Translate this page into:
Management of subtrochanteric fractures of femur: A narrative review
2 Department of Orthopaedics, Hamdard Institute of Medical Sciences and Research, New Delhi, India
3 Department of Orthopaedics, JPN Apex Trauma Centre, AIIMS, New Delhi, India
Corresponding Author:
Arvind Kumar
Department of Orthopaedics, Hamdard Institute of Medical Sciences and Research, New Delhi
India
arvindmamc@gmail.com
| How to cite this article: Ashraf J, Kumar A, Khan R, Mittal S. Management of subtrochanteric fractures of femur: A narrative review. J Musculoskelet Surg Res 2020;4:72-81 |
Abstract
Subtrochanteric fractures constitute complex proximal femoral fractures. These fractures are often associated with complications related to fracture union, loss of reduction, and implant failure. Reduction and stable fixation have been implicated as the major predictors for favorable outcomes. This narrative review briefly discusses various aspects of the management of subtrochanteric fractures along with various technical tips, which are helpful in achieving a satisfactory reduction of these fractures.
Introduction
Subtrochanteric fractures are among the less common variants of proximal femoral fractures and usually result from high energy trauma.[1] However, in the elderly population, such fractures can often result from trivial falls, due to their osteoporotic bone, and may also present as atypical fractures in the bisphosphonate-treated bones. The treatment of subtrochanteric fractures is not simple because of the complex and strong muscle forces around the proximal femur that prevents the reduction in these fractures. This zone is also at risk of malalignment as it forms the major load transmission zone from hip to thigh.[2] With the ever-evolving literature concerning the management of subtrochanteric fractures, it has been advocated that the quality of reduction and its maintenance play a vital role in favorable outcomes of these fractures.[3],[4] Inadequate reduction often results in varus collapse, malunion, and nonunion of the subtrochanteric fractures.[3],[4],[5] Therefore, careful preoperative planning and its execution are required for obtaining and maintaining a well-aligned reduction of the subtrochanteric fractures to avoid complications related to fracture healing. Contrary to the earlier concerns of impairment of the fracture vascularity with open techniques affecting fracture healing, no such evidence is available against a well-reduced fracture treated with open techniques.[4],[5],[6] The present review is aimed at discussing the various aspects related to the management of subtrochanteric fractures that are crucial in obtaining an appropriate reduction, stable fixation, and satisfactory outcomes.
Classification
The subtrochanteric fractures are defined as fractures within 5 cm distal to the lesser trochanter.[7] The classification forms an important aspect in the management of subtrochanteric fractures. One of the main characteristics that differentiate the subtrochanteric fracture pattern for other femoral fractures is a great difficulty in the reduction of the proximal fragment. Even simple-looking fractures can pose a major challenge in the reduction because the iliopsoas and hip abductors pull the proximal fragment in flexion and varus, respectively, which make the close reduction quite difficult in a supine position with traction applied. Interestingly, the comminuted fractures where lesser trochanter is avulsed may not displace the proximal fragment as much, making the reduction much easier.
These fractures may require some additional maneuvers and tricks to obtain appropriate reduction and stable fixation. There are several classifications for subtrochanteric fractures. Among the classic ones, the classification by Fielding,[8] based on the distance of fracture from the level of the lesser trochanter, has seldom been used due to its low reproducibility. On the other hand, the Russell–Taylor classification has better clinical implications as it considers the details of the complexity of fracture being adopted for classification. The involvement of piriformis fossa and lesser trochanteric comminution are important parameters for surgical planning. The Seinsheimer classification is probably the most anatomical classification for subtrochanteric fractures as it counts in the number and type of fractured fragments, which again are important in surgical planning.[9] The new AO classification provides a grading based on the fracture complexity and location.[10] The subtrochanteric fractures are classified as proximal diaphyseal injuries with a numeric code of “32,” depicting the diaphyseal region of the femur followed by a capital alphabet describing the complexity of the fracture, A for simple fractures, B for wedge fractures, and C for segmental and multifragmentary fractures. This is followed by a numeric code (1, 2, 3) which describes the fracture severity and a qualifier letter (a, b, c, i, j, k) describing the extent of the fracture. Although it is one of the most comprehensive classifications and also recommended by the Orthopaedic Trauma Association (OTA), it has a limitation in the morphological depiction of complex fractures. For example, a subtrochanteric fracture with two or three intermediate fragments between the proximal and distal segments and another subtrochanteric fracture with extensive intermediate comminution will both be classified as 32C3(i) injury. While the fracture reduction in the former may require a simple cerclage around to the fragments followed by conventional intramedullary nailing, the latter may require a bridging fixation without disturbing the comminuted fragments. Similarly, it is hard to convey the information regarding secondary fracture lines exiting the piriformis fossa or away from that on the basis of this classification that can play a major role in surgical planning.
It is difficult to devise all in one fracture classification, and most subtrochanteric fractures are different from each other in one or more aspects. The AO fracture classification is simple and good for the purpose of communication. However, the fracture details should be documented in the patient records, and surgical planning needs to be based on those details.
Implant Selection
To date, the devices used for the definitive fixation of subtrochanteric fractures include dynamic hip screw (DHS), dynamic condylar screw (DCS), angled blade plates, locking plates, and intramedullary nails. Although there have been studies showing the effectiveness of each of these devices, the DHS and DCS carry a higher risk of loss of reduction, implant failure, and need for reoperation in general [Figure - 1].[11]
 |
| Figure 1: Dynamic condylar screw carries a high risk of implant failure (a) and varus collapse (b) in unstable subtrochanteric fractures |
The literature in support of blade plates and locked plates is limited.[12],[13] However, they provide a more stable fixation when compared to the barrel plates. The most consistent results concerning the stable fixation and its maintenance and the biomechanical superiority belong to the intramedullary fixation devices.[3],[4],[13],[14] The cephalomedullary nails should be preferred when trochanteric locking nails do not provide adequate working length. In certain fractures where comminution is severe to an extent that an intramedullary device can actually create more fracture displacement, the blade plates and locking plates are more useful [Figure - 2]. The plates are also helpful in cases where intramedullary nails are difficult to insert as in narrow intramedullary canal, both in cases with severe deformities, which could result in malalignment with the nail insertion, and in cases where better screw purchase and stability are required as in periprosthetic fractures. Besides these, the plates should always be kept as backup options for a failed intramedullary nailing procedure. These plates can be applied over the lateral aspect of the proximal femur, while the fracture alignment remains maintained on a traction table or using manual traction. A closed or open reduction is obtained before the plate application. A lateral approach is used for the plate application that can be minimally invasive if the closed reduction is satisfactory. For multifragmentary fractures, the fragments are reduced and secured with multiple Kirschner wires (K-wires) entering the bone away from the desired plating area. The plate can then be applied to a provisionally reduced fracture. For unstable fractures, the proximal fractured segment can first be secured with the proximal portion of the plate, and then, the distal portion of the plate is aligned with the remaining shaft.[15] The angle-stable construct of the locking plates and angled blade plates can thus help in reducing the unstable fractures with this easy maneuver. Once proper alignment is obtained between the proximal and distal segments, the lower segment screws can be inserted.
