Translate this page into:
Obtaining a bone biopsy in acute hematogenous osteomyelitis using a new surgical instrument: A technical note
*Corresponding author: Ilnur I. Yagudin, Department of Pediatric Surgical Diseases, Izhevsk State Medical Academy, Izhevsk, Russian Federation. yagudin-ilnur@bk.ru
-
Received: ,
Accepted: ,
How to cite this article: Shklyaev PO, Yagudin II, Kiryanov NA, Yuditskiy AD. Obtaining a bone biopsy in acute hematogenous osteomyelitis using a new surgical instrument: A technical note. J Musculoskelet Surg Res, 2023;7:210-3.
Abstract
Acute hematogenous osteomyelitis is an infectious and inflammatory tubular bone disease involving the bone marrow. The final diagnosis is made based on a morphological study obtained from a bone biopsy. We have developed and patented a surgical instrument (Patent RU No 176629) for one-stage osteoperforation and trepan biopsy. Bone biopsy specimens obtained have been tested for their suitability for morphological examination, namely light and electron microscopy. It has a diagnostic and therapeutic function. This report aimed to describe a new bone biopsy tool that allows obtaining specimens suitable for morphological studies.
Keywords
Acute hematogenous osteomyelitis
Osteoperforation
Trepan-biopsy
Light microscopy
Electron microscopy
INTRODUCTION
Acute hematogenous osteomyelitis (AHO) is an infectious and inflammatory bone disease involving the bone and bone marrow.[1] This disease can occur at any age but predominantly affects children. Some data have identified the childhood age period with the most frequent occurrence between 7 and 10 years of age.[2] This is explained by the fact that bones are formed in the metaphyseal areas of growth, which leads to the slowing of blood flow in this area, that is, stasis. Slowing hemodynamics of metaphyseal areas increases the likelihood of pathogenic microflora lingering and affecting these areas.[3] This is where the development of osteomyelitis usually begins. Early diagnosis is important in this disease to reduce the risk of complications. The final diagnosis is made based on a morphological study obtained from a bone biopsy, and the specimen is sent for culture.[4] At the moment, there are a large number of analogs that can be used to obtain a biopsy of bone tissue. The distinctive feature of our new instrument is the one-stage osteoperforation and trepan biopsy. This report aimed to describe a new bone biopsy tool that allows obtaining specimens suitable for morphological studies. It is important to understand that this procedure has a diagnostic and therapeutic function.
OPERATIVE TECHNIQUE
We have developed and patented a surgical instrument to perform osteoperforation and trepan biopsy for a single-stage diagnostic and therapeutic procedure (Patent RU No.176629). The device’s dimensions are 12 cm long and 7 mm in diameter. This instrument makes it possible to perforate the bone tissue to take a bone biopsy and then leave it in the cavity of the tubular bone to drain it later [Figure 1]. The principle of the operation is to make an incision in the soft tissues and then access the affected bone, namely, the area where the abscess is supposed to be located. The localization is chosen based on the results of the radiological diagnostic methods. Once the area is identified, the surgeon uses an instrument for simultaneous osteoperforation and trepan biopsy [Figure 2]. The instrument is placed in the selected area and the trepan is attached to it. Then light, smooth, and progressive movements are used to drill the bone tissue.
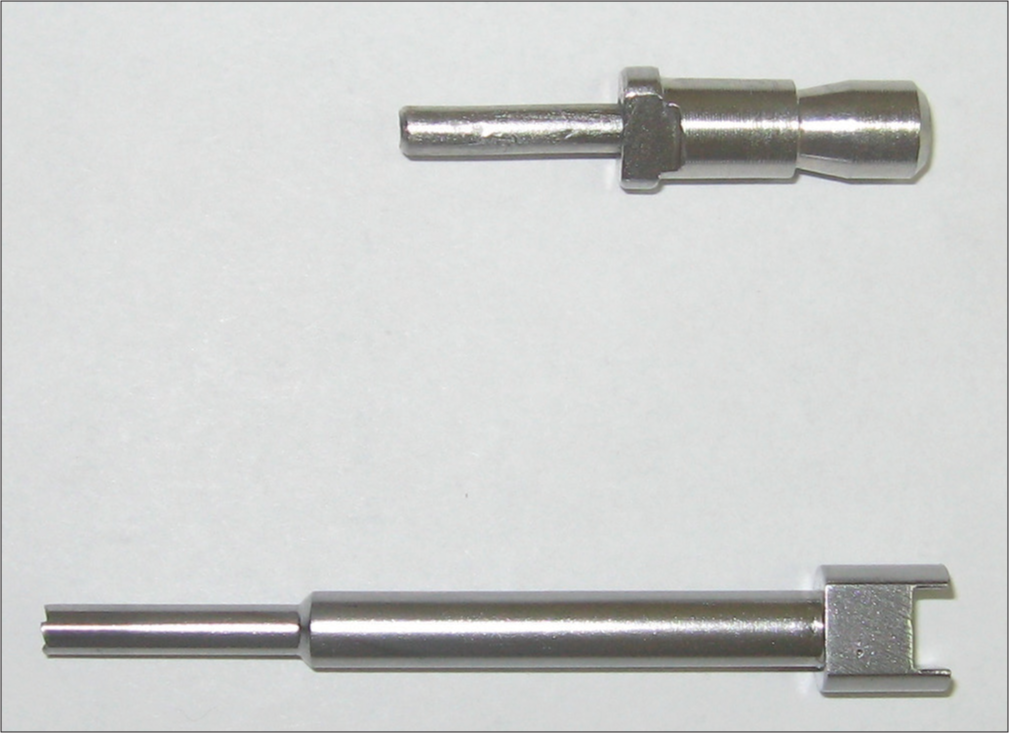
- Instrument for trepan-biopsy and osteoperforation.
