number CSPMED/20/OCT/62/121
AUTHORS’ CONTRIBUTIONS
TVR collected the data required for the study. PKV and TVR did the data and statistical analysis of the study. MMK was the chief surgeon for all the cases. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
USE OF ARTIFICIAL INTELLIGENCE (AI)- ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patients consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study received no specific grant from public, commercial, or not-for-profit funding agencies.
References
- Role of the posterior cruciate ligament in total knee arthroplasty. J Am Acad Orthop Surg. 1998;6:176-87.
- [CrossRef] [PubMed] [Google Scholar]
- Retention of the posterior cruciate in total knee arthroplasty. J Arthroplasty. 1988;3(Suppl):S13-9.
- [CrossRef] [PubMed] [Google Scholar]
- Kinematics of posterior cruciate ligament-retaining and-substituting total knee arthroplasty: A prospective randomised outcome study. J Bone Joint Surg Br. 2005;87B:646-55.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior stabilized TKA reduce patellofemoral contact pressure compared with cruciate retaining TKA in vitro. Knee Surg Sports Traumatol Arthrosc. 2009;17:1159-65.
- [CrossRef] [PubMed] [Google Scholar]
- Cruciate-retaining total knee arthroplasty at 5 to 7 years follow up. Clin Orthop Relat Res. 2005;436:177-83.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior cruciate supplementing total knee replacement using conforming inserts and cruciate recession. Effect on range of motion and radiolucent lines. Clin Orthop Relat Res. 1994;309:146-9.
- [Google Scholar]
- Functional comparison of posterior cruciate-retaining versus posterior stabilized total knee arthroplasty. J Arthroplasty. 2004;19:349-53.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior-stabilized TKA is inferior to posterior-stabilized TKA in terms of postoperative posterior stability and knee flexion in osteoarthritic knees: A prospective randomized controlled trial with bilateral TKA. Knee Surg Sports Traumatol Arthrosc. 2020;28:3217-25.
- [CrossRef] [PubMed] [Google Scholar]
- Intra-operative fractures in primary total knee arthroplasty-a systematic review. Knee Surg Relat Res. 2020;32:40.
- [CrossRef] [PubMed] [Google Scholar]
- Fracture of the polyethylene tibial post in a posterior stabilized knee prosthesis: A case report and review of literature. J Orthop. 2015;12:160-3.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior-stabilized inserts are preferable to cruciate-substituting ultracongruent inserts due to more favourable kinematics and stability. Knee Surg Sports Traumatol Arthrosc. 2018;26:3300-10.
- [CrossRef] [PubMed] [Google Scholar]
- Different intraoperative kinematics, stability, and range of motion between cruciate-substituting ultracongruent and posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2018;26:1465-70.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in total knee arthroplasty implant utilization. J Arthroplasty. 2015;30:739-42.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior cruciate-retaining versus posterior-stabilized total knee arthroplasty: A meta-analysis. J Arthroplasty. 2013;28:439-44.
- [CrossRef] [PubMed] [Google Scholar]
- Does the severity or cause of preoperative stiffness affect the clinical results and range of motion after total knee arthroplasty? PLoS One. 2018;13:e0205168.
- [CrossRef] [PubMed] [Google Scholar]
- No differences in clinical outcomes or isokinetic performance between cruciate-substituting ultra-congruent and posterior stabilized total knee arthroplasties: A randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2021;29:3443-9.
- [CrossRef] [PubMed] [Google Scholar]
- Functional outcomes of a new mobile-bearing ultra-congruent TKA system: Comparison with the posterior stabilized system. J Arthroplasty. 2015;30:2137-42.
- [CrossRef] [PubMed] [Google Scholar]
- Condylar-stabilizing tibial inserts do not restore anteroposterior stability after total knee arthroplasty. J Arthroplasty. 2015;30:587-91.
- [CrossRef] [PubMed] [Google Scholar]
- No difference in range of motion between ultracongruent and posterior stabilized design in total knee arthroplasty: A randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017;25:3515-21.
- [CrossRef] [PubMed] [Google Scholar]
- Deep-dish congruent tibial component use in total knee arthroplasty: A randomized prospective study. Clin Orthop Relat Res. 2000;380:36-44.
- [CrossRef] [PubMed] [Google Scholar]
- Joint line elevation and tibial slope are associated with increased polyethylene wear in cruciate-retaining total knee replacement. J Orthop Res. 2020;38:1596-606.
- [CrossRef] [PubMed] [Google Scholar]