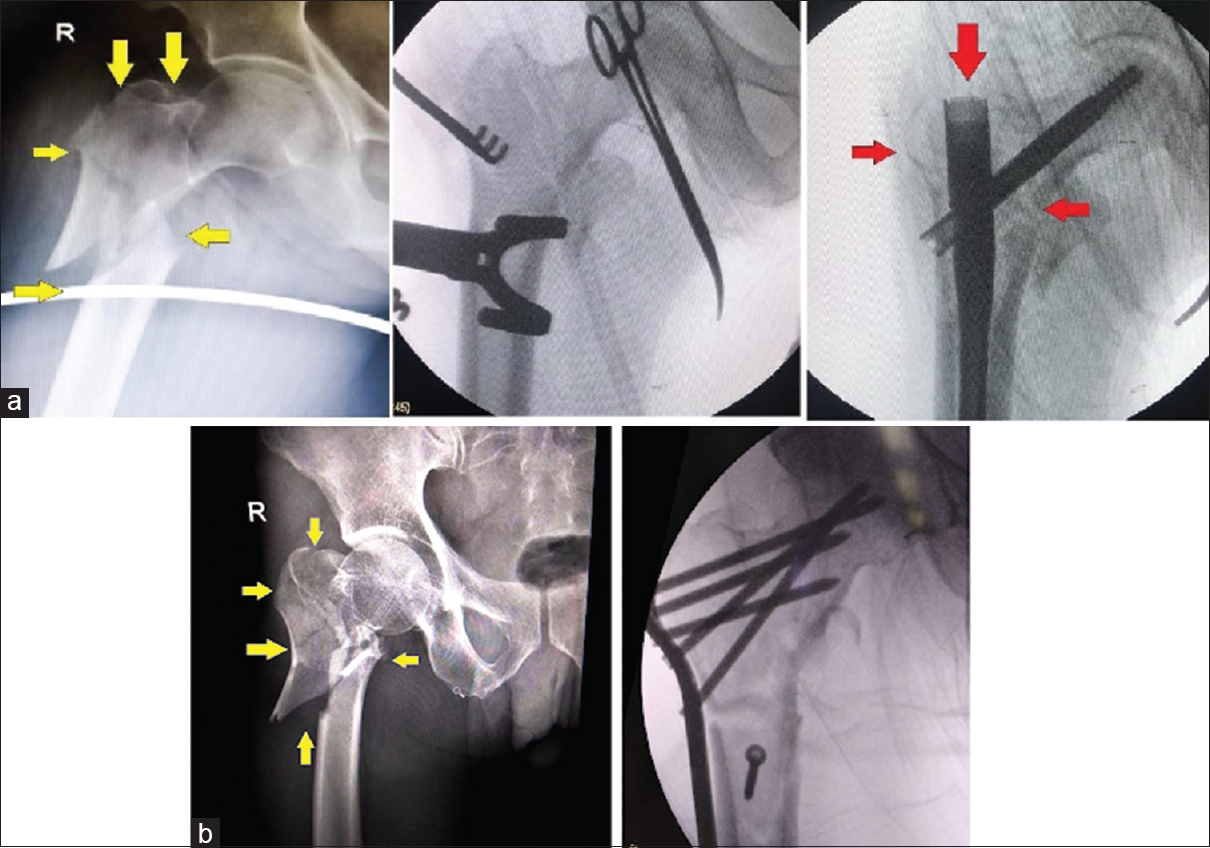 |
| Figure 2: (a) In unstable fracture patterns with multiple fracture lines involving trochanteric fossa and lateral wall, cephalomedullary nail insertion can actually displace the fragments with opening up a well-reduced fracture and cause malreduction. (b) Such fracture should be better treated with plate fixation that allows maintenance of reduction and stable fixation |
The results of proximal femoral locking plates have been inconsistent, and more evidence is still needed to comment upon the same.[16],[17]
The intramedullary devices should be the preferred modality for the fixation of subtrochanteric fractures, due to their biomechanical superiority and higher rates of fracture consolidation.[18] The plating methods should be kept as backup options for fractures with extensive comminution or in fractures where the fragments are difficult to stabilize during the various steps of serial reaming and nail insertion. Minimally invasive methods with minimal interference with the comminution zone should be used for fracture reduction whenever feasible to preserve the fracture biology.
Patient Positioning
Both conventional surgical and fracture tables have been used for operating on subtrochanteric fractures. In a conventional table, when using lateral position, there is an ease of entry point as well as better directional control for proximal reaming. However, caution should be exercised to prevent varus angulation at the fracture site due to the pull of abductors on the proximal fragment and/or due to the pull of adductors and gravity on the distal fragment. In simple fractures, once the fracture length is restored, the reduction has its own inherent stability due to muscle tension, and the assistant has easy control over the alignment. However, in comminuted fractures or unstable patterns, the assistant needs to hold the limb in a correct length and alignment, which may get disturbed with manipulation while intramedullary reaming. Once an undesirable intramedullary track is created, the nail will follow the same even if the reduction is further maintained by the assistant. Thus, complex subtrochanteric fractures in the lateral decubitus would need expert hands. In the supine position, the techniques are similar to those used on a fracture table. Either assistant holds the limb in traction, or distractor is used to maintain reduction and alignment.
The traction table is probably the most convenient arrangement for operating subtrochanteric fractures, with advantages of less workforce requirement and constant and fixed traction, which is difficult with the pull by the assistant who is bound to get fatigued to some extent with duration.[19] Second, a higher amount of traction force can be applied on a fracture table, which is helpful in countering very strong deforming forces and in late presenting cases where the manual pull by the assistant may not suffice. Third, stable traction provides a no-disturbance zone at the fracture site where other technical tips and maneuvers can be applied for fine-tuning the reduction.
Traction tables provide a controlled and hassle-free reduction and realignment of the subtrochanteric fractures [Figure - 3]. The “banana positioning” of the patient with the torso and pelvis tilted toward the contralateral side when positioned supine, helps in gaining a desirable entry point and direction of the proximal guide pin by providing clearance from the trunk and better access to the greater trochanter.[20] The contralateral hip can be flexed and abducted with calf rested on the leg support to provide space between the two limbs for image intensifier access. The “banana position” can, however, contribute to the displacement of fragments and varus angulation. Limiting the adduction to a minimum will help in preventing fracture displacement. The primary purpose of this position is to gain an appropriate entry point. Once the guide pin enters the proximal fragment, the adduction can be further reduced to bring back the fracture reduction. The area under the ipsilateral buttock should be kept clear of any hindrance to help in directing the proximal guide pin along with the anterior bow of the femur in the proximal region.
