Translate this page into:
Prognosis of early supervised rehabilitation after knee arthroscopic surgery
*Corresponding author: Rabab S. Zaghlol, Department of Rheumatology and Rehabilitation, Faculty of Medicine, Zagazig Unversity, Zagazig, Egypt. rababzaghlol@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Alzahrani KH, Sayeed AB, Zaghlol RS. Prognosis of early supervised rehabilitation after knee arthroscopic surgery. J Musculoskelet Surg Res, 2023;7:120-7.
Abstract
Objectives:
The anterior cruciate ligament (ACL) is one of the most commonly injured knee ligaments. The majority of ACL tears are treated with arthroscopic reconstruction surgery. However, the literature on early postoperative rehabilitation is deficient. This study aims to determine the effects of early and supervised rehabilitation following an arthroscopic reconstruction on pain and function in the patients. In addition, the impact on rehabilitation unit discharge timing.
Methods:
A retrospective single-center study reviewed all post-operative unilateral arthroscopic ACL reconstructions using hamstring auto-graft with or without arthroscopic meniscectomy or meniscal repair, followed by standardized supervised rehabilitation in the hospital unit, from January 2017 to January 2020. Patients were divided into two groups: Those who started supervised rehabilitation within 14 days and those who started it after 14 days.
Results:
The mean duration from the day of surgery to the start of rehabilitation was (In Group I; mean: 10.97 and standard deviation [SD]: 3.21, in Group II; mean: 27.27 SD: 17.92). Both study groups improved significantly from the baseline in terms of pain, knee flexion and extension, and manual muscle testing (P ≤ 0.05). Patients in Group I who underwent isolated ACL reconstruction had the highest percentage of pain and degree of knee flexion changes (80% and 54.2%, respectively). The discharge time in Group I was faster than in Group II.
Conclusion:
Early supervised rehabilitation after arthroscopic ACL reconstruction can begin within the first 2 post-operative weeks, resulting in faster recovery, reduced total rehabilitation time, and a quicker return to the patient’s previous level of activities.
Keywords
Arthroscopy
Discharge
Knee
Rehabilitation
Supervised
INTRODUCTION
Anterior cruciate ligament (ACL) injury is one of the most common knee injuries. There is a large disparity in the prevalence of ACL injuries worldwide, with some studies reporting that more than 100,000 new ACL injuries occur each year in the United States.[1] ACL reconstruction is performed approximately 2 million times worldwide yearly.[2] Over the past 30 years, the number of arthroscopic ACL reconstructions has increased significantly.[3]
ACL injuries usually affect young, active people, and athletes, and they are more common in those who participate in high-activity sports such as football, basketball, and soccer. It primarily affects overweight/obese subjects and those who reported more weekly training hours. Other risk factors, such as car accidents, lifting heavy objects, and falling from great heights, were unknown.[4]
The estimated time for athletes to return to the pre-injury level of sports after the ACL reconstruction is approximately 1 year.[5] However, only 63% of patients returned to their pre-injury activity levels and only 44% returned to competition.[6] Many factors could contribute to the inability to return to the pre-injury level of sports, such as the type and time of rehabilitation programs, lack of compliance, fear of reinjury, or psychological factors.[7-9]
After different procedures, early post-operative rehabilitation protocols are expected to improve functional ability, reduce the risk of developing future osteoarthritic changes, and facilitate a safe return to sports and work.[10] Post-operative rehabilitation aims to control pain, improve the range of motion (ROM), and strengthen the quadriceps. However, a recent systematic review and meta-analysis on delayed versus accelerated weight-bearing rehabilitation protocol following ACL reconstruction concluded that it is not possible to determine the best time to begin weight-bearing training following ACL reconstruction.[11] Due to the considerable variation in rehabilitation protocols across studies, this study aimed to determine the proper timing and impact of early supervised rehabilitation following an ACL reconstruction with or without arthroscopic meniscectomy or meniscal repair on pain and function among the operated patients for elective arthroscopic knee surgery. The secondary outcome was to assess the impact of early supervised rehabilitation on the discharge timing from the rehabilitation unit.
