Translate this page into:
Large intramuscular and parosteal lipoma of the upper limb: A case report and literature review
*Corresponding author: Khalid Alghamdi, SBOS. Department of Orthopedic Surgery, Security Forces Hospital, Riyadh, Saudi Arabia. khalid-ghamdi@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Alghamdi K, Alshayie M. Large intramuscular and parosteal lipoma of the upper limb: A case report and literature review. J Musculoskelet Surg Res. 2024;8:75-80. doi: 10.25259/JMSR_183_2023
Abstract
Although lipomas are the most common benign soft-tissue tumors, the intramuscular type is rare and the parosteal type is even rarer. These types of tumors can present like malignant tumors like liposarcoma. Unlike superficial lipomas, deep lipomas (intramuscular/parosteal) require magnetic resonance imaging to evaluate for and rule out malignant features. We report this patient with giant and mixed types of rarest lipomas (intramuscular and parosteal) that arise from the humeral periosteum and within the brachioradialis muscle with encasement of the radial nerve. We aimed to increase awareness to think outside the box and shed light on this giant, rarest mixed type of intramuscular and parosteal lipomas. Furthermore, it emphasizes the need for careful investigations to rule out malignant tumors like liposarcoma. Finally, many orthopedic oncology centers designate large, deep lipomas as low-grade liposarcoma due to the risk of local recurrence.
Keywords
Intramuscular lipoma
Liposarcoma
Parosteal lipoma
Periosteum
Soft-tissue neoplasms
INTRODUCTION
One percent of soft-tissue lumps are malignant, while lipomas are the most common benign soft-tissue tumors managed by surgeons. The majority of lipomas is asymptomatic and can be superficial or deep. Lipomas in deeper layers can be classified as inter or intramuscular, infiltrative, and rarely parosteal (near the bone periosteum) lipomas. Careful attention is mandatory for lipomas >5 cm or deep to the fascia, which require a magnetic resonance imaging (MRI) before surgery. Unplanned resection of sarcoma as a lipoma will lead to increased patient morbidity and loss of the chance of limb salvage procedure and end up by amputation. This is why a better understanding of lipomas is required and proper referral is necessary. Many orthopedic oncology centers designate large, deep lipomas as low-grade liposarcoma due to the risk of local recurrence. As orthopedic surgeons, we need to manage a lipomatous soft-tissue tumor when they are near the site of an intended standard orthopedic procedure.[1,2]
Intramuscular lipomas incidence is <1% of all lipomas; its cause is still unknown. As it is deep to the fascia where the muscle is found, it presents like a malignant soft-tissue tumor. This is why it is crucial to do an MRI.[3] While the incidence of parosteal lipoma is 0.3% of all lipomas and 0.1% of primary bone tumors.[4]
We aimed to increase awareness to think outside the box and shed light on this large, rarest mixed type of intramuscular and parosteal lipomas. Furthermore, it emphasizes the need for careful investigations to rule out malignant tumors like liposarcoma.
CASE REPORT
A 54-year-old diabetic and hypertensive female presented with a slowly progressive, painless swelling of her left arm for 5 years, which has recently and gradually become a cause of discomfort. The patient denied any itchiness, pain, bleeding, or drainage at the same site. In addition, she denied any history of trauma, weight loss, or radiation exposure.
On examination, the swelling was located on the left distal anterolateral arm with no skin changes. It was a rubbery, non-tender, well-circumscribed, dome-shaped, mobile mass with elbow motion, measuring 8.5 cm × 4 cm, with no lymphadenopathy identified and intact distal neurovascular examination.
A plain radiograph showed no clear endosteal scalloping of the humeral cortex but tiny cortical radiolucency on the anterior distal humeral cortex. Furthermore, soft-tissue shadows with septations were seen over the distal anterolateral arm [Figures 1 and 2]. MRI showed a high signal intensity mass that arose from the mid-lateral humerus periosteum and ran within the brachioradialis muscle and nearly covered the entire muscle diameter. Unfortunately, the radial nerve was adherent to the capsule. Furthermore, it showed a classic lipoma signal, which is bright in T1, intermediate in T2, and suppressed in fat [Figures 3-5]. After discussing and confirming with the radiologist that this was a benign parosteal and intramuscular lipoma, the case was discussed thoroughly with the patient, which included but was not limited to the risk of radial nerve palsy and she opted for surgical excision.