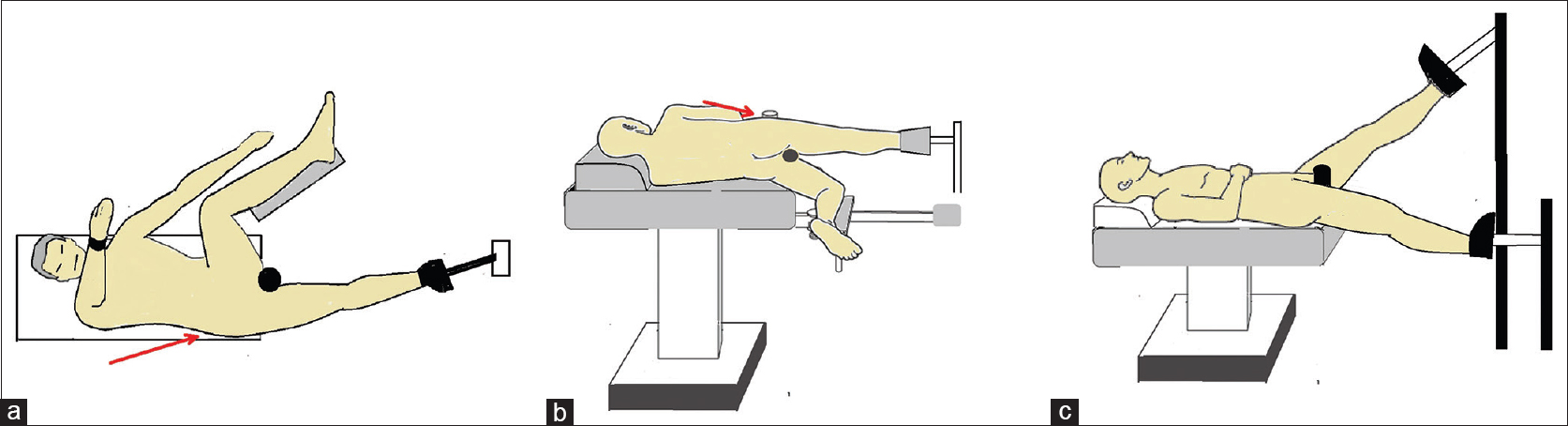 |
| Figure 3: (a) A supine “banana position” on the fracture table allows easy access to the trochanteric region and helps in directing the proximal guide pin. (b) Lateral position on the fracture table has an advantage of the nonhindering flank region, especially in obese patients. Further, the tendency of varus displacement of the proximal fragment is reduced. (c) Scissoring position is used in cases with difficult abduction and where abduction can result in complications. The operated limb is kept flexed at the hip joint and the contralateral limb is kept in a relaxed extended position |
Lateral positioning of the patient on a traction table has also been described.[19],[20],[21] The operated limb is kept on the top in a slightly flexed and adducted position, while the contralateral limb is kept flexed at the knee and in neutral alignment at the hip joint. A well-padded perineal post is kept between the two limbs with anterior attachment to the traction table. The lateral position on the fracture table offers advantages of easy access to piriformis fossa for guidewire placement with minimal obstruction from flank and trunk, especially in obese patients. The flexion of the proximal fragment gets neutralized with the flexed alignment of the limb as a whole, and the varus tendency of proximal fragment gets reduced in lateral position. Lateral position contributes to an enhanced reduction of the anterior displaced proximal femoral fragment against the central post, while this advantage may not be possible in a supine position. The scissor position in the supine decubitus is useful for patients with difficult hip abduction and where excess abduction needs to be avoided. The operated side is kept at a higher level to obtain a cross-table fluoroscopic lateral view with an image intensifier.
The advantages of the fracture tables are not without any drawbacks.[21] Just like a tourniquet, there are potential pressure sites that carry the risk of soft tissue damage and nerve compression when prolonged traction is used. The most common nerve compression with prolonged use of the traction table is the pudendal nerve, with a variable incidence being reported. Erectile dysfunction is the most common manifestation of the pudendal nerve injury. The perineal post should be well padded, and the traction should be released when duration crosses the limit of 120 min.[22] Perineal skin and soft tissue damage can occur with prolonged traction, especially in obese patients. The contralateral lower limb carries a risk of sciatic nerve palsy when a hemilithotomy position is used. A flexion of >90° at the hip and a knee flexion of <90° carry the risk of sciatic nerve stretching. The flexion of the hip should, therefore, be kept to a minimal and hemilithotomy position should be avoided. Tight strapping of the contralateral limb should be avoided as it carries a risk of compartment syndrome which can be a devastating complication. Although most of the nerve palsies recover without any intervention, few cases have unpredictable outcomes and may result in a permanent deficit.[23] Thus, it is important to release traction at intervals when surgery gets prolonged to prevent such complications.
Conventional tables are reasonably useful for simple subtrochanteric fractures as the critical step is to pass the intramedullary guidewire through the fracture site that becomes automatically realigned with cortical contact between proximal and distal segments. Constant traction may not be required, unlike the complex fractures.
Intraoperative Imaging
Fluoroscopy plays an important role in assessing intraoperative reduction, alignment, and appropriate placement of the cephalomedullary screws when newer generation nails are used. When a conventional table is used, the anteroposterior (AP) view can be taken in a usual fashion, and a lateral oblique view should be taken to avoid overlap of the contralateral limb. With the use of a fracture table, the contralateral hip and knee can be flexed and abducted to provide clear space between the two limbs for positioning of the C-arm. In cases with difficult abduction and flexion of the hip of the contralateral limb and at times as per the surgeon's preference, a scissor position of the limbs is used on the fracture table.[24] The C-arm is positioned beside the contralateral limb. Routine AP and lateral views are taken. In proximal femur, an oblique lateral view is taken to avoid overlap of the contralateral hip. A preliminary reduction should be obtained before the surgery, and both AP and lateral projections are reviewed for planning further maneuvers and techniques and also to look for the need for repositioning of the limb and table attachments that may hinder a good AP and lateral projection. Frequently, the central perineal post, which acts as a countertraction mechanism, may block the adequate view of the femoral head in the lateral projection. The post needs to be adjusted medially or laterally before surgery to obtain a clear fluoroscopic view.