MATERIALS AND METHODS
A retrospective and single-center study reviewed patient data from January 2017 to January 2020 for all postoperative elective arthroscopic knee cases referred to the rehabilitation unit. The study included all the patients who underwent elective unilateral arthroscopic ACL reconstruction using hamstring autograft followed by standardized supervised post-operative physiotherapy rehabilitation in the hospital unit. Patients were excluded if they had any of the following criteria: revision surgery, knee pain caused by other diseases (e.g., inflammatory arthritis, metabolic joint disease, and autoimmune diseases), or concurrent medical illness that could affect the ability to perform the post-operative rehabilitation program (e.g., systemic cardiovascular, chronic respiratory illness, hearing disorder, psychiatric disorder, deep vein thrombosis, and neurological disease), and patients who elected to perform their post-operative rehabilitation program in other institutes.
Rehabilitation program
A standardized rehabilitation program was performed for all patients postoperatively. The rehabilitation program was developed and adapted collaboratively by sports surgeons and rehabilitation physicians based on the best available published evidence.[12,13] All the physiotherapists were well-trained to follow the approved program. The frequency of supervised physiotherapy was the same for all the patients, and the progression primarily depended on the patient’s condition and response. In addition, all patients received home physiotherapy program instructions from a qualified physiotherapist in the day surgery unit. A detailed printed booklet of the home training program was provided to all patients. In addition, a soft copy was available on the hospital’s official website to be performed daily at home.
The rehabilitation program’s primary intent was to restore muscle strength and improve pain and function. This was conducted through progressive resisted exercises to the quadriceps and hamstrings muscles and knee ROM through active or assisted movement or cycling concerning postoperative weight bearing ability, ROM restrictions, and use of brace frame. Patients were discharged by a multidisciplinary team decision using several criteria, including full active knee ROM, normal gait, appropriate muscle strength of the operated knee, and ability to return to the previous level of daily activities and occupational and recreational participation.[14]
Although the medical records showed that rehabilitation clinic appointments had been scheduled for all cases within the first 14-day postoperatively, not all patients began early. The most common reasons were concern about increased pain during exercises, lack of transportation, or missing appointments. Other factors were patient non-compliance, excess exhaustion, or poor pain management. The flow of participants in the study is illustrated in [Figure 1]. We categorized patients into two groups based on the starting time of the rehabilitation program. Patients who began early supervised rehabilitation during the first 14 days following surgery were classified as Group I (early rehabilitation ≤14 days). In contrast, Group II (late rehabilitation >14 days) was for patients who began the rehabilitation program after 14 days.
Outcome measures
The same physiatrist conducted all patients’ assessments and reassessments. The clinical data were collected from the patients’ medical records. The patients completed self-reported questionnaires at the baseline visit and after 3 months of treatment. The outcome measures used to assess patient outcome include the visual analog scale (VAS) to evaluate the pain,[12,15] and activities of daily living to determine the physical functional abilities.[14] In addition, we collected clinical data such as active knee ROM using a goniometer, Barthel index,[16] and manual muscle testing (MMT),[17] including the medical research council scale.[18]
Data collection technique and tools
Demographic and clinical data were collected accordingly. The collected data were patients age, gender, duration from surgery time to first visit in the rehabilitation clinic, operated side, type of surgery, hospital length of stay, body mass index (BMI), duration of surgery, estimated blood loss, and the discharge time from the rehabilitation unit. In addition, the rehabilitation program was categorized according to the surgical procedure performed: Isolated ACL reconstruction by hamstring graft or in association with partial meniscectomy or meniscus repair.
Statistical analysis
The collected data were coded, entered, presented, and analyzed by computer using Statistical Package for the Social Science version 22. Quantitative variables were expressed as the mean ± standard deviation (SD) and range, and the categorical variables were expressed as numbers and percentages. An independent samples t-test (t) was used for quantitative variables to compare the means of two groups for normally distributed data. In contrast, the Mann–Whitney U test was used for non-normally distributed data. In addition, paired sample t-test was used to detect a difference in the same group before and after the intervention for normally distributed data. At the same time, Wilcoxon signed ranks test was used for non-normally distributed data.