- A plain radiograph of the left humerus shows no clear endosteal scalloping of the humeral cortex, but soft-tissue shadows with septations are seen over the distal anterolateral arm.

- A plain radiograph of the left humerus shows soft-tissue shadows with septations over the distal anterior arm and just posterior to this septation. There is tiny cortical radiolucency.
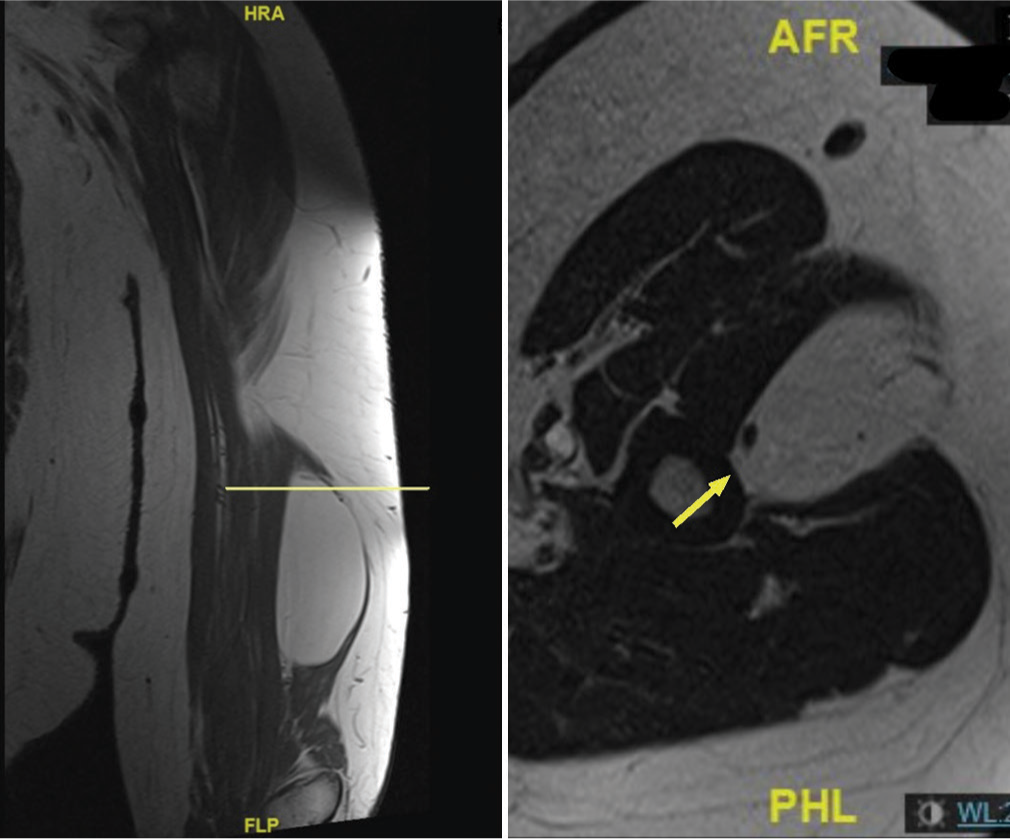
- Magnetic resonance imaging with synchronized coronal (T1) and axial (T2) cuts. On the coronal view, the level is set on the proximal lipoma, and on the axial view, we can see the proximal attachment of the lipoma to the bone periosteum (arrow). Coronal T1 showed a bright signal, and axial T2 showed an intermediate signal, which is classic for lipoma.