Technical Considerations
The current evidence suggests that the quality of reduction alone is the chief parameter in deciding the outcomes of subtrochanteric fractures.[18],[25] Simple subtrochanteric fractures close to the diaphyseal region can be treated on similar lines to the femoral shaft fractures. The medullary canal provides an inherent counter mechanism to the reamer, and the interlocking nail prevents the displacement of fragments. The only requirement is to direct the guidewire as per the requirements of the specific nail type. As the simple fractures, well below the lesser trochanter and in the diaphyseal region of the femur, are inherently stable, the entry point need not be manipulated. For a greater trochanteric entry nail, the entry point should be kept at the trochanteric tip only. However, as for any other fractures, the fracture must be in a stable and reduced position. Attention should be paid to the fluoroscopic images when the reamer reaches the fracture site. If the fracture tends to displace with the passage of the reamer through the fracture site, it will result in a noncentral reaming and ultimately fracture displacement with nail insertion. In such cases, noninvasive methods such as a manual force to the displacing fragment and special devices such as F-device can be used as counter mechanisms [Figure - 4]. Minimally invasive tools such as bone spikes, bone levers, and percutaneous cerclage tools for oblique fractures can also be used.
 |
| Figure 4: The F-device can help in controlling the displacement of proximal as well as a distal fragment. The terminal arm of the device is kept above the thigh, and the other one is kept beneath it. The proximal thigh is then pushed downward, and the distal thigh is brought upwards by rotating the device |
As the fractures extend more proximally, the muscular forces have an increased impact on fracture displacement, thereby making it more difficult to control the proximal fragment by traction alone. The classical displacement of the proximal fragment is abduction (varus), external rotation, and flexion. The flexion component may not be profound in cases with fractured and separated lesser trochanter.
Indirect Reduction Techniques
Proximal fragment joystick
A Schanz screw or Steinmann pin is inserted in the proximal fragment in “miss the nail” zone, which is anterior or posterior to the desired path of the nail, and the proximal fragment is manipulated against the deforming forces, i.e., varus, external rotation, and flexion [Figure - 5].[26],[27] Once the alignment gets corrected, the proximal guide pin is inserted in the desired direction while the reduction is maintained by the joystick pin, followed by proximal reaming and long guidewire insertion when cephalomedullary nails are used. The head of the nail will follow the route of the proximal reamed cavity, and the joystick pin will help in maintaining the alignment both when the reamer and the nail are inserted. The Schanz screw/Steinmann pin can be removed once the guide pin for the cephalomedullary screw is inserted if any hindrance with the cephalomedullary screw is anticipated. In cases where plating is performed, the proximal fragment can be secured with multiple K-wires after realigning with Schanz screw, and the plate can then be applied in an appropriate compression or neutralization mode.
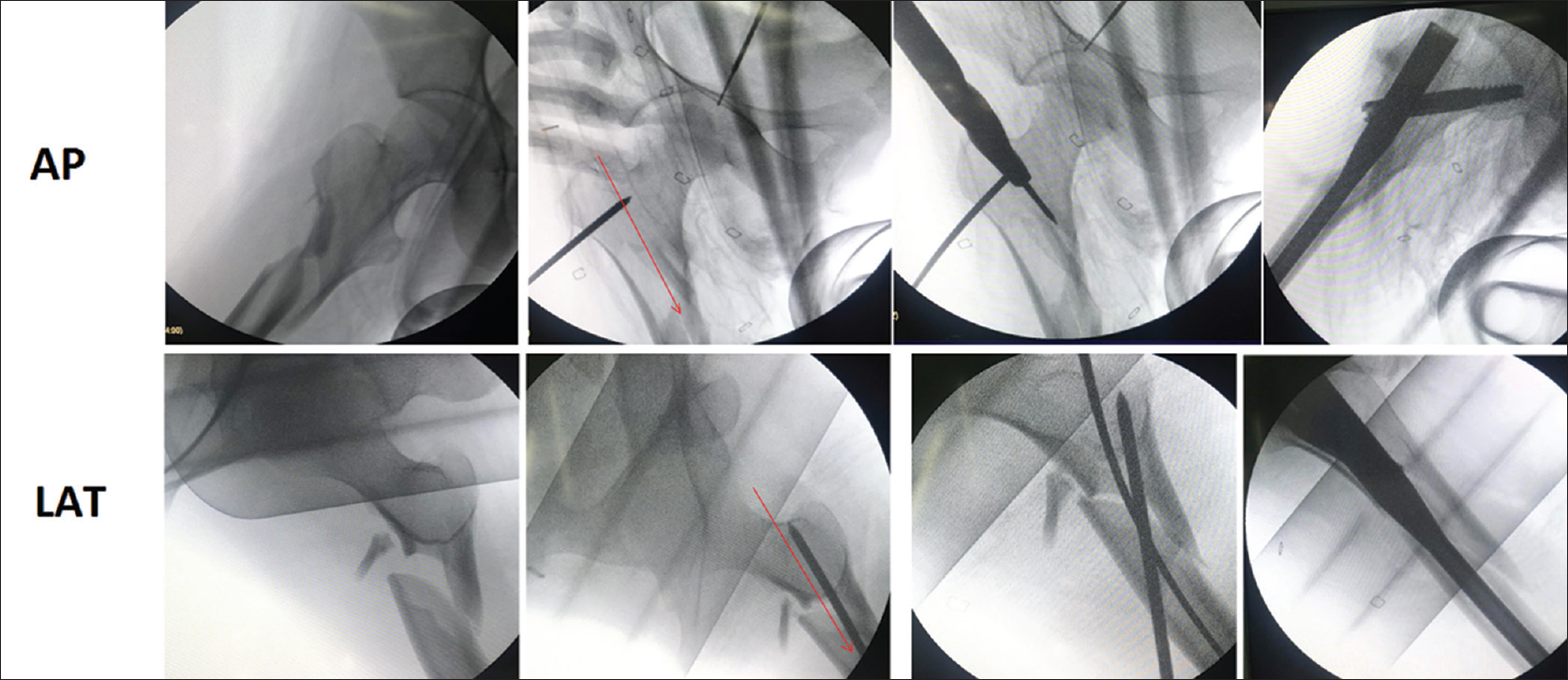 |
| Figure 5: Joystick technique: Sequential images (anteroposterior and lateral) of a displaced subtrochanteric fracture in which the proximal fragment is manipulated against the deforming forced to achieve a reduced position with the help of a Steinmann pin in the proximal fragment. The Steinmann pin is placed in such a position that it would not hinder the desired path of the nail (red line) |
Role of entry point
In simple diaphyseal fractures, the entry point should be created as per the manufacturer's guidelines. In fractures extending in proximal (trochanteric/metaphyseal region/high diaphyseal) region, which have a tendency to displace in varus with or without flexion, a modification in the entry point can actually convert the proximal angulated part of the nail into a reducing device.[28] A medial entry point (medial to the trochanteric tip) with guidewire directed slightly lateral to the proximal medial cortex can create a more vertical track than with standard trochanteric entry point [Figure - 6]. When the proximal segment of the cephalomedullary nail traverses this zone, it displaces the proximal fragment into valgus, and thus, the varus is avoided. Similarly, a posterior entry point with the guide pin directed more toward anterior cortex than posterior creates a posterior proximal to anterior distal track, which, when spanned with the proximal segment of the nail, brings an extension of the proximal fragment [Figure - 7].
