Translate this page into:
Migrated posterior sternoclavicular joint dislocation into the mediastinum along with clavicle diaphyseal fracture in a child
2 Division of Orthopedic, Department of Surgery, College of Medicine, Taif University, Taif, Saudi Arabia
Corresponding Author:
Amaal M Aldosari
Department of Surgery, Al Noor Specialist Hospital, Makkah
Saudi Arabia
dr_amaal@hotmail.com
| How to cite this article: Aldosari AM, Bajuifer SJ, Bukhary HA. Migrated posterior sternoclavicular joint dislocation into the mediastinum along with clavicle diaphyseal fracture in a child. J Musculoskelet Surg Res 2021;5:128-131 |
Abstract
The sternoclavicular joint (SCJ) is one of the least frequently dislocated joints, especially in a posterior direction. Posterior SCJ dislocation is a rare injury in orthopedic surgery compared to anterior dislocation, especially in children. The properties of anatomical structures and biomechanics around the SCJ are the primary cause of this rarity. Posterior dislocation may lead to fatal mediastinum injuries. Strict physical examination and diagnostic images should be carefully evaluated if there is any doubt of this injury to avoid delayed or misdiagnosis and complications. The authors report this rare instance of traumatic posterior SCJ dislocation with a middle clavicle fracture, which was associated with the migration of the proximal end into the aortopulmonary window in a 9-year-old child. It was early diagnosed in the Emergency Department by a computed tomography scan. The patient was managed by open reduction with suture fixation, and the stability was assessed intraoperatively. The thoracic surgery team assistance was valuable. The purpose of reporting this unique case is to discuss the rarity of the radiological findings in a child with SCJ dislocation, that is regularly a physeal fracture-dislocation, according to the literature. Furthermore, to discuss our approach to avoid misdiagnosis and complications.
Introduction
The last growth plate that ossifies in the human body is at the clavicle's proximal part, between 18 and 25 years.[1],[2],[3],[4],[5],[6],[7] Accordingly, sternoclavicular joint (SCJ) dislocation could be confused with a fracture of the proximal clavicular growth plate that needs to be excluded.[3],[6] Posterior SCJ dislocations are less frequent injury than anterior dislocations.[1],[2],[3],[6],[7],[8],[9] They can manifest with medial clavicular pain that increases with the arm movement, but it can also present with other manifestations. These manifestations can be due to compression of the trachea, esophagus, vital vascular and neurological structures, which will need an intervention urgently.[1],[2],[3],[4],[5],[6],[7],[8],[10],[11],[12] It frequently occurs as contact sports injury through an indirect force to the shoulder's posterolateral part.[2] Posterior dislocation can happen less frequently when posterior energy is transmitted directly to the medial clavicle's exterior surface that is estimated for barely 10%–25% of SCJ injuries, which can happen during sport situations or motor vehicle accidents.[2],[3],[9],[12] Clavicle bone fractures in children account for about 5%–15% of all pediatric fractures.[13] At the same time, posterior SCJ dislocation is rare with, an incidence of only 3% of all shoulder girdle injuries.[1],[2],[3],[4],[8],[10] Posterior SCJ dislocation is a much severe injury than anterior that may jeopardize mediastinal structures and the thoracic outlet.[1],[2],[5],[6],[7],[10] Closed reduction usually works in managing most of the acute stable posterior dislocations. In contrast, operative open reduction should be considered if the closed reduction was ineffective or there was persistent SC instability.[1],[2],[3],[4],[5],[6],[7],[8],[9],[10],[11],[14] This case report illustrates an unusual variety of clavicular injury, in which a middle third clavicular fracture has occurred, along with posterior SCJ dislocation in a child. Even though in this age group, medial physeal fracture-dislocation is more prevalent.[3],[4],[7],[14] Our aim of publishing this unprecedented case is to explain the radiological findings of a child who had posterior SCJ dislocation with a diaphyseal fracture. In addition, bringing attention to the importance of computed tomography (CT) scan in confirming and evaluating the diagnosis. Moreover, to share our experience in the management of this injury.