Chi-square and Fisher’s exact tests were used to compare the categorical variables between the two studied groups. In addition, MC “Nemar test was used to detect the difference in the same group before and after the intervention when appropriate.” P ≤ 0.05 was considered statistically significant (S).
RESULTS
Among the 152 patients identified, 102 males met our inclusion criteria [Figure 1], with a mean age of 31.28 ± 6.06 years. The data showed that Group I had 69 patients (67.6%) who began supervised rehabilitation within 14 days, and Group II had 33 patients (32.4%) who began supervised rehabilitation after 14-day postoperatively. Furthermore, the study groups were matched in terms of patient age, BMI, operated side, type of operated lesion, surgical time, hospital length of stay (days), Barthel index, and estimated blood loss [Table 1]. Isolated ACL reconstruction by hamstring graft was found in 57.8% and 42.2% of patients had ACL reconstruction with arthroscopic meniscectomy or meniscal repair [Table 2].

- The flowchart of participants in the study.
| Characteristic | All patients (n=102) | Group I Rehabilitation start ≤14 days (n=69) | Group II Rehabilitation start >14 days (n=33) | P-value |
|---|---|---|---|---|
| Age (years): Mean±SD | 31.28±6.06 | 31.6±6.12 | 32.27±6.02 | a0.608 |
| BMI at admission (kg/m2): Mean±SD | 28.3±4.8 | 28.6±4.8 | 27.6±4.98 | a0.31 |
| Operated side | ||||
| Right n (%) | 59 (57.8) | 44 (63.8) | 15 (45.5) | b0.08 |
| Left n (%) | 43 (42.2) | 27 (36.2) | 18 (54.5) | |
| Hospital length of stay (days): Mean±SD | 0.66±0.47 | 0.65±0.49 | 0.67±0.45 | c0.655 |
| Surgery time (minutes): Mean±SD | 76.1±25.8 | 73.3±30 | 82±53.6 | c0.09 |
| Estimated blood loss (mL): Mean±SD | 115.78±56.72 | 108.11±57.1 | 131.81±79.46 | c0.382 |
| Barthel index: Mean±SD | 95.98±8.2 | 96.23±7.49 | 95.45±9.63 | a0.657 |
| Type of operated lesions | All patients (n=102) (%) | Group I Rehabilitation start ≤14 days (n=69, 67.6%) | Group II Rehabilitation start >14 days (n=33, 32.4%) | P-value |
|---|---|---|---|---|
| Isolated ACL reconstruction by hamstring graft n (%) | 59 (57.8) | 42 (60.9) | 17 (51.5) | a0.371 |
| Combined lesions n (%) | 43 (42.2) | 27 (39.1) | 16 (49.5) |
The mean duration of starting rehabilitation from operation day was 16.24 ± 12 days, with a statistically significant difference between the two groups (In Group I; mean: 10.97 and SD: 3.21, in Group II; mean: 27.27 SD: 17.92) [Table 3].
| Duration from operation time to first rehabilitation clinic visit | All patients (n=102) | Group I Rehabilitation start ≤14 days (n=69) | Group II Rehabilitation start >14 days (n=33) | P-value |
|---|---|---|---|---|
| Mean±SD (days) | 16.24±12.96 | 10.97±3.21 | 27.27±17.92 | c<0.001* |
*Statistically significant(P≤0.05), cMannwhitney test
As shown in [Table 4], both study groups demonstrated statistically significant differences in VAS, degree of knee flexion and extension, and MMT between the first visit of rehabilitation and 3 months later (P = 0.05). As a result, all patients in both groups improved significantly compared to the baseline.
