Translate this page into:
Posterior slope of the tibial plateau in cohort of Omani patients undergoing total knee arthroplasty
*Corresponding author: Ahmed K. Al Ghaithi, Department of Surgery, Division of Orthopedic, Sultan Qaboos University, Muscat, Oman. a.alghaithi@squ.edu.om
-
Received: ,
Accepted: ,
How to cite this article: Al Badwi SA, Al Kindi NS, AlZeedi MH, Al Ghaithi AK, Luthra JS. Posterior slope of the tibial plateau in cohort of Omani patients undergoing total knee arthroplasty. J Musculoskelet Surg Res, 2023;7:176-9.
Abstract
Objectives:
Posterior tibial slope (PTS) is an important factor in restoring joint biomechanics after total knee arthroplasty (TKA). Given ethnic variation and the lack of recorded values for PTS, this study aimed to report PTS in a cohort of Omani patients (Arab ethnicity).
Methods:
This retrospective study included all Omani patients who underwent TKA in a specialized center between May 2017 and March 2020. Patients with revision TKA, extra-articular deformity, and tibial defects necessitating bony build-up and traumatic indications were excluded. Data collected include age, gender, and pre-and post-operative PTS.
Results:
A total of 128 patients were included in the study, 94 (73.4%) were female and 34 (26.6%) were male. The mean age of the patients was 65.16 years, standard deviation (SD) 8.47 (Maximum 87–Minimum 43). The mean pre-operative PTS was 10.6° (SD 3.65), whereas most current TKA designs aim for a 5–6° posterior slope. We found no correlation between PTS value and age or gender (P > 0.05).
Conclusion:
Given the higher PTS angle found in this study, which is consistent with those reported in the literature for Asian and Arab populations. This study indicates the importance of examining PTS variation within the population served. The proximal tibia shape and cutting angle can be varied to avoid any discrepancy in PTS after implantation.
Keywords
Arthroplasty
Knee
Posterior tibial slope
Tibia
Total knee arthroplasty
INTRODUCTION
Total knee arthroplasty (TKA) aims to restore the anatomy of the knee joint to its normal status. Therefore, restoring the angles and axes around the joint in this type of surgery is crucial.[1] One of the angles is the posterior tibial slope (PTS), which plays a major role in joint biomechanics. PTS was measured preoperatively by the angle between a line perpendicular to the tibia anatomical axis and a line joining tibial plateau proximal points [Figure 1]. Some considered it a key factor in the success of knee reconstruction, preserving the normal axis of the lower limb and increasing the longevity of the implant.[2]

- Posterior tibial slope angle, which was measured preoperatively by the angle between a line perpendicular to the tibia anatomical axis and a line joining tibial plateau proximal points.
While it is essential to achieve appropriate axial and rotational alignment in TKA, there is no consensus on the ideal PTS. Most current designs aim for a posterior slope of 3–7°. However, studies have shown a wide variation in pre-operative PTS between ethnicities and genders.[3,4] For instance, while a reported mean PTS from the Italian population was 8.6°, a subgroup analysis showed variation between ethnic groups with high values in the black race.[5] Moreover, reports from Indian populations showed higher values of 14.1°.[6]
Given this variation and the paucity of documented PTS angle values among Arabs groups, the main objective of this study was to measure the pre-operative PTS in a cohort of Omani patients undergoing TKA.
MATERIALS AND METHODS
This paper presents a retrospective cross-sectional study of 128 patients who underwent TKA in a specialized center between May 2017 and March 2020. A single surgeon operated on the patients using TKA systems (NexGen LPS, Zimmer Biomet® – Warsaw, IN, USA, PFC Sigma®, Warsaw, IN, USA). We included all Omani patients (Arab ethnicity) with a degenerative joint disease who have undergone primary TKA, which provided that they have full weight-bearing pre-and post-procedure radiographs with lateral and anteroposterior views. We excluded patients with revision TKA, extra-articular deformity, tibial defects requiring bony build-up, and traumatic indications.
Only true lateral pre-operative and post-operative radiographs were accepted. The superimposition of both femoral condyles confirms the true lateral radiograph, and there is a slight superimposition of the fibular head with the tibia.[7] An electronic picture archiving and communication system was used to retrieve the radiographs. PTS was measured preoperatively by the angle between a line perpendicular to the tibia anatomical axis and a line joining tibial plateau proximal points.[8] The tibial anatomical axis is defined as a line bisecting the midpoint of cortical diameter at 5 and 10 cm distal to the joint.[9] Post-operative PTS was measured as a line perpendicular to the anatomical axis of the tibia and a line along the cut area of the tibia connecting the two proximal points.[6] The operating surgeon decided the planned slope, “keeping in mind the native slope,” is within a range from 0° to 7°. Data collected include surgery date, age, gender, and pre-and post-operative PTS. Data were analyzed using IBM Statistical Package for the Social Sciences (SPSS, IBM Armonk, NY, statistics version 26.0), categorical variables were presented with frequency and percentage, and continuous age information was presented with mean and standard deviation (SD). The outcome variable PTS was tested for normality using the Kolmogorov-grove–Smirnov test, and data met the approximately normal distribution. Preand post-measurements of PTS were compared using paired t-tests. The influence of age and gender on PTS was tested using paired sample t-tests. P < 0.05 was considered, as statistical significance.