Case Report
A 9-year-old boy presented to the emergency room as a pedestrian hit by a car. He complained of pain and limited range of motion of his nondominant left side upper extremity. His past medical history was unremarkable. Examination showed stable vitals and oxygen saturation of 99% on room air. The skin was healthy, with no swelling or ecchymosis of the neck, chest, and extremities. The examination of the airway, respiratory, and cardiovascular systems was unremarkable. Local examination showed a less prominent left clavicle compared to the right side. The left clavicular head could not be palpated because of tenderness at the left SCJ. There was no subcutaneous emphysema. His range of motion and strength were limited by pain. Neurologic and vascular examination of the left upper extremity was within the normal limits.
Plain anterior-posterior chest radiograph showed a suspicion of asymmetry across the SCJ and probable fracture of the middle third of the left clavicle [Figure - 1]. However, it did not allow for a precise evaluation of the nature of the injury. Pan CT was requested as a part of the implementation of our local trauma protocol. It verified the left clavicular fracture involving the middle of the clavicle [Figure - 2]a and [Figure - 2]b. The proximal end of the clavicle migrated to the mediastinum at the aortopulmonary window. It was compressing the pulmonary trunk. A suspicion of a retrosternal hematoma was striking [Figure - 3]a,[Figure - 3]b,[Figure - 3]c,[Figure - 3]d. In addition, there was a fracture of the right scapula with pneumomediastinum plus bilateral pneumothorax. The trachea and esophagus were within normal limits, and there was no pleural or pericardial effusion. The patient was admitted and prepared for open reduction.