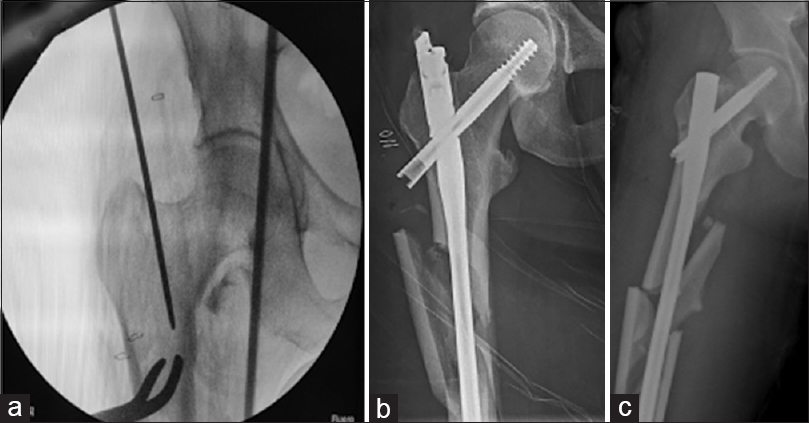 |
| Figure 6: An entry point slightly medial to the tip of the greater trochanter in anteroposterior view (a) is preferred in subtrochanteric fractures. A medial entry point prevents a varus malreduction (b), while a trochanteric entry point may result in residual varus after the nail insertion (c) |
 |
| Figure 7: (a) Subtrochanteric fractures carry a risk of residual flexion of the proximal fragment after nail insertion. (b) A posterior entry point with the guide pin directed toward anterior cortex distally in the lateral view after achieving an appropriate reduction can help in preventing residual flexion of the proximal fragment after nail insertion |
Less invasive tools
A variety of tools, when combined with stable traction and modified entry point, can help in reducing the subtrochanteric fractures.[29] A pointed ball spike can be used to correct the varus and flexion of the proximal fragment [Figure - 8]. Besides helpful in directing the proximal guide pin, it also helps in maintaining reduction during various steps of nailing. A bone lever from the proximal incision for nail insertion can be directed along the anterior cortex of the proximal femur and is helpful in controlling flexion of the proximal fragment [Figure - 9]. A collinear clamp can be used in two-part oblique fractures to control the varus displacement of the fracture. A prior percutaneous cerclage system can be used to secure fracture fragments from opening up during the reaming and nail insertion [Figure - 10]. A Poller screw can also be inserted close to the fracture site to prevent the translation of the distal or proximal fragment. The lateral translation of the proximal fragment that results in varus opening can be prevented by the insertion of a medial blocking screw in the proximal segment adjacent to the fracture. This screw blocks the passage of the intramedullary nail through the medial portion of the femoral canal, and thus, the nail engages the lateral portion of the canal, thereby preventing the lateral opening of the proximal segment. Similarly, a lateral blocking screw in the distal fragment, close to the fracture site, prevents medial translation of the distal segment, especially in reverse oblique fractures [Figure - 11].
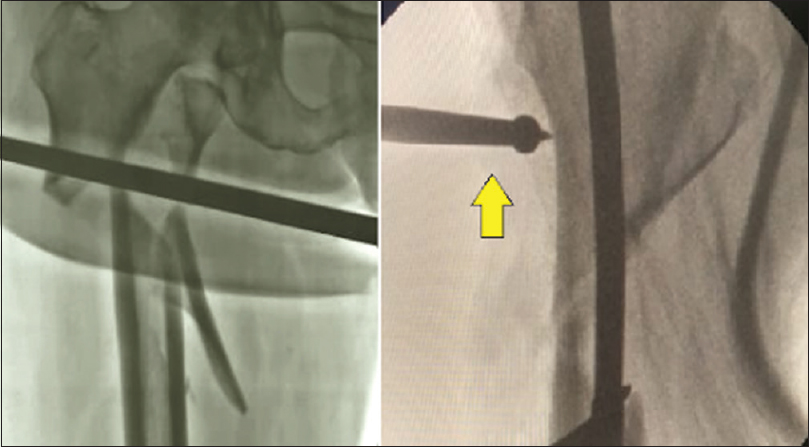 |
| Figure 8: A pointed ball spike (yellow arrow) can be used to control the displacement of the fracture fragments percutaneously during various steps of intramedullary reaming and nail insertion |
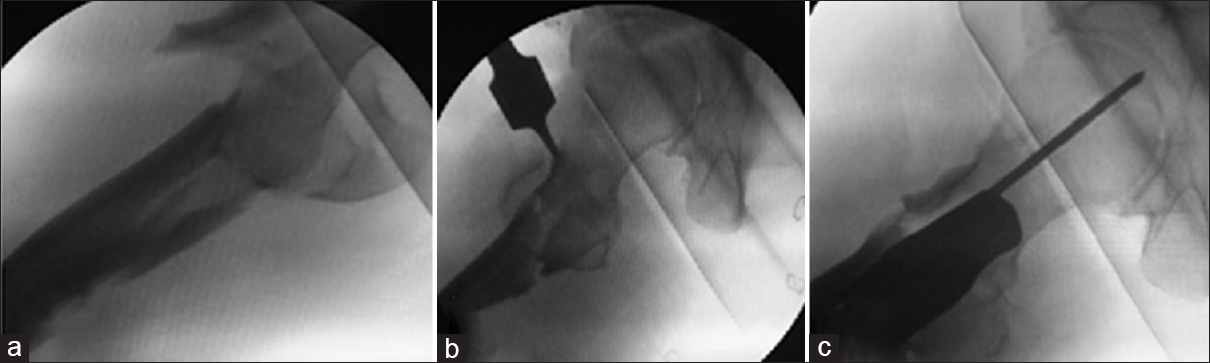 |
| Figure 9: An anterior bone lever can be brought to the anterior surface of the proximal fragment through the proximal incision for nail entry and can be used to control the flexion of the proximal fragment (a and b). The fragment becomes stable once the cephalomedullary screw guide pin is inserted (c) |
 |
| Figure 10: Percutaneous cerclage using can be performed to maintain a reduction in oblique and vertical fracture patterns |
 |
| Figure 11: A Poller screw (red circle) can be placed close to the fracture site, opposite to the direction of displacement of the concerned fragment |
Direct Reduction/open Techniques
The closed and minimally invasive techniques may not always be sufficient in obtaining a satisfactory reduction in subtrochanteric fractures, especially in those with vertical splits, reverse oblique peritrochanteric fractures, spiral fractures, and fractures with displaced lateral wall fragments. The fracture then needs to be opened up in such cases. However, all care should be undertaken to prevent devascularizing the fracture fragments. Vastus reflecting approach is preferred as it provides clean exposure to the proximal femur. The periosteum needs not to be stripped off, and a submuscular plane of reduction should be created. Single or multiple clamps can be applied to secure the fragments in their appropriate position [Figure - 12].[26],[27],[28],[29] The reduction can be secured with multiple cerclage cables, unicortical miniplates at the unstable fracture zones, or a temporary buttressing low profile plate on the lateral cortex [Figure - 13].[26],[27],[28],[29],[30],[31] The purpose of these systems is to provide a stable alignment while various steps of reaming and nail insertion are carried out. The clamp to bone assembly should be removed only after insertion of the proximal and distal interlocking screw as the fracture site may still have instability in multiple planes, and that may displace the fragments. The cephalomedullary screw and the distal screws of the nail control the primary proximal and distal fragments to prevent fracture re-displacement after clamp removal.
