Translate this page into:
Morphometry of the lower lumbar spinal canal among a sample of the Saudi population: Are we at risk?
*Corresponding author: Khalid Alghamdi, Department of Orthopedic Surgery, Security Forces Hospital, Riyadh, Saudi Arabia. khalid-ghamdi@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Alghamdi K, Omer I. Morphometry of the lower lumbar spinal canal among a sample of the Saudi population: Are we at risk? J Musculoskelet Surg Res, 2023;7:91-7.
Abstract
Objectives:
Lumbar disk bulge is a common cause of lower back pain. A high percentage of patients improve with conservative management, but unfortunately, some do not. We postulate that an anatomically narrowed lumbar spinal canal might contribute to this variation in response to conservative management. One of the major causes of spinal stenosis is idiopathic congenital-developmental stenosis, and here, we aimed to observe if this non-modifiable risk factor is present among the Saudi population, by analyzing the lower lumbar canal dimensions in computed tomography (CT) scan axial cuts, which might be later a reference and guide in clinical practice.
Methods:
This retrospective descriptive study included 279 patients aged 20–40years old. We included those who underwent diagnostic CT abdomen and CT lumbar spine with no evidence of lumbar spinal disease or fracture at the level where measures were taken from the axial cuts. Furthermore, exclusion criteria included gross spinal pathologies such as fractures, tumors, deformities, major chronic systemic diseases, congenital anomalies (dwarfism), and metallic artifacts.
Results:
Of the 279 patients, 137 (49%) were male and 142 (51%) were female. Different measurements were taken from the CT scan of axial cuts of the lower lumbar canal (L3, L4, and L5). The pattern of segmental variation of the lower lumbar vertebral canal was found to be like other populations. In contrast, the mean lower lumbar vertebral canal diameters were characteristically different from the other population (non-compensating).
Conclusion:
In the Saudi population, anterior-posterior and interpedicular diameters were narrowed (non-compensating). We found a high prevalence (32%) of trefoil configuration in the Saudi population.
Keywords
Trefoil spine
Prevalence
Saudi Arabia
Spinal stenosis
Risk factors
INTRODUCTION
It is usual to observe physique variations among the same population, and for sure, there will be major differences in different body parts comparing different populations. One of these body parts variations is the lower lumbar spinal canal.
A lumbar disk bulge is a common cause of lower back pain. A high percentage of patients improve with conservative management, but unfortunately, some do not. We postulate that an anatomically narrowed lumbar spinal canal might contribute to this variation in response to conservative management.[1]
Moreover, knowing that the lower lumbar spinal canal is narrowed in a specific population would help in awareness, screening programs, early prevention, diagnosis, and follow-up and a higher index of suspicion for the early conservative treatment failure. Moreover, early diagnosis and management’s importance include preventing intractable pain and permanent neurologic deficit. Many studies postulated that lumbar canal volume is important in symptomatic patients, and they proved that narrowed lumbar canal volume participates in lumbar radiculopathy.[1-3]
One of the major causes of spinal stenosis is idiopathic congenital-developmental stenosis as mentioned by Ciricillo and Weinstein,[4] and another study in Iraq by Kitab et al., showed the anatomic variations caused by this maldevelopment which include trefoil bony spinal canal.[5] The highest prevalence of this trefoil configuration is found in South Africa and Scotland.[6,7] Another study by Postacchini et al. did an anatomic study of the lumbar vertebrae in two groups of skeletons (Italian and Indian) and compared them to South African, which all of them have narrowed midsagittal diameters of the spinal canal and found that the Italians have more narrowed canal than the South Africans but wider than the Indians.[8] In addition, Azimi et al. examined the relationship between morphologic stenosis grades (Trefoil and Triangle) and the pre-operative walking ability in patients with lumbar canal stenosis. They found that walking ability is more profoundly affected in patients with trefoil-type stenosis.[9]
We aimed to observe if this non-modifiable risk factor is present among the Saudi population by analyzing the lower lumbar canal dimensions in computed tomography (CT) scan axial cuts, which might be later a reference and guide in clinical practice. Furthermore, knowing the prevalence of this risk factor and keeping it in mind is crucial as it predicts the early failure of conservative management. It affects intraoperative decisions, since trefoil configuration is narrowed laterally, more lateral decompression is vital to alleviate pressure on the neural elements; and since more lateral decompression is required, the spine’s stability might be compromised during far lateral decompression and fixation needed. Finally, the trefoil configuration is tricky. If not kept in mind, the surgeon could easily breach into the canal medially due to its shape, which might lead to neural elements compromise.