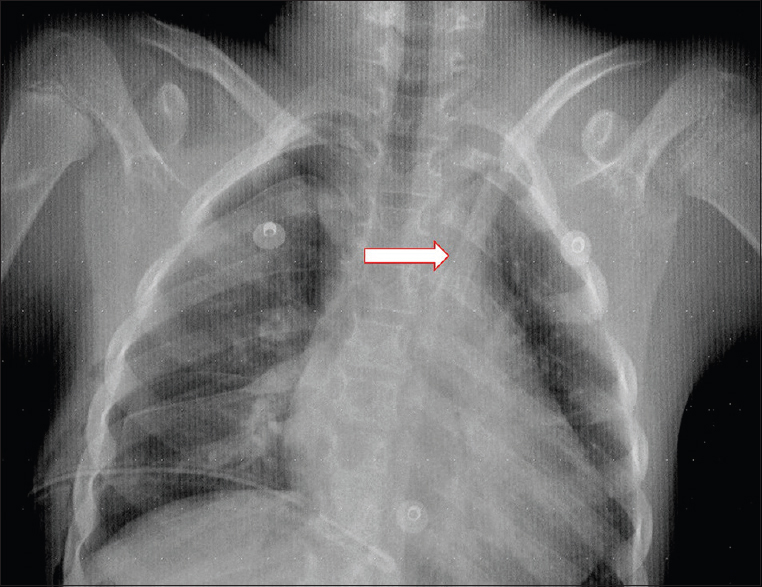 |
| Figure 1: An anteroposterior thoracic radiographs. Note the displaced medial end of clavicle (arrows) on the left side |
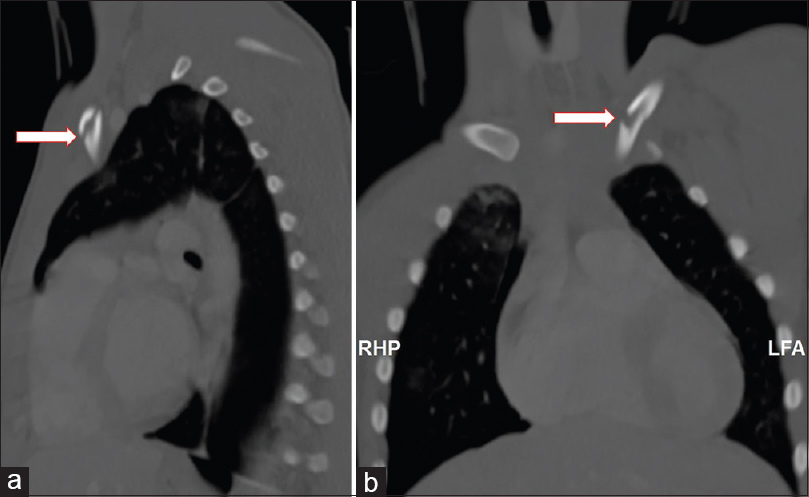 |
| Figure 2: Computed tomography scan of the chest showing: sagittal (a) and coronal (b) views with left clavicle diaphyseal fracture (arrows) |
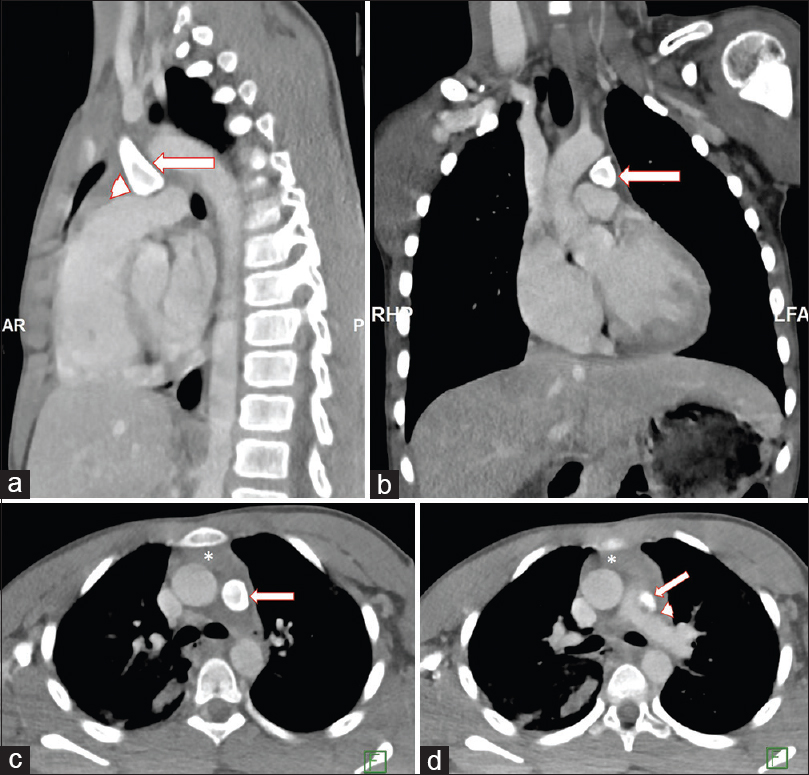 |
| Figure 3: Computed tomography scan of the chest showing: sagittal (a), coronal (b), and axial (c and d) views with complete posterior dislocation of left sternoclavicular joint (arrow) with evidence of medial clavicle compressing the pulmonary trunk (arrowhead) and the presence of retrosternal hematoma (white asterisk) |
Surgical procedure
On the next day, the patient was shifted to the operating room. He was placed in a supine position under general anesthesia with a sandbag placed between the scapulae. An eight cm incision was done, starting from the manubrium to the middle of the clavicle. The thoracic surgeon started the open exploration, directing the dissection to the left clavicle. A careful dissection over the medial third of the clavicle was performed. It showed that the anterior part of the SCJ ligament was avulsed from its origin with the clavicular periosteum. The articular disc was identified, and it was minimally torn. The posterior SCJ ligament was also torn. A nondisplaced incomplete fracture of the middle third of the clavicle was recognized. The proximal part of the clavicle was completely dislocated into the mediastinum. Gentle closed reduction was not possible, so the thoracic surgeon freed the dislocated clavicle. The reduction of SCJ was made by the orthopedic surgeon after repairing the articular disc tear.