 |
| Figure 12: Open reduction and direct clamp-assisted reduction can be used in fractures with unstable patterns when less invasive methods fail to bring satisfactory reduction or when the fracture gets displaced during reamer or nail insertion |
 |
| Figure 13: Open reduction of the subtrochanteric fracture and application of a mini-buttress plate with unicortical screws, centered over the fracture site, can help in the prevention of lateral displacement of the proximal fragment during reaming and nail insertion |
For extramedullary fixation devices, the fragment can be temporarily stabilized with multiple K-wires or definitively with single or multiple lag screws before the plate application. Bridge plating should be preferred in extensively comminuted fractures.
Technical Considerations in the Management of Atypical and Pathological Subtrochanteric Fractures
Atypical subtrochanteric fractures are stress fractures in the proximal diaphyseal region, potentially resulting from prolonged bisphosphonate therapy.[32] Besides their atypical fracture pattern with transverse fracture of the lateral cortex extending obliquely into the medial cortex, these fractures have a high risk of progression to nonunion. The preferred management of these fractures is cephalomedullary nail fixation with over reaming of the medullary canal by a reamer 2.5 mm larger than the desired nail diameter.[33] The potential issues associated with intramedullary nail fixation are narrow medullary canal, sclerotic bone, risk of malreduction, and femoral bowing in elderly patients that does not match up with the shape of the intramedullary nail. Intramedullary nail fixation of atypical subtrochanteric fractures can often be challenging as the affected bone is already sclerotic and a slight mismatch between the curvature and shape of the nail from that of the femoral medullary canal can result in fracture malalignment that can hamper the fracture healing.[34] Similarly, the entry point of nail insertion should be selected based on the shape of the femur and angulation of the proximal part of the cephalomedullary nail. A small-diameter nail should be preferred as a well-fitting nail could actually cause malalignment with a slight mismatch with the intramedullary track.[35] Plate fixation should always be kept as backup for atypical subtrochanteric fractures.[36] Intramedullary nail insertion carries the risk of intraoperative diaphyseal fractures and distal femoral fractures during nail insertion, especially in bowed femurs and those with a narrow intramedullary canal. The plating option should be considered only when necessary as the plating does not help in endosteal healing (because the bisphosphonates remain in place), unlike the intramedullary nail insertion following reaming, and also, the plating methods create a rigid construct in the already sclerotic bone which carries the risk of delayed union. Thus, a long-spanning plate fixation should be preferred to span both metaphyseal ends that reduce the stress-risers, and also, a flexible construct should be created with widely spaced screws from the fracture site that promotes secondary healing.
Pathological subtrochanteric fractures result from the weakened bone in the subtrochanteric region of the femur. The weakened bone could result from a variety of lytic lesions. The most common cause of subtrochanteric lytic lesions in adult patients is skeletal metastasis.[37] A majority of these lesions are associated with major bone destruction. The purpose of fixation in pathological subtrochanteric fractures is to relieve pain, restore limb function, and improve quality of life. The lytic lesion that carries a risk of a future subtrochanteric fracture needs to be fixed prophylactically. The preferred modality of fixation in pathological subtrochanteric fractures is a long cephalomedullary nail that allows a stable fixation and early mobilization.[38] The weight-bearing protocol needs to be tailored on an individual basis based on the extent of the lytic lesion. These fractures carry a high risk of implant failure owing to the weakened bone and excessive stress on the nail and cephalomedullary screw junction.[39] Cement augmentation provides good stability in excessive bone loss and is an appropriate option for the patient with short-term survival. For longer life expectancy, cement augment can impair the fracture healing process and may result in nonunion and implant failure. Plate augmentation with intramedullary nailing can be done to add stability around the fracture site. For cases with extensive bone loss, endoprosthetic replacement would be a more reasonable option but has its own long-term complications such as risk of infection, loosening, metallosis, and a need for later revision.[40] Thus, the treatment modality should be decided based on the bone loss and the life expectancy of the patient. Owing to a lower risk of complications than endoprosthetic replacement, a bone-preserving modality should be preferred in patients in which long-term survival is anticipated.
Outcomes of Surgical Management of Subtrochanteric Fractures and Related Complications
Literature suggests that the complication rate in subtrochanteric fractures is high.[3-14,41-43] The major fracture healing-related complications are loss of reduction, nonunion, implant failure, and malunion of the fracture. These complications are mostly related to the quality of reduction and its fixation. Miedel et al.,[3] in their clinical study on subtrochanteric fractures, observed a high reoperation rate in fractures that had an acceptable reduction and nil reoperations in cases with good reduction. Further, contrary to the earlier popular belief of open procedures carrying the risk of complications related to fracture healing, Beingessner et al.[4] showed nil reoperation and nil wound infection in all their cases (n = 56) of subtrochanteric fractures treated with open reduction and intramedullary nailing.
Freigang et al.[25] in their retrospective study compared the factors associated with two groups of surgically managed subtrochanteric fractures, one with uncomplicated fracture healing and the other with complicated fracture healing. They observed that a satisfactory fracture reduction and slight valgization of the neck-shaft angle is associated with uncomplicated fracture healing. Another important outcome that needs to be borne in mind while following these patients is that the incidence of delayed union is as high as 50% with healing time as long as 12 months. Thus, the majority of these patients will need only observation and reassurance.
Concerning the extramedullary and intramedullary fixation, irrespective of open and closed methods, the surgical duration, operative blood loss, and length of hospital stay were found to be shorter in the extramedullary fixation group.[18] The differences between infection rates and fracture healing rates were found to be nonsignificant. Intramedullary fixation is superior to extramedullary fixation in terms of lower implant failure rates, lower risk of reoperation, and early time to weight-bearing and therefore should be the preferred modality.
