Translate this page into:
Posterior approach versus lateral approach for primary total hip arthroplasty: An updated systematic review and meta-analysis
2 College of Medicine, King Saud bin Abdulaziz University for Health Sciences; King Abdullah International Medical Research Center; Department of Orthopedic Surgery, King Abdulaziz Medical City, Jeddah, Saudi Arabia
Corresponding Author:
Abdullah A Ghaddaf
College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Jeddah 21423; King Abdullah International Medical Research Center, Jeddah
Saudi Arabia
abdullahg.official@gmail.com
| How to cite this article: Ghaddaf AA, Alomari MS, Abdulhamid AS, Alshehri MS. Posterior approach versus lateral approach for primary total hip arthroplasty: An updated systematic review and meta-analysis. J Musculoskelet Surg Res 2021;5:85-95 |
Abstract
Total hip arthroplasty (THA) has become one of the most therapeutic and cost-effective procedures that are frequently carried out in orthopedic surgery. This review aimed to systematically compare postoperative outcomes between the two most commonly performed surgical approaches for THA posterior approach (PA) and lateral approach (LA) for abductor strength, operative time, perioperative blood loss, and limb length discrepancy. We searched Medline, Ovid, Europe PMC, Web of Science, and CENTRAL to identify eligible studies comparing PA and LA for patients who underwent primary THA for any indication. No restrictions on date or language were applied. Out of 15,764 records identified, 16 studies were deemed eligible, including five randomized controlled trials, five prospective cohort studies, and six retrospective cohort studies, providing data for 16,964 patients. PA was associated with a significant recovery in abductor strength (standardized mean difference (SMD) = 0.39, 95% confidence interval [CI] 0.14–0.63) postoperatively. No significant difference between PA and LA was found in terms of operative time (SMD = 0.05, 95% CI − 0.40–0.50), perioperative blood loss (SMD = −0.29, 95% CI − 0.62–0.03), or mean radiographic limb length discrepancy (LLD) (SMD = 0.02, 95% CI − 0.21–0.25). After removing the heterogeneity source, the sensitivity analysis showed consistent results except for operative time, which was significantly lower in the PA group (SMD= −0.72, 95% CI − 0.81–0.62). This review found PA to be associated with a significant enhancement in abductor strength recovery following THA. No significant difference was found between the two surgical approaches in operative time, perioperative blood loss, and LLD. However, after removing the source of heterogeneity, the sensitivity analysis showed a significantly lower mean operative time in favor of the PA group. Further studies are warranted to delineate the surgical approach's influence on abductor strength recovery in the long term.
Introduction
Since its commencement in the middle of the 20th century, total hip arthroplasty (THA) heralded a new era in arthroplasty and became one of the most therapeutic and cost-effective procedures that are frequently carried out in orthopedic surgery.[1],[2] It is expected that the quality of life will be considerably improved following THA.[3] Determining the surgical approach that confers the most favorable postoperative clinical outcomes following THA has recently become an area of interest in the literature.[4] The two most commonly performed surgical approaches for THA worldwide are the posterior approach (PA) and lateral approach (LA). Globally, PA is more commonly used for THA (45%) compared to LA (42%).[5] Studies comparing the two surgical approaches have shown conflicting results, leaving uncertainty about the surgical approach choice for THA.[4],[6],[7],[8],[9],[10],[11]
A recent systematic review and meta-analysis concluded that PA was associated with a reduction in Trendelenburg gait, dislocation rate, heterotopic ossification, and stem malposition. However, the review was limited by a relatively small sample size due to the paucity of studies.[12] Since the most recent meta-analysis, nine further studies that compare PA to LA representing 16,319 patients were introduced to the literature since the most recent meta-analysis.[13],[14],[15],[16],[17],[18],[19]
Given the addition of 16,319 patients, we sought to conduct an updated systematic review and meta-analysis comparing PA and LA with specific regard to abductor strength at different time points, operative time, perioperative blood loss, and radiographic limb length discrepancy (LLD).
Materials and Methods
This systematic review was conducted according to a protocol established at inception and registered at PROSPERO (CRD42020176864). This systematic review's reporting follows the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) checklist.[20]
Eligibility criteria
This systematic review included all available randomized controlled trials (RCTs), prospective cohort studies (PCSs), and retrospective cohort studies (RCSs) that involved a direct comparison between PA and LA and reported at least one of the following outcomes: abductor strength, operative time, perioperative blood loss, or radiographic LLD for patients who underwent primary THA for any indication. Abductor strength should be measured objectively using a dynamometer or manually, according to the Medical Research Council.[21]
Although systematic reviews of RCTs are considered to provide the highest level of evidence, a discrepancy has been found to exist between the effect sizes obtained from RCTs and the effect sizes obtained from observational studies for the same treatment arms.[22],[23],[24],[25] Moreover, the incorporation of well-designed observational studies along with high-quality RCTs provides an insight into various clinical settings, a broader set of patients, and longer periods of treatment effects, enabling the assessment of small treatment effects and rare outcome measures.[26],[27] Therefore, we sought to include well-designed PCSs and RCSs along with RCTs.
For the purpose of this review, LA was defined as the dissection of one-third of the gluteus medius without trochanteric osteotomy. The descriptions of Hardinge as well as Mulliken et al., and Frndak et al. modification of the Hardinge approach were accepted as LA.[28],[29],[30] The descriptions of Kocher and Langenbeck and the modifications by Gibson and Moore of that approach were accepted as PA.[31],[32],[33] Studies reporting revision THA results, bipolar hemiarthroplasty, and hip resurfacing were excluded.
