Translate this page into:
Massive bone defect in open leg fracture: A case report
*Corresponding author: Assala Abu Mukh, Department of Orthopedics and Traumatology, Vita-Salute San Raffaele University - San Raffaele Hospital, Milan, Italy. assala.abumukh@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Placella G, Abu Mukh A, Ometti M, Salini V. Massive bone defect in open leg fracture: A case report. J Musculoskelet Surg Res. 2024;8:406-11. doi: 10.25259/JMSR_24_2024
Abstract
Open fractures with massive defects are likely the most challenging conditions to manage in traumatology, particularly due to the scarcity of cases described in the literature where limb preservation was feasible. This report illustrates the management of an open fracture with a massive bone defect in which the physicians recurred to amputation after an attempt to preserve the patient’s quality of life through initial reparative treatment. A 57-year-old male presented with an open fracture with a de novo 25-cm bone defect following a motorcycle accident. Despite the large laceration, the injury presented with a relatively conserved surrounding muscular tissue; the distal two-thirds of the tibia were missing; yet, no neurovascular damage was documented. The patient was managed with a temporary external fixator and antibiotic-loaded cement spacer. Due to the patient’s desire to ride his motorcycle again, the authors performed a custom-made tibiotalar nailing arthrodesis 22 weeks later. This case presented the risk of infection and low quality of life, which led to amputation 74 weeks after the nailing procedure was performed. The treatment remains challenging in cases of massive bone defects and a relatively preserved biological-functional environment, and efforts should be made to develop tailored strategies. Although individualized care provides patients with time and hope, it might still fail to guarantee a decent quality of life and risks being a temporary solution before reverting to amputation.
Keywords
Amputation
Bone defect
Fibula
Fracture
Lower extremity
Tibia
INTRODUCTION
Open fractures are among the most challenging conditions to manage in traumatology, especially when correlated with large bone defects. Although uncommon, studies report a variable frequency, from 2.6% to 23.5%.[1,2] Nevertheless, open fractures present significant sequelae for the patients and their quality of life.
Larger wounds are less common and have been reported by Mwafulirwa et al. around 21.7% of all open fractures.[3] In this report, we present a rare case handled in an emergency setting in which a massive bone defect was encountered and initially treated with a limb salvage strategy to preserve the patient’s quality of life. However, this attempt fails, and amputation becomes mandatory.
CASE REPORT
An otherwise healthy 57-year-old male, victim of a motorcycle accident (178 cm, 74 kg, body mass index 23.36 kg/m2), was rushed into our emergency department. An initial evaluation revealed an open left leg fracture and no further comorbidities [Figure 1]. The patient presented with a 35-cm-long laceration over the left anteromedial leg and several abrasions over the left knee, right distal leg, and upper right thigh. No pre-existent pathological bone condition was known in this patient.

- Left anteromedial distal leg exposition estimated around 35 cm.
A computed tomography scan with three-dimensional reconstruction showed a 42C comminuted tibial shaft fracture (AO classification)[4] with D3C massive bone defect and a fibular 4F2B midshaft fracture based on Tetsworth classification of bone defects.[5] The vascular surgeon performed an emergency lower-limb Doppler ultrasound, and no vascular damage was encountered. Following the initial assessment, the fracture was classified as Gustilo-Andersen IIIA[6] and scored 7 on the Mangled Extremity Severity Score (MESS). However, the surgeons attempted limb salvage surgery due to the relatively preserved soft tissue and young age.
The patient was led to the operation theater, and the surgeons prepped the operative field for damage control surgery following intravenous Cefazolin administration. After a thorough inspection, the bone defect was confirmed. The two proximal anterior bone fragments were still attached to the remnant origin of the tibialis anterior muscle [Figure 2]. There was massive bone loss of the tibial diaphysis and distal metaphysis that included the whole distal articular surface. Remnants of the deltoid ligament were identified, and the great saphenous vein was spared. Besides partial tibialis anterior muscle origin (with its bony component) and a small part of the medial gastrocnemius belly, all other muscles and tendons were intact [Figure 3].