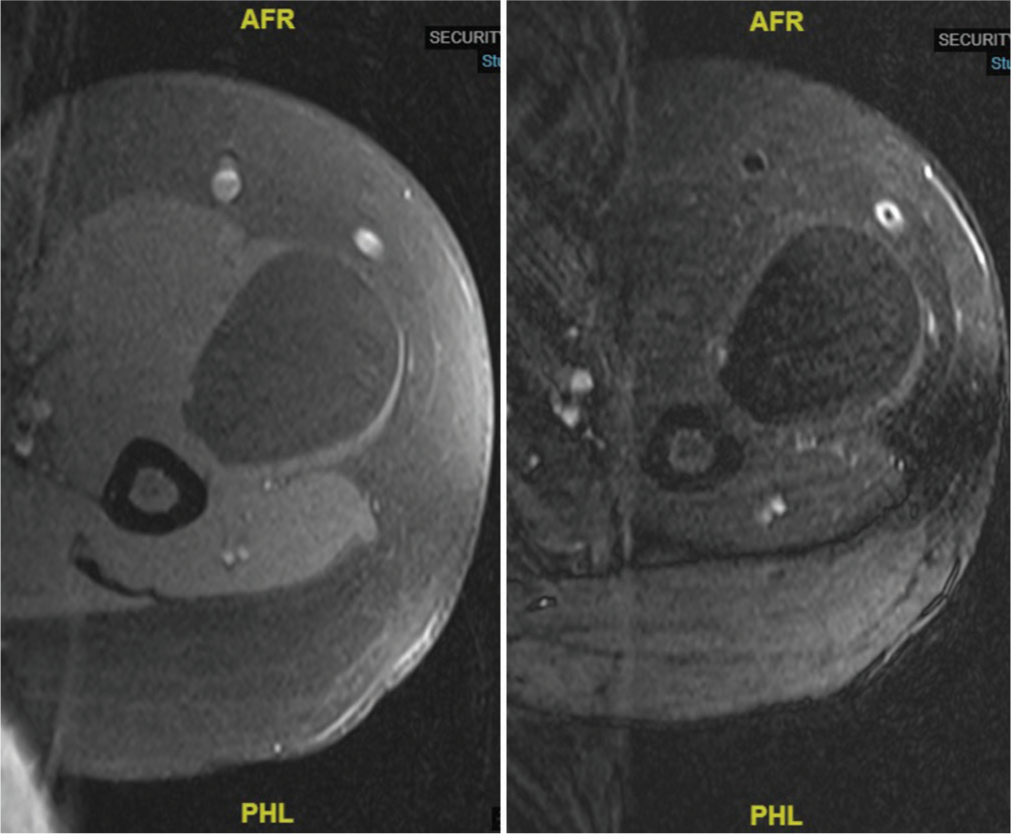
- Magnetic resonance imaging axial T1 (left) and T2 (right) fat suppression cuts showed a suppressed signal, which is classic for lipoma.
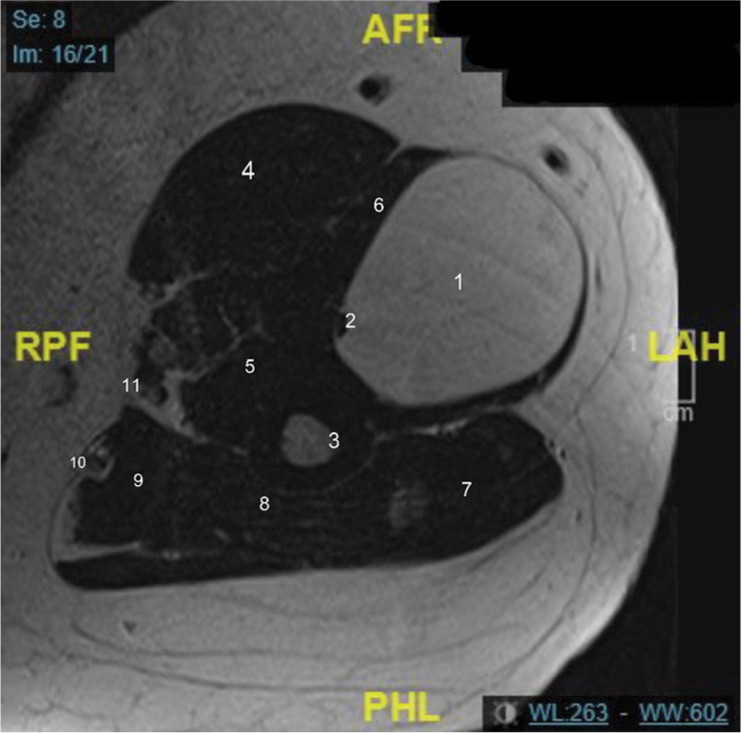
- Magnetic resonance imaging axial (T2) cut with labels as follows. 1: Lipoma, 2: Radial nerve, 3: Humerus, 4: Biceps brachii muscle, 5: Brachialis muscle, 6: Brachioradialis muscle, 7: Lateral head of triceps muscle, 8: Medial head of triceps muscle, 9: Long head of triceps muscle, 10: Ulnar nerve, 11: Median nerve.
