Translate this page into:
Prevalence of burnout of residents in oman medical specialty board: A cross-sectional study in Oman
2 Department of Orthopedic Surgery, Armed Forces Hospital, Muscat, Oman
3 Orthopedic Surgery Program, Oman Medical Specialty Board, Muscat, Oman
4 Radiology Program, Oman Medical Specialty Board, Muscat, Oman
Corresponding Author:
Ahmed S Al Jahwari
Department of Orthopedic Surgery, Armed Forces Hospital
Oman
Ahmedaljahwari111@gmail.com
| How to cite this article: Al Subhi AA, Al Lawati HA, Shafiq MO, Al Kindi SS, Al Subhi MA, Al Jahwari AS. Prevalence of burnout of residents in oman medical specialty board: A cross-sectional study in Oman. J Musculoskelet Surg Res 2020;4:136-140 |
Abstract
Objective: Burnout is a state of physical and emotional exhaustion and a sense of low personal accomplishment. Our aim was to study the prevalence of burnout among all residents of Oman Medical Specialty Board (OMSB), to increase awareness of burnout among trainers and trainees not only within Oman but also in other countries with similar residency programs. This would help residency directors to increase the performance of their residents. Methods: This is a cross-sectional study with residents of OMSB involved in 17 training programs from April 2018 to April 2019. The residents were invited to answer a validated burnout questionnaire (Maslach Burnout Inventory). Only exclusion criteria were programs with at least three residents. Results: A total of 343 of 555 residents (61.8% of the total OMSB residents) participated in the study. The response rate was 100% of those who got the survey. The overall burnout rate was 16.6%. From postgraduate years (PGY) 1–5, there was a sudden spike of burnout at PGY 2 and PGY 5 at 17.6% and 25%, respectively. Emergency residents had the highest incidence of burnout at 46.2%. Burnouts among surgical, medical, and diagnostic specialties were 13.9%, 19.0%, and 12.8%, respectively. Chi-squared test showed no significant association between burnout and marital status, gender, or number of children at 0.18, 0.88, and 0.55, respectively. The percentage of residents who reported emotional exhaustion was 61.2%, while the highest percentage of depersonalization was 42.6%. Conclusion: Emergency medicine program burnout is alarming. PGY 2 and 5 show higher burnout. The overall burnout in OMSB is low.
Introduction
Burnout is a state of physical and emotional exhaustion and a sense of low personal accomplishment that may have an impact on efficiency at work. It is characterized by depersonalization, fatigue, low self-esteem, and inability to perform at an efficient level.[1]
It is more apparent in professions that require intense involvements with people like physicians, nurses, social workers, and teachers. Residency training may produce a significant level of burnout, leading to interference in academic and clinical performance. The processual character of burnout refers to cumulative negative consequences of long-term work-related stress as a result of exhaustion. In clinical settings, evidence shows that burnout causes prescription errors and reduces the quality of medical services, potentially affecting the interprofessional relationships as well as patients' lives. Burnout contributes to poor job satisfaction and a negative impact on their mental and physical health.[2] In recent years, the risk of residents developing burnout has been further aggravated by increasing peer competition, clinical and administrative loads, medical litigation, and expectations of training.[3] However, this is often overlooked by clinical supervisors and hospital administration.
Various investigators have reported the prevalence of burnout among residents in different specialties worldwide. Lu et al. measured the burnout in emergency physicians, and their results showed a burnout rate of 57.1%, with no difference between attending and resident physicians.[4] Aldrees et al. reported a high prevalence of burnout among otolaryngology residents in Saudi Arabia, where year 3 residents were found to be affected the most. Their response rate was 60%, yet this study was only about one specialty.[5] Another report by them among residents of the Saudi plastic surgery residency program showed a low burnout rate of 18%.[6] Shafiq et al. explored in their cross-sectional study in the Gulf Cooperation Council (GCC) countries the journey from orthopedic residency to fellowship and the common barriers encountered. Burnout was one among the other barriers, such as lack of time and lack of ample exposure.[7] Alshammari et al. in another study investigated influences, barriers, and mental pressures of female orthopedic surgery residents and fellows and found that gender intolerance did exist, which might discourage female doctors from pursuing orthopedic surgery, although burnout due to this was not directly studied; the authors postulated that perhaps this could be one of the reasons.[8] Another study that was done in Saudi Arabia regarding burnout by Alsheikh et al. showed a high burnout of 56.3% among orthopedic residents.[9]
All the above studies hint toward the need for increased awareness of burnout among residents.