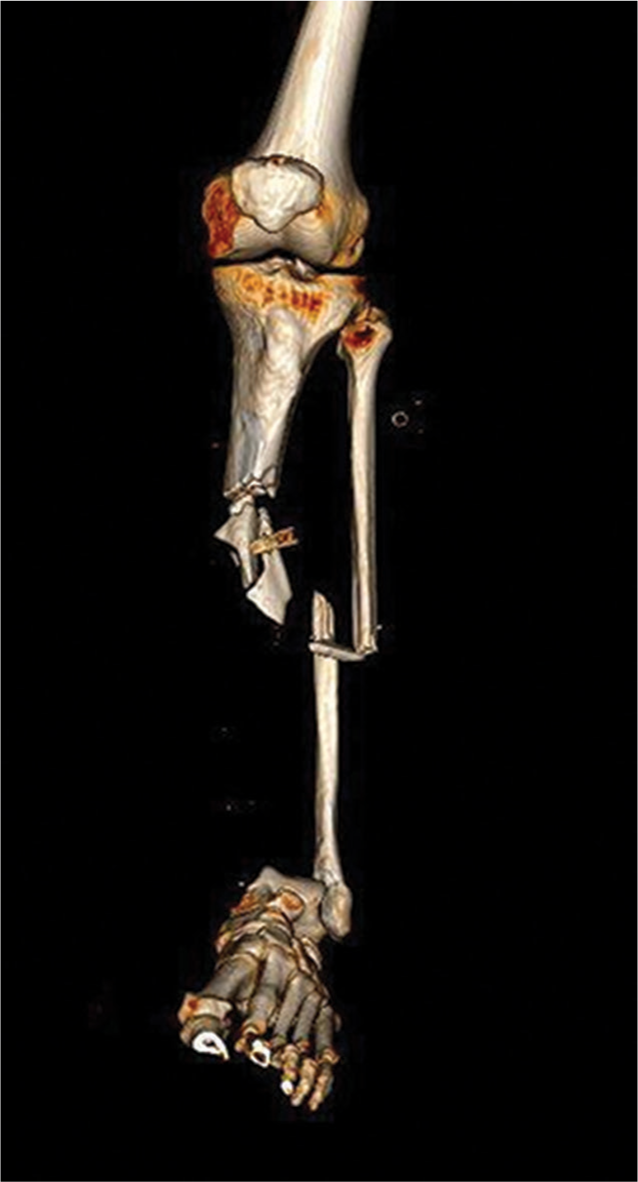
- A three-dimensional reconstruction of left lower limb – Computerized tomography.
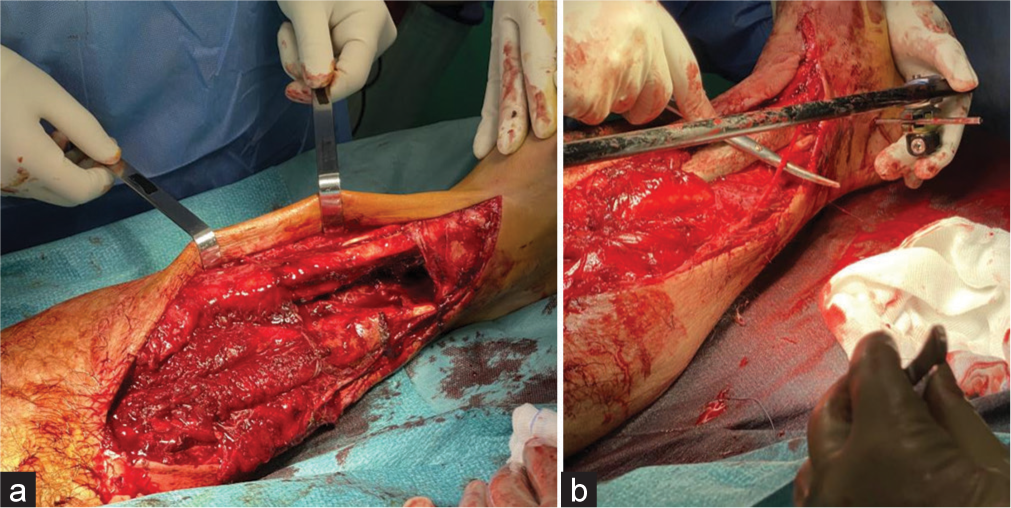
- (a) Pictures exhibiting the open injury site and (b) the right great saphenous vein is indicated and intact.
Surgeons performed abundant lavage, disinfection, and antibiotic-loaded cemented spacer (ALBC) assemblage in preparation for definitive surgery, in accordance with the Masquelet technique.[7,8] Following tissue debridement, an external fixator was assembled. We inserted two pins at the proximal end of the tibia and one trans-calcaneus threaded pin. The pins were connected with translucent carbon bars. We chose external fixation to maintain the lower limb length and alignment; the fibula served as a reference [Figure 4]. To prevent tissue shrinkage and possible infection, a 24.5-cm-shaped ALBC was inserted. The loaded antibiotics consisted of vancomycin, gentamicin, and clindamycin [Figure 5]. The proximal end of the tibialis anterior muscle was sutured to the gastrocnemius in coverage of the ALBC, creating a favorable biological environment for future reconstructions. The wound was surgically closed [Figure 5], and postoperative radiographs of the ALBC spacer position and limb alignment were obtained [Figure 6].