| Outcome measures | Studied groups | P-value | |
|---|---|---|---|
| Group I early rehabilitation started ≤14 days (n=69) | Group II late rehabilitation started >14 days (n=33) | ||
| Visual analog scale | |||
| Baseline (1st visit) | |||
| Mean±SD | 3.91±1.52 | 2.87±1.98 | c0.013* |
| After 3 months | |||
| Mean±SD | 0.95±0.96 | 1.15±1.14 | c0.471 |
| P-value | e<0.001* | e<0.001* | |
| Knee flexion (degrees) | |||
| Baseline (1st visit) | |||
| Mean±SD | 85.76±33.9 | 101.96±19.11 | c0.04* |
| After 3 months | |||
| Mean±SD | 126.25±7.3 | 125.1±11.17 | a0.518 |
| P-value | e<0.001* | d<0.001* | |
| Knee extension (degrees) | |||
| Baseline (1st visit) | |||
| Mean±SD | 4.79±3.48 | 3.36±4.27 | c0.034* |
| After 3 months | |||
| Mean±SD | 0.63±2.3 | 0.63±1.57 | c0.391 |
| P-value | e<0.001* | e0.001* | |
| Manual muscle testing | |||
| Baseline (1st visit) | |||
| Mean±SD | 3.36±0.48 | 3.6±0.32 | a0.012* |
| After 3 months | |||
| Mean±SD | 4.35±0.47 | 4.21±0.37 | a0.135 |
| P-value | d<0.001* | d<0.001* | |
| ADLs Baseline (1st visit) |
|||
| Dependent n (%) | 2 (2.9%) | 2 (6.1%) | b0.441 |
| Independent n (%) | 67 (97.1%) | 31 (93.9%) | |
| After 3 months | |||
| Dependent n (%) | 0 (0.0%) | 0 (0.0%) | ----- |
| Independent n (%) | 69 (100%) | 33 (100%) | |
| P-value | f0.5 | f0.5 | |
Regarding arthroscopic procedures, Group I patients who underwent isolated ACL reconstruction by hamstring graft had the highest percentage of changes in VAS and degree of knee flexion (80% and 54.2%, respectively). In comparison, all patients (100%) in both groups demonstrated a high percentage of change in knee extension [Table 5].
| Outcome measures | Group I early rehabilitation started ≤14 days | Group II late rehabilitation started >14 days | ||
|---|---|---|---|---|
| ACL reconstruction by hamstring graft (n=42) | Combined (n=27) | ACL reconstruction by hamstring graft (n=17) | Combined (n=16) | |
| VAS | ||||
| Baseline (1st visit) | ||||
| Mean±SD | 4.52±1.17 | 2.96±1.53 | 2.35±1.9 | 3.34±1.96 |
| After 3 months | ||||
| Mean±SD | 1.09±1.07 | 0.74±0.71 | 0.94±1.8 | 1.37±1.2 |
| P-value(e) | e<0.001* | e<0.001* | 0.018* | 0.003* |
| Percentage of change | 80 | 66.7 | 50 | 75 |
| Degree of knee flexion | ||||
| Baseline (1st visit) | ||||
| Mean±SD | 81.97±35.12 | 91.66±31.65 | 100.58±20.98 | 103.48±17.84 |
| After 3 months | ||||
| Mean±SD | 126.4±8.91 | 126.11±3.75 | 126.35±12.14 | 123.75±10.24 |
| P-value(e) | e<0.001* | e<0.001* | d<0.001* | d<0.001* |
| Percentage of change | 54.2 | 37.6 | 25.6 | 19.6 |
| Degree of knee extension | ||||
| Baseline (1st visit) | ||||
| Mean±SD | 3.66±3.37 | 6.55±2.91 | 0.58±1.66 | 6.3±4.2 |
| After 3 months | ||||
| Mean±SD | 0.8±2.75 | 0.37±1.33 | 0.0±0.0 | 1.31±2.08 |
| P-value(e) | e<0.001* | e<0.001* | 0.157 | 0.001* |
| Percentage of change | 100% | 100% | 100% | 100% |
The early supervised rehabilitation that began within 14 days in Group I compared to Group II resulted in a shorter timeframe to discharge from the rehabilitation unit [Table 6]. The majority of Group I patients (94.2%) were discharged at 4 months, while only 57.6% of patients in Group II were discharged at 4 months [Figure 2].