MATERIALS AND METHODS
This retrospective descriptive study was conducted at one of the prominent health-care institutes in Riyadh, Saudi Arabia. A total of 279 patients aged 20–40 years were included in this study who underwent diagnostic CT abdomen and CT lumbar spine with no evidence of lumbar spinal disease or fracture at the level where measures were taken. Of the 279 patients, 137 (49.1%) were male and 142 (50.9%) were female.
Exclusion criteria included gross spinal pathologies such as fractures, tumors, deformities, major chronic systemic diseases, congenital anomalies (dwarfism), and metallic artifacts.
Unenhanced CT was performed with sections of 2 mm thickness. Measurement was done in axial cuts as shown [Figure 1] to study both the lower lumbar spinal canal diameters and to study the configuration of the canal (different configurations demonstrated in [Figure 2], measurement of the trefoil configuration shown in [Figure 3], and different trefoil configurations shown in [Figure 4]). The trefoil configuration defined as a ratio of a transverse measurement (TM) taken at one-third of the distance from the midpoint of the interpedicular diameter (IPD) to the apex of the neural arch, and the full interpedicular diameter. Trefoil configuration defined when the ratio is less than 0.6667 [Figure 3].[6]

- Method of measurement of the lower lumbar spinal canal diameters.

- Different spinal canal configurations.

- Eisenstein S. The trefoil configuration of the lumbar vertebral canal. A study of South African skeletal material. The Journal of bone and joint surgery. 1980;62:73–7.

- Different trefoil configurations.
RESULTS
Anterior-posterior diameter (APD)
Two hundred and seventy-nine patients underwent CT scanning. The mean APD of the lower lumbar spinal canal (L3, L4, and L5) and its standard deviation (SD) in both male and female patients were measured [Table 1]. The total mean of the APD of both males and females is as the following, L3 15.2 mm (SD 1.5), L4 15.8 mm (SD 2.0), and L5 16.6 mm (SD 2.2).
| Mean APD of the lumbar spinal canal in males and females | ||||||
| Level | Males | Females | Total | |||
| Mean APD (mm) | SD | Mean APD (mm) | SD | Mean APD (mm) | SD | |
| L3 | 15.1 | 1.4 | 15.3 | 1.6 | 15.2 | 1.5 |
| L4 | 15.9 | 2.2 | 15.73 | 1.7 | 15.8 | 2.0 |
| L5 | 16.8 | 2.3 | 16.5 | 2.1 | 16.6 | 2.2 |
| Mean IPD of the lumbar spinal canal in males and females | ||||||
| Level | Males | Females | Total | |||
| Mean IPD (mm) | SD | Mean IPD (mm) | SD | Mean IPD (mm) | SD | |
| L3 | 24.2 | 1.8 | 23.1 | 1.6 | 23.6 | 1.6 |
| L4 | 25.0 | 2.3 | 23.8 | 1.6 | 24.4 | 1.9 |
| L5 | 29.0 | 3.3 | 27.1 | 2.7 | 28.0 | 3.0 |
APD: Anterior-posterior diameter, IPD: Inter-pedicular diameter, SD: Standard deviation
The mean IPD of the lower lumbar spinal canal (L3, L4, and L5) and its SD in both male and female patients were measured [Table 1]. The total mean of the IPD of both males and females is L3 23.6 mm (SD 1.6), L4 24.4 mm (SD 1.9), and L5 28.0 mm (SD 3.0).
APD of the canal to the APD of the vertebral body ratio
The ratio of the mean APD of the canal to the APD of the vertebral body in males and females was measured [Table 2]. The ratio for males was L3 0.50, L4 0.51, and L5 0.52; for the females, L3 0.56, L4 0.56, and L5 0.56.
| Ratio of the mean APD of the canal to the APD of the vertebral body in males and females | ||||||
| Level | Males | Females | ||||
| APD-Canal | APD-Body | Ratio | APD-Canal | APD-Body | Ratio | |
| L3 | 15.15 | 30.09 | 0.50 | 15.39 | 27.40 | 0.56 |
| L4 | 15.9 | 30.81 | 0.51 | 15.73 | 27.97 | 0.56 |
| L5 | 16.87 | 32.30 | 0.52 | 16.58 | 29.60 | 0.56 |
| Ratio of the mean IPD of the canal to the TD of the vertebral body in males and females | ||||||
| Level | Males | Females | ||||
| Mean IPD | TD | Ratio | Mean IPD | TD | Ratio | |
| L3 | 24.2 | 40.1 | 0.60 | 23.1 | 35.9 | 0.64 |
| L4 | 25.0 | 41.2 | 0.59 | 23.8 | 37.4 | 0.63 |
| L5 | 29.0 | 44.8 | 0.55 | 27.1 | 41.1 | 0.65 |
APD: Anterior-posterior diameter, IPD: Interpedicular diameter, TD: Transverse diameter
IPD of the canal to the transverse diameter of the vertebral body ratio
The ratio of the IPD of the canal to the transverse diameter of the vertebral body in males and females was measured [Table 2]. The ratio for males was L3 0.60, L4 0.59, and L5 0.55; for the females, L3 0.64, L4 0.63, and L5 0.65.
