Translate this page into:
Ipsilateral shoulder and elbow dislocation: Camel bite-related injury
2 Department of Orthopedics, Prince Mohammed Bin Abdulaziz Hospital, Almadinah Almunawwarah, Saudi Arabia
Corresponding Author:
Yaser A Alshabi
Department of Orthopedics, King Fahad Hospital, Almadinah Almunawwarah
Saudi Arabia
yaser.alshabi@gmail.com
| How to cite this article: Alshabi YA, Alhumaidi IM, Albouq FK, Mohammed Aziz FA, Khalil MA. Ipsilateral shoulder and elbow dislocation: Camel bite-related injury. J Musculoskelet Surg Res 2021;5:57-61 |
Abstract
Ipsilateral dislocation of the shoulder and elbow joints is a quite rare injury. Due to its rare presentation, one of the two-dislocation diagnoses can be delayed or even missed. We present a unique case of camel-bite injury, resulting in ipsilateral shoulder and elbow fracture dislocation with open ulna shaft fracture that has not been reported in the English literature before. Camel-bites injuries should be taken seriously as it can result in severe, devastating open injuries. The gripped extremity should raise the suspicion of multiple injuries, so careful assessment of the entire extremity should be carried out. Moreover, proper surgical and medical management can prevent unpleasant outcomes.
Introduction
Concomitant shoulder and elbow joint dislocation is not a common presentation. It can be easily missed if the patient is not adequately examined at the initial presentation.[1]
Camel-related injuries are common in Saudi Arabia. It accounts for 80% of animal-related injuries.[2] Biting the victim and lifting him/her along with shaking with jerky movements and then throwing him/her are the common scenario.[3]
Saxena et al. classified the camel bites according to the severity of soft tissue involvement to skin and subcutaneous tissue (Grade I), with muscle (Grade II), with bone (Grade III), and neurological injury without and with bone involvement (Grade IV and V, respectively), or traumatic amputation (Grade VI).[4] Camel bites carry a high risk of complications, and infection rates have been reported as high as 86.3%. Polymicrobial infection usually occurs, and common pathogens include Pasteurella aerogenes, Actinobacillus, and Aeromonas. Bone complications (i.e., osteomyelitis) can result in severe osteolysis that has been reported in the literature. If both camel and handlers have not been appropriately vaccinated, patients who sustain camel bites are at risk of rabies and tetanus infections.[5]
We present a unique case of camel bite injury, resulting in ipsilateral shoulder and elbow fracture dislocation with open ulna shaft fracture and its management not reported in the English literature.
Case Report
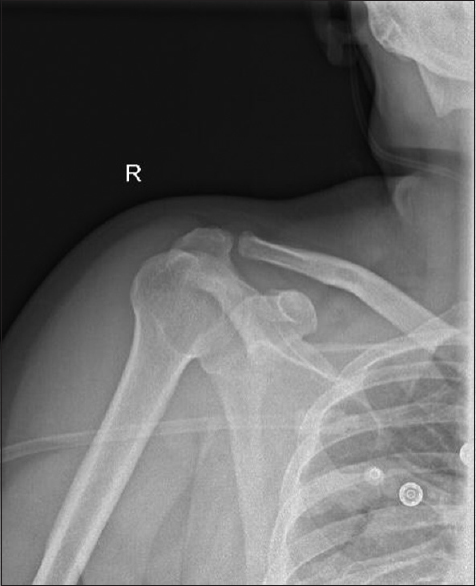
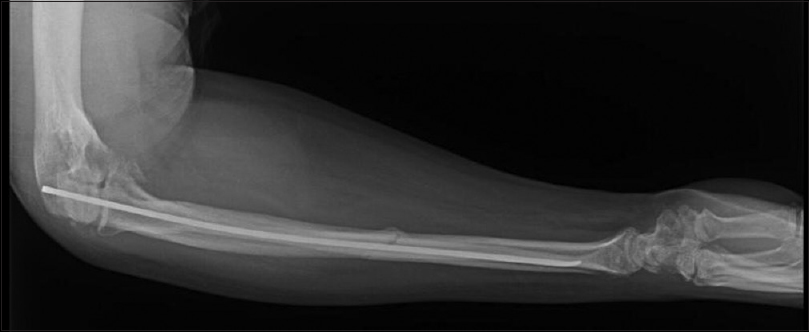
A 42-year-old obese (body mass index 34 kg/m2) male camel caregiver presented to the emergency department (ER) with severe pain over his right elbow joint 1 h after being bitten on his right forearm by an aggressive camel. The injury occurred on the farm, while the patient was trying to remove the camel harness. The camel turned aggressive, gripped the patient's right forearm firmly and consistently, lifted the patient in the air, and shook him forcefully. A patient's friend tried to rescue the patient by pulling him. On presentation, the affected extremity was supported with the opposite hand to keep the shoulder abducted, externally rotated, and elbow flexed. After his initial evaluation in the ER, the patient was found to be stable with injuries only to his right upper limb. On examination, there were a gross deformity of the elbow joint and an approximately 4 cm × 3 cm lacerated wound on the proximal dorsal aspect of the right forearm, which showed macerated muscle that extended to the bone and another two lacerated wounds located on the volar aspect measure approximately the same and multiple abrasions and small wounds all over the forearm [Figure - 1] and [Figure - 2]. Furthermore, the examination of the right shoulder joint showed loss of shoulder contour, both shoulder and elbow joints range of motion were limited, and the patient did not allow any movement of the upper extremity due to pain. The distal neurovascular examination was normal, and no associated injuries were detected. Radiographs of the right upper extremity revealed anterior dislocation of the right shoulder, posteromedial dislocation of the right elbow, coronoid process