| Discharge time | Group I (n=69) | Group II (n=33) | P-value | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Within 4 months | 65 | 94.2 | 23 | 57.6 | 0.001* |
| After 4 months | 4 | 5.8 | 10 | 42.4 | |
Chi-square test, *Statistically significant (P≤0.05). ACL: Anterior cruciate ligament
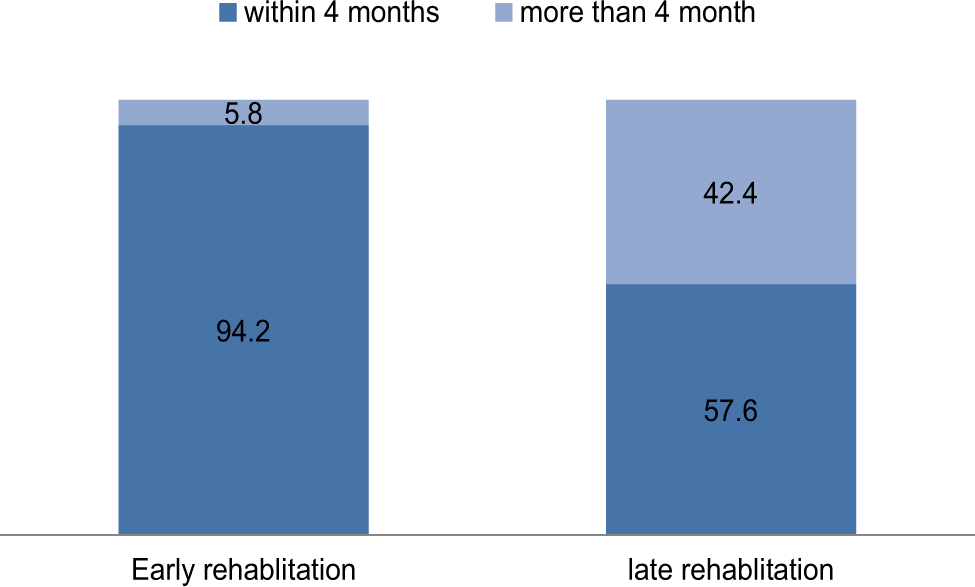
- Percentage of discharge time in postoperative knee arthroscopic patients with comparison of both studied groups.
DISCUSSION
Post-operative rehabilitation is crucial to achieving successful and satisfactory outcomes in arthroscopic ACL reconstruction patients.[18-20] However, information on the appropriate timing and prognosis of early rehabilitation is limited. Early supervised rehabilitation in the present work was presumed to begin within the first 14-day postoperatively. To the best of our knowledge, this is the first study that describes the outcome of early supervised rehabilitation following an arthroscopic knee ACL reconstruction with or without meniscectomy or meniscal repair.
Our study showed that the highest percentage of improvement in VAS and degree of knee flexion was noticed within Group I patients who started early supervised rehabilitation. Most patients who started rehabilitation within 14 days were discharged at 4 months (94.2%). Therefore, it can be speculated that early supervised rehabilitative exercise provided in our proposed protocol could decrease the length of rehabilitation sessions and positively influence patients’ capacity to return to regular daily activities.
It has been shown that early initiation of quadriceps exercises in the post-operative period has improved early ROM.[21] In addition, early quadriceps strength and ROM restoration will promote active patient participation in the subsequent rehabilitation phases. Compared to standard rehabilitation, a randomized and controlled study evaluating early progressive eccentric exercise beginning 3 weeks following ACL reconstruction found that early progressive eccentric exercise resulted in significant gains in quadriceps femoris and gluteus maximus muscle mass.[22] Therefore, different training activities can be carried out on the knee joints and ensure long-term ROM maintenance and reduce the risk of arthrofibrosis.[23]
Although most of the studies mentioned above stressed the benefit of early post-operative rehabilitation exercises, they did not address the appropriate timing to start a supervised program nor the duration of supervised rehabilitation before discharge. Our results demonstrated the benefits of early supervised rehabilitation that helps patients gain the required functional abilities and encourages early discharge to return to regular duties.