The spinal canal configurations
For L3, the prevalence of oval canal configuration was 90.7%, intermediate 7.4%, and trefoil 1.9%. Moreover, for L4, the prevalence of intermediate canal was 88.75%, trefoil 9.4%, and triangular 1.85%. Furthermore, for L5, the prevalence of triangular canal was 65.05%, trefoil 32.2%, and irregular 2.75% [Table 3].
| Level | Males | Females | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Oval | Intermediate | Trefoil | Triangular | Irregular | Oval | Intermediate | Trefoil | Triangular | Irregular | |
| L3 | 88.4% | 8.5% | 3.1% | - | - | 93% | 6.3% | 0.7% | - | - |
| L4 | - | 82.4% | 15.3% | 2.3% | - | - | 95.1% | 3.5% | 1.4% | - |
| L5 | - | - | 33.8% | 62.1% | 4.1% | - | - | 30.6% | 68% | 1.4% |
The mean APD of the lower lumbar spinal canal compared in trefoil and non-trefoil
The APD in non-trefoil as follows L3 15.5 mm, L4 16 mm, and L5 17.4 mm. Moreover, in trefoil configuration, the APD is as follows L3 13.8 mm, L4 14.8 mm, and L5 15.7 [Table 4]. Reduction of the APD in trefoil configuration showed P = 0.0001, which is highly significant.
| Mean APD of the lumbar spinal canal in trefoil versus non-trefoil configuration | ||
| Level | Mean APD (mm) | |
| Trefoil | Non-trefoil | |
| L3 | 13.8 | 15.5 |
| L4 | 14.8 | 16 |
| L5 | 15.7 | 17.4 |
| Mean IPD of the lumbar spinal canal in trefoil versus non-trefoil configuration | ||
| Level | Mean IPD (mm) | |
| Trefoil | Non-trefoil | |
| L3 | 23.6 | 23.6 |
| L4 | 25.6 | 24.8 |
| L5 | 28.2 | 28.1 |
APD: Anterior-posterior diameter, IPD: Inter-pedicular diameter
The mean IPD of the lower lumbar canal compared in trefoil and non-trefoil
The IPD in non-trefoil is as follows L3 23.6 mm, L4 24.8 mm, and L5 28.1 mm. Moreover, in trefoil configuration, the IPD was L3 23.6 mm, L4 25.6 mm, and L5 28.2 mm [Table 4].
DISCUSSION
The values of the parameters have been concluded and compared with the Caucasoid, Zulu Negroid, Nigeria, France, India, Italian, Japan, Swiss, Ohio, and California populations [Table 5 and Charts 1 and 2]. The pattern of segmental variation of the diameters was found to be like other populations, although the mean diameters were characteristically different (non-compensating).[8-17]
| Mean anterior-posterior diameter of the canal (mm) | |||||||||
| Author | Eisenstein | Gouzien | Postacchini | Marchesi | Scoles | Present study | |||
| Year | 1977 | 1990 | 1983 | 1988 | 1988 | 2023 | |||
| Population | Caucasoid | Zulu Negroid | France | Indian | Italian | Swiss | Ohio | Saudi | |
| L3 | 16 | 15 | 16 | 13.7 | 15.8 | 16.2 | 16.4 | 15.2 | |
| L4 | 16 | 15 | 17 | 13.8 | 15.1 | 16.3 | 16.5 | 15.8 | |
| L5 | 18 | 16 | 18 | 14 | 16.1 | 17.7 | 17.6 | 16.6 | |
| Mean transverse diameter of the canal (mm) | |||||||||
| Author | Amonookuofi | Gouzien | Chhabra | Panjabi | Marchesi | Hinck | Present study | ||
| Year | 1982 | 1990 | 1991 | 1992 | 1988 | 1966 | 2023 | ||
| Population | Nigeria | France | Indian | Japanese | Swiss | California | Saudi | ||
| L3 | 24.5 | 24.9 | 29.7 | 24.3 | 24.0 | 26.8 | 23.6 | ||
| L4 | 26.0 | 26.0 | 32.5 | 25.4 | 24.5 | 27.6 | 24.4 | ||
| L5 | 28.7 | 31.0 | 37.4 | 27.1 | 27.0 | 30.7 | 28.0 | ||

- Anterior-posterior diameter comparison of the lumbar canal.