Residents must develop skills during their training to cope with multiple issues such as sleep deprivation, high workload, and other responsibilities of patient care while completing their in-training exams, research, and many other academic activities.
Our aim in this study was to find out the prevalence of burnout among all residents of Oman Medical Specialty Board (OMSB). No study to date has taken place in Oman inclusive of all programs, especially because OMSB is relatively new, having been established in 2006. The secondary aims were to find out if there is a difference in burnout among surgical, medical, and diagnostic specialties and whether marital status and having children affect burnout rates.
The importance of this study is to increase awareness among residents, practicing physicians, residency directors, and OMSB about burnout. This study will be resourceful to residency directors who can reflect at their resident group and identify the current residents requiring help and in future residents who can be advised on how to manage their residency training and avoid burnout.
Materials and Methods
A cross-sectional survey was done from April 2018 to April 2019 using a self-report Maslach Burnout Inventory (MBI) with the target population of all residents of OMSB. OMSB is the only body in Oman to train and accredit postgraduate doctors to become specialized in different medical specialties. Currently, 555 residents are in training in OMSB in 18 programs of different specialties. The sample size needed was calculated as 289 based on the following formula:
Sample size = (distribution of 50%)/([margin of error%/confidence level score] 2).
All residents undergoing training in OMSB were invited to answer the survey while using a random sampling technique. The questionnaires in papers were distributed among residents during their regular weekly academic activities. It was chosen to have paper-based questionnaires for various reasons. Electronic questionnaires are often ignored and not taken as seriously. Most of the reminders are kept in Junk in the mailbox. After obtaining the permission from respective program directors, authors attended the teaching session of each program where all residents were attending. Authors distributed the questionnaire, collected the completed ones, sealed in an envelope to maintain privacy and confidentiality.
The MBI is a validated instrument that has long been recognized as the leading measure of burnout. The survey measures three components of burnout, which are depersonalization, emotional exhaustion, and personal satisfaction. The survey consists of demographic variables and three sections. Section A represented emotional exhaustion and has 7 items. Section B represented depersonalization and has 8 items. Section C, which contains 8 items, represented personal satisfaction. The MBI takes approximately 5–10 min to complete.
The responses were measured on a 7-point Likert scale ranging from 0 to 6, with scores summed and categorized into published instrument standards of “low,” “moderate,” and “high” scores in each subscale category. High scores on emotional exhaustion (27 or over) or depersonalization (31 or over) or low scores on personal satisfaction (<31) indicate symptoms of burnout.
Certain questions in the questionnaire were set deliberately as a repeat to assess the correctness of the response. The difference in answers of those repeated questions was excluded. Data were entered into SPSS (IBM Corp., Armonk, NY, USA), and analysis was done. An excel sheet was utilized to create graphs and bar charts.
Inclusion/exclusion criteria were based on sending questionnaires to all programs with at least three residents, no upper limit was set, and no other condition was set. The biochemistry program was excluded as it had only one resident. The significance threshold was set at 0.05.
Results
A total of 343 of 555 residents (61.8% of the total OMSB residents) participated in the study. The response rate was 100% of those who got the survey.
The demographics of OMSB residents are shown in [Figure - 1], which shows that the majority of the responses were from females at 61.8%, and most of the residents were married (60.9%). The mean age was 29 (minimum age of 25 and a maximum age of 35) years. Chi-squared test showed no significant association between burnout and marital status, gender, or number of children at 0.179, 0.88, and 0.55, respectively.