Search strategy
We searched the electronic databases Medline/PubMed, Ovid, Europe PMC, and Web of Science. Medical Subject Headings for each electronic database was extensively explored to retrieve the different keywords assigned for the same concept. No restrictions on date or language were applied. The search strategy is shown in the supplementary material. All identified articles were exported to EndNote X9 (Clarivate, Philadelphia, Pennsylvania, USA) to manage references and remove duplicates. We also searched the following trial registries: Cochrane Central Register for Controlled Trials (CENTRAL), ISRCTN registry, Australian New Zealand Clinical Trials Registry, and UMIN Clinical Trials Registry. We screened abstracts provided by the Orthopedic Proceedings Journal. The last search was done on the May 2, 2020. We searched bibliographic references of the included studies thoroughly to recognize articles that might not appear during the systematic search of the electronic databases. We contacted the authors of the eligible studies in case of missing data to obtain further information.
Study selection and data extraction
Two independent review authors (ASA and MSA) screened titles and abstracts of the identified articles by applying the eligibility criteria of this systematic review, and any disagreement regarding the eligibility of a particular study was resolved by discussion. If consensus could not be achieved with discussion, a third reviewer (AAG) decision was considered. The two independent review authors (ASA and MSA) then read the full texts of the eligible articles and retrieved data using a predefined data collection file. The following data were extracted from included studies: name of the first author, year of publication, mean follow-up, study design, surgical approaches used, the number of patients assigned for each surgical approach, year(s) data collected, final diagnoses, and demographic data (i.e., gender, mean age, and mean body mass index [BMI]). The desired outcomes, including mean postoperative abductor strength (±standard deviation [SD]) at different time points, mean operative time in minutes (±SD), mean peri-operative blood loss (±SD), and mean postoperative LLD (±SD), were extracted. For studies with multiple publications, data were extracted from the original study and only the data related to abductor strength (if applicable) were extracted from follow-up publications.
Meta-analysis