Besides these, the patient lifestyle factors may also have implications on fracture healing and need to be modified on individual basis. Osteoporosis, although may not impair the healing process, is a potential cause of varus collapse, cephalomedullary screw cut out, and sometimes, implant failure as well.[42],[43] Thus, the mobilization protocol needs to be individualized to avoid complications related to the fragility of bone. In comminuted fractures, an appropriate weight-bearing protocol should be followed after the radiological signs of fracture consolidation have appeared.
The wound complications are probably related to soft tissue handling and skin condition at the fracture site. There has not been any consistent evidence, suggesting any relationship of the open techniques with wound complications.[4],[26],[27],[28],[29],[30]
Besides these, the patient comorbidities, especially systemic diseases such as diabetes, renal failure, and hypertension in the elderly group, should be considered, and all attempts should be undertaken to avoid surgical delay in these patients because evidence suggests that the general condition of patients deteriorates with the delay in surgery.[43]
Some of the complications can also be attributed to the fixation as well. A stiffer construct using multiple closely placed screws around fracture when using a locking plate can delay the healing process. Similarly, a gap at the fracture site in a statically locked intramedullary nail can impair fracture healing. Excessive periosteal stripping can damage fracture vascularity and result in unfavorable outcomes. Therefore, the general principles of fracture management should be strictly followed to achieve favorable outcomes.
Conclusion
In the management of subtrochanteric fractures, close attention should be paid on fracture morphology, and surgical planning should be done according to the fracture pattern. Stable and accurate fracture reduction or at least alignment of proximal and diaphyseal segments in comminuted fractures should be aimed for, regardless of the techniques used, closed or open. A medial entry point, use of Poller screws, indirect reduction devices, and clamps can be used to obtain accurate reduction. Intramedullary nails, preferably cephalomedullary nails, should be the implant of choice, and plating fixation methods should be preferred for comminuted multifragmentary fractures with extension proximally into the trochanteric fossa and in those where a satisfactory reduction is not achieved before the nailing process, even in simple fracture patterns. The plates come handy in cases with severely narrow femoral canal, in cases with severe femoral deformities, and in cases with periprosthetic fractures where a better screw purchase is required. A vastus reflecting approach and minimal periosteal stripping of the bone in open techniques can help in preventing soft tissue and wound complications. Finally, early surgery and tailored mobilization protocol are required to minimize the complications associated with these fractures.
Ethical consideration
This is a review article that does not involve patients or patients' information.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors' contribution
JA contributed with concept, design, manuscript preparation, manuscript editing, and manuscript review. AK contributed with data acquisition, data analysis, manuscript preparation, and manuscript editing. RK contributed with data acquisition, manuscript editing, and manuscript review. SM contributed with literature search, clinical studies, data acquisition, data analysis, manuscript preparation, manuscript editing, and manuscript review. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Charles MC, Stuart AA, Daren F, O'Toole RV. The epidemiology of fractures. In: Charles RA, David GP, Robert BW, editors. Rockwood and Green's Fractures in Adults. 7th ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams and Wilkins; 2010. p. 53-84. [Google Scholar] |
| 2. | Sims SH. Subtrochanteric femur fractures. Orthop Clin North Am 2002;33:113-26, viii. [Google Scholar] |
| 3. | Miedel R, Törnkvist H, Ponzer S, Söderqvist A, Tidermark J. Musculoskeletal function and quality of life in elderly patients after a subtrochanteric femoral fracture treated with a cephalomedullary nail. J Orthop Trauma 2011;25:208-13. [Google Scholar] |
| 4. | Beingessner DM, Scolaro JA, Orec RJ, Nork SE, Barei DP. Open reduction and intramedullary stabilisation of subtrochanteric femur fractures: A retrospective study of 56 cases. Injury 2013;44:1910-5. [Google Scholar] |
| 5. | Riehl JT, Koval KJ, Langford JR, Munro MW, Kupiszewski SJ, Haidukewych GJ. Intramedullary nailing of subtrochanteric fractures – Does malreduction matter? Bull Hosp Jt Dis (2013) 2014;72:159-63. [Google Scholar] |
| 6. | Afsari A, Liporace F, Lindvall E, Infante A Jr., Sagi HC, Haidukewych GJ. Clamp-assisted reduction of high subtrochanteric fractures of the femur. J Bone Joint Surg Am 2009;91:1913-8. [Google Scholar] |
| 7. | Kanakaris NK, Giannoudis PV. Subtrochanteric fractures. In: Lasanianos N, Kanakaris N, Giannoudis P, editors. Trauma and Orthopaedic Classifications. London: Springer; 2015. p. 317-9. [Google Scholar] |
| 8. | Fielding JW. Subtrochanteric fractures. Clin Orthop Relat Res 1973;92:86-99. [Google Scholar] |
| 9. | Loizou CL, McNamara I, Ahmed K, Pryor GA, Parker MJ. Classification of subtrochanteric femoral fractures. Injury 2010;41:739-45. [Google Scholar] |
| 10. | Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and Dislocation Classification Compendium-2018 J Orthop Trauma 2018;32 Suppl 1:S1-170. [Google Scholar] |
| 11. | Kregor PJ, Obremskey WT, Kreder HJ, Swiontkowski MF. Unstable pertrochanteric femoral fractures. J Orthop Trauma 2014;28 Suppl 8:S25-8. [Google Scholar] |
| 12. | Joglekar SB, Lindvall EM, Martirosian A. Contemporary management of subtrochanteric fractures. Orthop Clin North Am 2015;46:21-35. [Google Scholar] |
| 13. | Herscovici D Jr., Pistel WL, Sanders RW. Evaluation and treatment of high subtrochanteric femur fractures. Am J Orthop (Belle Mead NJ) 2000;29:27-33. [Google Scholar] |