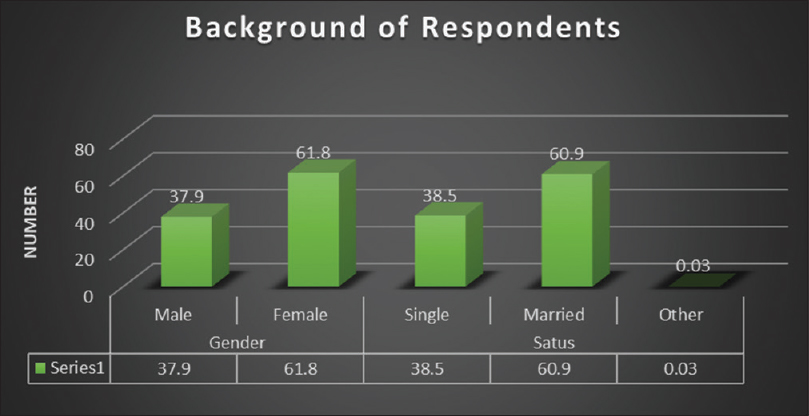 |
| Figure 1: Demographics of Oman Medical Specialty Board residents |
The highest number of residents in OMSB was from the internal medicine program (57) followed by family and community medicine (49), pediatrics (39), and obstetrics and gynecology (23), as shown in [Figure - 2]. There was no link seen between the number of residents in a program with their burnout score (P = 0.6).
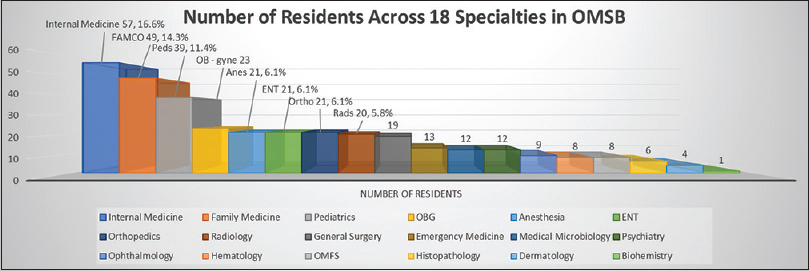 |
| Figure 2: Representation of numbers and percentages of the residents in different specialties in the Oman Medical Specialty Board |
The highest burnout was seen among emergency medicine residents (46.2%) followed by hematology residents (25%) and then internal medicine residents (24.6%), as shown in [Figure - 3]. The lowest burnout was seen with otolaryngology residents at 4.3% and no burnout was seen among the residents of maxillofacial surgery, histopathology, and dermatology residents.
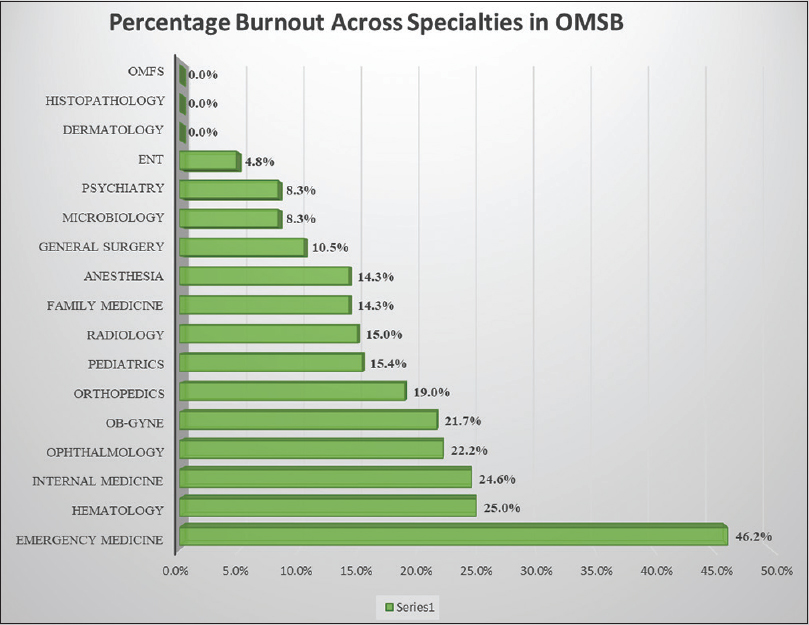 |
| Figure 3: Burnout among different specialties in the Oman Medical Specialty Board and the effect of each program in general burnout in the Oman Medical Specialty Board |
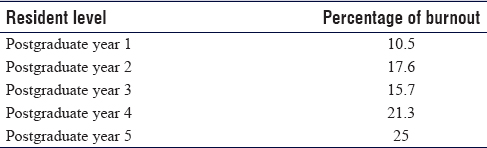
The burnout was then seen across the postgraduate year (PGY) from 1 to 5. It was seen that PGY 2 and 5 had the most burnout 17.5% and 25%, respectively, where the lowest was seen in PGY 1 at 10.5% [Table - 1].