After a comprehensive literature review, we found limited studies addressing early supervised rehabilitation’s impact on ACL reconstruction outcomes. However, a qualitative focus group analysis to study patients’ barriers and facilitators of rehabilitation after ACL reconstruction suggested that less intensive supervised rehabilitation might be a viable option for patients who cannot afford supervised rehabilitation, have limited access to physiotherapy, or are highly motivated to perform their rehabilitation independently.[24]
In contrast to these findings, a systematic review investigating knee arthroscopic surgery rehabilitation exercises’ efficacy concluded that supervised and home programs were equally effective.[25] These implications were clarified by a randomized controlled study, which found that the exercise group had statistically significant functional improvements compared to the control group (without a home exercise program). Therefore, possibly a more relevant finding is that well-planned physiotherapy exercise programs delivered either in a hospital setting or in a home setting are beneficial.[26]
Furthermore, a questionnaire survey of expert knee surgeons in Australia was undertaken to determine the recommended timing for beginning post-operative rehabilitation following ACL reconstruction showed that rehabilitation was routinely recommended at a mean of 2 weeks postoperatively.[27] Notably, this finding is consistent with our recommendation to start supervised rehabilitation protocol for ACL patients within 2 weeks after surgery.
It must be noted that rehabilitation after knee ACL reconstruction has no time constraints. There is no defined time frame for returning to any activity. Depending on their functional progression, patients usually return to sports 6 months after surgery.[26]
It has been shown that delaying the initiation of rehabilitation for more than 1 month following reconstruction was associated with negative objective outcomes.[28] Therefore, we believe that obtaining early post-operative supervised rehabilitation exercises allows the patients to reduce the duration of the rehabilitation program and eventually get discharged earlier. However, current evidence still recommends cautiously choosing post-operative rehabilitation programs.[11] Regardless, patients’ programs should be individually prescribed and monitored to ensure that the rehabilitation protocol is followed and that they progress without adverse events.[29]
The present study has some limitations as this is a retrospective analysis, but we should point out that rehabilitation protocols were applied uniformly to all the patients. Another limitation that can be considered is that the protocol’s influence on physical activity and muscle endurance was not sufficiently assessed in this study. Moreover, the fact that it was a single-center study. Further multi-center research with longer follow-up is needed to assess the long-term prognosis.
CONCLUSION
Early supervised rehabilitation after arthroscopic ACL reconstruction can begin within the first 2 postoperative weeks, resulting in faster recovery, reduced total rehabilitation time, and a quicker return to the patient’s previous level of activities.
RECOMMENDATIONS
The actual timing and prognosis of early rehabilitation are limited after elective knee arthroscopy. A future randomized and controlled study is recommended to validate the early rehabilitation strategy’s benefits and efficacy following arthroscopic knee surgery throughout long-term follow-up.
AUTHORS’ CONTRIBUTIONS
KHA, ABS, and RSZ conceived and designed the study and provided research materials. KHA, ABS, and RSZ collected and organized data. KHA, ABS, and RSZ analyzed and interpreted data and wrote the initial and final draft of the article. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
ETHICAL APPROVAL
The approval was obtained from the Security Forces Hospital ethics committee, Makkah No. SFHM-IRB 0378-02092, dated: 09/14/2020. The study was conducted in accordance with the ethical standards of the Declaration of Helsinki.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms for this study. In the form, the patients have given their consent for the images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study received no specific grant from public, commercial, or not-for-profit funding agencies.
References
- Three distinct mechanisms predominate in non-contact anterior cruciate ligament injuries in male professional football players: A systematic video analysis of 39 cases. Br J Sports Med. 2015;49:1452-60.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament injury risk in sport: A systematic review and meta-analysis of injury incidence by sex and sport classification. J Athl Train. 2019;54:472-82.
- [CrossRef] [PubMed] [Google Scholar]
- The Danish knee ligament reconstruction registry. Clin Epidemiol. 2016;8:531-5.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence and determinants of anterior cruciate ligament rupture among athletes practicing football in Jeddah Avenues 2020. J Family Med Prim Care. 2022;11:4528-35.
- [CrossRef] [PubMed] [Google Scholar]
- Fear of reinjury in athletes: Implications for rehabilitation. Sports Health. 2017;9:162-7.
- [CrossRef] [PubMed] [Google Scholar]
- Return to sport following anterior cruciate ligament reconstruction surgery: A systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45:596-606.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical decision algorithm associated with return to sport after anterior cruciate ligament reconstruction. J Athl Train. 2020;55:691-8.