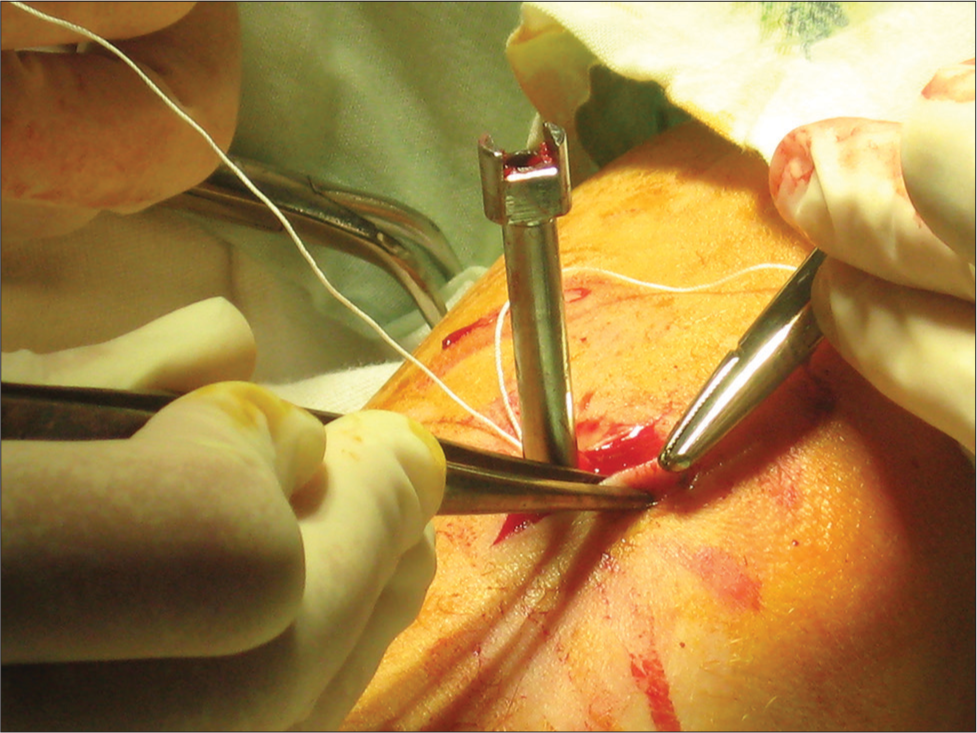
- Inserting an instrument into the bone.
After that, the trepan is removed and the instrument implanted in the bone remains. It is necessary for further drainage of the affected area. The following need to be done to perform a biopsy: A pusher is inserted, allowing the surgeon to get a bone biopsy. Thus, this surgical instrument allows one-stage osteoperforation and trepan biopsy. It is important to note that the obtained biopsy specimens should simultaneously be sent for bacterial culture as it is necessary to identify the pathological culture for diagnosis. This is necessary to choose the correct antibiotic therapy. Ten operations were performed during the development of the instrument, and 20 biopsy specimens were obtained. The obtained biopsy specimens were not damaged and met the quality standards, which allowed morphological and laboratory studies. This method is distinguished by the fact that it allows performing osteoperforation and trepan biopsy in one step, so the instrument has a diagnostic and therapeutic function. The cost of the instrument is low because it does not contain electronic devices and expensive materials, and the tool itself is made of steel, so it belongs to reusable tools. Furthermore, its low cost is because the instrument is reusable. When using this instrument, the speed of surgery is significantly increased.