On the day of surgery, the patient was placed supine with an arm board under sedation and a brachial plexus block. The usual sterile prepping and draping were done and prophylactic antibiotic was given. The skin marking was done around the edges of the lipoma and a skin incision over the midline of the lipoma was done. Subcutaneous dissection was done, the cephalic vein was identified and protected, the lipoma capsule was protected, and a circumferential dissection was done [Figure 6]. The radial nerve, which was seen on the posteromedial aspect of the capsule, was freed and protected. The capsule was attached proximally to the bone periosteum, which was released and then the lipoma was removed. On the back table, a lipoma measured 12 cm × 5 cm × 5 cm [Figure 7]. The wound was irrigated and closed in layers and dressing was applied. The patient was doing fine in recovery with no wrist or fingers drop and was discharged home. A two-week follow-up showed a healing wound with normal distal neurovascular examination. The final histopathology report confirmed our pre-operative diagnosis as benign mature adipose tissue, also another slice from the tissue sample showed mature adipose surrounded by fibrous tissue (periosteum) consistent with parosteal lipoma [Figures 8 and 9].

- Intra-operative picture showing the lipoma on the distal anterolateral arm after partial dissection and release.

- Intra-operative picture showing the excised lipoma on the back table measuring around 12 cm × 5 cm × 5 cm.

- Microscopic photos of the same sample showed a benign mature adipose tissue.
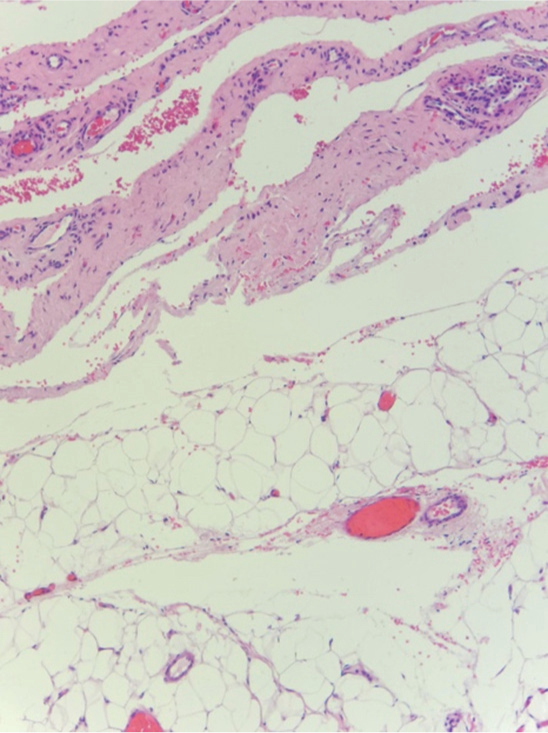
- Another slice from the tissue sample showed mature adipose surrounded by fibrous tissue (periosteum) consistent with parosteal lipoma.
DISCUSSION
A more than 5 cm size of a lipoma is categorized as a giant lipoma. It can be symptomatic as it will act as a space-occupying lesion, especially if it is located within a smaller upper limb muscle, like the brachioradialis. As in our case, it is crucial to check preoperatively and postoperatively the presence of motor or sensory deficit of the encroachment neurovascular structures. In addition, we cannot emphasize more on the importance of MRI to rule out features of liposarcoma or atypical lipomatous tumors.[5] Moreover, features of intramuscular lipoma could resemble a well-differentiated liposarcoma, which makes it difficult to distinguish. Many orthopedic oncology centers designate large, deep lipomas as low-grade liposarcoma due to the risk of local recurrence.[5,6] Lipomas located superficial to the facia have high sensitivity and specificity with ultrasound. However, lipomas deep in the fascia have more varied features on ultrasound. For preliminary investigation, ultrasonography is good, but MRI is superior, especially for pre-operative planning.[7] In general, lipomas are benign with no malignancy transformation and do not require referral to an orthopedic oncologist. The treatment is observation if asymptomatic, but if the mass is symptomatic, growing, or the patient has cosmetic concerns, and the treatment is marginal excision. If there is an incidental finding of a lipoma in relation to a planned orthopedic surgery, treatment options are as mentioned earlier. If located superficial to the fascia and <5 cm, it can be treated with excisional biopsy without prior MRI. However, if it is >5 cm or deep to the fascia, an MRI is a must before any surgical intervention. The local recurrence of lipomas is <5% but increases with infiltrating intramuscular lipomas.[1,8-10] The features favor well-differentiated liposarcoma include size >10 cm, percent fat <75%, thick or nodular (>2 mm) septa, nodular/globular areas, prominent high T2 signal foci, prominent enhancement, associated non-adipose mass, lower limb location, and intramuscular location. The features that favor lipoma include size <10 cm, percentage fat >75%, no or few thin (<2 mm) septa, no or minimal enhancement, no or minimal high T2 signal foci, and subcutaneous location.[11-13] A comprehensive literature review was done in both intramuscular and parosteal lipomas of the upper limb [Table 1].