fracture, and ulnar midshaft fracture [Figure - 3], [Figure - 4], [Figure - 5]. Empirical antibiotic therapy (piperacillin-tazobactam 4.5 g intravenously) was administered immediately; tetanus and postexposure rabies prophylaxis were initiated. Under conscious sedation, the elbow joint was reduced first, then wounds were covered with a sterile dressing, and a back slab was applied. Reduction of the shoulder was carried out after, and the patient was kept on arm sling. Postreduction radiographs showed a concentric reduction with no joint space widening and maintained anatomical bony relations of both elbow and shoulder joints [Figure - 6] and [Figure - 7], and the decision was made to take the patient to the operating room for irrigation and debridement. The procedure began with debridement, and further exploration showed no other tendinous or neurovascular structures injury. The wounds were subsequently irrigated, and the skin was approximated. The examination pointed to instability of the elbow joint, while the shoulder joint was found to be stable. A back slab was reapplied, and 48 h later, the patient was taken to the operating room for second look irrigation and debridement and primary closure of the wound, and because of the soft tissue condition, stabilization of the nondisplaced ulna fracture using flexible intramedullary nail (size 2.5 mm) was carried out. Elbow instability at 50° short of full extension mandated transfixing the ulnohemeral joint using 2 Kirschner wires (K-wires) size 2 mm to maintain concentric reduction. An above elbow back slab was applied [Figure - 8]. The patient was observed for 48 h, then discharged home on prophylactic antibiotics (ciprofloxacin 500 mg twice daily and cefuroxime 500 mg twice daily for 7 days), and continued his planned rabies vaccines on the outpatient clinics as recommended by infectious disease team. One week later, the wound was well and there were no signs of infection. The patient was kept on his above elbow back slab and started on pendular exercises of his right shoulder. On 3-week follow-up, the sutures and the transarticular K-wires were removed at that time, and a hinged elbow brace with 50° of extension block applied with instructions was given upon physiotherapy referral for 10° weekly advancement of extension. After 6 weeks of follow-up, the patient was found to have a full range of motion of his shoulder and 20°–110° of elbow with no instability detected on examination. Radiographs showed a concentric reduction of both joints and on-going healing of his fractures [Figure - 9] and [Figure - 10]. The patient was followed up regularly to 4 years; the ulna fixation was removed after 3 months from the initial injury. Although the radiographs showed arthritic changes on his elbow joint at 1-year follow-up [Figure - 11] and [Figure - 12], the patient found to have a painless functional range of motion (10°–120°) with no restriction to his daily activities.
 |
| Figure 1: Volar forearm wounds upon presentation |
 |
| Figure 2: Dorsal forearm wounds upon presentation |
 |
| Figure 3: Initial shoulder radiograph showing anterior shoulder dislocation |
 |
| Figure 4: Initial elbow radiograph showing posteromedial elbow fracture dislocation |
 |
| Figure 5: Initial forearm radiograph showing ulna shaft fracture |
 |
| Figure 6: Immediate postreduction shoulder radiograph |
 |
| Figure 7: Immediate postreduction elbow radiograph |
 |
| Figure 8: Postoperative radiograph showing transarticular fixation of the ulnohumeral joint and intramedullary nailing of the ulna fracture |
 |
| Figure 9: Six-week follow-up lateral radiograph showing concentric reduction of the elbow after Kirschner wires removal |
 |
| Figure 10: Six-week follow-up anteroposterior radiograph showing concentric reduction of the elbow after Kirschner wires removal |
 |
| Figure 11: One-year follow-up elbow anteroposterior radiographs showing arthritic changes of the elbow joint |
 |
| Figure 12: One-year follow-up elbow lateral radiographs showing arthritic changes of the elbow joint |
Discussion
In our case, the association between the camel-bite contaminated injury and the ipsilateral shoulder and elbow fracture dislocation along with ulna fracture makes its unique presentation and complexity. When reviewing the literature, we found that most of the mechanism of injury of the reported cases was either motor vehicle accident, pedestrian injury, or a fall down.
