Translate this page into:
Primary subacute osteomyelitis of the talus in a child
2 Joint Program of Postgraduate Studies of Family Medicine, Jeddah, Saudi Arabia
3 College of Medicine, Taibah University, Almadinah Almunawwarah, Saudi Arabia
Corresponding Author:
Abdulmuhsen N Alshammari
Department of Orthopedics, King Fahad Hospital, P.O. Box: 3892, Almadinah Almunawwarah
Saudi Arabia
m_shamari@hotmail.com
| How to cite this article: Alshammari AN, Alotaibi MH, Abouelnaga MA, Almohammadi AM. Primary subacute osteomyelitis of the talus in a child. J Musculoskelet Surg Res 2018;2:34-37 |
Abstract
Primary subacute osteomyelitis of the talus is very rare in healthy children, and the diagnosis can be delayed or even missed, because of its uncommon presentation. Only a few cases of primary subacute osteomyelitis of the talus have been reported in the literature. In this article, we report a case of primary subacute osteomyelitis of the talus in a child and describe its symptoms, signs, radiographic appearance, and the outcome of the surgical management along with a short course of antibiotics coverage. We present this rare case report and its management to increase the awareness for the possibility of this pathology, and to avoid misdiagnosis.Introduction
Brodie's abscess falls under the category of subacute osteomyelitis. In early literature, Sir Benjamin Brodie (1832) referred to it as a localized bone abscess, which has no connection to any prior systemic illness.[1] Billroth (1881) subsequently labeled the condition as “subacute.”[2] Subacute osteomyelitis makes up 2.4% of osteomyelitis cases,[3] although in East Africa it is known to be the most common form.[4] Furthermore, boys are more commonly affected than girls, with a ratio of 3:2, respectively.[4],[5] It also tends to occur more often in younger patients averaging 19.5 years of age.[5] The tibia is the most common location that is affected, seldom involving the tarsal bones.[4],[5],[6]
The pathogenesis of subacute osteomyelitis is not well understood. Subacute osteomyelitis is characterized by minimal, or no symptoms and clinical signs at the initial presentation, which makes its diagnosis extremely difficult.[7],[8] The diagnosis is based on the clinical history, physical examination, and the radiological findings. The management of subacute osteomyelitis remains controversial, and the treatment ranges from curettage, biopsies, specimen cultures, the use of impregnated antibiotic beads, cancellous bone grafting after curettage followed by immobilization to the use of antibiotic therapy alone, without surgery. Nevertheless, successful outcomes have been reported with oral antibiotic therapy only.[7],[9] Hamdy et al. reported that out of the 44 patients in the treatment group, 24 patients were treated with antibiotic therapy only. Moreover, 20 had surgical debridement followed by antibiotic therapy. All patients had responded well, regardless of whether the treatment was surgical or nonsurgical.[10] In general, a total of 6 weeks with antibiotic therapy, administrated wholly, or partially by an intravenous route, was recommended.[11] The study by Olasinde et al. reported that the patients with subacute osteomyelitis responded well to surgical curettage of the abscesses, cancellous bone grafting, and antibiotic therapy.[3] There is controversy over the need for antibiotics after debridement in a culture negative lesion, as reported by some authors.[12],[13],[14] Early diagnosis and appropriate treatment of the condition is essential to avoid potential unnecessary morbidities. In this report, we present a child with primary subacute osteomyelitis of the talus and describe its symptoms, signs, radiographic appearance, and the outcome of the surgical management along with a short course of antibiotics coverage. We present this rare case report and its management to increase the awareness for the possibility of this pathology, and to avoid misdiagnosis.
Case Report
A 9-year-old boy presented with a 3-month history of intermittent pain and swelling of the left ankle. The pain was mainly in the anterior aspect of the ankle joint. One month after the onset of the pain, his parents noticed a change in his gait. There was no history of trauma or constitutional symptoms.
On examination, there was a mild swelling of the anterior aspect of the ankle with tenderness. There were no signs of acute inflammation; however, dorsiflexion of the ankle was limited and painful. Inflammatory markers including white blood count (WBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) were normal, and the blood cultures were negative.