Meta-analyses were conducted using Comprehensive Meta-Analysis version 3 (Biostat, Inc. Eaglewood, New Jersey, USA) using the random-effects model. The measure of effect used to express the desired outcomes was the standardized mean differences (SMD). Between-study statistical heterogeneity was assessed using I2 and the P of the χ2 test for heterogeneity. A confidence level of 95% was used, and P < 0.05 was considered to be significant to reject the null hypothesis. We performed a subgroup analysis for the primary outcome, abductor strength, according to the following follow-up periods: 3 months, 6 months, and ≥12 months. If the statistical heterogeneity was significant (I2 > 50%), a sensitivity analysis was performed by removing each individual study at a time to identify the potential source of heterogeneity.
Risk of bias assessment
Two independent review authors (ASA and MSA) assessed the quality of eligible RCTs using the Revised Cochrane Bias Risk Assessment tool.[34] The quality of nonrandomized studies (i.e., PCSs and RCSs) was assessed using The Newcastle Ottawa Quality Assessment Scale (NOS).[35] Any disagreement was resolved by discussion and decision of the third review author (AAG) if it was not settled by discussion. The potential publication bias was investigated through visual inspection of the funnel plot of the primary outcome (i.e., abductor strength) along with Egger's test assessing the funnel plot asymmetry.[36]
Results
The literature search yielded 15764 potentially related articles. After removing duplicates, screening abstracts, and reading 42 full-text articles, 16 accessible studies (18 publications) were found to be eligible.[13],[14],[15],[16],[17],[18],[37],[38],[39],[40],[41],[42],[43],[44],[45],[46] Five studies were RCTs (6 publications),[13],[16],[37],[42],[43],[44] five were PCSs (6 publications),[14],[17],[38],[39],[41],[45] and six were RCSs.[15],[18],[19],[40],[46],[47] The review progress in this study is shown in the PRISMA flow chart [Figure - 1].
 |
| Figure 1: Study flow diagram |
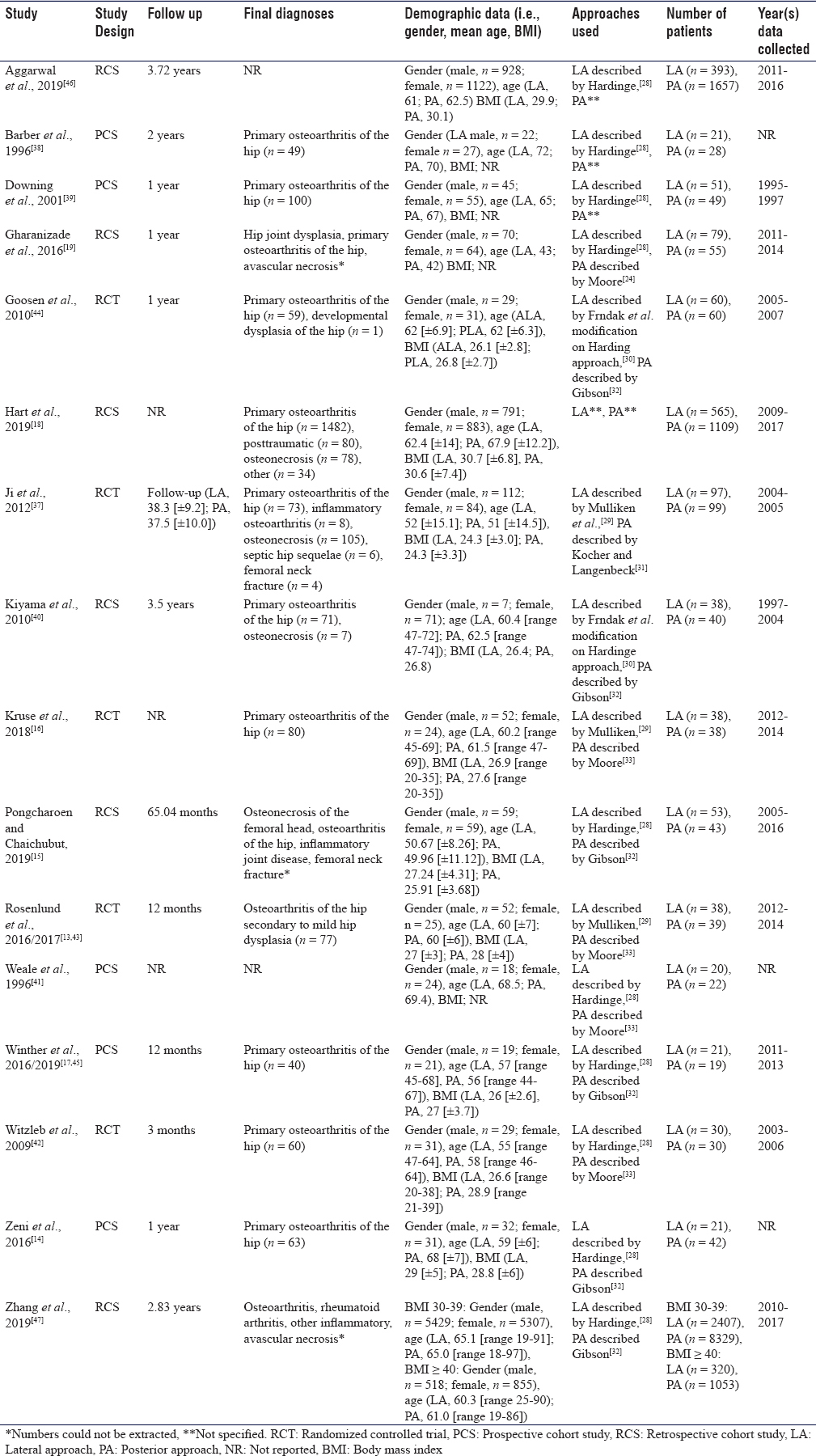
Trial characteristics
The included studies were published between 1996 and 2019. The overall number of patients was 16,964 (4,252 (25.1%) and 12,712 (74.9%) allocated to LA and PA, respectively). The mean age of the patients ranged between 42 and 72 years. The detailed characteristics of the included studies are shown in [Table - 1].
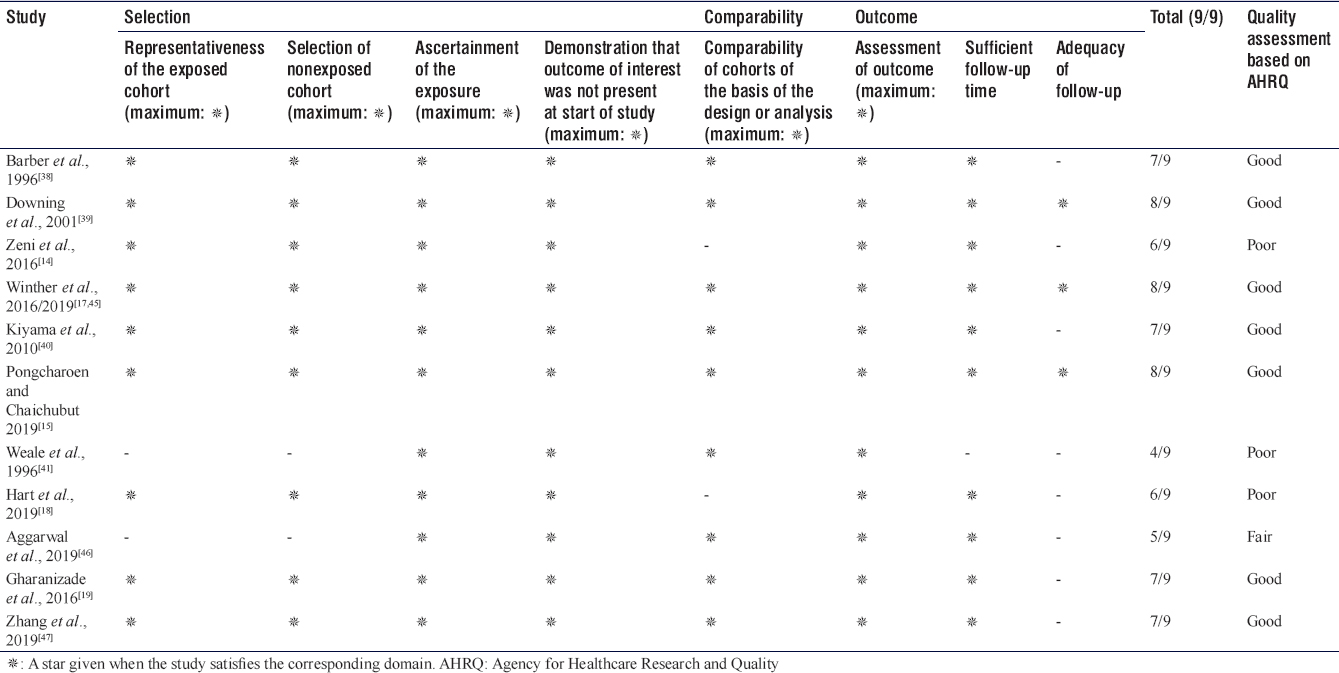
Risk of bias assessment
All of the included RCTs were found to have an overall low risk of bias according to the Revised Cochrane Bias Risk Assessment tool [Table - 2]. Of the 11 observational studies, seven were found to have an overall good quality, one had fair quality, and three had poor quality according to NOS [Table - 3]. The funnel plot for the primary outcome was asymmetrical and Egger's test showed a statistical significance (P < 0.01), suggesting evidence of publication bias [Supplementary Figure 1].