| 14. | Borens O, Wettstein M, Kombot C, Chevalley F, Mouhsine E, Garofalo R. Long gamma nail in the treatment of subtrochanteric fractures. Arch Orthop Trauma Surg 2004;124:443-7. [Google Scholar] |
| 15. | Shah MD, Kapoor CS, Soni RJ, Patwa JJ, Golwala PP. Evaluation of outcome of proximal femur locking compression plate (PFLCP) in unstable proximal femur fractures. J Clin Orthop Trauma 2017;8:308-12. [Google Scholar] |
| 16. | Saini P, Kumar R, Shekhawat V, Joshi N, Bansal M, Kumar S. Biological fixation of comminuted subtrochanteric fractures with proximal femur locking compression plate. Injury 2013;44:226-31. [Google Scholar] |
| 17. | Wirtz C, Abbassi F, Evangelopoulos DS, Kohl S, Siebenrock KA, Krüger A. High failure rate of trochanteric fracture osteosynthesis with proximal femoral locking compression plate. Injury 2013;44:751-6. [Google Scholar] |
| 18. | Xie H, Xie L, Wang J, Chen C, Zhang C, Zheng W. Intramedullary versus extramedullary fixation for the treatment of subtrochanteric fracture: A systematic review and meta-analysis. Int J Surg 2019;63:43-57. [Google Scholar] |
| 19. | Perez EA, Jahangir AA, Mashru RP, Russell TA. Is there a gluteus medius tendon injury during reaming through a modified medial trochanteric portal? A cadaver study. J Orthop Trauma 2007;21:617-20. [Google Scholar] |
| 20. | White TO, Mackenzie SP, Gray AJ, editors. Hip fractures. In: McRae's Orthopedic Trauma and Emergency Fracture Management. 3rd ed. Edinburg: Elsevier; 2016. p. 367. [Google Scholar] |
| 21. | Flierl MA, Stahel PF, Hak DJ, Morgan SJ, Smith WR. Traction table-related complications in orthopaedic surgery. J Am Acad Orthop Surg 2010;18:668-75. [Google Scholar] |
| 22. | Callanan I, Choudhry V, Smith H. Perineal sloughing as a result of pressure necrosis from the traction post during prolonged bilateral femoral nailing. Injury 1994;25:472. [Google Scholar] |
| 23. | Lyon T, Koval KJ, Kummer F, Zuckerman JD. Pudendal nerve palsy induced by fracture table. Orthop Rev 1993;22:521-5. [Google Scholar] |
| 24. | Bible JE, Mir HR. Well-leg positioning on a fracture table: Using a pillow sling. Am J Orthop (Belle Mead NJ) 2014;43:571-3. [Google Scholar] |
| 25. | Freigang V, Gschrei F, Bhayana H, Schmitz P, Weber J, Kerschbaum M, et al. Risk factor analysis for delayed union after subtrochanteric femur fracture: Quality of reduction and valgization are the key to success. BMC Musculoskelet Disord 2019;20:391. [Google Scholar] |
| 26. | Kokkalis ZT, Mavrogenis AF, Ntourantonis DI, Igoumenou VG, Antoniadou T, Karamanis R, et al. Reduction techniques for difficult subtrochanteric fractures. Eur J Orthop Surg Traumatol 2019;29:197-204. [Google Scholar] |
| 27. | Yoon RS, Donegan DJ, Liporace FA. Reducing subtrochanteric femur fractures: Tips and tricks, do's and don'ts. J Orthop Trauma 2015;29 Suppl 4:S28-33. [Google Scholar] |
| 28. | Barbosa de Toledo Lourenço PR, Pires RE. Subtrochanteric fractures of the femur: Update. Rev Bras Ortop 2016;51:246-53. [Google Scholar] |
| 29. | Kasha S, Yalamanchili RK. Management of subtrochanteric fractures by nail osteosynthesis: A review of tips and tricks. Int Orthop 2019; [Epub ahead of print]. [Google Scholar] |
| 30. | Falkensammer ML, Benninger E, Meier C. Reduction techniques for trochantericand subtrochanteric fractures of the femur: A practical guide. Acta Chir Orthop Traumatol Cech 2016;83:300-10. [Google Scholar] |
| 31. | Kumar A, Chouhan D, Narang A, Khan R, Mittal S. “Clamp and plate”-A simple technique for prevention of varus malreduction in reverse oblique peritrochanteric fractures. J Clin Orthop Trauma. 2020. [In press]. [Google Scholar] |
| 32. | Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, et al. Atypical subtrochanteric and diaphyseal femoral fractures: Second report of a task force of the American Society for Bone and Mineral Research: AFF Task Force Report. J Bone Miner Res 2014;29:1-23. [Google Scholar] |
| 33. | Shane E, Burr D, Ebeling PR, Abrahamsen B, Adler RA, Brown TD, et al. Atypical subtrochanteric and diaphyseal femoral fractures: Report of a task force of the American Society for Bone and Mineral Research: Atypical Femoral Fractures Task Force Report. J Bone Miner Res 2010;25:2267-94. [Google Scholar] |
| 34. | Prasarn ML, Ahn J, Helfet DL, Lane JM, Lorich DG. Bisphosphonate-associated femur fractures have high complication rates with operative fixation. Clin Orthop Relat Res 2012;470:2295-301. [Google Scholar] |
| 35. | Tosounidis TH, Lampropoulou-Adamidou K, Kanakaris NK. Intramedullary nailing of sequential bilateral atypical subtrochanteric fractures and the management of distal femoral intraoperative fracture. J Orthop Trauma 2015; [Epub ahead of print]. [Google Scholar] |
| 36. | Schilcher J, Sandberg O, Isaksson H, Aspenberg P. Histology of 8 atypical femoral fractures: Remodeling but no healing. Acta Orthop 2014;85:280-6. [Google Scholar] |
| 37. | Choy WS, Kim KJ, Lee SK, Yang DS, Jeung SW, Choi HG, et al. Surgical treatment of pathological fractures occurring at the proximal femur. Yonsei Med J 2015;56:460-5. [Google Scholar] |
| 38. | Willeumier JJ, van der Linden YM, van de Sande MA, Dijkstra PD. Treatment of pathological fractures of the long bones. EFORT Open Rev 2016;1:136-45. [Google Scholar] |
| 39. | Zafiropoulos G, Pratt DJ. Fractured Gamma nail. Injury 1994;25:331-6. [Google Scholar] |
| 40. | Zacherl M, Gruber G, Glehr M, Ofner-Kopeinig P, Radl R, Greitbauer M, et al. Surgery for pathological proximal femoral fractures, excluding femoral head and neck fractures: Resection vs. stabilisation. Int Orthop 2011;35:1537-43. [Google Scholar] |
| 41. | Boopalan PR, Jepegnanam TS, Nithyananth M, Venkatesh K, Cherian VM. Functional outcome of biological condylar blade plating of subtrochanteric fractures. J Orthop Sci 2012;17:567-73. [Google Scholar] |
| 42. | Gupta RK, Gupta V, Gupta N. Outcomes of osteoporotic trochanteric fractures treated with cement-augmented dynamic hip screw. Indian J Orthop 2012;46:640-5. [Google Scholar] |
| 43. | Klestil T, Röder C, Stotter C, Winkler B, Nehrer S, Lutz M, et al. Impact of timing of surgery in elderly hip fracture patients: A systematic review and meta-analysis. Sci Rep 2018;8:13933. [Google Scholar] |
Fulltext Views
12,561
PDF downloads
2,438