Simultaneous ipsilateral shoulder and elbow dislocation is an uncommon associated injury pattern. Fractures may accompany the joint dislocations, so maintaining a high degree of suspicion and a thorough assessment of the extremity involved is a must, especially in obese patients, when changes of the shoulder contour and deformities can be minimal. Moreover, radiological evaluation of the proximal and distal bones of the involved joints is necessary.[6],[7]
Camel bites can have severe consequences, especially in the presence of bony involvement. The associated fractures should be considered as open contaminated fractures. Surgical treatment should include proper vigorous irrigation and debridement, preferably with soap or povidone–iodine solution, as it can reduce rabies' development by up to 90%.[8] The wounds should be explored to determine the extent of soft tissue injuries, and necrotic or crushed tissues should be debrided. Wounds should be kept open initially, and gabs can be approximated loosely. Delayed primary closure can be considered after ensuring the absence of infection. Medical management should include tetanus prophylaxis, antibiotic coverage, and rabies vaccination.[5],[8]
Complex elbow dislocations are challenging injuries that can result in significant patient morbidity, including posttraumatic arthritis and chronic instability. Evaluation of such complex injuries should include a thorough history and physical examination. Proper radiographic evaluation before and after joint reduction, including a computed tomography scan, is valuable for injury evaluation and surgical planning. Temporary external fixation of the elbow joint can be applied initially, and the definitive management, including coronoid fracture fixation and ligaments reconstruction, if needed, should be carried out as early as soft tissue condition allow.[9]
In our case, the multiple deep bites necessitated two sessions of irrigation and debridement. Due to the presence of elbow instability, we transfixed the elbow joint for 3 weeks. Furthermore, the soft tissue condition prevented the coronoid and ulna fracture definitive fixation. We were worried about the persistence of the instability. However, after the hinge brace was removed in the outpatient clinic, the elbow examination showed no varus or valgus rotatory instability, so we proceeded with physiotherapy to maintain a functional range of motion.
In the later follow-ups, the radiographic assessment showed arthritic changes of the elbow joint. Although the initial injury may have contributed to this, ideally earlier fixation of the coronoid fracture and repair or reconstruction of the lateral ulnar collateral ligament would have helped prevent or delay it.
Conclusion
Camel bites should be taken seriously as it can result in severe, devastating injuries. Camel gripping of the extremity should raise the suspicion of multiple injuries, so careful assessment of the entire extremity should be carried out. Proper surgical and medical management can prevent unpleasant outcomes.
Ethical consideration
This study was approved by the ethical committee of our institution. The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published, and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
YAA and MAK conceived and designed the study, and IMA, FKA, and FAM collected and organized data, while YAA, IMA, and FKA wrote the initial and final draft of the article and provided critical input. All authors have critically reviewed and approved the final draft and are responsible for the manuscript's content and similarity index.
| 1. | Ali FM, Krishnan S, Farhan MJ. A case of ipsilateral shoulder and elbow dislocation: An easily missed injury. J Accid Emerg Med 1998;15:198. [Google Scholar] |
| 2. | Janjua KJ, van den Berg AA. Animal injuries presenting to Riyadh Armed Forces Hospital: A survey. Trop Doct 1994;24:84. [Google Scholar] |
| 3. | Abu-Zidan FM, Hefny AF, Eid HO, Bashir MO, Branicki FJ. Camel-related injuries: Prospective study of 212 patients. World J Surg 2012;36:2384-9. [Google Scholar] |
| 4. | Saxena PS, Sharma SM, Singh M, Saxena M. Camel bite injuries. J Indian Med Assoc 1982;79:65-8. [Google Scholar] |
| 5. | Calleo VJ, Curtin PO, Biondich AS. Camel bites: A case study with a summary of current epidemiology, injury patterns, and treatment modalities. Wilderness Environ Med 2018;29:380-2. [Google Scholar] |
| 6. | Cobanoğlu M, Yumrukcal F, Karataş C, Duygun F. Simultaneous shoulder and elbow dislocation. BMJ Case Rep 2014;2014:bcr2014204686. [Google Scholar] |
| 7. | Meena S, Saini P, Rustagi G, Sharma G. Ipsilateral shoulder and elbow dislocation: A case report. Malays Orthop J 2012;6:43-5. [Google Scholar] |
| 8. | Green D, Wolfe S, Hotchkiss R, Pederson W, Kozin S, Cohen M. Green's Operative Hand Surgery. Philadelphia: Elsevier; 2017. [Google Scholar] |
| 9. | Wyrick JD, Dailey SK, Gunzenhaeuser JM, Casstevens EC. Management of complex elbow dislocations: A mechanistic approach. J Am Acad Orthop Surg 2015;23:297-306. [Google Scholar] |
Fulltext Views
3,847
PDF downloads
2,110