Abductor strength
Six studies (7 publications), including a total of 556 participants (PA, n = 288; LA, n = 268), reported mean abductor strength.[13],[14],[17],[38],[39],[40],[45] All of the studies measured abductor strength objectively using a dynamometer except for Barber et al.,[38] who manually measured the abductor strength according to the Medical Research Council.[21] Overall, there was a significant enhancement in abductor strength recovery following THA in favor of PA (SMD = 0.39, 95% confidence interval [CI] 0.14–0.63, P = 0.002; I2 = 50%) [Figure - 2]. The subgroup analysis revealed that the recovery in abductor strength conferred by PA reached statistical significance at 6 months (SMD = 0.85, 95% CI 0.21–1.50, P = 0.009; I2 = 0%) and ≥12 months postoperatively (SMD = 0.34, 95% CI 0.05–0.64, P = 0.02; I2 = 50%). After sensitivity analysis, there was still a statistical significance in abductor strength recovery in favor of PA (SMD = 0.51, 95% CI 0.28–0.75, P < 0.001; I2 = 8%) [Table - 4].
 |
| Figure 2: Mean abductor strength (posterior approach versus lateral approach) |

Operative time
The mean operative time was reported by seven studies, including a total of 12,949 participants (PA, n = 9,715; LA, n = 3,234).[15],[18],[37],[41],[43],[47] Operative time ranged from 76.1 to 109.8 min for PA and from 60 to 132 min for LA. No significant difference was found between PA and LA (SMD = 0.05, 95% CI − 0.40–0.50, P = 0.82; I2 = 98%) [Figure - 3]. Zhang et al. provided mean operative time for two BMI classes: the obese class (BMI 30–39) and morbidly obese class (BMI ≥40). Therefore, we decided to include the mean operative time for the obese class (BMI 30–39) in the analysis and to narratively report the mean operative time for the morbidly obese class (BMI ≥ 40), which also showed no significant difference between PA and LA (SMD = −0.01, 95% CI − 0.14–0.10, P = 0.79).[47] After removing the source of heterogeneity, operative time ranged from 78 to 109.8 min for PA and from 107 to 132 min for LA. The sensitivity analysis showed a significant reduction in mean operative time in favor of PA (SMD = −0.72, 95% CI − 0.81–0.62, P < 0.001; I2 = 0%) [Table - 4].
 |
| Figure 3: Mean operative time (posterior approach versus lateral approach) |
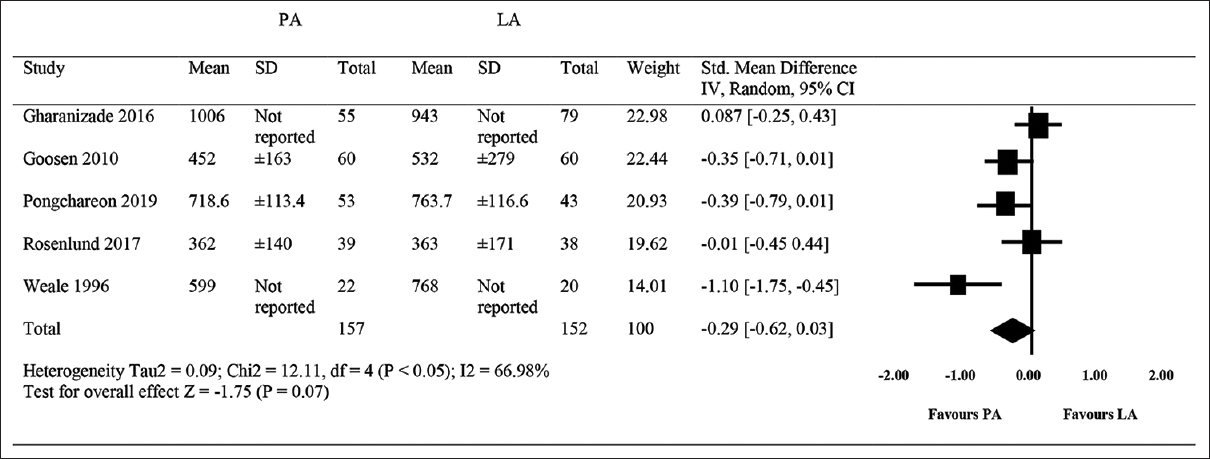
Perioperative blood loss
Five studies reported mean perioperative blood loss, including a total of 209 participants (PA, n = 157; LA, n = 152).[15],[19],[41],[43],[44] Perioperative bleeding volume ranged from 362 to 1006 ml for PA and from 363 to 943 ml for LA. The amount of bleeding volume was similar between PA and LA (SMD = −0.29, 95% CI − 0.62-0.03, P = 0.07; I2 = 67%) [Figure - 4]. Similarly, perioperative bleeding volume ranged from 362 to 1006 ml for PA and from 363 to 943 ml for LA. The sensitivity analysis also did not show any significant difference in mean perioperative blood loss (SMD = −0.16, 95% CI − 0.40–0.08, P = 0.18; I2 = 37%) [Table - 4].
 |
| Figure 4: Peri-operative blood loss (posterior approach versus lateral approach) |
Limb length discrepancy
Four studies reported mean radiographic LLD, including a total of 408 participants (PA, n = 193; LA, n = 215).[16],[19],[40],[44] LLD ranged from − 0.05 to 3.3 cm for PA and from 0.05 to 3.5 cm for LA. The pooled effect showed no significant difference between the two groups (SMD = 0.02, 95% CI − 0.21–0.25, P = 0.85; I2 = 30%) [Figure - 5].
 |
| Figure 5: Mean radiographic limb length discrepancy (posterior approach versus lateral approach) |
Discussion
Our results demonstrated a significant enhancement in the abductor strength recovery associated with PA at 6 months and ≥12 months' postoperatively. We found PA and LA to have comparable results in terms of mean operative time, mean perioperative blood loss, and mean radiographic LLD. After removing the source of heterogeneity, the sensitivity analysis showed consistent results except for operative time, which was significantly lower in the PA group.