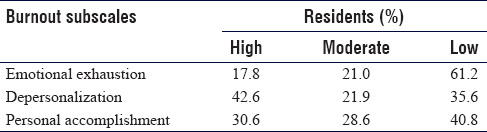
OMSB residents showed the lowest emotional exhaustion (low: 61.2%) and the highest depersonalization (high: 42.6%). Sense of accomplishment was also on the lower side (40.8%), as shown in [Table - 2] and [Figure - 4].
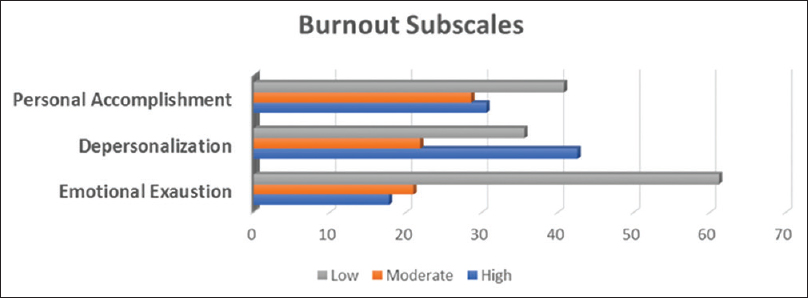 |
| Figure 4: The percentage of residents is 61.2% who report low emotional exhaustion. And, the highest percentage of depersonalization is seen at 42.6% |
Discussion
Our results have shown an overall 16% prevalence of burnout among OMSB residents. The prevalence of burnout in our institute compared to various European training institutes is significantly less when some European institutes researched on Dutch residents (the Netherlands, Aruba, Belgium, Curacao, Sint Maarten, and Suriname) reported rates of 49.5%.[10]
There are multiple reasons for this observation. Usually, physicians are last to admit if they have issues. Most physicians do not acknowledge their symptoms or admit that they can be affected by burnout and refuse to seek help, leading to a two-fold increased risk of suicidal ideation.[11],[12] Burnout among OMSB residents could be low due to culture. It is not accepted within Omanis to complain or find fault. Another reason could be that residents are afraid to speak out and voice their opinion as this could cost them their relationship with their program directors and seniors.
Low burnout rate could also be low due to workshops that are mandatory at every level of residency, which addresses topics on the resident as a teacher and awareness of burnout and fatigue and address well-being. The Wellness Center of OMSB also does separate workshops on IT and patient records management on tips and ease for residents to enter records smoothly. Certain workshops from the Wellness center are based on life management skills as well. These may not be mandatory, but many residents attend and benefit from them. Although some workshops are mandatory, an increase in workshops and lectures about burnout would help increase in the performance of the residents.
Other reasons could be job security as all the residents of OMSB are hired by the Directorate of General Health Services known as DGHS of their area or governorate under the umbrella of the Ministry of Health. In Oman, residents do not need to find jobs once they graduate as compared to other regions around the world.
Al-Alawi et al. recently reported the prevalence of burnout among medical students at Sultan Qaboos University, Muscat, and found it to be less than that of the residents (7.4%).[13] Comparing residents to undergraduate students, the more stress and responsibilities can explain this observation.
Dyrbye et al. measured the burnout among US medical students, residents, and early career physicians and found that 50% of residents have burnout.[14] It could be argued that job security plays a vital role in burnout.