RESULTS
Of the 128 patients included in the study, 94 (73.4%) were female and 34 (26.6%) were male. The mean age of the patients was 65.16 years, SD 8.47 (Maximum 87–Minimum 43). Among the studied patients, the mean pre-operative PTS was 10.6°, SD 3.7, [Figure 2]. The mean pre-operative PTS for women was 10.5°, SD 3.8 and for men, 10.68°, SD 3.4. The mean post-operative PTS for women was 6.2°, SD 2.6 and for men, 5.1°, SD 2.8. Age and gender did not influence the PTS value (P > 0.05).
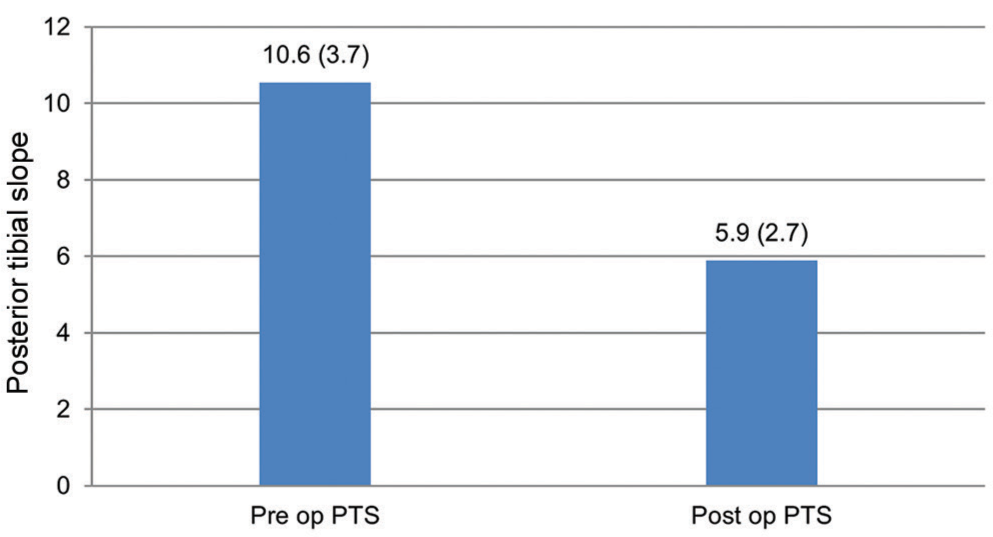
- The mean of pre-operative and post-operative posterior tibial slope measurements (standard deviation).
The precision of the mechanical jig used for getting the posterior tibial cuts was examined. On analyzing post-surgery radiographs, the mean of post-operative PTS was 5.89°, SD 2.71. The difference between the pre-and post-PTS of 4.66° showed statistical significance with P < 0.001.
Our study did not aim to compare the post-operative PTS between the two TKR designs using NexGen®/PFC sigma®. We found that extramedullary jigs used in the studied patients could maintain the desired post-operative PTS. The post-operative PTS mean was 5.89°, SD 2.7, which is within the required values (3–7°).[10]
DISCUSSION
Normal values for PTS across different populations have yet to be established. Although published reports until now show variability between various ethnic groups. In general, Asian populations have a relatively larger PTS (>10°) than Western literature.[5,11,12] Our study showed the pre-operative PTS to be 10.6°, which is in accordance with the reported angle by Yoo et al. in a Japanese population of 10.6° and Yoga et al. in a Malaysian group of 10.1°.[9,13] Moreover, the report of Saudi, Pakistani, and Indian populations showed higher values of 13.6°, 11.6°, and 14.1°, respectively [Table 1].[6,14,15] This could be attributed to the differences in cultural and lifestyle activities among these populations. Asian populations, and Arabs in particular, spend a long time of their day kneeling and cross-legged for social and spiritual activities.[16]
| Study author | Year | Population | Pre-op Posterior tibial slope |
|---|---|---|---|
| Bisicchia et al. | 2017 | Italian | 8.6 |
| Yoga et al. | 2009 | Malaysian | 10.1 |
| Mohanty et al. | 2013 | Indian | 11.6 |
| Khattak et al. | 2010 | Pakistani | 14.1 in females 12.5 in males |
| Yoo et al. | 2008 | Japanese | 10.6 |
| Chiu et al. | 2000 | Chinese | 11.5 |
| Aljuhani et al. | 2020 | Saudi | 13.6 |
| Current study | 2023 | Omani | 10.6 |
It is reported that an increase in post-operative PTS can result in biomechanical advantage by improving flexion tightness, where flexion improves by 1.7° for every 1° extra-PTS.[17] However, despite the proposed biomechanical advantages of increasing PTS, the variability between different ethnic groups should be considered, as anthropometric variability influences tibial plateau morphology. Mohamed et al. showed ethnic differences of proximal tibial plateau by studying 1000 normal adult knees (Caucasian, African American, and East Asian) using a knee three-dimensional morphology model.