The stability of the joint was assessed, and it was not stable. The fracture of the middle third of the clavicle shaft was checked, and it was stable after the reduction, so it was left without fixation. Eventually, the posterior SCJ ligament was fixed using a polydioxanone suture. Then, an augmentation of the anterior SCJ ligament was done using a transosseous suture technique. Finally, the remnants of the capsule were sutured to increment the repair. The shoulder was examined, and joint stability was noted. Hemostasis was affirmed, closure of the wound and subsequent tissues was done in layers. The arm was immobilized with a sling for 6 weeks. He was kept under observation for 24 h following the procedure. Then he was discharged home on the third postoperative day. [Figure - 4] shows the early postoperative radiographs.
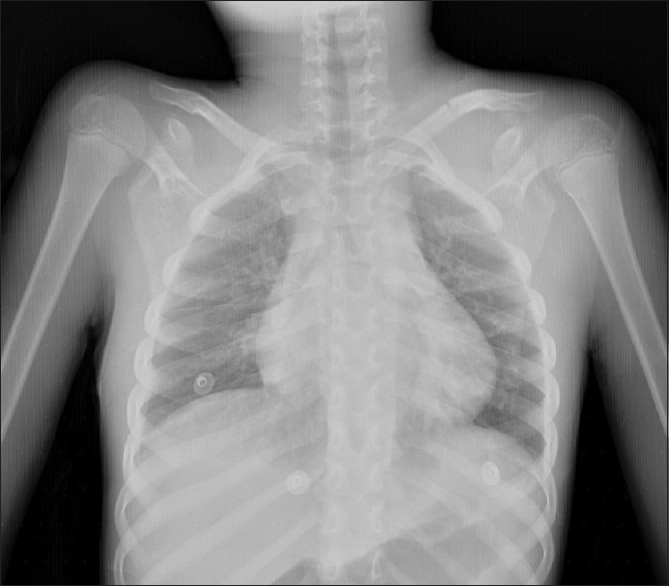 |
| Figure 4: Postoperative radiograph |
He was instructed to start physiotherapy sessions on the 6th week as a passive shoulder range of motion to reach an abduction of 60° and forward flexion of 90°. On the 6-week and 3-month postoperative follow-up visits, he displayed clinical healing of the surgical wound and an acceptable range of motion.
Discussion
In this reported case, the mechanism of injury was due to direct injury to the shoulder. The capsular ligaments of the posterior SCJ are significantly more durable than the anterior portion. Thus, more considerable energy is needed (more than twice the force needed for the anterior dislocation) to dislocate the joint posteriorly.[2],[9]
The patient with posterior SCJ dislocation will frequently complain of pain and swelling that sometimes can be intense and disproportionate to clinical findings. Their signs may be subtle, so a careful and distinctive doubt is required for diagnosing posterior SCJ dislocation. Therefore, in the setting of significant trauma, it can be commonly missed.[3],[10],[12] Besides these symptoms, others can also be associated with posterior SCJ displacement like shortness of breath if the trachea was compressed or if the patient developed pneumothorax. Furthermore, choking, difficult or painful swallowing if the esophagus got compressed. Voice changes if the nerves were pressed.[1],[2],[3],[5],[6],[7],[8],[10],[11],[12] Life-threatening accidents may be connected to posterior displacement of the SCJ due to the closeness of critical upper mediastinal organs. Posterior SCJ disruptions have joined intrathoracic or superior mediastinal insults in up to 30% of incidents. Posterior displacement must be rolled out due to the high mortality linked to this type of injury, which accounts for 12.5% of all SCJ dislocations. This scary associated incident involves compression or tear of large vessels, lungs pleura, trachea, esophagus, and injury to the brachial plexus.[1],[3],[6],[7],[9],[10],[11],[12] Accurate history, clinical examination, and plain radiographs do not dispense the need for urgent CT scan or angiographic CT scan whenever there is a suspicion of dislocation.[5],[12],[14]
Physicians must know the inadequacy of conventional radiographs in identifying and diagnosing posterior SCJ dislocation. They may need to supplement their data with CT imaging to evaluate soft tissues and eliminate the possibility of mediastinal structures injury.[5],[12] For instance, posterior dislocation of the SCJ can be questionable in an anteroposterior radiograph. It can happen if a discrepancy with >50% of the clavicle head width in a craniocaudal relative position.[5] Although, with some radiographic view adjustment, a particular correlation view that is fit for solitary SCJ injuries may help in the diagnosis. This view is called the serendipity view, which would permit a comparison between the normal clavicle to the injured one. It is done by centering the beam on the SCJ with 40° angled cephalically.