Radiographs showed a subchondral lytic lesion in the talus [Figure - 1]. Magnetic resonance imaging (MRI) was used as a second-line investigation, and T1 postcontrast image demonstrated intense marginal enhancement of the lytic lesion, along with an enhancement of the bony edema and ankle joint effusion [Figure - 2].
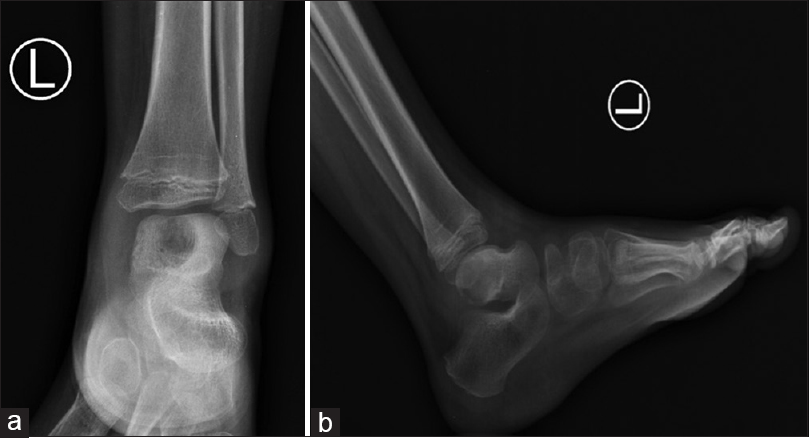 |
| Figure 1: (a) X-ray of the left ankle joint. Anteroposterior X-ray showing a central osteolytic lesion in the central part of the talus. It shows loss of bony trabeculation with surrounding reactive sclerosis. (b) Lateral x-ray showing focal osteopenia along the posterior part of the talus with resorption of the overlying cortex and associated surrounding soft-tissue swelling |
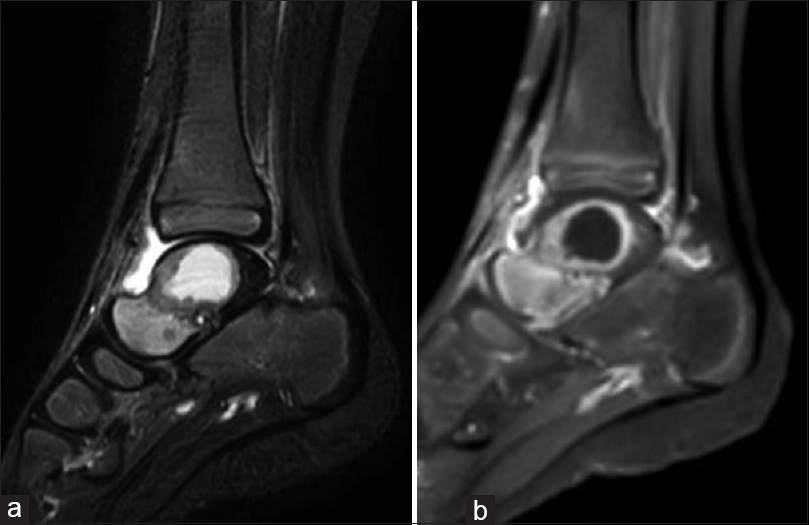 |
| Figure 2: (a) Magnetic resonance imaging of the ankle. Sagittal T2-weighted image with fat suppression showing central bony necrosis within the body of the talus appearing as a well-defined area of bright signal intensity with surrounding bony edema and ankle joint effusion. (b) T1 postcontrast image showing intense marginal enhancement of the abscess cavity along with enhancement denoting bony edema and surrounding soft tissue around the ankle joint. There is intense synovial thickening and enhancement along the anterior ankle joint |
Concern was taken over the possible collapse. Thus, surgical exploration of the lesion was prompted through an anteromedial approach of the ankle. During the surgical exploration of the talus, thick dark-colored fluid was drained from the cavity. The lesion was curetted, and the cavity was packed with cancellous bone allograft [Figure - 3]. Postoperatively, intravenous first-generation cephalosporin was administered.
 |
| Figure 3: Postoperative x-ray showing the cavity filled with bone graft |
A pus swab and curetted bone were sent for bacterial culture and sensitivity; it yielded no positive results. A piece of the synovial membrane and curetted bone were sent for histopathological examination and acid-fast bacilli (AFB) stain; the histopathology report revealed a non-caseating granulomatous inflammation, and AFB stain was negative. Postoperatively, the CRP test was within normal limits.