DISCUSSION
As an inflammatory process caused by a bacterial pathogen, AHO proceeds with alteration, exudation and proliferation stages.[5] During these periods, one of the important pathological factors is an increase in tissue edema. Still, since the inflammation is localized inside the bone, the edema is exacerbated because the dense structure of the bone does not allow it to respond to even minimal tissue stretching. Hence, the edema squeezes the tissue even more, exacerbating tissue damage by ischemia.[6] As a result, osteoperforation with a trepan is performed to release pus and reduce edema, leading to reduced ischemia and getting rid of bacterial semination of the body.[7]
Thanks to a new surgical instrument for osteoperforation and trepan biopsy, the results were obtained, and it proved to be excellent in obtaining bone biopsy specimens. The quality of the bone biopsy specimens obtained with the new surgical instrument was analyzed. The histological preparations made from bone biopsy specimens were entirely suitable and met all quality requirements for examining morphological structures. Namely, both light and electron microscopy were performed. The micropreparation was stained with hematoxylin and eosin and showed bone marrow edema and infiltration with a large number of leukocytes [Figure 3]. When stained according to van Gibson’s, interbody spaces and fibrous structures edema is shown in [Figure 4]. Next, electron microscopy was performed to assess qualitative parameters, which showed excellent results. Proliferative and vascular-exudative reaction near the inflammation focus, near the Havers’ canal of the developing osteon of the compact substance of the cortical bone layer, was detected. Adhesion and marginal standing of erythrocytes and leukocytes in the venule are visible. Emigration of leukocytes (leukodiapedesis) through the vessel wall into the perivascular space [Figure 5]. Morphological images from bone tissue biopsy specimens, which were obtained using the new surgical tool, proved useful in practice for diagnosing AHO. This instrument can be used to treat children from the age of 3 years and only on the long tubular bones. Therefore, limitations are the use in treating children under the age of 3 years and the use on other than long bones. Unless the lesion is near the growth plate and the surgeon needs to avoid injuring it. To clarify the diagnosis, a computed tomography diagnosis is also necessary.
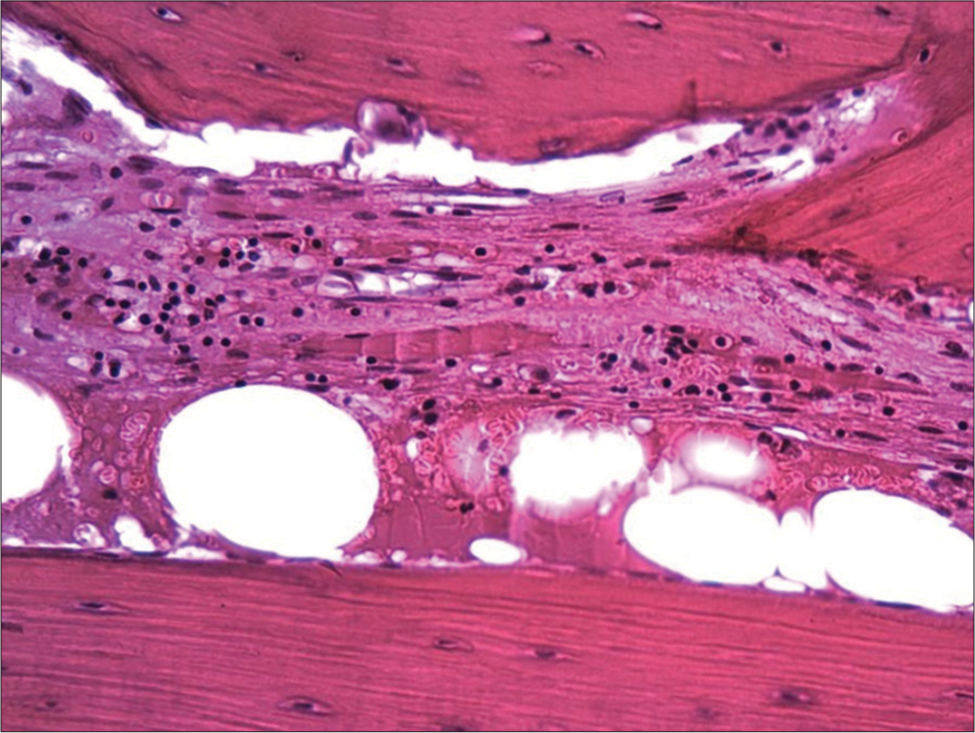
- Bone marrow edema and leukocyte infiltration. Light microscopy. Hematoxylin and eosin staining. Magnification ×100.