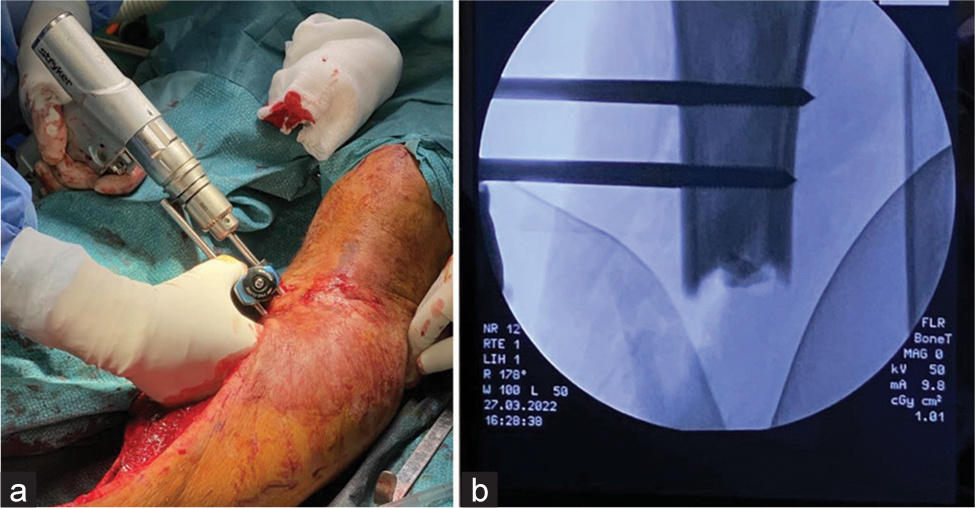
- (a) External fixator assembly and (b) intraoperative imaging.

- Final post-operative result illustrating wound closure and external fixator.

- Anteroposterior and lateral post-operative radiographs.
Post-operative Doppler-ultrasound documented appropriate patent femoral, popliteal, tibial, peroneal, and dorsalis pedis arteries, and antibiotic prophylaxis was given with amoxicillin and clavulanic acid. The surgeons kept the patient non-weight-bearing following surgery. Wound dressings, clinical evaluations, and radiographs assessing construct stability were performed regularly.
Tibiotalar arthrodesis using a custom-made nail was performed 22 weeks following the incident [Figure 7]. The custom-made device dictated this timeframe as it required modification and remanufacturing. Even though gait was possible, the Short-Form Health Survey 36 assessed the quality of life at four and eight months following definitive treatment. He scored 45 and 50.8, respectively, indicating a significantly impaired quality of life.[9] The radiographic and clinical patient outcomes at eight months of follow-up after definitive surgery are shown in Figure 8 and Video 1.
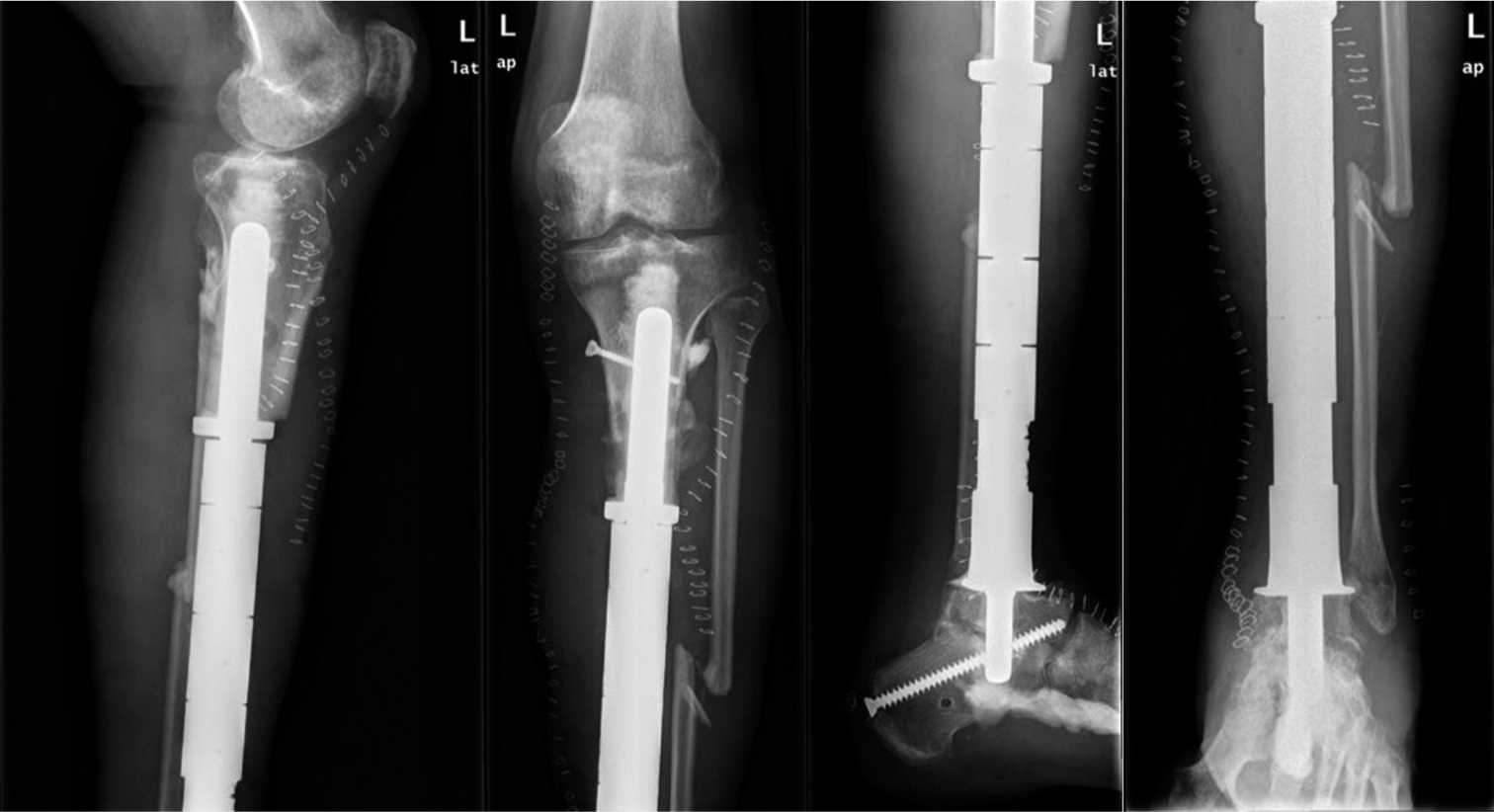
- Radiographs illustrating post-operative results following custom-made nail implant for arthrodesis of the tibiotalar joint. Anteroposterior and lateral radiographs of the proximal and distal leg are illustrated.

- Post-operative weight-bearing scanogram of the lower limbs.
Despite the low chances[10] of limb salvage on MESS assessment, the patient desired to preserve his leg and ride his motorcycle again, which required an individualized approach. A custom-made nail arthrodesis of the tibiotalar joint was designed for the patient. This treatment was esthetically appealing while permitting basic daily activities.