- [CrossRef] [PubMed] [Google Scholar]
- Failure to return to preinjury activity level after hamstring anterior cruciate ligament reconstruction: Factors involved and considerations in goal setting. Indian J Orthop. 2019;53:714-20.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with psychological readiness to return to sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2018;46:1545-50.
- [CrossRef] [PubMed] [Google Scholar]
- Principles of postoperative anterior cruciate ligament rehabilitation. World J Orthop. 2014;5:450-9.
- [CrossRef] [PubMed] [Google Scholar]
- Delayed versus accelerated weight-bearing rehabilitation protocol following anterior cruciate ligament reconstruction: A systematic review and meta-analysis. J Rehabil Med. 2022;54:jrm00260.
- [CrossRef] [PubMed] [Google Scholar]
- Teaching your patient to use a pain rating scale. Nursing. 2002;32:17.
- [CrossRef] [PubMed] [Google Scholar]
- Rehabilitation and return to play after anatomic anterior cruciate ligament reconstruction. Clin Sports Med. 2013;32:165-75.
- [CrossRef] [PubMed] [Google Scholar]
- Studies of illness in the aged: The index of ADL: A standardized measure of biological and psychosocial function. JAMA. 1963;185:914-9.
- [CrossRef] [PubMed] [Google Scholar]
- The verbal numeric pain scale: Effects of patient education on self-reports of pain. Acad Emerg Med. 2006;13:853-9.
- [CrossRef] [PubMed] [Google Scholar]
- The Barthel ADL Index: A reliability study. Int Disabil Stud. 1988;10:61-3.
- [CrossRef] [PubMed] [Google Scholar]
- Daniels and Worthingham's Muscle Testing: Techniques of Manual Examination (8th ed). St. Louis, Mo: Saunders Elsevier; 2007.
- [Google Scholar]
- Early functional rehabilitation after meniscus surgery: Are currently used orthopedic rehabilitation standards up to date? Rehabil Res Pract. 2020;2020:3989535.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of accelerated rehabilitation for arthroscopic anterior cruciate ligament (ACL) reconstruction in football players. Int J Phys Med Rehabil. 2016;4:1-5.
- [CrossRef] [Google Scholar]
- Rehabilitation following meniscal repair: A systematic review. BMJ Open Sport Exerc Med. 2018;94:e000212.
- [CrossRef] [PubMed] [Google Scholar]
- Do early quadriceps exercises affect the outcome of ACL reconstruction? A randomised controlled trial. Aust J Physiother. 2005;51:9-17.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of early progressive eccentric exercise on muscle size and function after anterior cruciate ligament reconstruction: A 1-year follow-up study of a randomized clinical trial. Phys Ther. 2009;89:51-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arthrofibrosis following ACL reconstruction-reasons and outcome. Arch Orthop Trauma Surg. 2004;124:518-22.
- [CrossRef] [PubMed] [Google Scholar]
- Such a massive part of rehab is between the ears'; Barriers to and facilitators of anterior cruciate ligament reconstruction rehabilitation: A qualitative focus group analysis. BMC Sports Sci Med Rehabil. 2022;14:106.
- [CrossRef] [PubMed] [Google Scholar]
- The effectiveness of postoperative physical therapy treatment in patients who have undergone arthroscopic partial meniscectomy: Systematic review with meta-analysis. J Orthop Sports Phys Ther. 2013;43:560-76.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of functional exercise training on performance and muscle strength after meniscectomy: A randomized trial. Scand J Med Sci Sport. 2009;19:156-65.
- [CrossRef] [PubMed] [Google Scholar]
- Current Australian trends in rehabilitation following anterior cruciate ligament reconstruction. Knee. 2002;9:121-6.
- [CrossRef] [PubMed] [Google Scholar]
- Factors affecting subjective and objective outcomes and return to play in anterior cruciate ligament reconstruction: A retrospective cohort study. Joints. 2018;6:23-32.
- [CrossRef] [PubMed] [Google Scholar]
- Aspetar clinical practice guideline on rehabilitation after anterior cruciate ligament reconstruction. Br J Sports Med 2023:1-15. ahead of print
- [CrossRef] [PubMed] [Google Scholar]