Our findings are consistent with some of the previous studies revealing a significantly better abductor muscle strength in patients allocated to PA for up to 2 years' postoperatively.[48],[49],[50],[51] A recent systematic review and meta-analysis found that patients allocated to LA have significantly higher Trendelenburg gait at a mean of 15.5 months.[11] High Trendelenburg gait manifestations in patients allocated to LA have been attributed to the intraoperative dissection of the abductor muscle group (i.e., gluteus medius and minimus).[29],[52],[53] Other studies, however, found that Trendelenburg gait manifestations associated with LA disappeared within 12 months' postoperatively.[6],[12],[54] The absence of Trendelenburg signs in the LA group at 12 months has been attributed to the over-activation of the gluteus medius muscle in order to compensate for the weakness and support the pelvis during walking.[55] A recent RCT found abductor strength to be significantly better in the LA group at 3 months, 6 months, and 12 months. We believe that this improvement is attributed to their use of a modified antero LA, which does not involve cutting through gluteus medius muscle.[56] Judd et al. and Rasch et al. found abductor strength to be similar in patients who underwent THA through PA compared to healthy controls at 3 months, 6 months, and 12 months but not as strong as contralateral healthy limb even 2 years' postoperatively.[57],[58] A gait analysis study conducted by Madsen et al. found 30% of patients in the PA group were restored to their normal gait, while none of the patients in the LA group were restored to their normal gait at 6 months' postoperatively.[59] Furthermore, Meermans et al. reported that postoperative gait analysis results were similar regardless of the surgical approach.[8]
Our findings suggest no statistical difference in operative time between the two surgical approaches with high statistical heterogeneity. However, after removing the source of heterogeneity, the sensitivity analysis showed a significantly lower mean operative time in favor of the PA group. Cantrell et al., in a systematic review, stated that the mean operative time was relatively stable and not amenable to be influenced by the surgical approach over the past 20 years.[60] Some studies found LA to be higher in terms of mean operative time,[61],[62],[63] whereas Rasch et al. found PA to be higher.[58] The discrepancy in mean operative time has been attributed to the impact of many factors, including BMI, surgeon experience, and presence of trainee.[56],[60]
Our findings revealed no significant difference in mean bleeding volume between PA and LA. Even after removing the source of heterogeneity, the sensitivity analysis did not show any significant difference in mean perioperative blood loss. However, many studies found that LA is associated with a higher amount of blood loss.[62],[63]
Our findings demonstrated no statistical difference between the two surgical approaches in terms of mean radiographic LLD. Previous reviews consistently showed no significant difference.[11],[12] Gore et al. displayed that mean LLD was significantly lower in female patients allocated to the PA, while it was significantly lower in male patients allocated to the LA.[50]
The present review has some limitations. First, it was limited by the small number of included RCTs, and most of the data was derived from observational studies. However, all of the included RCTs had an overall low risk of bias and most of the observational studies were found to have good quality. Second, although the results of abductor strength displayed by our review were measured objectively and unlikely to be influenced by outcome assessors, our review was not able to determine whether the enhancement in abductor strength recovery associated with PA continue to be significant on the long-term follow up (i.e., >2 years).
Conclusion
This review displayed a significant improvement in abductor strength associated with PA post-THA. No significant difference was found between PA and LA in terms of mean operative time, mean bleeding volume, and mean radiographic LLD. However, after removing the source of heterogeneity, the sensitivity analysis showed a significantly lower mean operative time in favor of the PA group. Further RCTs are warranted to assess the influence of the surgical approach on abductor strength in the long term.
Ethical approval
The authors confirm that this review had been prepared in accordance with COPE roles and regulations. Given the nature of the review, the IRB review was not required.
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Author contributions
AAG contributed to the research idea, design of the study, data extraction, statistical analysis and interpretation, risk of bias assessment, writing, and editing, MSAO contributed the design of the study, data extraction, statistical analysis and interpretation, writing, and editing, ASA, contributed to the data extraction, statistical analysis and interpretation, risk of bias assessment, writing, and editing, MSAS contributed to the statistical analysis and interpretation, and editing. All authors have critically reviewed and approved the final draft and are responsible for the manuscript's content and similarity index.
Pubmed – 6921