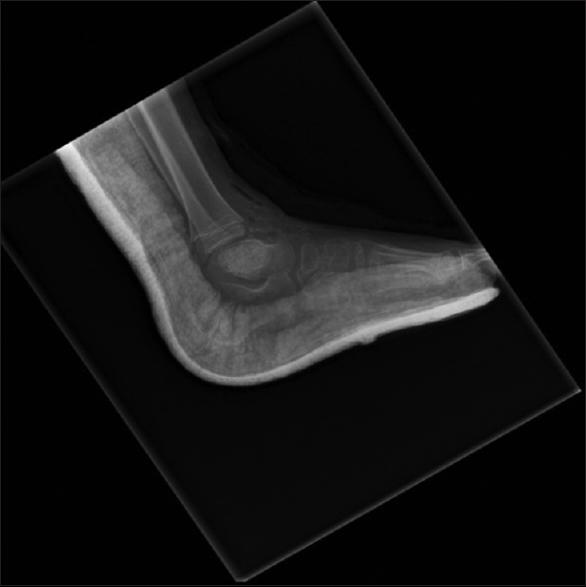
On the third postoperative day, based on the clinical assessment, the negative result from bacterial cultures, and a normal CRP value, the intravenous antibiotic was discontinued, and the child was discharged home on oral analgesics. The ankle was immobilized in a below-knee back slab for 8 weeks then the patient was allowed to weight bear as tolerated. At 10 weeks after surgery, the patient was doing well, with no wound discharge, tenderness, or swelling. The ankle and subtalar joint movements were normal and pain-free. At 3 months after surgery, he had no complaints, he could walk without pain, and the radiographs showed that the bone graft was well incorporated. At 4 months, he was asymptomatic, and he had returned to full activity level. At the 7-month follow-up examination, the patient was asymptomatic, and there was no evidence of local recurrence [Figure - 4] and [Figure - 5].
 |
| Figure 4: (a) Clinical picture showing ankle range of motion at 7-month follow-up. Active ankle dorsiflexion. (b) Active ankle plantar flexion |
 |
| Figure 5: Seven-month postoperative radiograph |
A written informed consent was obtained from the patient's father for publication of this case report alongside the accompanying images.
Discussion
The accurate diagnosis of subacute osteomyelitis of the talus bone might face undesirable delays. The reason behind this is due to its uncommon location, as well as its relatively rare presentation, as demonstrated in our case. Subacute osteomyelitis of the talus bone is rare in children, and extremely rare in adults.[7] Roberts et al., in a review of 55 patients with osteomyelitis described primary subacute osteomyelitis in only 18 patients, none of whom had any involvement of the foot.[15] In the 212 cases of acute osteomyelitis reported by White and Denison, only five cases of this disease affecting tarsal bones were documented.[16] The disease has a sudden onset and mild signs and symptoms with no systemic reaction. This, in turn, renders it difficult to diagnose, sequentially causing a potential delay in delivering proper treatment, as we faced in our case. The MRI findings; a lytic cavity with sclerotic margins are typical radiological characteristics of the disease. However, they are not specific and may be suggestive of benign or malignant neoplasms.[17] It also excluded other key differentials such as chondroblastoma, aneurysmal bone cyst, osteoidosteoma, intraosseous bone cyst, and lipoma. Laboratory tests, such as the WBC, ESR, CRP, and blood cultures, are not useful in many cases, as no specific laboratory tests are available for the subacute osteomyelitis.[18] For instance, in our case, laboratory data did not support the diagnosis of infection, and all the cultures were negative. Furthermore, no evidence of a benign tumor or tuberculosis was indicated in the histopathology findings. The management of subacute osteomyelitis in children remains controversial.[3] In our case, however, the decision of surgical management in the form of curettage and bone grafting was indicated based on the size of the lesion, which involved almost all of the body of the talus. The risk of fracture and collapse in a weight-bearing bone was reduced, and the outcomes in 7 months of follow-up both clinically and radiologically were satisfactory.