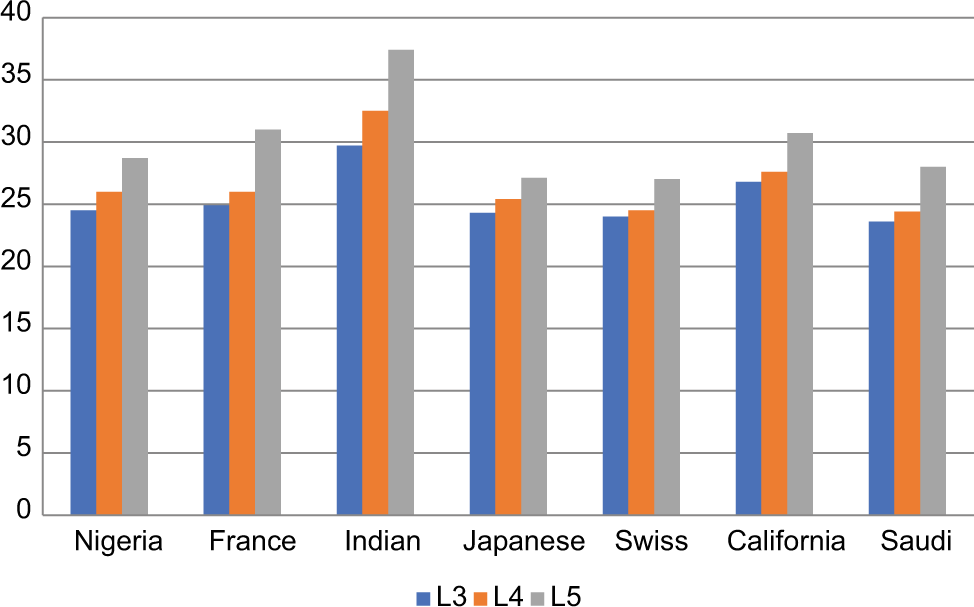
- Transverse diameter comparison of the lumbar canal.
The Indian population has the narrowest anteroposterior (AP) diameter of the lower lumbar canal, which was compensated by having the widest IPD. Compared to the Indian population, we also observed that the Saudi population is among the lowest three populations to have the narrowest AP diameter and the narrowest IPD. Based on this observation, the Saudi population is at increased risk of spinal canal stenosis by not having compensated IPD.
The trefoil configuration of the lower lumbar spinal canal can be problematic with clinical consequences; when the canal volume is reduced by bony narrowing, there is relatively less space for soft-tissue components and in case of any disk bulge, segmental displacement, or dynamic activity of extension the spinal components might be compromised in such small canal volume.
The trefoil configuration of the lower lumbar spinal canal has been an area of interest and research in different populations. One of the results observed is that the most common location of the trefoil configuration is L5 (92%).[6,7] The overall prevalence of trefoil configuration in South Africa is 14%,[6] and in Scotland is 25%.[7] Interestingly, our study found that the prevalence of trefoil configuration [Table 6] in the Saudi population is higher (32%).
| Source (Year) | Eisenstein (1980) | Papp (1995) | Present study (2023) |
|---|---|---|---|
| Population | South African | Scotland | Saudi |
| Prevalence | 14% | 25% | 32% |
Acknowledging limitations always shed light on room for improvements in the future. Our study design is a retrospective descriptive study, which could be improved by conducting a prospective study. The sample size was 279 subjects, which was calculated using the Daniel equation based on the previous prevalence of trefoil configuration, which ranged from 14% to 25% but in the Saudi population found to be higher and a larger sample is needed for future studies. Although, as mentioned earlier, the most common location of the trefoil configuration is the lower lumbar spine, a more comprehensive study is recommended. Finally, we did our measurements retrospectively on CT scans that were done either on the abdomen for different reasons of abdominal emergencies and far away from spinal pathology and lumbar CT scans that were done for traumatic causes after excluding any spinal gross pathologies such as fractures, tumors, deformities, major chronic systemic diseases, congenital anomalies (dwarfism), and metallic artifacts. This method of measurements on CT scans might be good for bony assessment in such a retrospective study, but for higher-level prospective studies to avoid radiation hazards, magnetic resonance imaging (MRI) measurements are possible and recommended.[18,19]
CONCLUSION
The pattern of segmental variation of the lower lumbar vertebral canal was found to be like other populations. Furthermore, the mean lower lumbar vertebral canal diameters were characteristically different from the other population (non-compensating). Both APD and IPD were narrowed (non-compensating) in the Saudi population. The Saudi population has a high trefoil configuration prevalence (32%).