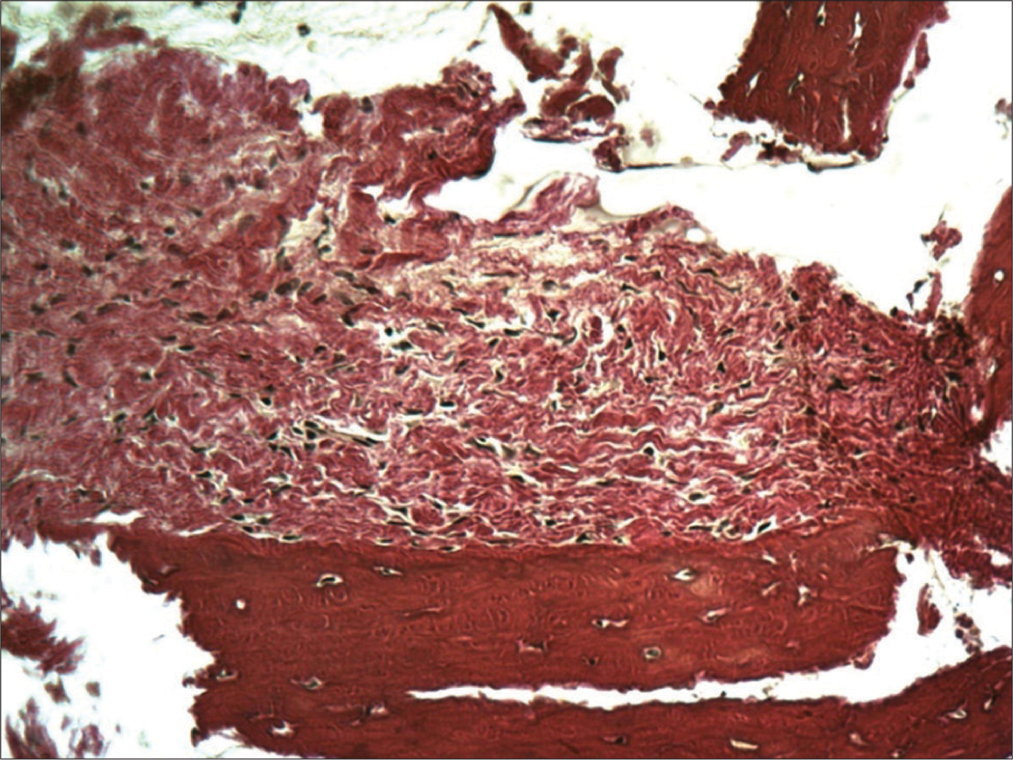
- Swelling of fibrous structures in the interbody spaces. Light microscopy. Van Gieson staining. Magnification ×200.

- Adhesion and marginal standing of erythrocytes and leukocytes in the venule. Emigration of leukocytes leukodiapedesis) through the vessel wall into the perivascular space. Scanning electron microscopy.
CONCLUSION
The presented instrument allows for performing a single-step osteoperforation and trepan biopsy perfectly. Furthermore, the obtained biopsy specimens are suitable for further morphological study. It is important to note that the instrument is easy to use and has a low cost in creation and operation, as it excludes electronic and massive add-ons. Due to this, the device can be relevantly used by hospitals with varying degrees of funding, potentially improving performance rates. At present, this surgical instrument is already being used in clinical practice, proving its applicability.
ETHICAL APPROVAL
The study followed the principles of the Declaration of Helsinki and was approved by the Ethics Committee of the Izhevsk State Medical Academy (protocol number 550).
AUTHOR’S CONTRIBUTIONS
POS carried out the conception and technique idea and performed the surgery. IIY, NAK, and ADY acquired data, organized data, and performed a literature search. The authors drafted the manuscript and designed the figures. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Acute hematogenous osteomyelitis in children: Pathogenesis, diagnosis, and treatment. Orthop Clin North Am. 2017;48:199-208.
- [CrossRef] [PubMed] [Google Scholar]
- Acute hematogenous osteomyelitis in children: Clinical presentation and management. Infect Drug Resist. 2020;13:4459-73.
- [CrossRef] [PubMed] [Google Scholar]
- Bone and joint infections in children: Acute hematogenous osteomyelitis. Indian J Pediatr. 2016;83:817-24.
- [CrossRef] [Google Scholar]
- Acute haematogenous osteomyelitis in children: Diagnostic algorithm and treatment strategies. Orthopade. 2017;46:541-56.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment for Brodie's abscess of the radius in an adolescent: A case report. Int J Surg Case Rep. 2020;73:134-40.
- [CrossRef] [PubMed] [Google Scholar]
- Physeal separation in pediatric osteomyelitis. Pediatr Radiol. 2019;49:1229-33.
- [CrossRef] [PubMed] [Google Scholar]