Conclusion
The surgical treatment of a large osteolytic lesion is crucial for weight-bearing bones, and it is achieved by surgical curettage, cancellous bone grafting, and the coverage with a short course of antibiotics would all, in combination, lead to satisfactory outcomes. We recommend this management, but further testing is required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Acknowledgment
The authors would like to thank Dr. Ali AlSaadi, Pediatric Radiology Consultant, for his assistance with the radiographs and MRI interpretation of this case. In addition, we would like to thank the reviewers for their detailed comments and suggestions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
MAA and ANA conceived and designed the study. MHA and AMA collected and organized data while ANA and MHA wrote initial and final draft of the article and provided critical input. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Brodie BC. An account of some cases of chronic abscess of the tibia. Med Chir Trans 1832;17:239-49. [Google Scholar] |
| 2. | Abulfotooh M. Osteomyelitis: Historical review. Pan Arab J Orthop Trauma 2003;7:95-109. [Google Scholar] |
| 3. | Olasinde AA, Oluwadiya KS, Adegbehingbe OO. Treatment of brodie's abscess: Excellent results from curettage, bone grafting and antibiotics. Singapore Med J 2011;52:436-9. [Google Scholar] |
| 4. | Khoshhal K, Letts M. Subacute Osteomyelitis (Brodie Abscess): Background, Anatomy, Pathophysiology; 2017. Available from: http://www.emedicine.medscape.com/article/1248682-overview#a7. [Last accessed on 2017 Nov 13]. [Google Scholar] |
| 5. | Lopes TD, Reinus WR, Wilson AJ. Quantitative analysis of the plain radiographic appearance of brodie's abscess. Invest Radiol 1997;32:51-8. [Google Scholar] |
| 6. | Yazdi H, Shirazi MR, Eghbali F. An unusual presentation of subacute osteomyelitis: A talus brodie abscess with tendon involvement. Am J Orthop (Belle Mead NJ) 2012;41:E36-8. [Google Scholar] |
| 7. | Pabla R, Tibrewal S, Ramachandran M, Barry M. Primary subacute osteomyelitis of the talus in children: A case series and review. Acta Orthop Belg 2011;77:294-8. [Google Scholar] |
| 8. | Skevis XA. Primary subacute osteomyelitis of the talus. J Bone Joint Surg Br 1984;66:101-3. [Google Scholar] |
| 9. | Ezra E, Wientroub S. Primary subacute haematogenous osteomyelitis of the tarsal bones in children. J Bone Joint Surg Br 1997;79:983-6. [Google Scholar] |
| 10. | Hamdy RC, Lawton L, Carey T, Wiley J, Marton D. Subacute hematogenous osteomyelitis: Are biopsy and surgery always indicated? J Pediatr Orthop 1996;16:220-3. [Google Scholar] |
| 11. | Ezra E, Khermosh O, Assia A, Spirer L, Wientroub S. Primary subacute osteomyelitis of the axial and appendicular skeleton. J Pediatr Orthop B 1993;1:148-52. [Google Scholar] |
| 12. | Gledhill RB. Subacute osteomyelitis in children. Clin Orthop Relat Res 1973;96:57-69. [Google Scholar] |
| 13. | Hayes CS, Heinrich SD, Craver R, MacEwen GD. Subacute osteomyelitis. Orthopedics 1990;13:363-6. [Google Scholar] |
| 14. | Gaubert J, Mezieres M, Bardier M, Corberand J, Paille P. Subacute or initially chronic osteomyelitis in children. A series of 17 cases- Chir Pediatr 1986;27(6); 339-47. [Google Scholar] |
| 15. | Roberts JM, Drummond DS, Breed AL, Chesney J. Subacute hematogenous osteomyelitis in children: A retrospective study. J Pediatr Orthop 1982;2:249-54. [Google Scholar] |
| 16. | White M, Denison WM. Acute haematogenous osteitis in childhood: A review of 212 cases. J Bone Joint Surg 1952;34-B:608-23. [Google Scholar] |
| 17. | Thakral R, Khan F, Mulcahy D. An unusual case of chronic foot pain: Brodie's Abscess of the talus bone in an adult. Foot and Ankle Surgery. 2006;12:29-31. [Google Scholar] |
| 18. | Rasool MN. Primary subacute haematogenous osteomyelitis in children. J Bone Joint Surg Br 2001;83:93-8. [Google Scholar] |
Fulltext Views
6,947
PDF downloads
2,665