[Figure - 3] shows the percentage of burnout; it clearly shows an alarming burnout rate among emergency physicians as their percentage of residents is 3.8%, and they have the highest burnout rate of 46.2%. This could be due to an increase in the load shared by emergency residents who are less in number in their program. There are programs with a high number of residents with moderate to a low number of burnouts such as internal medicine and family medicine. Although the burnout of emergency physician residents is still lower than the international literature, it is not explainable based on the other programs and their burnout rate.
The authors predict that this could be due to an individual response rate of 50% by emergency physicians. Further than this, not much information can be concluded as shift change, workload, and other details are applicable to other residents in other programs too. Further studies are needed to understand this phenomenon observed.
Subscales of burnout, namely, emotional exhaustion, depersonalization, and personal accomplishment, showed that 61.2% reported low emotional exhaustion. Moreover, the highest percentage of depersonalization is seen at 42.6%. A state in which one's thoughts and feelings seem unreal or not to belong to oneself. It could also be that residents did not understand the meaning of “Depersonalization” as the mother tongue of Oman is Arabic, and the questionnaire was not translated into Arabic. This could also be a contributing factor toward the higher results of depersonalization.
There was no statistically significant difference in burnout among surgical, medical, and diagnostic specialties, which were 13.9%, 19%, and 12.8%, respectively (P > 0.05). This could be explained by multiple reasons. The population studied is homogenous. All the residents, as explained before, are of the same background. All are one nationality. Hence, the culture, habits, and coping skills must be, to some extent, similar. The same set of hospitals is utilized by medical students and residents; hence, familiarity is higher when students move up the ladder of residency. The staff in each department is known and duty hours are managed accordingly.
Burnout was increasing with the seniority of the residents, as shown in [Table - 1]. Williams et al. reported no difference between burnout levels among junior and senior residents.[15]
Our study showed that among junior residents, PGY 2 had more burnout than PGY 3. This could be explained by the board part 1 exam at the end of PGY 2, which is a qualifying exam. If failed, residents are not allowed to move to the senior residency post.
Our study showed that year 4 and year 5 had much more burnout than year 1–3 combined. This could be explained by the increasing responsibilities of the senior residents. Senior residents continue to take calls till last year while sitting for the board exam, part 2 in their final year. Approaching the Part 2 examination as a PGY5 while managing family and working hours can cause an increase in burnout. These residents not only need to do the above, but they also need to give international exams to secure fellowships.[7] This contrasted to other residency centers in the West, which is very different as the structure is that after a 5-year residency, they are transferred to fellowships based on their own board scores and recommendation letters. They do not have to sit for separate international exams.
There are a few limitations to our study. Although 61.8% of the residents in OMSB were involved in this study, some programs participated with <50% of their residents, such as the emergency medicine program.
Conclusion
There was a concern regarding burnout among emergency medicine specialty, which requires to be addressed. PGY 2 and 5 showed a higher burnout among other residents. The overall burnout in OMSB is low compared to that of the literature.
Recommendation
Together with the mandatory workshops, it is our recommendation to increase workshops and lectures about burnout and fatigue and time management, which would increase awareness among trainees and trainers, ultimately increasing the performance of residents.
Moreover, a mentor–mentee program would also benefit the resident and give the mentor an idea about the academic burnout and other professional issues of the resident.
More attention should be given to PGY 2 and PGY 5 residents who have board exams by perhaps scheduling lighter rotations around the exam time.
We recommend starting local or across GCC fellowship programs, which would lessen the burden on PGY 5 residents in securing a spot in the other countries.
Residency directors of surgical specialties should be more aware of their residents that are prone to burnout. The emergency medicine program needs to re-evaluate reasons for the higher burnout with individual attention to each resident.
Multiple studies are required further to associate working hours with burnout among OMSB residents. Further studies after a period of 5 years on the burnout of graduates of OMSB would be an interesting comparison with our current research and burnout rate. This could lead to residency directors and decision makers to help residents further.
The results of these studies should be anticipated not only to benefit Oman and OMSB, but also to find application in similar residency systems.
Ethical consideration
The approval of the study was done by Oman Medical Specialty Board on 08\02\2018, no. 2018/2/1/1582.