The Caucasian population showed a larger morphological difference from the African American and East Asian with higher PTS among Asian populations.[18] This is why it is important to quantify morphological tibia variation across populations, which can improve deformity correction with implant design, soft-tissue balancing, or bone defect augmentation to resort to original sagittal alignment.
Furthermore, despite the suggested biomechanical advantages of increasing PTS, higher PTS rates may increase the range of motion and increase the potential for loosening around the implant. Thus, more research is needed on these complication rates among populations with a higher PTS compared to other population groups. A lower PTS may further demonstrate the importance of maintaining the slope at a certain level after TKA. This has not yet been investigated, as no studies have been found to make such a comparison.
There are a few limitations that were faced in this study that should be highlighted. First, our sample size was 128 patients after excluding a significant number of radiographs, which were not true lateral radiographs. Using a more advanced imaging, modality like a computed tomography scan or magnetic resonance imaging may improve the measurement accuracy of the PTS. Another limitation is that our study is a retrospective single-center study. Further multi-center research is needed to find kinematic relationships and PTS in Asian/Far Eastern/Middle Eastern patients.
CONCLUSION
Given the higher PTS angle found in this study, which is consistent with those reported in the literature for Asian and Arab populations. This study indicates the importance of examining PTS variation within the population served. The proximal tibia shape and cutting angle can be varied to avoid any discrepancy in PTS after implantation.
AUTHORS’ CONTRIBUTIONS
SAA and JL contributed to developing the project idea, helped interpret the results, and prepared and revised the manuscript. MA and NA contributed to idea development, data collection, preparation, and revising the manuscript. AA contributed to developing the idea and critically revising the manuscript. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
ETHICAL APPROVAL
The ethical approval was granted for this study by the Khoula Hospital’s Research and Ethical Review and Approve Committee, Muscat, Oman (RERAC number PRO012021076 1/2021).
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patients consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Effect of posterior tibial slope change on postoperative range of motion and clinical outcomes after posterior cruciate-substituting total knee arthroplasty. J Knee Surg. 2023;36:87-94.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32:376-82.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior slope of tibial plateau in Chinese. J Arthroplasty. 2000;15:224-7.
- [CrossRef] [PubMed] [Google Scholar]
- Measurement of posterior tibial slope using magnetic resonance imaging. Arch Bone Jt Surg. 2017;5:435-9.
- [Google Scholar]
- Do ethnicity and gender influence posterior tibial slope? J Orthop Traumatol. 2017;18:319-24.
- [CrossRef] [PubMed] [Google Scholar]
- Correlation of posterior tibial slope with metaphysio-diaphyseal angle in total knee arthroplasty: A radiological study. Indian J Orthop. 2013;47:67-71.
- [CrossRef] [PubMed] [Google Scholar]
- The lateral knee radiograph: A detailed review. J Knee Surg. 2022;35:482-90.
- [CrossRef] [PubMed] [Google Scholar]
- Optimization of the posterior condylar offset, tibial slope, and condylar roll-back in total knee arthroplasty. J Arthroplasty. 2006;21:889-96.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomical references to assess the posterior tibial slope in total knee arthroplasty: A comparison of 5 anatomical axes. J Arthroplasty. 2008;23:586-92.
- [CrossRef] [PubMed] [Google Scholar]
- How to interpret postoperative X-rays after total knee arthroplasty. Orthop Surg. 2014;6:179-86.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior tibial slope in the normal and varus knee. Am J Knee Surg. 1999;12:165-8.
- [Google Scholar]
- In vitro study of inter-individual variation in posterior slope in the knee joint. Clin Biomech (Bristol Avon). 2009;24:488-92.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior slope of the tibia plateau in Malaysian patients undergoing total knee replacement. Malays Orthop J. 2009;3:78-80.
- [CrossRef] [Google Scholar]
- Lower-limb alignment and posterior tibial slope in Pakistanis: A radiographic study. J Orthop Surg (Hong Kong). 2010;18:22-5.
- [CrossRef] [PubMed] [Google Scholar]
- Variability of the posterior tibial slope in Saudis: A radiographic study. Cureus. 2020;12:e10699.
- [CrossRef] [Google Scholar]
- Good clinical success rates are seen 5 years after meniscal repair in patients regularly undertaking extreme flexion. Arthrosc Sports Med Rehabil. 2021;3:e1835-42.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of tibial slope on maximal flexion after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2005;13:193-6.
- [CrossRef] [PubMed] [Google Scholar]
- Three-dimensional morphology of the knee reveals ethnic differences. Clin Orthop. 2012;470:172-85.
- [CrossRef] [PubMed] [Google Scholar]