Knowing the prevalence of this risk factor and keeping it in mind is crucial as it predicts the early failure of conservative management. It affects intraoperative decisions; since trefoil configuration is narrowed laterally, more lateral decompression is vital to alleviate pressure on the neural elements; and since more lateral decompression is required, the spine’s stability might be compromised during far lateral decompression and fixation needed. Finally, the trefoil configuration is tricky. If not kept in mind, the surgeon could easily breach into the canal medially due to its shape, which might lead to neural elements compromise.
RECOMMENDATIONS
We suggest to do a multicenter study to increase the sample size. Furthermore, we recommend to study the patients with symptoms of spinal canal stenosis for more correlations. We want to shed light on the new method of lumbar spine measurements, which can be done using MRI instead of a CT scan, which carries numerous radiation hazards.
AUTHORS CONTRIBUTIONS
KA (corresponding author) contributed to the literature review and data analysis and was a major contributor to writing the manuscript. IO contributed to the literature review, data collection and analysis, interpretation, and paper writing. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
Approved by Research Ethics Committee at Security Forces Hospital, Riyadh, Saudi Arabia. IRB number H-01-R-069, dated April 11, 2021.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patients consent forms for this study. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Variations in size of the bony lumbar canal in patients with prolapse of lumbar intervertebral discs. Clin Radiol. 1976;27:301-7.
- [CrossRef] [PubMed] [Google Scholar]
- Herniated lumbar disc syndrome and vertebral canals. Spine (Phila Pa 1976). 1986;11:433-5.
- [CrossRef] [PubMed] [Google Scholar]
- The spinal canal in symptomatic lumbar disc lesions. J Bone Joint Surg Br. 1978;60:485-7.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomic radiological variations in developmental lumbar spinal stenosis: A prospective, control-matched comparative analysis. Spine J. 2014;14:808-15.
- [CrossRef] [PubMed] [Google Scholar]
- The trefoil configuration of the lumbar vertebral canal. A study of South African skeletal material. J Bone Joint Surg Br. 1980;62:73-7.
- [CrossRef] [PubMed] [Google Scholar]
- Trefoil configuration and developmental stenosis of the lumbar vertebral canal. J Bone Joint Surg Br. 1995;77:469-72.
- [CrossRef] [PubMed] [Google Scholar]
- Morphometry of the lumbar vertebrae. An anatomic study in two Caucasoid ethnic groups. Clin Orthop Relat Res. 1983;172:296-303.
- [CrossRef] [Google Scholar]
- Preliminary results of relationship between preoperative walking ability and magnetic resonance imaging morphology in patients with lumbar canal stenosis: Comparison between trefoil and triangle types of spinal stenosis. Asian Spine J. 2017;11:580-5.
- [CrossRef] [PubMed] [Google Scholar]
- The morphometry and pathological anatomy of the lumbar spine in South African Negroes and Caucasoids with specific reference to spinal stenosis. J Bone Joint Surg Br. 1977;59:173-80.
- [CrossRef] [PubMed] [Google Scholar]
- Measurements of the normal lumbar spinal canal by computed tomography. Segmental study of L3-L4 and L4-L5 related to the height of the subject. Surg Radiol Anat. 1990;12:143-8.
- [CrossRef] [PubMed] [Google Scholar]
- Morphometric analysis of the thoracolumbar and lumbar pedicles, anatomoradiologic study. Surg Radiol Anat. 1988;10:317-22.
- [CrossRef] [PubMed] [Google Scholar]
- Vertebral body and posterior element morphology: The normal spine in middle life. Spine. 1988;13:1082-6.
- [CrossRef] [PubMed] [Google Scholar]
- Maximum and minimum lumbar interpedicular distances in normal adult Nigerians. J Anat. 1982;135:225-33.
- [Google Scholar]
- Transverse diameter of the lumbar vertebral canal in North Indians. J Anat Soc India. 1991;41:25-32.
- [Google Scholar]
- Human lumbar vertebrae. Quantitative three-dimensional anatomy. Spine. 1992;17:299-306.
- [CrossRef] [PubMed] [Google Scholar]
- Normal interpediculate distances (minimum and maximum) in children and adults. Am J Roentgenol Radium Ther Nucl Med. 1966;97:141-53.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance morphometry of the adult normal lumbar intervertebral space. Surg Radiol Anat. 2018;40:1055-61.
- [CrossRef] [PubMed] [Google Scholar]