| Reference | Type of lipoma | Sex | Age (years) | Symptoms | Duration of symptoms | Dimensions (cm) | Location | Treatment |
|---|---|---|---|---|---|---|---|---|
| Allagui et al.[14] |
IM | F | 48 | Inability to extend the fingers of the left hand (PIN compression) | 6 months | 5×3 | Forearm (supinator) | Surgical excision; recovered and no recurrence |
| Toft[15] | IM | M | 71 | Cosmetic | 8 months | 7×3×1 | Arm (biceps brachii) | Surgical excision; no comment on follow-up |
| Park et al.[16] | IM | F | 49 | Shoulder pain | 2 months | 4×2×1 | Shoulder (infraspinatus) | Surgical excision: pain resolved |
| D’Alfonso and Shin[17] | IM | F | 63 | Incidental while a routine mammogram | - | 2×1×1 | Breast (pectoralis) | Conservative for clinical follow-up |
| Balabram et al.[18] | IM | F | 58 | Axillary lump | - | 9 | Axilla (subscapularis) | Surgical excision; no comment on follow-up |
| Berlund and Kalamaras[19] | IM | M | 46 | Painful wrist triggering with associated carpal tunnel syndrome | months | 1.5×1×1 | Hand (lumbrical) | Surgical excision; recovered and no recurrence |
| Papakostas et al.[20] |
IM | M | 59 | Numbness index finger | 2 years | 4×3×2 | Hand; dorsal 1st web space (? dorsal interosseous) | Surgical excision; recovered and no recurrence |
| Tuaño et al.[21] |
IM | F | 62 | Pain, weakness, and paresthesias of forearm and hand | 1 year | - | Forearm (flexor carpi ulnaris) | Surgical excision, cubital tunnel release, and ulnar nerve transposition; recovered |
| Byeon et al.[22] |
IM | F | 42 | Forearm lump | 6 months | 2×5 | Forearm (extensor pollicis brevis) | Surgical excision; recovered and no recurrence |
| Huang et al.[23] |
IM | F | 48 | Catching sensation during wrist motion and a progressive tingling sensation on the palmar aspect of the hand | 2 years | 2.5×2×2 | Wrist (flexor digitorum superficialis) | Surgical excision; recovered and no recurrence |
| Al-Mnayyis et al.[24] |
P | M | 33 | Pain and swelling anterior proximal forearm | - | 4×3×5 | Forearm (supinator) with internal radial bone protuberance | Surgical excision; recovered and no recurrence |
| Yadav et al.[4] |
P | M | 45 | Swelling at the base of the middle finger | 3 years | 4×3×4 | Proximal phalanx | Surgical excision; recovered and no recurrence |
| Vikas et al.[25] |
P | F | 54 | Weak MCP joints extension | 5 months | 4×3 | Forearm (proximal shaft and neck of radius) | Surgical excision; recovered and no recurrence |
| Murugharaj et al.[26] |
P | M | 55 | Mechanical block to the elbow movement | 30 years | 8×8×4.5 | Forearm (radius) | Surgical excision; recovered and no recurrence |
IM: Intramuscular, P: Parosteal, M: Male, F: Female, MCP: Metacarpophalangeal
CONCLUSION
MRI is a must in such atypical cases, especially for pre-operative planning and to avoid injury to adherent neurovascular structures. Moreover, atypical lipoma is often not differentiated from classic lipoma until after marginal excision, where histology shows greater cellularity with a higher chance of local recurrence and is usually large and deep. The bottom line is that classic lipoma can be treated as an atypical lipoma (well-differentiated liposarcoma) by adequate marginal excision.
AUTHORS’ CONTRIBUTIONS
KA contributed to patient diagnosis, evaluation, management, and follow-up. Also, contributed to the literature review, data analysis and major role in paper writing. MA contributed to patient diagnosis, evaluation, management, and follow-up. Also, contributed to case supervision. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
Ethical approval
Institutional Review Board approval is not required.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patients consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Lipomatous soft-tissue tumors. J Am Acad Orthop Surg. 2018;26:779-88.