((“Total hip arthroplasty” OR “hip joint replacement” OR “total hip replacement” OR “Arthroplasty, Replacement, Hip”[Mesh]) AND (“method” OR “approach” OR “procedure” OR “technique”) AND ((“Leg Length Inequality”[Mesh] OR “LLD” OR “leg leg discrepancy” OR “leg length discrepancy”) OR (“lateral”) OR (“abductor muscle power”) OR (“abductor muscle strength”) OR (“blood loss”) OR (“Muscle, Skeletal/injuries”[Mesh]) OR (“Muscle, Skeletal/physiopathology”[Mesh]) OR (“Muscle, Skeletal/pathology”[Mesh]) OR (“Muscle, Skeletal/physiology”[Mesh]) OR (“Tendon Injuries/physiopathology”[Mesh]) OR (“Blood Loss, Surgical”[Mesh]) OR (“posterior”) OR (“hardinge”) OR (“anterolateral”) OR (“direct lateral”) OR (Kocher-Langenbeck) OR (“Postoperative Complications”[Mesh]) OR (“Southern/Moore”) OR (“lower limb discrepancy”) OR (“posterolateral”)))
Europe PMC - 8524
(“Total hip arthroplasty” OR “hip joint replacement” OR “total hip replacement” OR “Arthroplasty, Replacement, Hip”) AND (“method” OR “approach” OR “procedure” OR “technique”) AND ((“Leg Length Inequality” OR “LLD” OR “leg leg discrepancy” OR “leg length discrepancy”) OR (“lateral”) OR (“abductor muscle power”) OR (“abductor muscle strength”) OR (“blood loss”) OR (“Muscle, Skeletal/injuries”) OR (“Muscle, Skeletal/physiopathology”) OR (“Muscle, Skeletal/pathology”) OR (“Muscle, Skeletal/physiology”) OR (“Tendon Injuries/physiopathology”) OR (“Blood Loss, Surgical”) OR (“posterior”) OR (“hardinge”) OR (“anterolateral”) OR (“direct lateral”) OR (“Kocher-Langenbeck”) OR (“Postoperative Complications”) OR (“Southern/Moore”) OR (“lower limb discrepancy”) OR (“posterolateral”)) AND ((“posterolateral”) OR (“direct lateral”) OR (“posterior”) OR (“lateral”))
Ovid – 86
((“Total hip arthroplasty” or “hip joint replacement” or “total hip replacement” or “Arthroplasty, Replacement, Hip”) and (“method” or “approach” or “procedure” or “technique”) and (“Leg Length Inequality” or “LLD” or “leg leg discrepancy” or “leg length discrepancy” or “lateral” or “abductor muscle power” or “abductor muscle strength” or “blood loss” or “Muscle, Skeletal/injuries” or “Muscle, Skeletal/physiopathology” or “Muscle, Skeletal/pathology” or “Muscle, Skeletal/physiology” or “Tendon Injuries/physiopathology” or “Blood Loss, Surgical” or “length of stay” or “posterior” or “hardinge” or “anterolateral” or “direct lateral” or Kocher-Langenbeck or “Postoperative Complications” or “Southern/Moore” or “lower limb discrepancy”))
Web of Science – 233
TI=((“Total hip arthroplasty” OR “hip joint replacement” OR “total hip replacement” OR “Arthroplasty, Replacement, Hip” ) AND (“method” OR “approach” OR “procedure” OR “technique”) AND ((“Leg Length Inequality” OR “LLD” OR “leg leg discrepancy” OR “leg length discrepancy”) OR (“lateral”) OR (“abductor muscle power”) OR (“abductor muscle strength”) OR (“blood loss”) OR (“Muscle, Skeletal/injuries”) OR (“Muscle, Skeletal/physiopathology”) OR (“Muscle, Skeletal/pathology”) OR (“Muscle, Skeletal/physiology”) OR (“Tendon Injuries/physiopathology”) OR (“Blood Loss, Surgical”) OR (“length of stay”) OR (“posterior”) OR (“hardinge”) OR (“anterolateral”) OR (“direct lateral”) OR (“Kocher-Langenbeck”) OR (“Postoperative Complications”) OR (“Southern/Moore”) OR (“lower limb discrepancy”) OR (“posterolateral”)))
Cochrane – 370
ID Search
#1 MeSH descriptor: [Arthroplasty, Replacement, Hip] this term only
#2 “Total hip arthroplasty”
#3 “Total hip replacement”
#4 method
#5 technique
#6 approach
#7 procedure
#8 MeSH descriptor: [Leg Length Inequality] this term only
#9 “leg length discrepancy”
#10 MeSH descriptor: [Muscle Strength] this term only
#11 ”abductor”
#12 MeSH descriptor: [Postoperative Complications] this term only
#13 MeSH descriptor: [Blood Loss, Surgical] this term only
#14 (#1 OR #2 OR #3) AND (#4 OR #5 OR #6 OR #7) AND (#8 OR #9 OR #10 OR #11 OR #12 OR #13)
| 1. | Daigle ME, Weinstein AM, Katz JN, Losina E. The cost-effectiveness of total joint arthroplasty: A systematic review of published literature. Best Pract Res Clin Rheumatol 2012;26:649-58. [Google Scholar] |
| 2. | Learmonth ID, Young C, Rorabeck C. The operation of the century: Total hip replacement. Lancet 2007;370:1508-19. [Google Scholar] |
| 3. | Weber M, Craiovan B, Woerner ML, Schwarz T, Grifka J, Renkawitz TF. Predictors of outcome after primary total joint replacement. J Arthroplasty 2018;33:431-5. [Google Scholar] |
| 4. | Petis S, Howard JL, Lanting BL, Vasarhelyi EM. Surgical approach in primary total hip arthroplasty: Anatomy, technique and clinical outcomes. Can J Surg 2015;58:128-39. [Google Scholar] |
| 5. | Chechik O, Khashan M, Lador R, Salai M, Amar E. Surgical approach and prosthesis fixation in hip arthroplasty world wide. Arch Orthop Trauma Surg 2013;133:1595-600. [Google Scholar] |
| 6. | Masonis JL, Bourne RB. Surgical approach, abductor function, and total hip arthroplasty dislocation. Clin Orthop Relat Res 2002;405:46-53. [Google Scholar] |
| 7. | Cheng T, Feng JG, Liu T, Zhang XL. Minimally invasive total hip arthroplasty: A systematic review. Int Orthop 2009;33:1473-81. [Google Scholar] |
| 8. | Meermans G, Konan S, Das R, Volpin A, Haddad FS. The direct anterior approach in total hip arthroplasty: A systematic review of the literature. Bone Joint J 2017;99-B: 732-40. [Google Scholar] |
| 9. | Wang Z, Hou JZ, Wu CH, Zhou YJ, Gu XM, Wang HH, et al. A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty. J Orthop Surg Res 2018;13:229. [Google Scholar] |
| 10. | Moyer R, Lanting B, Marsh J, Al-Jurayyan A, Churchill L, Howard J, et al. Postoperative gait mechanics after total hip arthroplasty: A systematic review and meta-analysis. JBJS Rev 2018;6:e1. [Google Scholar] |
| 11. | Jolles BM, Bogoch ER. Posterior versus lateral surgical approach for total hip arthroplasty in adults with osteoarthritis. Cochrane Database Syst Rev 2006:CD003828. [Google Scholar] |