[1],[3],[6],[7] Many authors favor CT scan to be done with intravenous contrast as required if a vascular injury is clinically suspected as the most trusted mode of investigations.[3],[5],[6],[8],[12] Moreover, CT scans are essential in identifying skeletal fractures or mediastinal soft-tissue damages.[3],[4],[5],[6],[7],[10],[12],[14] It must involve the proximal part of both clavicles in each side of the chest to correlate between the affected and unaffected segments.[1] Besides, it has been valued for its convenience as the most beneficial emergency case tool compared to Magnetic Resonance Imaging.[1]
Regardless of dislocation direction, all acute and displaced traumatic SCJ had less clinical outcome results if left untreated.[11] Since dislocations of SCJ in the posterior direction are not like other directions due to the need for extra critical recognition and attention.[1],[3],[7],[14] Furthermore, they demand accurate judgment and treatment. Besides, numerous pediatric dislocation injuries do not get discovered; complications could vary from mild chronic pain to death by critical bleeding.[1],[2],[3]
Nevertheless, 30%–68% stated a successive reduction when a posterior SCJ dislocation was closely reduced, much less successful close reductions were reported in medial physis fracture-dislocations.[3],[7] A non-operative close reduction can be accomplished under sedation or general anesthesia. According to most authors, a specialized trauma or a thoracic specialist is required to be accessible during repositioning of the SCJ because of the possibility of severe bleeding that could be fatal and may need different interventions.[1],[3],[6],[7],[11],[12] More than one way of close reduction of SCJ has been offered. The abduction traction maneuver is a well-established and efficient reduction method commonly used by using a sterilized towel clip to pull the proximal clavicular end along with shoulder traction in 90° of abduction. An inverse maneuver without a towel clamp is possible. This maneuver is by adduction traction to the arm accompanying shoulder retraction power supported via a bolster between both scapulae.[1],[2],[3],[6],[7],[14],[12]
In the presented clinical case, the degree of clavicle migration of the proximal side was significant. Alongside it reached the aortopulmonary window and was compressing the pulmonary trunk. The presence of a clavicular fracture on the middle third of the shaft did support the made decision. An open reduction and stabilization are currently recommended. That is because of the high number of recorded late complications and repeated instability.[1],[3],[4],[14] If a patient does require an open reduction, procedures differ with no report supporting one over the others. That is because of the low number of cases and short-term follow-up time.[4],[6],[7] The best outcomes were found in suture fixation, tenodesis, and open reduction internal fixation with less joined significant complications. At the same time, proximal clavicle resection plus tendon graft were marked the modest proportions practice, yet with significantly better outcomes.[1],[4],[7] Kirschner wire fixations were associated with deadly migration results that had reached within the spinal cord and the heart with its main great vessels.[1],[2],[3],[4],[6],[7],[9]
Conclusion
This case report illustrates posterior SCJ dislocation associated with migration of proximal end into the aortopulmonary window, which is a rare and severe injury. Strict physical examination and diagnostic images, especially CT scans, should be carefully evaluated if there is any doubt of SCJ injury to avoid misdiagnosis and complications. Orthopedic surgeons must be knowledgeable about the management.
Recommendation
The authors recommend open anatomical reduction and internal fixation by bone suture material associated with the periosteum and ligament repairs.