- [CrossRef] [PubMed] [Google Scholar]
- A case report on parosteal lipoma stretching the posterior interosseous nerve without causing palsy. Cureus. 2021;13:e14776.
- [Google Scholar]
- Intramuscular lipoma of the scapular region. Dermatol Online J. 2021;27:D327754370.
- [CrossRef] [PubMed] [Google Scholar]
- Parosteal lipoma of the proximal phalanx of hand. J Hand Surg Am. 2021;46:933.e1-5.
- [CrossRef] [PubMed] [Google Scholar]
- Upper extremity mass with lipomatous axillary involvement and multiple level encasement of the brachial plexus. Radiol Case Rep. 2022;17:4893-8.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomical distribution of intramuscular lipomas. J Forensic Sci Res. 2017;1:35-9.
- [CrossRef] [Google Scholar]
- The diagnostic accuracy of ultrasonography for soft tissue lipomas: A systematic review. Acta Radiol Open. 2017;6:2058460117716704.
- [CrossRef] [PubMed] [Google Scholar]
- WHO classification of soft tissue tumours: An update based on the 2013 (4th) edition. Pathology. 2014;46:95-104.
- [CrossRef] [PubMed] [Google Scholar]
- From the archives of the AFIP: Benign musculoskeletal lipomatous lesions. Radiographics. 2004;24:1433-66.
- [CrossRef] [PubMed] [Google Scholar]
- Intramuscular lipoma of the lower limb. Long-term follow-up after local resection. J Bone Joint Surg Br. 1989;71:812-5.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of fatty tumors: Distinction of lipoma and well-differentiated liposarcoma. Radiology. 2002;224:99-104.
- [CrossRef] [PubMed] [Google Scholar]
- Lipomas, lipoma variants, and well-differentiated liposarcomas (atypical lipomas): Results of MRI evaluations of 126 consecutive fatty masses. AJR Am J Roentgenol. 2004;182:733-9.
- [CrossRef] [PubMed] [Google Scholar]
- From the archives of the AFIP: imaging of musculoskeletal liposarcoma with radiologicpathologic correlation. Radiographics. 2005;25:1371-95.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior interosseous nerve syndrome due to intramuscular lipoma. Eur Orthop Traumatol. 2014;5:75-9.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical resection of a giant intramuscular lipoma of the biceps brachii: A case report and review of the literature. Arch Orthop Trauma Surg. 2022;142:373-9.
- [CrossRef] [PubMed] [Google Scholar]
- Painful intramuscular lipoma of the infraspinatus: Unusual location and presentation. Orthopedics. 2016;39:e370-3.
- [CrossRef] [Google Scholar]
- Intramuscular lipoma arising within the pectoralis major muscle presenting as a radiographically detected breast mass. Arch Pathol Lab Med. 2011;135:1061-3.
- [CrossRef] [PubMed] [Google Scholar]
- Intramuscular lipoma of the subscapularis muscle. Sao Paulo Med J. 2014;132:65-7.
- [CrossRef] [PubMed] [Google Scholar]
- A case report of trigger wrist associated with carpal tunnel syndrome caused by an intramuscular lipoma. Hand Surg. 2014;19:237-9.
- [CrossRef] [PubMed] [Google Scholar]
- Ulnar nerve compression at the elbow secondary to intramuscular lipoma of the flexor carpi ulnaris: A case report. JBJS Case Connect. 2023;13:e2300108.
- [CrossRef] [PubMed] [Google Scholar]
- Recurrent intramuscular lipoma at extensor pollicis brevis: A case report. World J Clin Cases. 2023;11:684-91.
- [CrossRef] [PubMed] [Google Scholar]
- Trigger finger at the wrist caused by an intramuscular lipoma within the carpal tunnel: A case report. World J Clin Cases. 2021;9:7564-71.
- [CrossRef] [PubMed] [Google Scholar]
- Parosteal lipoma of the forearm: A case report and a literature review. Medicine (Baltimore). 2021;100:e27876.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior interosseous nerve entrapment due to bilobed parosteal lipoma. J Clin Orthop Trauma. 2020;11:S174-6.
- [CrossRef] [PubMed] [Google Scholar]
- Parosteal lipoma of proximal radius: A case report of an unusual swelling and review of literature. J Orthop Case Rep. 2019;9:46-8.
- [Google Scholar]