| 12. | Berstock JR, Blom AW, Beswick AD. A systematic review and meta-analysis of complications following the posterior and lateral surgical approaches to total hip arthroplasty. Ann R Coll Surg Engl 2015;97:11-6. [Google Scholar] |
| 13. | Rosenlund S, Broeng L, Overgaard S, Jensen C, Holsgaard-Larsen A. The efficacy of modified direct lateral versus posterior approach on gait function and hip muscle strength after primary total hip arthroplasty at 12 months follow-up. An explorative randomised controlled trial. Clin Biomech (Bristol, Avon) 2016;39:91-9. [Google Scholar] |
| 14. | Zeni J Jr., Madara K, Rubano J. The effect of surgical approach on strength and function after total hip arthroplasty. Del Med J 2016;88:334-40. [Google Scholar] |
| 15. | Pongcharoen B, Chaichubut K. Limping following primary total hip replacement: Comparison of 3 surgical approaches. JB JS Open Access 2019;4:e0043. [Google Scholar] |
| 16. | Kruse C, Rosenlund S, Broeng L, Overgaard S. Radiographic cup position following posterior and lateral approach to total hip arthroplasty. An explorative randomized controlled trial. PLoS One 2018;13:e0191401. [Google Scholar] |
| 17. | Winther SB, Husby VS, Foss OA, Wik TS, Svenningsen S, Engdal M, et al. Muscular strength after total hip arthroplasty. A prospective comparison of 3 surgical approaches. Acta Orthop 2016;87:22-8. [Google Scholar] |
| 18. | Hart A, Wyles CC, Abdel MP, Perry KI, Pagnano MW, Taunton MJ. Thirty-day major and minor complications following total hip arthroplasty – A comparison of the direct anterior, lateral, and posterior approaches. J Arthroplasty 2019;34:2681-5. [Google Scholar] |
| 19. | Gharanizade K, Karimi Heris H, Abolghasemian M, Joudi S, Hassany Shariat Panahy P, Yoosefzadeh A. A comparative evaluation of primary total hip arthroplasty via lateral and posterolateral approaches. Shafa Orthop J 2016;3:e3901. [Google Scholar] |
| 20. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann Intern Med 2009;151:W65-94. [Google Scholar] |
| 21. | Compston A. Aids to the investigation of peripheral nerve injuries. Medical Research Council: Nerve Injuries Research Committee. His Majesty's Stationery Office: 1942; pp. 48 (iii) and 74 figures and 7 diagrams; with aids to the examination of the peripheral nervous system. By Michael O'Brien for the Guarantors of Brain. Saunders Elsevier: 2010; pp.[8] 64 and 94 Figures. Brain 2010;133:2838-44. [Google Scholar] |
| 22. | Benson K, Hartz AJ. A comparison of observational studies and randomized, controlled trials. N Engl J Med 2000;342:1878-86. [Google Scholar] |
| 23. | Concato J, Shah N, Horwitz RI. Randomized, controlled trials, observational studies, and the hierarchy of research designs. N Engl J Med 2000;342:1887-92. [Google Scholar] |
| 24. | Anglemyer A, Horvath HT, Bero L. Healthcare outcomes assessed with observational study designs compared with those assessed in randomized trials. Cochrane Database Syst Rev 2014:MR000034. [Google Scholar] |
| 25. | Abraham NS, Byrne CJ, Young JM, Solomon MJ. Meta-analysis of well-designed nonrandomized comparative studies of surgical procedures is as good as randomized controlled trials. J Clin Epidemiol 2010;63:238-45. [Google Scholar] |
| 26. | Arditi C, Burnand B, Peytremann-Bridevaux I. Adding non-randomised studies to a Cochrane review brings complementary information for healthcare stakeholders: An augmented systematic review and meta-analysis. BMC Health Serv Res 2016;16:598. [Google Scholar] |
| 27. | Frieden TR. Evidence for health decision making-beyond randomized, controlled trials. N Engl J Med 2017;377:465-75. [Google Scholar] |
| 28. | Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg Br 1982;64:17-9. [Google Scholar] |
| 29. | Mulliken BD, Rorabeck CH, Bourne RB, Nayak N. A modified direct lateral approach in total hip arthroplasty: A comprehensive review. J Arthroplasty 1998;13:737-47. [Google Scholar] |
| 30. | Frndak PA, Mallory TH, Lombardi AV Jr. Translateral surgical approach to the hip. The abductor muscle “split”. Clin Orthop Relat Res 1993:135-41. [Google Scholar] |
| 31. | Von Langenbeck B. Ueber die Schussverletzungen des Huftgelenks. Archi Klin Chir, German 1874;16:263-339. [Google Scholar] |
| 32. | Gibson A. Vitallium-cup arthroplasty of the hip joint: Review of approximately one hundred cases. J Bone Joint Surg Am. 1949;31:861-72. [Google Scholar] |
| 33. | Moore AT. The self-locking metal hip prosthesis. J Bone Joint Surg Am 1957;39-A: 811-27. [Google Scholar] |
| 34. | Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. [Google Scholar] |
| 35. | Wells G, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta Analyses; 2013. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. [Last accessed 2021 Apr 22]. [Google Scholar] |
| 36. | Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34. [Google Scholar] |
| 37. | Ji HM, Kim KC, Lee YK, Ha YC, Koo KH. Dislocation after total hip arthroplasty: A randomized clinical trial of a posterior approach and a modified lateral approach. J Arthroplasty 2012;27:378-85. [Google Scholar] |
| 38. | Barber TC, Roger DJ, Goodman SB, Schurman DJ. Early outcome of total hip arthroplasty using the direct lateral vs the posterior surgical approach. Orthopedics 1996;19:873-5. [Google Scholar] |
| 39. | Downing ND, Clark DI, Hutchinson JW, Colclough K, Howard PW. Hip abductor strength following total hip arthroplasty: A prospective comparison of the posterior and lateral approach in 100 patients. Acta Orthop Scand 2001;72:215-20. [Google Scholar] |