Following surgery, the patient presented with a series of recurrent high-fever episodes with swelling and pain. These episodes were sometimes associated with a turbid secretion from the plantar foot. Samples for Gram stain, culture for typical and atypical germs, and fungal species were analyzed in four different episodes, and all results were negative. Despite the patient’s inability to walk before this treatment, he repeatedly refused amputation even though unable to return to work, and his normal daily activities were severely compromised. After multiple consultations, the patient got convinced and consequently received amputation at a 74-week distance from the nailing procedure.
DISCUSSION
This patient’s unique distal tibia bone loss and disruption of the ankle mortise presented in the absence of neurovascular injury and relative preservation of the surrounding soft tissue. Although the literature’s recurrent attempts to find new preservation methods in critical cases were unsuccessful,[10] the patient insisted on limb preservation by any means necessary.
Thus, our treatment options besides amputation were the following: External fixation followed by tibia allograft transplantation. According to Baseri et al., this presents a high risk of infection (19.9%),[11] and if not controlled, it might lead to amputation.[12] Another option was to perform nailing following cadaveric transplantation. This presents the same risks as the procedure mentioned before and may not be feasible in the case of articular involvement. Even though this treatment offers relative stability, it is not absolute and requires graft integration, which would have slowed down the patient’s rehabilitation and weight-bearing.[13]
A study by Haines et al. defined the lower limits of critical bone defect; in their paper, the authors concluded that a defect larger than 25 mm has a higher probability of non-union even when nailing is performed.[14] Moreover, potential ankle instability in our patient was highly probable without possible ligamentous structure reconstruction surrounding an eventual distal tibia graft.