Ethical consideration
Ethical approval was obtained from The Research Ethics Committee in Makkah Region Health-Ministry of Health (02/09/2020, IRB: H-02-K-076-0820-329).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the child's parents have given their consent for images and other clinical information to be published. The child's parents understand that his name and initials will not be published, and due efforts will be made to conceal patient identity, but anonymity cannot be guaranteed.
Acknowledgment
The authors would like to thank the child's parents for approving reporting the case. Further, authors appreciate the support from The Research Ethics Committee of Planning and Research Department in Makkah - Ministry of Health, Saudi Arabia that approved the protocol for the study (IRB number: H-02-K-076-0820-329).
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
AMA has contributed with concepts, definition of intellectual content, literature search, data acquisition and manuscript preparation. HAB has contributed with concepts, design, definition of intellectual content, literature search, manuscript preparation, editing, and review final draft. SJB have data acquisition and manuscript preparation. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Groh GI, Wirth MA. Management of traumatic sternoclavicular joint injuries. J Am Acad Orthop Surg 2011;19:1-7. [Google Scholar] |
| 2. | Tepolt F, Carry PM, Heyn PC, Miller NH. Posterior sternoclavicular joint injuries in the adolescent population: A meta-analysis. Am J Sports Med 2014;42:2517-24. [Google Scholar] |
| 3. | Chaudhry S. Pediatric posterior sternoclavicular joint injuries. J Am Acad Orthop Surg 2015;23:468-75. [Google Scholar] |
| 4. | Glass ER, Thompson JD, Cole PA, Gause TM 2nd, Altman GT. Treatment of sternoclavicular joint dislocations: A systematic review of 251 dislocations in 24 case series. J Trauma 2011;70:1294-8. [Google Scholar] |
| 5. | Khorashadi L, Burns EM, Heaston DR, Warme WJ, Richardson ML. Posterior dislocation of the sternoclavicular joint. Radiol Case Rep 2011;6:439. [Google Scholar] |
| 6. | Morell DJ, Thyagarajan DS. Sternoclavicular joint dislocation and its management: A review of the literature. World J Orthop 2016;7:244-50. [Google Scholar] |
| 7. | Jaggard MK, Gupte CM, Gulati V, Reilly P. A comprehensive review of trauma and disruption to the sternoclavicular joint with the proposal of a new classification system. J Trauma 2009;66:576-84. [Google Scholar] |
| 8. | Stewart DP, Van Klompenberg LH. Posterior dislocation of the clavicle at the sternoclavicular joint. Am J Emerg Med 2008;26:108.e3-4. [Google Scholar] |
| 9. | Thut D, Hergan D, Dukas A, Day M, Sherman OH. Sternoclavicular joint reconstruction – A systematic review. Bull NYU Hosp Jt Dis 2011;69:128-35. [Google Scholar] |
| 10. | Jougon JB, Lepront DJ, Dromer CE. Posterior dislocation of the sternoclavicular joint leading to mediastinal compression. Ann Thorac Surg 1996;61:711-3. [Google Scholar] |
| 11. | Sernandez H, Riehl J. Sternoclavicular joint dislocation: A systematic review and meta-analysis. J Orthop Trauma 2019;33:e251-5. [Google Scholar] |
| 12. | Buckley BJ, Hayden SR. Posterior sternoclavicular dislocation. J Emerg Med 2008;34:331-2. [Google Scholar] |
| 13. | Schulz J, Moor M, Roocroft J, Bastrom TP, Pennock AT. Functional and radiographic outcomes of nonoperative treatment of displaced adolescent clavicle fractures. J Bone Joint Surg Am 2013;95:1159-65. [Google Scholar] |
| 14. | Bicos J, Nicholson GP. Treatment and results of sternoclavicular joint injuries. Clin Sports Med 2003;22:359-70. [Google Scholar] |
Fulltext Views
4,539
PDF downloads
1,490