| 40. | Kiyama T, Naito M, Shinoda T, Maeyama A. Hip abductor strengths after total hip arthroplasty via the lateral and posterolateral approaches. J Arthroplasty 2010;25:76-80. [Google Scholar] |
| 41. | Weale AE, Newman P, Ferguson IT, Bannister GC. Nerve injury after posterior and direct lateral approaches for hip replacement. A clinical and electrophysiological study. J Bone Joint Surg Br 1996;78:899-902. [Google Scholar] |
| 42. | Witzleb WC, Stephan L, Krummenauer F, Neuke A, Günther KP. Short-term outcome after posterior versus lateral surgical approach for total hip arthroplasty-A randomized clinical trial. Eur J Med Res 2009;14:256-63. [Google Scholar] |
| 43. | Rosenlund S, Broeng L, Holsgaard-Larsen A, Jensen C, Overgaard S. Patient-reported outcome after total hip arthroplasty: Comparison between lateral and posterior approach. Acta Orthop 2017;88:239-47. [Google Scholar] |
| 44. | Goosen JH, Kollen BJ, Castelein RM, Kuipers BM, Verheyen CC. Minimally invasive versus classic procedures in total hip arthroplasty: A double-blind randomized controlled trial. Clin Orthop Relat Res 2011;469:200-8. [Google Scholar] |
| 45. | Winther SB, Foss OA, Husby OS, Wik TS, Klaksvik J, Husby VS. Muscular strength and function after total hip arthroplasty performed with three different surgical approaches: One-year follow-up study. Hip Int 2019;29:405-11. [Google Scholar] |
| 46. | Aggarwal VK, Elbuluk A, Dundon J, Herrero C, Hernandez C, Vigdorchik JM, et al. Surgical approach significantly affects the complication rates associated with total hip arthroplasty. Bone Joint J 2019;101-B: 646-51. [Google Scholar] |
| 47. | Zhang J, Wyatt MC, Frampton CM, Anderson G. Does surgical approach affect early outcomes following primary total hip replacement in obese patients? Hip Int 2019. Epub 2019 Oct 13. [Google Scholar] |
| 48. | Baker AS, Bitounis VC. Abductor function after total hip replacement. An electromyographic and clinical review. J Bone Joint Surg Br 1989;71:47-50. [Google Scholar] |
| 49. | Bohatyrewicz A, Pawlowski Z, Ferenc M. O1332 Hip abductor strength following total hip arthroplasty: A prospective comparison of the posterolateral and anterolateral approach in 80 patients. Orthopaedic Proceedings. 2004;86-B:SUPP_III, 259-259. [Google Scholar] |
| 50. | Gore DR, Murray MP, Sepic SB, Gardner GM. Anterolateral compared to posterior approach in total hip arthroplasty: Differences in component positioning, hip strength, and hip motion. Clin Orthop Relat Res 1982:180-7. [Google Scholar] |
| 51. | Araújo P, Machado L, Cadavez D, Mónaco L, Januário F, Luís L, et al. Evaluation of the function and quality of life after total hip arthroplasty by different approaches. Acta Med Port 2017;30:623-7. [Google Scholar] |
| 52. | Demos HA, Rorabeck CH, Bourne RB, MacDonald SJ, McCalden RW. Instability in primary total hip arthroplasty with the direct lateral approach. Clin Orthop Relat Res 2001:168-80. [Google Scholar] |
| 53. | Johnston RC, Fitzgerald RH Jr., Harris WH, Poss R, Muller ME, Sledge CB. Clinical and radiographic evaluation of total hip replacement. A standard system of terminology for reporting results. J Bone Joint Surg Am. 1990;72:161-8. [Google Scholar] |
| 54. | Ploumis A, Tapsis K, Papageorgiou I, Terzidis I, Pouliopoulos D, Christodoulou A. Comparative study between posterior and lateral approach of total hip arthroplasty in patients with osteoarthritis. Orthopaedic Proceedings. 2003;85-B:SUPP_III, 225-6. [Google Scholar] |
| 55. | Antoniou J, Gomes SK, Zukor D, Huk O, Bergeron S, Robbins SM. Elevated and prolonged gluteus medius activation prevents trendelenburg gait following lateral approach total hip arthroplasty Orthopaedic Proceedings. 2019;101-B:SUPP_12, 30-30. [Google Scholar] |
| 56. | Xu Y, Duanmu QL, Yang M, Lin H, He J, He J, et al. Case-control study on effect of anterolateral and posterolateral approaches on early postoperative hip abductor strength in total hip arthroplasty. Zhongguo Gu Shang 2016;29:114-8. [Google Scholar] |
| 57. | Judd DL, Dennis DA, Thomas AC, Wolfe P, Dayton MR, Stevens-Lapsley JE. Muscle strength and functional recovery during the first year after THA. Clin Orthop Relat Res 2014;472:654-64. [Google Scholar] |
| 58. | Rasch A, Dalén N, Berg HE. Muscle strength, gait, and balance in 20 patients with hip osteoarthritis followed for 2 years after THA. Acta Orthop 2010;81:183-8. [Google Scholar] |
| 59. | Madsen MS, Ritter MA, Morris HH, Meding JB, Berend ME, Faris PM, et al. The effect of total hip arthroplasty surgical approach on gait. J Orthop Res 2004;22:44-50. [Google Scholar] |
| 60. | Cantrell WA, Samuel LT, Sultan AA, Acuña AJ, Kamath AF. Operative times have remained stable for total hip arthroplasty for >15 years: Systematic review of 630,675 procedures. JB JS Open Access 2019;4:e0047. [Google Scholar] |
| 61. | Mjaaland KE, Svenningsen S, Fenstad AM, Havelin LI, Furnes O, Nordsletten L. Implant survival after minimally invasive anterior or anterolateral vs. conventional posterior or direct lateral approach: An Analysis of 21,860 total hip arthroplasties from the norwegian arthroplasty register (2008 to 2013). J Bone Joint Surg Am 2017;99:840-7. [Google Scholar] |
| 62. | Buğlak F, Aksekili MA, Kiliçarslan K, Anaforoğlu B, Korkmaz I. A comparison of anterolateral and posterolateral approaches in primary total hip arthroplasty. Med J Islam World Acad Sci 2017;25:1-5. [Google Scholar] |
| 63. | Macedo CA, Galia CR, Rosito R, Valin MR, Kruel AV, Muller L, et al. Comparation of the antero-lateral and posterior approaches in primary total hip arthroplasty. Rev Fac Cien Med Univ Nac Cordoba 1999;56:91-6. [Google Scholar] |
Fulltext Views
3,788
PDF downloads
578