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Authors' contribution
AAAS, HAAL, and ASAJ conceived the concept and designed the study and provided research direction. AAAS, ASAJ, AL, MOS, SSAK, and MOS formed the research questions; did literature search and research proposal; and collected data. AAAS, ASAJ, and MAAS analyzed the data. All authors were involved in writing the manuscript, have critically reviewed, and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Blache J, Borza A, De Angelis K, Frankus E, Gabbianelli G, Korunka C, et al. Burnout intervention training for managers and team leaders: a practice report. Wien: Die Berater. 2011. [Google Scholar] |
| 2. | Golonka K, Mojsa-Kaja J, Gawlowska M, Popiel K. Cognitive Impairments in occupational Burnout-Error processing and its indices of reactive and proactive control. Front Psychol 2017;8:676. [Google Scholar] |
| 3. | Kang EK, Lihm HS, Kong EH. Association of intern and resident burnout with self-reported medical errors. Korean J Fam Med 2013;34:36-42. [Google Scholar] |
| 4. | Lu DW, Dresden S, McCloskey C, Branzetti J, Gisondi MA. Impact of burnout on self-reported patient care among emergency physicians. West J Emerg Med 2015;16:996-1001. [Google Scholar] |
| 5. | Aldrees T, Badri M, Islam T, Alqahtani K. Burnout among otolaryngology residents in Saudi Arabia: A multicenter study. J Surg Educ 2015;72:844-8. [Google Scholar] |
| 6. | Aldrees T, Hassouneh B, Alabdulkarim A, Asad L, Alqaryan S, Aljohani E, et al. Burnout among plastic surgery residents. National survey in Saudi Arabia. Saudi Med J 2017;38:832-6. [Google Scholar] |
| 7. | Shafiq MO, Khaja AF, Alshammari AN, Altayeb MA, Ghabban KM, Khoshhal KI. The journey of orthopaedic surgery from residency to fellowship: A cross-sectional study in the Gulf Cooperation Council countries. J Taibah Univ Med Sci 2019;14:131-8. [Google Scholar] |
| 8. | Alshammari AN, Shafiq MO, Altayeb MA, Khaja AF, Ghabban KM, Khoshhal KI. Gulf cooperation council female residents in orthopedics: Influences, barriers, and mental pressures: A cross sectional study. J Musculoskelet Surg Res 2018;2:51-6. [Google Scholar] |
| 9. | Alsheikh KA, Alhabradi FA, Almalik FF, Alsalim AA, Ahmed FE, Alhandi AA. Burnout syndrome among orthopedic surgery residents in Saudi Arabia: A multicenter study. J Musculoskelet Surg Res 2019;3:184-8. [Google Scholar] |
| 10. | Prins JT, Hoekstra-Weebers JE, van de Wiel HB, Gazendam-Donofrio SM, Sprangers F, Jaspers FC, et al. Burnout among Dutch medical residents. Int J Behav Med 2007;14:119-25. [Google Scholar] |
| 11. | Shanafelt TD, Balch CM, Dyrbye L, Bechamps G, Russell T, Satele D, et al. Special report: Suicidal ideation among American surgeons. Arch Surg 2011;146:54-62. [Google Scholar] |
| 12. | van der Heijden F, Dillingh G, Bakker A, Prins J. Suicidal thoughts among medical residents with burnout. Arch Suicide Res 2008;12:344-6. [Google Scholar] |
| 13. | Al-Alawi M, Al-Sinawi H, Al-Qubtan A, Al-Lawati J, Al-Habsi A, Al-Shuraiqi M, et al. Prevalence and determinants of burnout Syndrome and Depression among medical students at Sultan Qaboos University: A cross-sectional analytical study from Oman. Arch Environ Occup Health 2019;74:130-9. [Google Scholar] |
| 14. | Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med 2014;89:443-51. [Google Scholar] |
| 15. | Williams ES, Konrad TR, Scheckler WE, Pathman DE, Linzer M, McMurray JE, et al. Understanding physicians' intentions to withdraw from practice: The role of job satisfaction, job stress, mental and physical health. 2001. Health Care Manag Rev 2010;35:105-15. [Google Scholar] |
Fulltext Views
3,698
PDF downloads
1,292