A third option is distraction osteogenesis by performing a metaphyseal osteotomy. The patient would require an Ilizarov-type ring fixator for an extended period.[15] Considering the massive bone defect in question, it limits his functional capacity for a protracted period. In addition, this will not solve the distal joint disorder unless ankle fusion or arthroplasty is performed. A study by Adamczyk et al. suggested that bone regeneration time is reduced when both ends of a bone are diseased.[16] This method might be considered if the distal tibia was intact. However, if grafting was performed, we believe prolonged rehabilitation times combined with a relatively low success rate of ankle arthroplasty would have created more problems.[17]
Ilizarov method and the Masquelet technique were determined to be comparable in femoral bone defects. However, the Masquelet technique seems to be preferred for periarticular defects.[18]
Tibiotalar arthrodesis using a custom-made nail was performed 22 weeks following the incident, which was followed by a series of recurrent high-fever episodes with swelling and pain on the plantar foot. Samples for gram stain, culture for typical and atypical germs, and fungal species were all negative. After multiple consultations, the patient received amputation 24 months after the initial presentation (approximately 1½ years after nail insertion).
CONCLUSION
The bone is hardly substitutable despite surrounding tissue preservation, particularly in massive or articular bone defects. Nevertheless, treatments must be driven by each case evaluation, as every patient is different. Even though a case of large bone defect rarely presents in a relatively conserved biological context, its treatment remains challenging. Although individualized care provides patients with time and hope, it might still fail to guarantee a decent quality of life and risks being a temporary solution before recurring to amputation.
AUTHORS’ CONTRIBUTIONS
GP conceived, operated on, and followed up on the patient, documenting his history. AAM documented and collected data and wrote and revised the article. MO participated in documenting the patients’ history. VS coordinated and organized the patient’s treatment. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The Institutional Review Board approval was waived.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published, and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
Video 1 is available on:
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- The epidemiology of fractures United States: Lippincott Williams and Wilkins; 2010. p. :53-84.
- [Google Scholar]
- Epidemiology and management of open fractures of the lower limb. Br J Hosp Med. 1997;57:582-7.
- [Google Scholar]
- Epidemiology of Open Tibia fractures presenting to a tertiary referral centre in Southern Malawi: A retrospective study. Malawi Med J. 2022;34:118-22.
- [CrossRef] [PubMed] [Google Scholar]
- Classification AO des fractures In: Tome I. Les os longs. Berlin: Springer-Verlag; 1987.
- [CrossRef] [Google Scholar]
- Classification of bone defects: An extension of the orthopaedic trauma association open fracture classification. J Orthop Trauma. 2021;35:71-6.
- [CrossRef] [PubMed] [Google Scholar]
- In brief: Gustilo-Anderson classification. Clin Orthop Relat Res. 2012;470:3270-4. Erratum in: Clin Orthop Relat Res 2012;470:3624, Erratum in: Clin Orthop Relat Res 2019;477:2388
- [CrossRef] [PubMed] [Google Scholar]
- Reconstruction of the long bones by the induced membrane and spongy autograft. Ann Chir Plast Esthet. 2000;45:346-53.
- [Google Scholar]
- The concept of induced membrane for reconstruction of long bone defects. Orthop Clin North Am. 2010;41:27-37.
- [CrossRef] [PubMed] [Google Scholar]
- The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473-83.
- [CrossRef] [PubMed] [Google Scholar]
- Lower extremity assessment project (LEAP)--the best available evidence on limb-threatening lower extremity trauma. Orthop Clin N Am. 2010;41:233-9.
- [CrossRef] [PubMed] [Google Scholar]
- Bacterial contamination of bone allografts in the tissue banks: A systematic review and meta-analysis. J Hosp Infect. 2022;123:156-73.
- [CrossRef] [PubMed] [Google Scholar]
- Management of critical-sized bone defects in the treatment of fracture-related infection: A systematic review and pooled analysis. Arch Orthop Trauma Surg. 2021;141:1215-30.
- [CrossRef] [PubMed] [Google Scholar]
- Faster integration of human allograft bone than of the bovine substitute Lubboc Non-randomized evaluation of 20 cases with benign tumors or tumor-like conditions. Acta Orthop. 2004;75:217-20.
- [CrossRef] [PubMed] [Google Scholar]
- Defining the lower limit of a “critical bone defect” in open diaphyseal tibial fractures. J Orthop Trauma. 2016;30:e158-63.
- [CrossRef] [PubMed] [Google Scholar]
- Stiffness characteristics of the circular Ilizarov device as opposed to conventional external fixators. J Biomech Eng. 1990;112:15-21.
- [CrossRef] [PubMed] [Google Scholar]
- Masquelet technique versus Ilizarov bone transport for reconstruction of lower extremity bone defects following posttraumatic osteomyelitis. Injury. 2017;48:1616-22.
- [CrossRef] [PubMed] [Google Scholar]







